ORIGINAL ARTICLE | https://doi.org/10.5005/jp-journals-10079-1035 |
Technical Trick to Avoid Intra-articular Screw Placement in Posterior Wall Fractures of the Acetabulum
1–6Department of Trauma and Orthopaedics, Ganga Hospitals Private Limited, Coimbatore, Tamil Nadu, India
Corresponding Author: Sivakumar S Palanivelayutham, Department of Trauma and Orthopaedics, Ganga Hospitals Private Limited, Coimbatore, Tamil Nadu, India, Phone: +91 9994465917, e-mail: drspsiva@gmail.com
How to cite this article Perumal R, Patra SK, Sivakumar SP, et al. Technical Trick to Avoid Intra-articular Screw Placement in Posterior Wall Fractures of the Acetabulum. J Orth Joint Surg 2021;3(1):7–12.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Introduction: Screw placement at the posterior margin of the acetabulum while operating for wall fractures requires additional care to avoid articular penetration which can lead to poor functional outcomes. The main objective of this study is to describe a simple four-step surgical guide to avoid intra-articular screw penetration during fixation.
Materials and methods: We prospectively analyzed 23 patients (21 males and 2 females) with posterior wall acetabular fractures treated with the described technique in our institution from 2017 to 2019. Of these 23 patients, 8 patients had isolated posterior wall fractures, 9 patients had transverse with posterior wall fracture, and 6 patients had posterior wall and column fractures. Radiograph Judet views and computerized tomography (CT) scan were done in all the patients to check for intra-articular screws on the second postoperative day.
Results: By radiograph and CT scan in all the patients, there was no intra-articular screw penetration noticed following acetabular fracture fixation. All the 23 patients in our study had a good functional outcome with Merle D’aubigne score of ≥18 in 12 patients and ≥10 in 11 patients.
Conclusion: Good knowledge of the osseous anatomy of the pelvis is essential to prevent intra-articular screw placement during fixation of acetabular fractures. Our four-step surgical tip to insert periacetabular screws under direct vision helps prevent intra-articular screw placement during acetabular fracture fixation by posterior approach. Besides, this technique is easily reproducible and helps to minimize intraoperative radiation time.
Keywords: Four-step technical guide, Hip posterior approach, Periacetabular screws positioning, Posterior acetabular wall fractures, Screw insertion technique..
INTRODUCTION
Posterior wall fractures of the acetabulum are common and comprise approximately 20–30% of all acetabular fractures.1 Operative intervention is the gold standard to treat unstable and incongruous acetabular fractures.2–5 The main goals of surgery are joint stability and early mobilization, which can be achieved by anatomic reduction and rigid internal fixation.5 Open reduction and internal fixation of acetabular fractures often require insertion of screws close to the articular surface.1 Errant screw placement into the joint, although uncommon, can lead to arthrosis with a poor functional outcome despite otherwise satisfactory fracture reduction and fixation.6,7
In addition to using meticulous surgical techniques and having a general familiarity with the osseous anatomy of the pelvis, surgeons use intraoperative and postoperative radiographic imaging to evaluate possible joint penetration by periacetabular screws.6–8 Intraoperative detection of errant screw placement is more important, as corrective action can be taken before completion of the surgical procedure.7 Fluoroscopy and postoperative computerized tomography (CT) imaging are not without error and can result in false-positive or negative predictions coupled with dangers of radiation exposure for the surgeon and the patient.7 Intra-articular screw penetration is one of the recognized technical complications in acetabulum fixation.8 Intra-articular screw placement can lead to damage of the femoral head possibly ending up with arthritis of the joint.7,9 To address this, we devised an innovative intraoperative technique to prevent intra-articular screw placement in posterior wall fractures.
MATERIALS AND METHODS
We have prospectively analyzed 23 patients with posterior wall acetabular fractures treated with the described technique using posterior Kocher–Langenbeck’s approach in our institution from 2017 to 2019. Of these 23 patients, 8 patients had isolated posterior wall fractures, 9 patients had transverse with posterior wall fracture, and 6 patients had posterior wall and column fractures. There were 21 male and 2 female patients. The mean age was 41 years (range, 18–64 years) and the mean follow-up was 1.6 years (range, 1–3 years). Seven out of 23 patients presented with hip joint fracture-dislocation and all of them were reduced immediately in the emergency department. Radiograph Judet views and CT scan were done in all the patients to check for intra-articular screws on the second postoperative day.
SURGICAL TECHNIQUE
This technique is best suited to prevent joint penetration during lag screw placement for posterior wall fracture fragments that occur in isolation or combination with posterior column or transverse fractures. Following combined spinal and epidural anesthesia, the patient is positioned in the lateral position on a standard radiolucent operating table. The Kocher–Langenbeck approach is used to expose and isolate the fracture fragments. As demonstrated in the saw bone model in Figure 1A, we intend to reduce the posterior wall fragments with lag screws without joint penetration through four simple steps. First, the posterior wall fracture fragments were provisionally fixed after reduction with Kirschner wires (K wire) inserted at an angle >45° to the joint surface (Fig. 1B). Then one K-wire was removed, the fragment was drilled with an appropriately sized drill bit with the same angulation and a short lag screw (2.4 or 3.5 mm cortical screw) was inserted (just longer than the fragment length to cross the fracture site (Fig. 1C). Thirdly, the K-wires and lag screws were removed and the undersurface of the fragment was inspected for any screw cut out. A probe/depth gauge/guidewire or Kirschner wire was inserted into the drilled tract and the posterior wall along with the capsule was lifted and the joint was distracted to visualize if there has been any articular penetration by the screw threads by moving the probe around (Fig. 1D). After visually confirming the absence of screw penetration (inability to visualize the probe), the fourth step involves reducing the fragment and fixing it with a longer appropriately sized lag screw (2.4 or 3.5 mm cortical screw) through the same drilled tract (Fig. 1E). 2.4 mm cortical screw was used if fragment size was %3C;2 and 3.5 mm cortical screw was used for fragment size %3E;2 cm. The surgeon involved in the study had practiced the technique an adequate number of times prior in the saw bone model; hence, the direction of drilling the track was optimal in all the cases and we did not have any repeated attempts of screw drilling.

Figs 1A to E: (A) Saw bone model demonstrating fragments of posterior wall fracture; (B) Step 1: Fragment reduction and provisional K-wire fixation. Inserted at an angle >45°; (C) Step 2: K-wire replaced with an appropriate sized drill and a short lag screw inserted; (D) Step 3: Implants removed and under surface of articular fragments visualized for screw cut out. Probe inserted through the drilled tract and joint distracted to visualize the articular surface for screw thread penetration using the probe; (E) Step 4: Re-fix the fracture with appropriate sized lag screw
Additional plates are added based on fracture stability, fragment size, and based on the presence of an added posterior column or transverse fracture. The wound is closed in layers over a suction drain. Pelvis AP, Obturator Iliac (three views) are taken intraoperatively at the end of the procedure and in the postoperative period before discharging the patient. Computerized tomography scan was done in all the patients to check for intra-articular screws on the second postoperative day. Additional fluoroscopic views during drilling and screw insertion were avoided during the procedure. Postoperatively patients are mobilized on the 2nd postoperative day, non-weight bearing with walker support. Prophylaxis for deep vein thrombosis is given for 1 month postoperatively (75 mg aspirin, once a day). Partial weight-bearing with walker support is started at the end of 1 month and full weight bearing is started at the end of 2 months. Patients were screened with monthly radiographs for 6 months to look for osteonecrosis. Following this, patients were followed up once in 3 months up to 1 year and then yearly.
CASE DESCRIPTIONS
Case 1
Figure 2A shows the preoperative X-ray of a 55-year-old man with posterior dislocation of the hip with an associated posterior wall fracture. Following closed reduction, the CT scan showed an incongruent right hip due to an intra-articular fragment (Fig. 2B). Figure 2 shows our technique of probe placement in the short screw tract and distracting the joint to look for screw penetration. Figure 2 shows the postoperative X-rays of the same patient with an uneventful outcome.
Case 2
Figure 3 shows the preoperative and postoperative X-ray of a 58-year-old man with an acetabular fracture for which fixation was done using our four-step surgical guide technique to avoid Intra-articular screw placement.
RESULTS
Of the 214 cases of acetabulum fractures operated from 2012 to 2018, this technique was performed in 23 cases with posterior wall fractures. Of these 23 patients, there were 8 cases of isolated posterior wall fracture, 9 cases of transverse with posterior wall fracture, and 6 cases of the posterior wall and column fracture. The study population comprised 21 male and 2 female patients. Two patients had Brooker Class II Heterotopic Ossification which did not require any further intervention. There was no surgical Site infection in any of the patients. All the 23 cases in our study had good functional outcomes with Merle D’aubigne score of ≥18 in 12 cases and ≥10 in 11 cases.
Before the use of this technique, there was one case of screw penetration into the joint in a posterior wall fracture (Fig. 4). Following the introduction of this technique, there have been no instances of intra-articular screw penetration, confirmed by intraoperative fluoroscopy, postoperative X-rays, and CT scans.

Figs 2A and B: (A) Intra-articular screw placement prior to the introduction of this technique; (B) CT revealed intraarticular screw
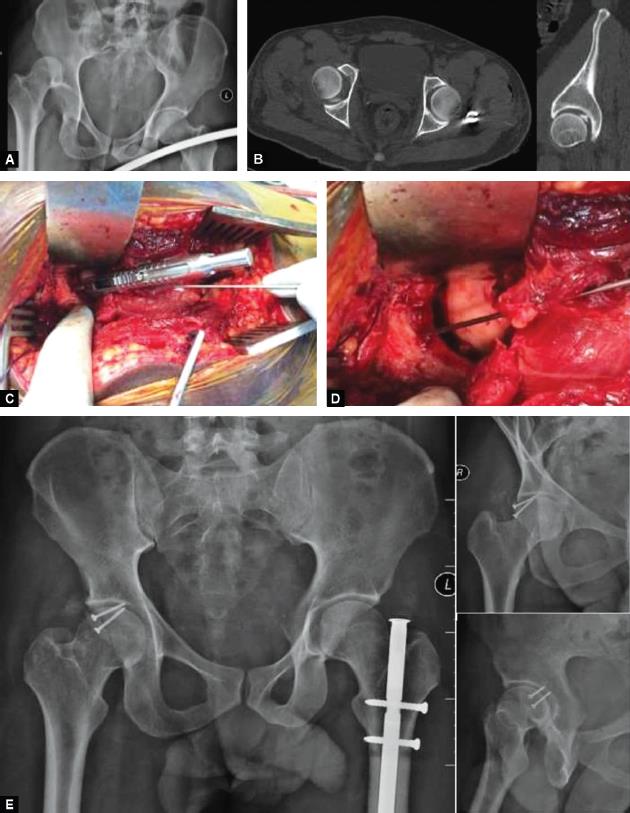
Figs 3A to E: (A) Fracture dislocation of right hip; (B) CT scan—Incongruent right hip due to intra-articular fragment; (C) Probe placement in short screw tract; (D) Distracting the joint to look for screw penetration; (E) Postoperative X-rays showing an uneventful outcome
DISCUSSION
The outcome of acetabular fracture surgery depends on the injury of the articular portion of the acetabulum and the femoral head and the ability to achieve anatomic reduction while avoiding intra-articular screw placement.2,3,10,11 Recent increase in geriatric acetabular fractures in the last 20 years represents a surgical challenge as more rigid fixation is needed in osteoporotic bones especially in those patients who are unable to comply with non-weight bearing protocol postoperatively.12 Most posterior wall fractures require rigid and stable internal fixation along with an anatomic reduction to achieve an excellent radiological and functional outcome, which often necessitates the placement of screws near the articular margin.
Intra-articular screw perforation rates of 0.9–7% are reported.1,13,14 Screw penetration into the joint can lead to disastrous outcomes, as seen from our case example (Fig. 4), causing increased morbidity to the patient in the form of prolonged hospital stay, re-surgery, poor function despite anatomical reduction and can also open up the operating surgeon to possible litigation.15,16 Thus, detecting errant screw placement intraoperatively is of paramount importance as corrective action can be taken immediately.7 Early discovery and removal of intra-articular screws are imperative to avoid mechanical erosion of the articular cartilage.6,7
Although meticulous surgical technique, experience, and familiarity with the osseous anatomy of the pelvis play a major role, several techniques have been described to detect or prevent joint penetration by screws.7 These include intraoperative fluoroscopy, navigation, postoperative CT scan, knowledge of the danger zone, and use of the safe zone for screw insertion.5,8,11 Posterior approaches with an arthrotomy (extended iliofemoral approach or surgical hip dislocation) also allow direct visual confirmation of extra-articular screw placement.11

Figs 4A and B: (A) Preoperative X-ray and CT scan—Dislocation of left hip with acetabular fracture; (B) Postoperative X-ray following fixation using four-step surgical guide
Intraoperative fluoroscopy and postoperative CT scans are widely used to detect Intra-articular screw placement. In fluoroscopy, the axial (“barrel”) view and the tangential view have been described as the best methods for visualizing the entire screw for this purpose.7 Carmack et al. have demonstrated that sensitivity, specificity, and percent correct interpretations were 95%, 84%, and 90%, respectively, for axial fluoroscopy and 85%, 89%, and 87% for tangential fluoroscopy, 100%, 84%, and 92% for the computed tomography scans with a 1-mm slice thickness at 1-mm intervals; and 100%, 58%, and 79% for the computed tomography scans with a 4-mm slice thickness at 3-mm intervals.7 Because of the spherical shape of the acetabulum, if the entire screw is demonstrated to be clear of the joint on any projection it must be extra-articular in fluoroscopy.7 Both these techniques expose the patient and the operating team (in the case of fluoroscopy) to harmful ionizing radiation. Often tangential fluoroscopy shows false-positive results owing to the inability to obtain a true tangential view due to obstruction of the C-arm by the patient’s torso on the operating table.7 Similarly, the large head of the 3.5 mm screw, directly overlying the joint may often lead to difficulty in interpreting the axial view. Problems with X-ray penetration related to the limitations of c-arm technology combined with patient-related factors (such as residual intracolonic contrast material, bowel gas, overlying drapes, patient positioning, and obesity) compromise its effectiveness. Postoperative CT through sensitivity necessitates a second surgery to revise the errant screw placement and is expensive. Further, there is a possibility of obscured screw position owing to artifacts, and false-positive reports of screw penetration owing to magnification with CT scans.7
Marvin Tile defined the danger zone of the acetabulum, as that part of the posterior wall and column at the mid-acetabulum lying above the ischial spine. Screws inserted in the danger zone are at risk of violating the hip joint. Unfortunately, this zone is frequently used in the fixation of the posterior wall and column fractures Screws placed at the margin of the danger zone and directed perpendicular to the posterior column tend to violate the hip joint.8 Ebraheim et al. analyzed 1 cm cross-sections through the acetabulum on cadavers and developed safe anatomic pathways for screw placement.8 They found that cortical screws (4.5 mm), placed at entry points of 2 and 3 cm medial to the lateral acetabular margin and angled medially 45° and 15°, respectively, did not violate the hip joint. The screws were angulated perpendicular to the posterior column. In this study, the average width of the posterior column at the mid-acetabular level was 4.8 cm. Guy et al. devised a safe zone for screw placement in the treatment of acetabular fractures when operated by an anterior approach.11
Our study describes a sequential four-step technique to avoid Intra-articular screw penetration in a saw bone model, and is superior to our control of the initial 21 cases which were operated by the same surgeon using the technique as described by Bosse in which the screws were inserted perpendicular to the body surface and we had one instance of intra-articular screw penetration among these cases.17 Our technique does not involve repeated exposure to harmful ionizing radiation as the joint is distracted and the screw tract is examined under direct vision. We used smaller 1.5 mm K-wires to ensure we get an adequate purchase during screw insertion. The posterior wall fragments were carefully handled during K-wire insertion, probe inspection, and screw insertion to avoid devascularization of the fragment. It is not time-consuming (when compared to navigation and fluoroscopy) and does not require any extensive preoperative planning or specialized instrumentation.18 The number and size of the K-wires used for provisional stabilization and the size of the screw used for fixation (2.4 or 3.5 mm) varied based on the size of the posterior wall fragment. Many such techniques have been described before but a proper four-step surgical guide with sequential steps in a saw bone model with zero failure has been demonstrated for the first time.
The limitation of the study was that it is possible that a screw could have penetrated the subchondral bone and violated the articular cartilage but not have penetrated the chondral surface and thus will not be directly visible. Such screws would, however, be detected by fluoroscopy, and hence we do recommend the use of fluoroscopy particularly when there is an unfamiliar resistance during screw insertion. Another limitation of this technique is that it is not feasible to reproduce the technique in case of severely comminuted posterior wall fractures or posterior wall fractures with marginal impaction as it is difficult to identify the drill hole through the comminuted fracture fragments. Also, in comminuted fractures and osteoporotic bone, there may be a loss of reduction due to the loosening of screws put through already drill holes. A multicentric study is needed in the future to know the reproducibility of the technique by other surgeons.
CONCLUSION
Insertion of periacetabular screws demands precise positioning to rigidly reconstruct the articular fragments while avoiding penetration of the articular surface. Our simple technique offers a readily reproducible alternative to prevent intra-articular screw placement thereby avoiding mechanical erosion of the articular cartilage which helps in obtaining an excellent functional outcome.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
1. Letournel E, Judet R. Fractures of the Acetabulum.New York, NY: Springer; 1993. pp.67–88.
2. Matta JM. Fracture of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. Orthopedic Trauma Directions 2011;9(02):31–36. DOI: 10.1055/s-0030-1267077.
3. Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res 2003;407(407):173–186. DOI: 10.1097/00003086-200302000-00026.
4. Giannoudis PV, Tzioupis C, Moed BR. Two-level reconstruction of comminuted posterior-wall fractures of the acetabulum. J Bone Joint Surg Br Vol 2007;89(4):503–509. DOI: 10.1302/0301-620X.89B4.18380.
5. Wu X, Chen W, Zhang Q, et al. The study of plate-screw fixation in the posterior wall of acetabulum using computed tomography images. J Trauma Acute Care Surg 2010;69(2):423–431. DOI: 10.1097/TA.0b013e3181ca05f6.
6. Kellam JF, Tile M. Surgical techniques. In: ed. M, Tile ed. Fractures of the Pelvis and Acetabulum.Baltimore: Williams and Wilkins; 1995. pp.355–396.
7. Carmack DB, Moed BR, McCarroll K, et al. Accuracy of detecting screw penetration of the acetabulum with intraoperative fluoroscopy and computed tomography. JBJS 2001;83(9):1370–1375. DOI: 10.2106/00004623-200109000-00012.
8. Ebraheim NA, Savolaine ER, Hoeflinger MJ, et al. Radiological diagnosis of screw penetration of the hip joint in acetabular fracture reconstruction. J Orthop Trauma 1989;3(3):196–201. DOI: 10.1097/00005131-198909000-00003.
9. Tile M, Helfet DL, Kellam JF. Fractures of the Pelvis and Acetabulum.Baltimore: Williams and Wilkins; 1995. pp.419–495.
10. Letournel E. Acetabulum fractures: classification and management. Orthop Trauma Directi 2007;5(05):27–33. DOI: 10.1055/s-2007-980136.
11. Guy P, Al-Otaibi M, Harvey EJ, et al. The ‘safe zone’ for extra-articular screw placement during intra-pelvic acetabular surgery. J Orthop Trauma 2010;24(5):279–283. DOI: 10.1097/BOT.0b013e3181bfcebf.
12. Sullivan MP, Baldwin KD, Donegan DJ, et al. Geriatric fractures about the hip: divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics 2014;37(3):151–157. DOI: 10.3928/01477447-20140225-50.
13. Gras F, Marintschev I, Klos K, et al. Screw placement for acetabular fractures: which navigation modality (2-dimensional vs. 3-dimensional) should be used? An experimental study. J Orthop Trauma 2012;26(8):466–473. DOI: 10.1097/BOT.0b013e318234d443.
14. Li Z, Li J, Li Z, et al. Comparative study of anatomical locking plate and reconstruction plate in treating acetabular fractures. Int Orthop 2021. 1–8. DOI: 10.1007/s00264-021-04970-1.
15. Yoon S, Park M, Matsuda DK, et al. Endoscopic resection of acetabular screw tip to decompress sciatic nerve following total hip arthroplasty. BMC Musculoskel Disord 2018;19(1):1–6. DOI: 10.1186/s12891-018-2091-x.
16. Ayob KA, Merican AM, Sulaiman SH, et al. The tale of two vessels, vascular complications following a breach of the pelvic inner table due to acetabular screws: a report of two cases. J Dis Relat Surg 2021;32(1):239–244.
17. Bosse MJ. Posterior acetabular wall fracture: a technique for screw placement. J Orthop Trauma 1991;5(2):167–172. DOI: 10.1097/00005131-199105020-00008.
18. Duncan JM, Nahas S, Akhtar K, et al. The use of a 3D printer in pre-operative planning for a patient requiring acetabular reconstructive surgery. J Orthop Case Rep 2015;5(1):23. DOI: 10.13107/jocr.2250-0685.247.
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.