section 1
Basic principles
Anatomy of the upper limbChapter 1
INTRODUCTION
2
3The upper limb, especially the hand, consists of multiple structures that together form a unique and versatile part of the body. To have a better understanding of the pathologic conditions compromising the function of the upper extremity, it is essential to have a detailed and in-depth appreciation of the normal patterns and functions of the anatomic constituents of the hand and the upper limb. In this chapter, we will discuss the relevant surface anatomy, skeletal framework, articular, musculotendinous, vascular, and nervous systems of the upper limb, with a particular emphasis on the anatomy of the hand.
TERMINOLOGY
First, it is important to be familiarized with the general terms and phrases used to describe joints movement, as well as the anatomic and topographic features of the upper limb. The use of a standardized terminology facilitates communication and avoids confusion between hand surgeons and between surgeons and other health-care professionals when describing upper limb pathology (Figure 1.1 a and b).
Figure 1.1: (a) Normal range of motion of the hand and forearm. Standard nomenclature and palmar surface of the palm.
Palmar/volar surface
This is the anterior surface of the hand, incorporating thick glabrous (hairless) skin with noticeable skin creases over the palm and fingers. More proximal, the anterior surface of the wrist and the forearm is known as the volar surface.
Dorsal surface
This is the posterior surface of the hand and forearm. In the hand, the dorsal surface is covered with thin mobile skin containing hair follicles.
Radial and ulnar borders
The radial border of the hand/upper limb is the side that is furthest away from the midline of the body containing the thumb, whereas the ulnar border of the hand/upper limb is the side closest to the midline and contains the small finger.
Abduction and adduction
Abduction is moving a body part away from the midline, whereas adduction is the opposite and means moving toward the midline. In the hand, the long finger is considered the midline of the hand, and therefore, finger abduction is spreading the fingers away from the long finger, whereas finger adduction is bringing the fingers together toward the long finger.
Flexion and extension
By definition, flexion is a bending movement that decreases the angle between two body parts, whereas extension is a straightening movement that increases the angle between body parts (e.g. wrist joint flexion and extension movements).
Pronosupination
This describes the inward (pronation) and outward (supination) rotation of a joint along its longitudinal axis, and is often used to describe the rotatory movement of the forearm at the proximal and distal radioulnar joints (DRUJs) (Figure 1.1 a).
EXTERNAL ANATOMY OF THE HAND
Skin and hand creases
Each hand consists of five rays/digits (standard nomenclature: thumb, index, long, ring, and small fingers), a palmar and a dorsal surface, attached proximally to the wrist joint, and is covered by a specialized skin envelope. Besides being a protective layer against infections and other types of injuries, the skin coverage of the hand has a remarkable ability of functional adaptation, and one of its major roles is enhancing the prehensile ability of the hand when executing daily activities.
The palmar and dorsal skin of the hand is functionally and anatomically different, each serving a specific purpose. On the palm, the skin is composed of thick keratinized papillary squamous epithelium that helps it withstand the shearing forces resulting from daily use of the hand. The dorsal skin is supple, thin, and mobile to allow the unrestricted movement of the underlying joints. By looking on the palm, one can see three distinct types of skin lines (Figure 1.1 b).
- Thick skin creases: Seen over the wrist joint (proximal and distal wrist creases), the palm (three palmar skin creases), and over the metacarpophalangeal (MCP) and interphalangeal (IP) joints of the fingers. These skin creases are tethered to the deep fascia, which stabilize the palmar skin and prevent skin gliding over the hand when handling objects. Additionally, these skin creases are sometimes referred to as the skin joints or folds; this is clinically important, because if a flexion crease is absent, this means that the underlying joint has not been moving, often seen in congenital conditions such as arthrogryposis when the joints are not developed normally.
A fine network of prominent skin folds known as the papillary ridges. The skin papillary ridges serve two important functions: first a tactile function (sense of touch) and second a mechanical function. A moist palm due to secretion of sweat together with these papillary ridges creates a friction coefficient that prevents slipping of objects during prehension. Tension skin lines, also known as Langer lines. It is postulated that along these lines, skin incisions would result in the least amount of scarring when the skin is closed by primary intention.
Underneath the skin is a layer of a fatty tissue, which is divided into fat lobules by fibrous septa extending from the skin to the deep fascia. This creates areas of prominent fat pads that are most noticeable over the hypothenar muscles, thenar muscles, the metacarpal arch, and over the fingers in between joint creases. The fat cushions/pads protect the hands against external forces and allow the hands to conform nicely around objects of various shapes, thus improving the act of prehension.
On the dorsum of the hand, the skin is thin owing to the much thinner dermis and epidermis as well as the lack of fat pads, when compared with the palmar skin. Additionally, the dorsal skin is very mobile due to the loose attachment it has with the deeper tissue. In spite of this great mobility, the skin on dorsum of the hand becomes maximally stretched when making a fist. It is important to realize this limitation when reconstructing soft tissue defects over the dorsum of the hand, as solely relying on skin mobility may not be sufficient to cover or reconstruct wound defects over the dorsum of the hand.
Arches of the hand
When the forearm is supinated and the hand is resting on a flat surface, a concavity is seen on the palmar surface of the hand. Three arches form the shape of this concavity: (1) The proximal transverse arch; (2) longitudinal arch(s); and (3) distal transverse arch, spanning the palmar surface of the hand (Figure 1.2).
- Proximal transverse (carpal arch): A concave curvature formed at the level of distal carpal row. The keystone (apex of the arch that bears maximum force) of this arch is the capitate bone
- Longitudinal arch(s): a carpometacarpophalangeal arch(s) that extends from the crease of the wrist through the four digital rays. The keystone of this arch is the MCP joint
- Distal transverse (metacarpal arch): A concave curvature formed at the metacarpal heads of the index, long, ring, and small fingers. The keystone of this arch is the head of the 3rd metacarpal bone
The longitudinal and distal transverse arches of the hand are mobile, whereas the proximal transverse arch is fixed/nonmobile. The mobility of these arches further deepens the concavity of the palm to accommodate for objects of different sizes (e.g. holding a ball using one hand, Figure 1.2). Besides the skeletal framework described above, the curvature of the palm is also maintained by the functional tone of intact intrinsic muscles. Thus, conditions that result in intrinsic muscle paralysis such as ulnar nerve palsy would consequently alter the shape of the hand due to the loss of the muscular tone. Another muscle is the palmaris brevis, which is innervated by the ulnar nerve. The palmaris brevis muscle arises from the transverse carpal ligament (TCL) and palmar aponeurosis (PA)5 and inserts superficially into the dermis of the skin. Contraction of this muscle results in cupping of the palm when grasping an object or drinking using the hands.
Figure 1.2: (a) Arches of the hand. (b) Mobility of the arches of the hand allows us to handle larger objects.
Surface landmarks
Knowledge of the surface anatomy is essential in the examination of the hand and for planning surgical incisions to avoid iatrogenic injuries of deep vital structures. On the palmar aspect of the hand, one can identify the approximate location of deeper structures using the Kaplan cardinal line. Although several definitions exist, Kaplan described the cardinal line as a line drawn from the junction of the MCP joint line of the thumb at the first interdigital fold to a point 2 cm distal to the pisiform. The proximal intersection of perpendicular lines drawn from the ulnar and radial borders of the long and ring fingers with Kaplan line provide an estimated location of the important structures of the hand (Figure 1.3). There is no general consensus on the accurate location of these structures; however, the following are useful measurements to identify pertinent deep structures of the hand based on the above description:
Figure 1.3: Kaplan cardinal line and its anatomical relationship to pertinent deep structures of the hand.
- Scaphoid tubercle: Palpable at the distal wrist crease just radial to the tendon of the flexor carpi radialis (FCR) muscle
- Pisiform: Palpable at the distal wrist crease on the ulnar side at the insertion of the flexor carpi ulnaris (FCU) muscle
- Hook of hamate: Located approximately 1 cm distal and slightly radial to the pisiform bone
- Motor branch of ulnar nerve: Located midway between the pisiform and hook of hamate lying deep in the Guyon canal
- Median nerve: The median nerve lies directly under the palmaris longus (PL) muscle (when present), ulnar to the FCR tendon
- Motor recurrent branch of median nerve: the motor recurrent branch of the median nerve emerges from under the distal edge of the TCL at the thenar skin crease to supply thenar muscle mass. 1 cm distal and slightly ulnar to the scaphoid tubercle is the ridge of trapezium. The distal edge of the TCL runs along a line between the hook of hamate and ridge of trapezium
- Superficial palmar arch (SPA): located approximately 1 cm distal to the distal edge of the TCL
On the dorsum of the hand, the following locations are useful to identify the following structures (Figure 1.4):
Figure 1.4: Demonstrating the proximal carpal row, radiocarpal, ulnocarpal, and distal radioulnar joints. Additionally, Lister tubercle is marked on the dorsum of the radius.
- Lister tubercle: A bony prominence on the dorsum of the distal radius that is palpable midway between the radial styloid and the DRUJ
- Body of the scaphoid: The scaphoid and trapezium are palpable on the floor of the anatomical snuffbox, which is located between the tendons of the extensor pollicis longus (EPL) and extensor pollicis brevis (EPB) on the radial side of the distal forearm
- Other important landmarks located on the dorsum of the hand including the radiocarpal joint, the lunate bone, and the scaphoid lunate joint are shown
INTERNAL ANATOMY OF THE HAND
Palmar aponeurosis (PA, Figure 1.5)
Following dissection of the skin and fat tissue, the next layer is the PA, also known as the palmar fascia. The PA is a triangular structure formed of tough connective tissue lying in the center of the palm, and is a continuation of the deep fascia of the forearm. The triangular fascia extends from its apex at the distal wrist crease to its base at a level just distal to the distal palmar crease. On the radial and ulnar sides, the PA joins the fascial covering of the thenar and hypothenar muscles, respectively. Proximally, the fascia gives an insertion to the tendon of the PL muscle (if present).
The PA consists of three layers running in different directions. In the sagittal plane, the layers of the PA are arranged as follows, from superficial to deep:
- Superficial longitudinal fibers: The superficial fibers of the PA fan out from the PL muscle at the level of the wrist crease and continue in the fingers as the pretendinous band, the superficial transverse ligament (natatory ligament), the spiral fibers, and the lateral digital sheet. The superficial layer also attaches to the overlying skin by multiple vertical septa, thus contributing to the stability of the palmar skin
- Deep fibers: The fibers of the deep layer assume a crisscross configuration. Thick fibrous bands (paratendinous bands) extend vertically from the deep surface of the PA to the volar interosseous fascia, forming tunnels that separate flexor tendons from the neurovascular bundle on the ulnar side and lumbrical muscles on the radial side of each finger (Figure 1.6)
The PA is a protective layer over the flexor tendons, neurovascular bundles, and other vital structures of the hand, as well as a stabilizer of the palmar skin of the hand. Good knowledge of this complex anatomy, especially of the superficial layer of the PA, is critical to the understanding and treatment of patients with Dupuytren disease.
Carpal tunnel (Figure 1.7)
The carpal tunnel is a fibro-osseous tunnel that forms a passage or an inlet for many of the long flexor tendons as well as the median nerve, when crossing the wrist joint from the forearm to the hand. The tunnel has a dorsal aspect formed by the concavities of the proximal and distal carpal bones, and a palmar aspect covered by the TCL (flexor retinaculum). On the radial side, the TCL attaches to the scaphoid tubercle and trapezium and ulnar to the hook of hamate and the pisiform. The TCL keeps tendons close to the volar side of the wrist and prevents bowstringing of the flexor tendons during wrist and finger flexion.
The carpal tunnel contains 10 structures: 4 tendons of the flexor digitorum superficialis (FDS) muscle, 4 tendons of the flexor digitorum profundus (FDP) muscle, the median nerve, and 1 tendon of the flexor pollicis longus (FPL) muscle. The superficialis tendons to the long and ring fingers are in the top layer, the superficialis tendons of the little and index fingers are in the middle layer, and all of the profundi are lined up in a row in the deep layer. The FPL runs separately. As the flexor tendons emerge from the carpal tunnel on their way to the fingers, the tendons of the FDP pass through a split opening of the FDS known as the Camper chiasm (over the proximal phalanx) to insert into the base of the distal phalanx, whereas the tendons of the FDS reunite and insert onto the base of the middle phalanx of each finger. Therefore, the FDS flexes the proximal interphalangeal (PIP) and MCP joints, whereas the FDP flexes the whole finger, including the distal interphalangeal (DIP) joint and both flexors of the wrist joint. The FPL tendon runs over the palmar aspect of the thumb to insert into the base of the distal phalanx and is responsible for thumb flexion.
Superficial to the TCL passes the palmar cutaneous branch of the median nerve to provide cutaneous innervation to the central area of the palm. During carpal tunnel surgery, the palmar cutaneous branch is rarely seen; however, if encountered it is best to preserve it to avoid the development of a painful neuroma.
Guyon canal
The Guyon canal, sometimes referred to as the ulnar tunnel, is a passage where the ulnar nerve and vessels travel through as they cross 7the wrist joint from the forearm to the hand. The canal is approximately 4 cm long and is bounded by the hook of hamate on the radial border and the pisiform bone and the muscle belly of the abductor digiti minimi (ADM) on the ulnar side. The floor of the canal is formed by the TCL (flexor retinaculum); thus, the ulnar nerve and vessels cross superficially and are not part of the contents of the carpal tunnel. The roof of the canal is formed by a fascial expansion known as the volar carpal ligament as well as the pisohamate ligament. The ulnar nerve passes through the Guyon canal and split into two branches: the superficial and deep ulnar nerves. The superficial branch supplies the palmaris brevis muscle and gives off cutaneous to the palm and the digits, whereas the deep branch supplies most of the intrinsic muscles of the hand (see below).
Digital flexor sheath and pulley system
The digital flexor sheath is a closed synovial system consisting of membranous and retinacular portions. The membranous portion is made up of visceral and parietal layers that invest the FDP and FDS tendons in the distal aspect of the hand, and contains synovial fluid that provides tendon nutrition through the process of synovial diffusion. The synovial sheaths of the index, long, and ring fingers extend from the base of the distal phalanx and end at a point near the level of the neck of the metacarpal bones. In the thumb and the small finger, the synovial sheath extends into the carpal tunnel and for approximately 2.5 cm into the distal forearm (Figure 1.8). Proximal communication between the tendon sheaths of the little finger and the thumb may occur at a level of proximal wrist crease also known as the space of parona. This is clinically important, as distal infections (originating in the fingers, e.g. septic tenosynovitis) may spread down along the course of the flexor tendon sheath resulting in pain and tenderness and/or collection of pus that can be palpable at the space of parona.
The retinacular aspect of the flexor sheath consists of a series of transverse annular and cruciate pulleys (fibrous bands) that overlay the flexor tendons and synovial sheaths, and extend from the palmar surface of the MCP joint to the DIP joint. The dorsal aspect of this tunnel is formed by the deep transverse metacarpal ligament, palmar plates of MCP and interphalangeal (IP) joints, and the palmar surfaces of the proximal and middle phalanx. There are five annular pulleys (A1–A5) and three cruciate pulleys (C1–C3) in the index to small fingers. However, in the thumb there are two annular pulleys (A1 and A2) and one oblique pulley. The main function of these retinacular pulleys is to prevent the forward displacement (bowstringing) of flexor tendons during fingers flexion. Keeping tendons close to the volar surface of the fingers concentrates the force of the flexor tendons during finger flexion, thus optimizing flexion movement and enhancing handgrip. Appreciation of the anatomy and biomechanics of the finger pulley system is important during flexor tendons repair and reconstruction procedures. The pulley system of the fingers and vinacular blood supply of the flexor tendons are depicted in Figure 1.9a and b.
Figure 1.9: (a) Annular and cruciate retinacular pulley system. (b) Vinacular blood supply of flexor tendons. FDS, flexor digitorum superficialis; FDP, flexor digitorum profundus; VBP, vinculum breve profundus; VBS, vinculum breve superficial; VLP, vinculum longus profundus; VLS, vinculum longus superficial.
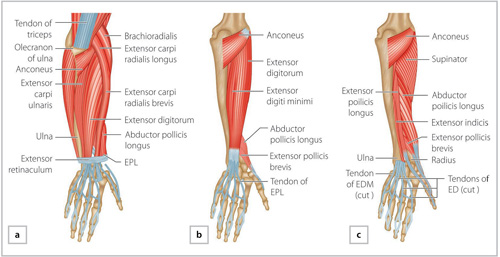
Extensor tendons
On the dorsum of the hand, the extensor retinaculum, also known as the dorsal carpal ligament, keeps the extensor tendons in close proximity with the dorsum of the wrist joint and prevents tendon bowstringing during wrist extension. The extensor retinaculum is a fascial condensation that is analogous and continuous with the TCL, and extends obliquely from the radial side of the distal radius to insert into the sheath of the FCU, the pisiform, the pisometacarpal ligament, and the base of the 5th metacarpal on the ulnar side of the wrist. The space between the retinaculum and the wrist joint is divided by five fibrous septa, creating six dorsal compartments (5 fibro-osseous and 1 fibrous tunnel, fifth compartment,Figure 1.10). This is the only area on the dorsum of the hand where the extensor tendons are covered with a synovial sheath, and thus they are prone to inflammatory synovitis due to inflammatory conditions such as rheumatoid arthritis, which may result in dorsal swelling of the wrist and spontaneous tendon rupture. The compartments of the extensor retinaculum (Figure 1.11), as well as the associated pathologic conditions of tendons within each compartment, are summarized in Table 1.1.
Figure 1.11: Compartments of the extensor retinaculum. APL, abductor pollicis longus; EPB, extensor pollicis brevis; ECRL, extensor carpi radialis longus; EPL, extensor pollicis longus; EDC, extensor digitorum communis; EIP, extensor indicis proprius; EDM, extensor digiti minimi; ECU, extensor carpi ulnaris.
8Upon emergence from the extensor retinaculum, the extensor tendons diverge to their respective fingers. Studies have found several variations in the anatomical arrangement of extensor tendons over the dorsum of the hand. Nevertheless, the most common pattern of extensor tendons on the dorsum of the hand is as follows: a single tendon of the extensor digitorum communis (EDC) to the index and long fingers, a double EDC tendon to the ring finger (a slip of ring finger tendon often powers the little finger), and an absent EDC tendon to the little finger. Additionally, a single extensor indicis proprius (EIP) tendon that lies ulnar and deep to the EDC of the index finger and a double extensor digiti minimi/quinti (EDM/EDQ) tendon that has a double insertion on the small finger. Because the index and the small finger are powered by additional (EIP and EDM) tendons, these two fingers can be extended independently from the other fingers. For example, pointing toward an object using the index finger while the rest of the fingers are in flexion. This posture demonstrates an extension of the index finger by the EIP tendon only. Even so, the EDC is the main extensor of the index to small finger. At a level near the MCP joints, the tendons of the extensor communis are joined by fibrous interconnections called tendon juncturae tendinum (Figure 1.10). 9It is because of these fibrous interconnections the long and especially the ring fingers have limited independent extension. However, the role of these connections becomes evident when an extensor tendon is completely divided proximal to the level of the juncturae. Despite a complete division of a tendon, the neighboring extensor tendon can achieve extension of the MCP joint that corresponds to the divided tendon, by powering the distal end of the severed tendon via the juncturae.
Perhaps the most complicated part of the extensor tendon anatomy is the composition of the extensor mechanism of the finger (Figure 1.12). On the dorsum of the proximal phalanx, the EDC trifurcates into a central tendon and two lateral slips. The central tendon becomes the central slip and inserts onto the base of the middle phalanx, while the two lateral slips join the lateral bands of the intrinsic muscles (interossei and lumbricals) to become the conjoined lateral bands on the radial and ulnar sides of the fingers, respectively. The conjoined lateral bands then unite to form a terminal tendon that inserts on the dorsum of the distal phalanx of each finger. At the MCP joints, the extensor tendons are encircled by the sagittal bands, which centralize the tendons over the dorsum of MCP joints. The sagittal bands arise from the palmar plate and span both sides of the MCP joint to insert with oblique and transverse fibers into the joint’s collateral ligaments and the extensor tendons. When the central extensor tendon contracts, it moves proximally and lifts up the proximal phalanx through the insertion of the sagittal bands onto the palmar plate of the MCP joint (Figure 1.13). Along this extensive network of tendons, there are three ligaments on the dorsum of the fingers that interconnect components of the extensor mechanism, and each serves a specific function:
Figure 1.12: Anatomy of the extensor tendon over the dorsum of the fingers and associated ligaments.
- Triangular ligament: A ligament that holds the lateral bands together on the dorsum of the finger and prevents their volar migration
- Transverse retinacular ligament: Arises from the flexor tendon sheath and spans over the sides of the finger to insert on the edge of the lateral bands. The transverse retinacular ligament prevents dorsal subluxation of the lateral bands during PIP joint extension. Dorsal subluxation of the lateral bands may lead to a finger deformity known as swan-neck deformity (discussed in Chapter 25)
- Oblique retinacular ligament (ORL): Arises from the flexor tendon sheath at the level of the PIP joint, spirals dorsally, and inserts distally with the terminal tendon on the dorsum of the distal phalanx. Because of its spiral structure as well as its course from the palmar to dorsal side of the finger, the ORL synchronizes the movement between the PIP and DIP joints so that the joints of the fingers flex and extend seamlessly. When the PIP joint extends, the ORL tightens to extend the DIP joint, and when the PIP joint is flexed, the ORL relaxes to allow for the simultaneous flexion of the DIP joint. Detailed illustrations demonstrating the anatomy of the tendons and ligaments over the dorsum of the hand and fingers are depicted in Figures 1.10 and 1.12
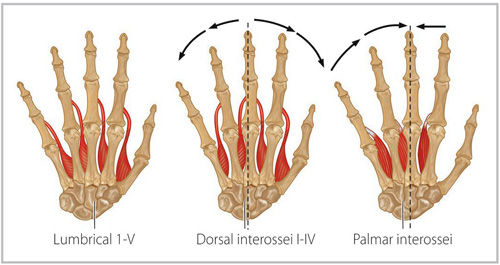
Intrinsic muscles (Figures 1.14 and 1.15)
These muscles are known as the intrinsic muscles of the hand because they originate and insert within the hand. These include the following groups of muscles:
Muscles supplied by the motor branch of the median nerve
- Thenar muscles (abductor pollicis brevis/APB, flexor pollicis brevis/FPB, and opponens pollicis)
- Radial 2 lumbricals
Muscles supplied by the motor branch (deep branch) of the ulnar nerve
- Interosseous muscles 7 (4 dorsal and 3 palmar)
- Ulnar 2 lumbricals
- Hypothenar muscles (ADM, flexor digiti minimi/FDM, and opponens digiti minimi)
- Adductor pollicis muscle
10The interosseous muscles arise from the shafts of adjacent metacarpals and insert by crossing deep to the sagittal bands into the extensor expansion of the extensor tendons and the base of the proximal phalanx of the index to the small finger, and contribute to the formation of the lateral bands with the lumbricals. As the interosseous muscles pass olar to the axis of rotation of the MCP joint, they flex the MCP joint and extend the IP joints. Additionally, the dorsal interossei abducts the fingers (DAB) whereas the palmar interossei adducts the fingers (PAD). The abduction of the little finger is executed by the abductor digiti minimi.
The lumbricals arise from the FDP tendons in the palm and insert into the radial lateral band of the extensor expansion of the index to small fingers by passing deep to the deep transverse metacarpal ligament. The lumbrical muscles are weak flexors of the MCP joints; however, as the lumbricals arise from the flexor tendons and insert into the extensor tendons, they have a unique function of coordinating the fine flexion extension movement of the fingers.
The delicate balance between the intrinsic and extrinsic muscles of the hand may be disrupted by pathologic conditions leading to the development of various deformities. For example, paralysis of the intrinsic muscles as a result of ulnar nerve palsy may lead to varying degrees of finger clawing, depending on the level of nerve injury (i.e. high vs. low ulnar nerve palsy). Finger clawing (aka. intrinsic minus deformity) is characterized by hyperextension of the MCP joint and flexion of the IP joints. This deformity is a result of weakness of intrinsic muscle function, which subsequently results in an unopposed extension of the MCP joints by the long extensors and flexion of the IP joints by the long flexors. In contrast, intrinsic muscle tightness/contracture, which occurs with conditions such as rheumatoid arthritis, is often associated with intrinsic plus deformity, characterized by flexion of the MCP joints and extension of the IP joints (see chapter on Stiff Digit for more details).
Skeletal framework of the hand
The hand and wrist consist of several articular surfaces connecting 27 bones that are stabilized by the normal joint architecture, intact restraining ligaments, and a complete balance of the musculotendinous system of the extrinsic and intrinsic muscles. Alteration to any of these structures can compromise hand function.
The metacarpophalangeal joint (MCP joint, Figure 1.16a and b )
Figure 1.16: (a) metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints in extension. (b) MCP, PIP, and DIP joints in flexion.
The MCP joint is formed by the articular surfaces of the metacarpal head and the base of the proximal phalanx. The MCP joint is a condyloid joint that allows movement in two planes (flexion/extension, abduction/adduction). A surrounding capsule, collateral ligaments, accessory collateral ligaments, and a palmar plate stabilize the joint. The collateral ligaments arise from the dorsum and sides of the metacarpal heads, and run downward and forward to insert on the palmar aspect of the base of the proximal phalanx and joint’s palmar plate. Because the metacarpal head has an asymmetric configuration of ‘volar flaring’, this creates a Cam effect where collateral ligaments are tightened by joint flexion and loosened by joint extension. The Cam effect is best described as a widening of the interarticular space between the metacarpal head and the base of the proximal phalanx due to the above-described asymmetry that exerts tension on the collateral ligaments during joint flexion.
The proximal interphalangeal joint (PIP joint, Figure 1.16a and b)
The PIP joint is formed by the articular surfaces between the proximal and middle phalanges. The PIP joint is a hinge joint that allows flexion and extension only. The joint can be described as a box shape surrounded by a joint’s capsule that is adherent to extensor tendon dorsally, and the palmar plate and the check-rein ligaments on the palmar side. The check-rein ligaments are volar extensions arising proximally from the palmar plate of the PIP joint and insert onto the palmar surface of the proximal phalanx. As their name implies, the check-rein ligaments together with the palmar plate keeps the PIP joint in ‘check’ and prevents joint hyperextension. Laterally, the joint is supported by collateral and accessory collateral ligaments as well as the fibers of the oblique retinacular ligament of Landsmeer (ORL).
The distal interphalangeal joint (DIP joint, Figure 1.16a and b)
The DIP joint is formed by the articular surfaces between the middle and distal phalanges. The DIP joint is a hinge joint that allows flexion and extension, and the joint is surrounded by a joint’s capsule. Laterally, the joint is supported by collateral and accessory collateral ligaments, whereas on the palmar side the joint capsule attaches to the palmar plate.
The wrist joint
11The wrist joint connects the forearm to the hand and is a transitional anatomical and functional region that allows the hand a great freedom of mobility, from a relatively limited pronosupination movement at the distal forearm to almost any degree of movement, including wrist flexion, extension, radial deviation, ulnar deviation, and circumduction.
The wrist is fairly a complex geometrical structure that is composed of eight carpal bones articulating among each other and also with the distal radius and ulna proximally and distally with the metacarpal bones. The carpal bones are arranged into two rows: the proximal carpal row that consists of the scaphoid, lunate, triquetrum, and pisiform bones and a distal row that is formed by the trapezium, trapezoid, capitate and hamate bones. Between the two carpal rows is the midcarpal joint that permits flexion and extension movement. The articular surface of the distal radius has two bony depressions: the scaphoid fossa and lunate fossa that accommodate the scaphoid and lunate bones, respectively and are known as the radiocarpal joint. On the ulnar aspect of the distal radius, the sigmoid notch articulates with the distal ulna head to form the DRUJ. The DRUJ permits pronosupination of the forearm. There is a discrepancy between the circumference of the sigmoid notch of the radius and that of the ulnar head. This mismatch results in joint incongruity, subsequently resulting in translation and rotation of the ulna during pronation and supination. The ulna translates dorsally in pronation and volarly in supination. However, the DRUJ is stabilized by several structures often referred to as the static and dynamic constraints. The static constraints include the triangular fibrocartilage complex (TFCC), the dorsal radioulnar ligament and volar radioulnar ligament, the ulnar collateral ligament, and the joint capsule. The dynamic muscle stabilizers include the extensor carpi ulnaris (ECU) tendon and the pronator quadratus (PQ) muscle.
At the ulnocarpal joint, the distal ulna is covered by triangular fibrocartilage, which is together with the ulnocarpal ligaments and the sheath of the ECU, forms theTFCC. The TFCC arises from the lunate and distal end of radius and inserts into the base of the ulnar styloid process. The peripheral part of the TFCC is well vascularized, whereas the center of the TFCC is an avascular load bearing part that articulates with the distal ulna and triquetrum. The intricate assembly of the carpal bones is supported by a number of volar and dorsal ligaments. The ligaments of the wrist are divided into extrinsic and intrinsic ligaments as described by Taleisnik. Extrinsic ligaments connect the distal radius and ulna to the carpal bones, and intrinsic ligaments connect carpal bones together, as they have their origins and insertions within the carpal bones.
Blood supply of the hand
An abundant network of arteries arising from the radial and ulnar arteries (branches of the brachial artery) supplies the hand. The radial artery enters the hand passing along the floor of the anatomical snuffbox, then pierces the dorsum of the first webspace (between the two heads of the first dorsal interosseous muscle) to enter the palm of the hand after giving off the princeps pollicis artery to the thumb. The anastomosis between the radial artery and the deep branch of the ulnar artery forms the deep palmar arch (predominately from the radial artery), which lies at the base of the metacarpals. Branches of the deep palmar arch include the radialis indicis artery, palmar metacarpal arteries, perforating arteries to the dorsal system, and recurrent branches to the palmar carpal arch. The SPA (see surface marking in Figure 1.3) lies just beneath the PA and is prone to injury due to its relative superficial location in the hand. The SPA (predominantly from the ulnar artery) is formed by the anastomosis between the ulnar artery and the superficial palmar branch of the radial artery. The major branches of the SPA are the common digital arteries (Figure 1.17).
On the dorsum of the hand, the posterior interosseous artery and the perforating branches of the anterior interosseous artery (branches of the common interosseous artery that arise from the ulnar artery at the level of the radial tuberosity proximal in the forearm) form the dorsal carpal arch. The 2nd, 3rd, 4th, and 5th dorsal metacarpal arteries branch from the dorsal carpal arch (Figure 1.18) and are the source of the blood supply of many of the local flaps performed on the dorsum of the hand (dorsal metacarpal artery system). The dorsal metacarpal arteries bifurcate to give off the dorsal digital arteries, which communicate with the palmar digital arteries in the fingers.
Distal in the palm, the common digital arteries bifurcate into the proper palmar digital arteries. The proper digital arteries run dorsal to their corresponding radial and ulnar digital nerves, respectively (Figure 1.19) and anastomose by perforating branches with the dorsal digital arteries. The venous drainage of the hand corresponds to these arteries; however, a superficial network of superficial veins is obvious on the dorsum of the hand that confluences to form the cephalic and basilic veins on the radial and ulnar sides of the dorsum of the hand, respectively. Finally, one must realize that there are large anatomical variations in the blood supply and venous drainage of the hand.
Nerve supply of the hand
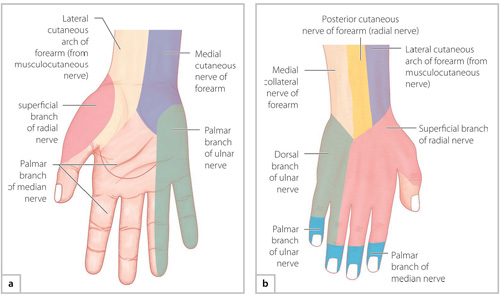
12The upper limb and the hand are innervated by branches arising from the roots, trunks, and divisions of the brachial plexus. In this section, we will discuss the sensory and motor innervation of three nerves: the radial, median, and ulnar nerves (Figure 1.20):
Figure 1.19: Cross section of the finger. Note that the digital arteries lie immediately dorsal to the digital nerves.
The radial nerve arises from the posterior cord (C5-T1) of the brachial plexus. In the arm, the radial nerve runs in the spiral groove of the humerus and supplies the triceps and anconeus muscles. The radial nerve then pierces the lateral intermuscular septum of the arm to run in the anterior compartment of the arm. The radial nerve enters the forearm anterior to the lateral epicondyle of the humerus and divides into two branches: a deep branch called the posterior interosseous nerve (PIN) that is a motor branch and supplies most of the extensors of the forearm below the elbow and a superficial sensory branch. The superficial radial nerve is a sensory branch and provides cutaneous innervation over the anatomical snuffbox and the 1st dorsal webspace of the hand (Figure 1.21a and b).
The median nerve is formed by contributions of the medial and lateral cords of the brachial plexus (C6-T1). The median nerve runs in the anterior compartment of the arm and through the cubital fossa (a triangular space on the volar side of the elbow joint) medial to the brachial artery. The median nerve enters the forearm by passing between the two heads of the pronator teres (PT) muscle (see anatomy of the forearm below). In the forearm, the median nerve gives off two branches: the anterior interosseous nerve (a motor branch) and a sensory palmar cutaneous branch. The median nerve then continues its course and passes through the carpal tunnel to supply the muscles and skin of the hand. The sensory distribution of the median nerve in the hand involves the palmar side of the radial three and a half fingers (thumb, index, long fingers, and radial half of the ring finger) as well as the skin over the dorsum of the distal phalanges, including the nail bed.
The ulnar nerve arises from the medial cord of the brachial plexus (C7-T1). The ulnar nerve initially runs in the anterior compartment before piercing the medial intermuscular septum to enter the posterior compartment of the arm. The ulnar nerve then enters the forearm behind the medial epicondyle by passing through the cubital tunnel (potential site of nerve compression). In the forearm, the ulnar nerve runs underneath the FCU alongside the ulnar artery. The ulnar nerve gives motor innervation to the medial half of the FDP and the FCU muscles. Along its course, the nerve is accompanied by the ulnar artery and both enter the hand by passing through the Guyon canal. Before entering the hand, the ulnar nerve gives off a dorsal and a palmar cutaneous branch that supplies the skin of the ulnar one and a half fingers (small and ulnar half of the ring finger). In the hand, the ulnar nerve supplies the intrinsic muscles of the hand as mentioned previously.
The nerves of the upper limb travel a long distance from the upper arm to the hand, thus they are prone to mechanical compression at several anatomic locations that leads to several clinical sequelae that are discussed in detail in later chapters of this book.
ANATOMY OF THE FOREARM
The forearm extends from the elbow joint proximally to the wrist joint distally. The skeletal framework of the forearm consists of two bones: the radius and the ulna. The two bones are joined together by a fascial condensation called the interosseous membrane, sometimes referred to as the interosseous ligament, and articulate at the proximal and DRUJs along the longitudinal axis. The muscles of the forearm are arranged into two groups on the volar and dorsal sides of the forearm and are surrounded by a tight investing fascia (antebrachial fascia) that gives off deep intermuscular septa that enclose the muscles of the extensor compartment and surround the flexor compartment. Thus, the muscles of the forearm are confined within a tight fascial space, and are therefore prone to the development of compartment syndrome due to a dramatic rise of the intracompartmental pressure following trauma or a reperfusion injury.
Figure 1.21: (a) Distribution of sensory innervation of the palm. (b) Distribution of sensory innervation on the dorsum of the hand.
On the radial border of the forearm lies a long muscle known as the brachioradialis muscle, which arises from the lateral supracondylar ridge of the humerus and inserts into the lateral side of the distal radius. The brachioradialis is the main flexor of the elbow joint and overlays the radial side of both the dorsal/extensor and volar/flexor compartments of the forearm. The muscle belly of the brachioradialis is noticeable when the elbow is in flexion against resistance while the forearm is in a neutral position.
On the dorsum of the forearm, we can find that the muscle bellies of the extensor compartment are arranged in layers and parallel to each other, this is also true when we will look later at the muscles of the flexor compartment of the forearm. The muscles of the superficial layer of the extensor forearm arise from a common extensor origin, which is the lateral epicondyle of the humerus. From radial to ulnar, the muscles are arranged as follows: extensor carpi radialis longus (ECRL), extensor carpi radialis brevis (ECRB), EDC, EDM/EDQ, and the ECU. With the exception of the supinator muscle, which inserts proximally on the dorsum of the forearm, the extensor muscles of the forearm pass underneath the extensor retinaculum as described previously to insert into the hand. A clinical caveat: most of the muscles of the extensor compartment of the forearm are supplied by the PIN except two muscles, the ECRL and brachioradialis, which are supplied by the radial nerve at a level above the elbow joint. Thus, with radial nerve palsy at the forearm, such as in PIN syndrome, the synergistic action of the extensor muscles is lost and wrist extension is achieved mainly by the ECRL, which results in extension and radial deviation of the wrist joint. A clinical distinction between high or low radial nerve palsy can 14be made based on the knowledge of this anatomy. In high radial nerve palsy, there is a wrist and finger drop deformity due to the paralysis of all of the muscles of the extensor compartment, whereas in low radial nerve palsy (i.e. below the elbow joint such as in PIN syndrome) there is only a finger drop deformity as the ECRL muscle is spared.
In the next layer of the extensor compartment of the forearm, the following muscles lie from radial to ulnar; the APL, EPB, EPL, and the EIP. The APL, EPB, and the EPL form the medial and lateral borders of the anatomical snuffbox, respectively, which is located over the radial side of the distal radius and carpal bones. The EPL tendon courses at an acute angle around a bony prominence on the dorsum of distal radius called the Lister tubercle (see surface marking above) to reach the dorsum of the thumb. This sharp angulation around the bony protuberance creates tension on the EPL tendon and may precipitate tendon attrition rupture. The layers of the extensor muscles of the forearm are shown in Figure 1.22.
Figure 1.22: Muscles of the extensor compartment of the forearm: (a) superficial, (b) middle, and (c) deep layers. ED, extensor digitorum; EDM, extensor digiti minimi; EPL, extensor pollicis longus.
On the flexor side of the forearm, the muscles are arranged from superficial to deep into three layers, with the FCR, the PL, and the FCU being the most superficial layer of the volar forearm. More proximal on the volar side of the forearm is the PT muscle. The PT, FCR, PL, FCU, and FDS all have a common flexor origin arising from the medial epicondyle of the humerus. The next layer is the FDS muscle belly as well as the FPL muscle. Underneath the FDS muscle lies the median nerve after emerging from between the two heads of the PT muscle. The median nerve (and its motor branch, AIN) supplies all of the muscles of the forearm except the FCU and medial part of the FDP (ring and small fingers) that is innervated by the ulnar nerve. In the distal forearm, the median nerve continues as described previously deep to the PL and ulnar to the tendon of the FCR to enter the carpal tunnel after giving off the palmar cutaneous branch of the palm approximately 5 cm proximal to the distal wrist crease. The ulnar nerve and ulnar artery lie deep and ulnar to the FCU tendon and superficial to the muscle belly of the FDP to enter the hand above the TCL by passing through the Guyon canal. In the deepest layer of the forearm, tendons of the FDP and the PQ muscle are found. The PQ muscle, together with the PT, pronates the forearm (Figure 1.23).
Figure 1.23: Muscles of the flexor compartment of the forearm: (a) superficial, (b) middle, and (c) deep layers.
ANATOMY OF THE ARM
Last but not the least is the anatomy of the upper arm. On studying the anatomy of the upper extremity, one must appreciate that the whole limb work as a functional unit and deformities of proximal joints would affect the distal ones. Similar to the other parts, the upper arm is divided into an anterior and a posterior compartment by an intermuscular septum. The anterior compartment of the arm is the flexor compartment, whereas the posterior compartment is the extensor compartment. In addition to the nerves and vessels described in the previous sections, the anterior compartment of the arm includes the biceps brachii muscle, the brachialis, and the coracobrachialis that are all supplied by the musculocutaneous nerve (MCN). The MCN arises from the lateral cord of the brachial plexus, and as the name implies serves as a motor nerve in the arm and continues as a sensory nerve to supply the lateral aspect of the forearm. The biceps muscle is the main supinator of the forearm and together with the brachialis and brachioradialis it flexes the elbow joint. On the posterior compartment are the three heads of the triceps muscle and a small muscle called the anconeus, both of which are supplied by the radial nerve. The triceps is the main extensor of the elbow joint with a less than modest contribution from the anconeus muscle. The muscles, nerves, and vessels of each compartment are demonstrated by the cross-sectional anatomy shown in Figure 1.24.15
SUGGESTED READING
- Doyle JR. Anatomy of the finger flexor tendon sheath and pulley system. J Hand Surg Am 1988; 13: 473–484. A cadaveric study performed on 61 fingers by Dr Doyle who was the first to describe and recognize the anatomical and functional importance of the pulley system of flexor tendons. The outcome of this study has reinforced our understanding of the anatomy of the pulley system as explained in this chapter and addressed other issues such as correct terminology of flexor tendons pulleys and their anatomic variation in the human hand.
- Frank H. Netter. Atlas of human anatomy. Chapter 7 , Upper Limb p. 293–346. A comprehensive atlas that includes detailed illustrations and descriptions of the anatomy of the upper limb.
- Kareklas K, Nettle D, Smulders TV. Water-induced finger wrinkles improve handling of wet objects. Biol Lett 2013; 9:20120999. This study sheds light on the role of papillary ridges of the palmar skin. The study compares the transit time of handling wet objects between two groups of healthy volunteers. Results show that wrinkled damp skin has a better ability to grasp wet objects than dry nonwrinkled palmar skin. The outcome of this study provides a new perspective on the understanding of the role of papillary skin ridges during prehension.
- Palmer AK, Skahen JR, Werner FW, Glisson RR. The extensor retinaculum of the wrist: an anatomical and biomechanical study. J Hand Surg Br 1985; 10: 11–16. An anatomic and biomechanical study performed on 65 cadaveric specimens to evaluate the anatomic variation and biomechanics of the extensor retinaculum.
- Sangole AP, Levin MF. Arches of the hand in reach to grasp. J Biomech 2008; 41: 829–837. A study investigating the biomechanics and kinematics of the arches of the hand during grasping motion. This study provides a clear anatomical description of the arches of the hand and thoroughly investigates the influence of motion on altering arches and the shape of the hand.
- Young CM, Rayan GM. The sagittal band: anatomic and biomechanical study. J Hand Surg Am 2000; 25: 1107–1113. A cadaveric study performed on 12 specimens to evaluate extensor tendon instability anatomy associated with the mechanical disruption of the sagittal bands.