Questions: MCQs
Questions: SBAs
Answers
Answer each stem ‘True’ or ‘False’.
1. The following form part of the superior anatomical boundary (pelvic inlet) of the true pelvis:
- Linea alba
- Sacroiliac joint
- Ischial fossa
- Iliac crest
- Iliopectineal line
2. The diameters of the pelvis:
- The anatomical anteroposterior diameter (true conjugate) is approximately 11 cm
- The obstetric conjugate is larger than the true conjugate
- The anatomical transverse diameter forms the largest pelvic diameter (approximately 13 cm)
- The obstetric transverse diameter bisects the true conjugate
- The external conjugate has no true obstetric importance
3. The pudendal nerve:
- Arises from the posterior rami of S2, S3 and S4
- Supplies the levator ani
- Leaves the pelvis through the greater sciatic foramen
- Supplies the clitoris
- Crosses over the ischial tuberosity, lateral to the internal pudendal artery
4. Pelvic nerve supply:
- Pelvic splanchnic nerves are derived from the dorsal primary rami of spinal nerves S2–S4
- The inferior rectal nerve is a branch of the pudendal nerve
- The rectal plexus is derived from the anterior part of the inferior hypogastric plexus
- The external anal sphincter is supplied by the inferior rectal nerve
- The anterior labial nerve is a branch of the ilioinguinal nerve
- The left ovarian vein drains directly into the inferior vena cava
- The internal pudendal vein passes through the pudendal canal
- The uterine venous plexus connects the ovarian vein and the vaginal venous plexus
- The internal pudendal vein drains into the great saphenous vein
- The rectal venous plexus is a site of portocaval anastomosis
6. With regard to innervation of the lower limb:
- The tibial nerve is derived from L4–S1
- Damage to the common peroneal nerve typically results in foot drop
- The femoral nerve divides into an anterior and posterior branch before passing beneath the inguinal ligament
- The femoral nerve is derived from the posterior division of L2–L4
- The sciatic nerve is derived from L4–S3
7. The anal canal:
- The upper half is lined with cuboidal epithelium
- The lower half is lined with non-keratinised stratified squamous epithelium
- The fibres of ischiococcygeus form part of the internal anal sphincter
- The dentate line lies at the border of the upper one-third and lower two-thirds of the anal canal
- Hilton's line indicates the junction between keratinised and non-keratinised stratified squamous epithelium
8. Rectus sheath:
- The rectus sheath is made up of the aponeuroses of transversus abdominis and internal oblique
- Below the arcuate line, the posterior rectus abdominis is separated from the peritoneum by transversalis fascia and connective tissue
- Pyramidalis is external to the rectus sheath
- The rectus sheath contains the ventral rami of lower eight thoracic nerves
- Contains an anastomosis between the internal thoracic artery and superior epigastric artery
9. The pudendal canal:
- Contains the pudendal nerve, artery and vein
- The pudendal nerve is not located in the pudendal canal
- Runs superiorly to the sacrotuberous ligament
- Runs laterally to obturator internus
- Passes medial to the ischial spines
10. The bladder:
- The pudendal nerve plays no part in innervation of the bladder
- The sympathetic nervous system has no motor function in the bladder
- The main blood supply to the bladder is from the branches of the posterior trunk of the internal iliac artery
- It is derived embryologically from the mesonephric duct
11. The human testis:
- Has an average length of 2– 3 cm
- Descends through the inguinal ring after birth to reside in the scrotum
- Are surrounded by the tunica vaginalis
- The tunica albuginea is covered by tunica vaginalis
- The hydatid of Morgagni is a remnant of the müllerian duct
12. The ureters:
- Are retroperitoneal structures
- Are 35 cm long
- Cross in front of the uterine arteries
- Originate embryonically from the ureteric buds
- Insert into the bladder posteromedially
13. The vagina:
- Is lined with striated squamous epithelium
- Has an acidic pH
- Has secretory glands which provide lubrication
- Is approximately 7 cm long anteriorly
- Is covered anteriorly by visceral peritoneum
14. The vagina:
- Has its venous drainage supplied by the external iliac vein
- Is derived from the embryonic mesonephros
- Originates from mesoderm
- Has a shorter anterior wall than posterior wall
- Has superiorly supplied by the uterine artery
15. Superiorly, the vagina:
- Receives its arterial blood supply from the uterine arteries
- Receives its lymphatic drainage via the inguinal lymph nodes
- Receives its venous supply from the uterine vein
- Receives somatic innervation via the pudendal nerve
- Is lined with secretory columnar epithelium
16. The uterus:
- In non-gravid state weighs approximately 90 g
- Consists of the three muscle layers: the perimetrium, the myometrium and the endometrium
- Is related anteriorly to the pouch of Douglas
- Is 10 cm long
- Receives its main arterial supply from the uterine arteries
17. The female urethra:
- Is directly related to the anterior vaginal wall
- In its upper two-thirds, it has the same blood supply as the bladder
- Is innervated by the pudendal nerve
- Is lined with transitional epithelium at its origin proximal to the bladder
18. The average female pelvis:
- Is gynaecoid in shape
- Has a round obturator foramen
- Has a heart-shaped inlet
- Has a wide pubic arch
- Has a subpubic angle of 60°
19. The adrenal glands:
- Sit superiorly to the kidneys
- The medulla originates from the embryonic endoderm
- The cortex develops from coelomic mesothelium
- Lymphatic drainage is from the lumbar lymph nodes
- The right adrenal gland sits anterior to the diaphragm
20. The adrenal glands:
- The left adrenal gland is triangular-shaped
- The adrenal medulla consists of chromaffin cells
- The right adrenal vein drains into the right renal vein
- Have part of their nerve supply provided by the thoracic splanchnic nerves
- The left adrenal gland is in contact with the spleen
21. The inguinal canal:
- Part of the external oblique forms the anterior wall of the canal
- Contains the ilioinguinal nerve
- The internal oblique originates from the lateral third of the inguinal ligament
- Contains the male spermatic cord
- The superficial inguinal ring lies superiorly and lateral to the pubic tubercle
22. The femoral triangle:
- The inguinal ligament provides the superior boundary
- The medial border is formed from the gracilis
- The lateral border is formed from both sartorius and iliacus
- The femoral artery lies medial to the femoral vein
- The femoral nerve lies lateral to the femoral artery
23. The femoral region:
- The femoral ring is bounded medially by the lacunar ligament
- The femoral artery is a continuation of the internal iliac artery
- The femoral septum is covered by parietal peritoneum
- The femoral canal often contain Cloquet's node
- The femoral sheath covers the femoral nerve
- Iliacus is innervated by the femoral nerve
- Iliopsoas acts to extend the thigh
- Arterial supply is predominantly from the abdominal aorta
- Quadratus lumborum is innervated by the subcostal nerve
- Psoas minor is absent in females
For each question, select the single best answer from the five options listed.
25. Which of the following structures does not pass through the diaphragm?
- Azygos vein
- Cisterna chyli
- Inferior vena cava
- Oesophagus
- Thoracic duct
26. Which vessel provides blood supply to the intestine from the splenic flexure of the transverse colon to the rectum?
- Inferior mesenteric artery
- Median sacral artery
- Middle colic artery
- Rectal artery
- Superior mesenteric artery
27. A 21-year-old woman undergoes a laparoscopic ovarian cystectomy to remove a dermoid cyst. Three days after the operation, she presents to the emergency department feeling unwell and her haemoglobin level is found to be 6 g/dL. Damage to a blood vessel is suspected from the laparoscopic procedure.
Which vessel crosses the common and external iliac artery in the infundibulopelvic fold?
- Femoral artery
- Inferior mesenteric artery
- Median sacral artery
- Ovarian artery
- Renal artery
28. What is the nerve root of the ilioinguinal nerve?
- T12 and L1
- L1
- L1 and L2
- L2
- L2 and L3
29. A 27-year-old woman has a cervical smear result which shows ‘borderline’ changes.
Which cells line the ectocervix?
- Ciliated cells
- Columnar epithelium
- Cuboidal epithelium
- Stratified squamous epithelium
30. A 32-year-old woman undergoes an emergency caesarean section for failure to progress at 9 cm cervical dilatation.
Which of the following correctly describes the pelvic shape which has an anteroposterior diameter of the inlet, greater than the transverse diameter?
- Android
- Anthropoid
- Gynaecoid
- Male
- Platypelloid
31. An 18-year-old woman attends the gynaecology clinic complaining of urinary incontinence, 3 months after suffering a third degree perineal tear during a normal vaginal delivery.
Which muscle forms the main bulk of the levator ani muscle?
- Bulbocavernosus
- Iliococcygeus
- Ischiococcygeus
- Pubococcygeus
- Urogenital diaphragm
32. Which of the following organs is derived from ectodermal neural crest cells?
- Adrenal gland inner medulla
- Adrenal gland outer cortex
- Liver
- Pancreas
- Spleen
33. A 63-year-old woman complains of numbness over her thigh following a radical hysterectomy for stage IV endometrial carcinoma.
What is the nerve root of the obturator nerve?
- Anterior division L1–L4
- Anterior division L2–L4
- Anterior division L3–L4
- Posterior division L2–L4
- Posterior division L3–L4
34. An 82-year-old woman attends her general practitioner's surgery complaining of a painful lump in the groin.
Which of the following does not form a boundary of the femoral triangle?
35. A 32-year-old woman complains of pain in the right buttock. She is 36 weeks pregnant and has a history of chronic back pain.
Which nerve supplies the gluteus maximus muscle?
- Inferior gluteal
- Internal obturator
- Internal obturator (lateral cutaneous nerve of the thigh)
- Sciatic
- Superior gluteal
36. Following a routine elective caesarean section, the rectus sheath is being sutured.
With regards to the rectus sheath which of the following is correct?
- Arcuate line demarcates the upper limit of the posterior layer of rectus sheath
- External oblique aponeurosis forms the posterior aspect of the sheath
- Internal oblique aponeurosis always passes in front of rectus abdominis
- Scarpa's fascia is superficial to Camper's fascia and the external oblique
- Transversalis fascia lies directly below the rectus sheath
37. A 47-year-old woman undergoes a routine transabdominal hysterectomy to remove a large fibroid uterus. She is found to have a fibroid in the broad ligament and there is concern that her ureter may have been damaged due to the difficult operation.
With regards to the path of the ureter, which of the following is correct?
- In the broad ligament, both ureters pass over their respective uterine artery
- Runs lateral to the internal iliac artery
- Ovarian vessels enter the pelvis posterior to the ureters
- Upper one-third of the ureters lie in the abdomen
- Ureters cross close to the bifurcation of the common iliac vessels
38. What structure does the right ovarian vein empty into?
- Azygos vein
- Inferior vena cava
- Internal iliac vein
- Right renal vein
- Right pudendal vein
39. A 27-year-old woman has a forceps delivery under regional block. She suffers multiple second degree tears to the lateral vaginal wall.
- Dorsal nerve of the clitoris
- Inferior hypogastric plexus
- Inferior rectal nerve
- Obturator nerve
- Pudendal nerve
40. Which artery supplies the structures derived from the foregut of the embryo?
- Coeliac trunk
- Inferior mesenteric
- Middle rectal
- Renal
- Superior mesenteric
41. A 73-year-old woman undergoes a laparoscopic assisted vaginal hysterectomy and oophorectomy. There is a large bleed during the procedure and it is converted to a laparotomy.
Which of the following provides the arterial blood supply of the left ovary?
- Abdominal aorta
- External iliac artery
- Internal iliac artery
- Left ovarian artery
- Obturator artery
42. During a laparoscopic-assisted vaginal hysterectomy the surgeon accidentally damages the ovarian artery.
Regarding the left ovarian artery, which of the following is correct?
- Anastomoses with the vaginal artery
- Is a branch of the abdominal aorta
- Follows the course of the left ovarian artery
- Lies inferiorly to the inferior mesenteric artery
- Supplies both left and right ovaries
43. Which of the following arteries is a terminal branch (not paired) of the abdominal aorta?
- Gonadal
- Median sacral
- Phrenic
- Renal
- Suprarenal
44. A 32-year-old woman has an episiotomy repaired following a forceps delivery.
Which of the following does not insert into the perineal body?
45. A woman undergoes an emergency caesarean section at full dilatation following a failed trial of instrumental delivery. There is a lateral extension to the uterine excision which is bleeding.
Identify which of the following gives the correct pairing of artery and its origin.
Artery | Origin |
A Internal pudendal | Posterior division of internal iliac |
B Ovarian artery | Common Iliac |
C Testicular artery | Abdominal aorta |
D Uterine artery | Abdominal aorta |
E Uterine artery | Anterior division of the internal iliac |
46. Which of the following is not part of the bony pelvis?
- Fourth lumbar vertebrae
- Ilium
- Ischium
- Pubis
- Sacrum
47. Which of the following describes the anatomy of the inguinal region?
- The deep inguinal ring lies at the lateral two-thirds of the inguinal ligament
- The deep inguinal ring transmits the ilioinguinal nerve
- The superficial inguinal ring lies below the pubic tubercle
- The superficial inguinal ring transmits the genitofemoral nerve
- The superficial inguinal ring transmits the round ligament
48. Which of the following nerves is transmitted by the superficial inguinal ring?
- Femoral nerve
- Genitofemoral nerve
- Ilioinguinal nerve
- Peroneal nerve
- Sciatic nerve
- False
- True
- False
- False
- True
The female pelvis can be divided anatomically into two broad areas: the false pelvis and the true pelvis. The false pelvis lies above the pelvic brim and has no obstetric importance. The true pelvis lies below the pelvic brim and is related to child birth.The true pelvis comprises an inlet, outlet and cavity. The pelvic inlet (brim) has the following boundaries: sacral promontory, sacroiliac joints, alae of sacrum, iliopectineal line, upper border of superior pubic rami and upper border of pubic symphysis.- True
- False
- True
- True
- True
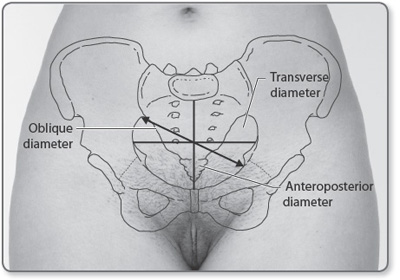
The diameters of the pelvis can be broadly categorised into transverse, anteroposterior and oblique (Figure 1.1).-
The pudendal nerve originates from the anterior (ventral) rami of S2, S3 and S4. After passing between piriformis and coccygeus, it leaves the pelvis through the greater sciatic foramen. It then crosses the ischial spine with the internal pudendal artery and re-enters the pelvis through the lesser sciatic foramen. The pudendal nerve passes medially to the internal pudendal artery (Figure 1.2).
- False
- True
- False
- True
- True
Pelvic splanchnic nerves provide parasympathetic innervation to the pelvis and are derived from the ventral primary rami of S2–S4. They control micturition, defaecation and erection. The inferior hypogastric plexus is formed from fibres of the sacral splanchnic nerves, pelvic splanchnic nerves and hypogastric nerves, and supplies the viscera of the pelvis. The rectal plexus is a posterior division of the inferior hypogastric plexus. The pudendal nerve gives off the inferior rectal nerves, before dividing into two terminal branches: the dorsal nerve of the penis/clitoris and the perineal nerve.- False
- True
- True
- False
- True
The right ovarian vein drains directly into the inferior vena cava. The left ovarian vein drains into the left renal vein. The internal pudendal vein drains into the internal iliac vein and the external pudendal vein drains into the great saphenous vein. The internal pudendal vein passes through the pudendal canal with the pudendal artery and nerve. The uterine plexuses lie in the superior angles of the uterus, between the two layers of the broad ligament. They connect the ovarian and vaginal plexuses and drain directly into the hypogastric vein. The two other sites of portocaval anastomosis are in the oesophagus and hepatic circulation.- False
- True
- False
- True
- True
Innervation of the lower limb is from the lumbosacral plexus, which is formed from the ventral rami of spinal nerves T12–S4. The sciatic nerve is a nerve of the posterior leg, derived from L4–S3 and contains fibres from anterior and posterior aspects of the lumbosacral plexus. The tibial nerve is derived from the anterior division of L4–S3 and is a branch of the sciatic nerve. The tibial nerve passes through the popliteal fossa and provides branches to the posterior aspect of the calf, as well as the knee joint. The femoral nerve arises from the dorsal division of the ventral rami of L2–L4. It passes beneath the inguinal ligament to enter the thigh, where it then divides into an anterior and posterior division. It provides innervation to the quadriceps muscle and sartorius, as well as anterior cutaneous branches.- False
- True
- False
- False
- True
The anal canal is approximately 3 cm long and lies between the anorectal junction and the anal orifice. The upper two-thirds is lined with cuboidal epithelium and is supplied by the superior rectal artery. The lower one-third is lined with 14 non- keratinised stratified squamous epithelium and is supplied by the inferior rectal artery. At the anal orifice there is a transition to keratinised stratified squamous epithelium with the presence of sweat glands and hair. Hilton's line is a white line which indicates the junction of the keratinised from the non-keratinised epithelium. The pectinate line is an important landmark embryologically which lies at the junction of the upper two-thirds and lower one-third. The fibres of pubococcygeus blend with the internal anal sphincter.- False
- True
- False
- False
- False
The rectus sheath is formed from the aponeurosis of the transversus abdominis, internal and external oblique muscles. At the lateral margin of the rectus abdominis, the internal oblique splits into an anterior and posterior layer, passing in front and behind. In front of the rectus abdominis runs the external oblique aponeurosis and the anterior layer of internal oblique. Behind the rectus runs the posterior layer of internal oblique and the transversus abdominis. The aponeuroses of each side meet at the central linea alba. Below the arcuate line, all aponeuroses pass in front of the rectus abdominis, meaning that the posterior aspect of the lower third of rectus is separated from the peritoneum by transversalis fascia and extraperitoneal connective tissue. The ventral rami of the lower seven thoracic nerves and anastomosis between the superior and inferior epigastric vessels occurs within the rectus sheath. Where pyramidalis is present, it lies within the rectus sheath anterior to rectus abdominis.- True
- False
- True
- False
- False
The pudendal canal contains the pudendal nerve, artery and vein. It runs medially to the obturator internus and is in close contact with the obturator fascia. It runs out through the greater sciatic foramen and passes laterally to the ischial spines before passing back in through the lesser sciatic foramen.- True
- True
- False
- True
- False
The urinary bladder is a muscular distensible organ that is located in the pelvis. The main blood supply to the bladder comes from the superior and inferior vesical 15 arteries, which are branches of the anterior trunk of the internal iliac artery. There is also some contribution from the uterine and vaginal arteries. The detrusor muscle is innervated from the S2–S4 nerve root, but the main contribution is from S3. The bladder is predominantly under parasympathetic control, from the inferior hypogastric plexus and the pelvic splanchnic nerves. The sympathetic nervous system only affects blood vessels in the bladder and has no motor function. The human bladder is derived in the embryo from the urogenital sinus.- False
- False
- True
- True
- True
The testes are oval glands that have an average length of 4–5 cm and a diameter of 2–3 cm. They originate embryologically in the abdomen, but descend through the inguinal canal prior to birth. Each testis is surrounded by the tunica vaginalis, which is a serous membrane, derived from the peritoneum. Underneath the tunica vaginalis is a fibrous layer that encapsulates the testis, called the tunica albuginea. It forms septa that divide each testis internally to form 200–300 lobules. It is within each of these lobules that the seminiferous tubules are located.- True
- False
- False
- True
- False
Ureters are muscular tubular structures, approximately 25 cm long, which run along the posterior abdominal wall. They are retroperitoneal through their entire course and carry urine from the kidneys to the bladder. The ureter begins at the kidney and descends from the renal pelvis along the medial border of the psoas muscle. From there, it enters the pelvis and crosses the common iliac artery. In females the ureters travel in the broad ligament and run under the uterine artery eventually inserting into the bladder posterolaterally. The openings of the ureters into the bladder are approximately 2–3 cm apart.- True
- True
- False
- True
- False
The vagina is a muscular elastic tube that extends from the cervix to the vulva. It is a tubular structure, is approximately 10 cm in length, and lies in a superior and posterior direction. The anterior wall is shorter than the posterior wall; the anterior 16 wall is 6.0–7.5 cm and the posterior wall up to 9 cm long. Vaginal lubrication is provided by the Bartholin's glands, which are situated at the 5 and 11 o'clock position near the vaginal opening. The vagina itself does not contain any glands. The epithelium of the vagina is non-keratinised stratified squamous. The overall pH of the vagina is acidic and this is caused in part from the degradation of glycogen which is stored in the vaginal mucosa.- True
- False
- True
- True
- True
The superior aspect of the vagina is supplied by the uterine artery and the middle to inferior aspect of the vagina supplied by the vaginal artery. The vaginal artery is a branch of the uterine artery. The vagina originates from the paramesonephric duct and urogenital sinus, which are mesodermal.- True
- False
- True
- False
- False
In outline, the blood and nerve supply to the vagina are:• Artery:superior – uterine arteryinferior – vaginal artery• Vein:vaginal vein• Lymph:superior – internal iliac nodesinferior – superficial inguinal nodes• Nerve:sympathetic – lumbar splanchnic plexusparasympathetic – pelvic splanchnic nerves- True
- True
- False
- False
- True
The average uterus weighs around 90 g and is approximately 7.5 cm long. This muscular organ has three layers: perimetrium, myometrium and endometrium. The major part of the uterus is the body: the fundus forms the superior portion of the uterus and sits above the openings to the fallopian tubes; and the cervix forms the base of the uterus, which partially projects into the vagina. The uterus sits between the 17bladder (anteriorly) and the rectum (posteriorly). A covering of peritoneum extends over the anterior and superiors aspects of the uterus. Anteriorly, the peritoneum also covers the bladder, the area between both organs forming the vesicouterine pouch. Posteriorly, the peritoneum reflects down over the body of the uterus, over the posterior fornix of the vagina and then over the front and lateral aspects of the rectum to form the rectouterine pouch, also known as the pouch of Douglas.- True
- False
- False
- True
- True
The female urethra has the same blood supply as the bladder in its upper third, which is the pudendal artery. The lower two-thirds has the same supply as the clitoris and anterior vaginal wall, namely the vaginal artery. The ureter nerves running to the urethra come from the pudendal nerve, with afferents going to the pelvic splanchnic nerves.- True
- False
- False
- True
- True
The typical female, gynaecoid pelvis has an oval-shaped inlet (heart-shaped in males), a large pelvic outlet in comparison to males, a wide pubic arch and a subpubic arch of around 90°; the female obturator foramens are oval. The male pelvis is thicker and generally heavier than the female pelvis. The male pelvic inlet is heart-shaped with a small outlet; the subpubic angle is around 60°. The female pelvis may have male characteristics and be described as an android pelvis. Two further types of pelvis have been described: platypelloid and anthropoid.- True
- False
- True
- True
- True
The adrenal glands are paired retroperitoneal organs, found superiorly to the kidneys. Each is approximately 3–5 cm long and weighs 5 g. The adrenal gland is divided into two different functional regions: the peripheral cortex, which makes up about 80% of the gland and the central medulla. The adrenal cortex has embryological origin from mesoderm and the adrenal medulla is derived from neural crest cells. Each adrenal 18gland has a corresponding vein. The right adrenal vein drains directly into the inferior vena cava and the left adrenal vein into the renal vein.- False
- True
- False
- True
- True
The adrenal (or suprarenal glands) sit below the diaphragm and above the kidneys. The left gland has a semi-lunar shape and sits snug proximal to the spleen, pancreas and stomach. The right triangular adrenal gland sits slightly lower than its counterpart, making contact with the liver and inferior vena cava (IVC). The outer cortex of the glands originates from mesoderm and is responsible for corticosteroid and androgen production. The inner medulla derives from neural crest cells and its chromaffin cells secrete catecholamines. The glands receive their blood supply from the suprarenal arteries (superior, middle and inferior). The left suprarenal vein drains into the left renal vein and the right suprarenal vein drains into the IVC.- True
- True
- False
- True
- True
The inguinal ligament is formed in part from the external oblique aponeurosis. The inguinal canal passes between the deep inguinal ring and the superficial inguinal ring. Contents of the inguinal canal include the round ligament, a branch of the genitofemoral nerve and the ilioinguinal nerve.- True
- False
- False
- True
- False
The boundaries of the femoral triangle are:- Superiorly: the inguinal ligament
- Laterally: sartorius muscle
- Medially: adductor longus muscle (medial border)
- Floor: adductor longus, pectineus, iliacus and psoas major
- Contents: femoral nerve, femoral vein, femoral artery, lymph nodes and fat
-
The femoral vessels pass beneath the inguinal ligament. The femoral sheath is produced from the transversalis as the vessels pass inferiorly into the thigh region. The femoral sheath has the femoral nerve laterally to it. The node of Cloquet is a lymph node that drains the clitoris and glans penis and it is located in the femoral canal, which is also situated within the femoral sheath.
- True
- False
- True
- True
- False
The major muscles of the posterior abdominal wall are the psoas major, iliacus and quadratus lumborum. The psoas major originates at the lateral aspects of all five of the lumbar vertebrae, passing downwards and laterally where it attaches to the lesser trochanter of the femur. It allows for lateral flexion of the trunk ipsilaterally. It is innervated by the ventral rami of the lumbar nerves L1–L3 (or L2–L4). Iliacus originates from the anterior superior iliac spine and also the sacrum. It joins the psoas major (also inserting at the lesser trochanter of the femur) and they form iliopsoas, which is the major flexor of the thigh. Iliacus is innervated by the femoral nerve (L2–L4). Quadratus lumborum originates at the 12th rib and as it descends becomes broader. It inserts into the aponeurosis of the iliolumbar ligament and the iliac crest. It flexes laterally and also extends the spinal column, as well as fixing the 12th rib during inspiration. Psoas minor is only present of 50% of humans, irrespective of gender.- B Cisterna chyliThe cisterna chyli is a dilated sac at the base of the thoracic duct, which forms part of the lymphatic drainage of the pelvis and abdomen. The lymph passes to the thoracic duct which, after passing through the aortic hiatus, opens into the junction of the left subclavian vein and internal jugular vein (Table 1.1).
- A Inferior mesenteric arteryThe inferior mesenteric artery arises just behind the horizontal part of duodenum (part 4). It lies retroperitoneally and crosses the left common iliac artery, medial to the ureter. The distribution of blood supply extends from the splenic flexure to the upper part of the rectum, which includes the descending colon and sigmoid colon. The distribution of blood supply of the inferior mesenteric artery corresponds to the embryonic hindgut. Branches include the left colic artery and the superior rectal artery.
- D Ovarian arteryOvarian arteries are a branch of the abdominal aorta. They run retroperitoneally, leaving the abdomen by crossing the common or external iliac arteries in the infundibulopelvic fold. They are medial to the ureter in the upper abdomen and cross obliquely anterior to the ureter in the middle to lower lumbar region, lying lateral to the ureter in the lower abdomen and pelvis. The infundibulopelvic ligament is a fold of the peritoneum, also known as the suspensory ligament of the ovary. It passes laterally from the ovary to the wall of the pelvis. See Figure 1.3 for the abdominal aorta and its branches.
-
The ilioinguinal nerve arises from the L1 nerve root along with the larger iliohypogastric nerve. It travels obliquely across the quadratus lumborum and perforates the transversus abdominis near the anterior part of the iliac crest. It travels through part of the inguinal canal, passing through the superficial inguinal ring. It supplies the mons pubis and labium majus.
- E Stratified squamous epitheliumThe cervix has a conical shape with a varied epithelium. The ectocervix is the lower intravaginal portion of the cervix and is lined by non-keratinised stratified squamous epithelium. The endocervix is the cavity of the cervix, linking the external and the internal os. It is lined by mucin-secreting simple columnar epithelium. The border between these two types of epithelium is the squamocolumnar junction, or transformation zone. The transformation zone is the area where metaplasia frequently takes place and it is from here that the cervical smear test is taken. There are certain times when metaplasia is physiological, such as during puberty when the endocervix everts and postmenopause when the transformation moves upwards.
- B AnthropoidThe basic shapes of the pelvis are as follows:
- Gynaecoid pelvis (50%): normal female type, inlet is slightly transverse oval; sacrum is wide with average concavity and inclination; subpubic angle is 90–100°.
- Anthropoid pelvis (25%): ape-like; anteroposterior (AP) diameters are long; transverse diameter short; sacrum long and narrow, subpubic angle is narrow.
- Android pelvis (20%): male type, inlet is triangular or heart-shaped with anterior narrow apex, subpubic angle is narrow < 90°.
- Platypelloid pelvis (5%): flat female type, AP diameter is short, transverse diameter is long, subpubic angle is wide.
- D PubococcygeusThe levator ani muscle is formed by the pubococcygeus, iliococcygeus and ischiococcygeus. Although considered in three parts, the muscle forms a continuous sheet, which provides significant support to the pelvic organs.Pubococcygeus forms the bulk of the levator ani muscle, arising from the back of the pubis and the white line that runs in front of the obturator canal. Its fibres form a U-shaped loop which runs around the urethra, vagina and anorectal junction, with the medial fibres blending with the upper urethra. Intermediate fibres loop around the vagina, closing the lower end on contraction. Lateral fibres run around the anus, inserting into the lateral and posterior walls of the anal canal between the internal and external sphincters.Iliococcygeus arises from the white line behind the obturator canal and inserts into the lateral margins of the coccyx.Ischiococcygeus arises from ischial spine and inserts into the coccyx.
-
The adrenal glands are retroperitoneal endocrine organs and are situated near the kidneys. They are surrounded by adipose tissue and renal fascia and are usually found at the level of the 12th thoracic vertebra. The outer cortex is mainly responsible for the synthesis of corticosteroid hormones and aldosterone and is derived from coelomic mesothelium. The inner medulla chromaffin cells are the source of catecholamines and these cells are derived from ectodermal neural crest cells.
- B Anterior division L2–L4The obturator nerve arises from the anterior division of L2–L4. It emerges from the medial border of the psoas major and descends along the muscle. It runs above and in front of the obturator vessels. It passes through the obturator foramen and enters the thigh through the obturator canal. After passing through the obturator canal, it divides into the anterior and a posterior branch. The anterior branch provides an articular branch to the hip and anterior adductor muscles. The obturator nerve provides sensory innervation to the skin on the medial surface of the thigh. The posterior branch innervates the deeper adductor muscles. The femoral nerve is formed from the posterior division of L2–L4.
- C Obturator internusThe femoral triangle is an anatomical area in the upper thigh. The borders of the femoral triangle can be remembered by the mnemonic, SAIL: Sartorius (laterally), Adductor longus (medially) and Inguinal Ligament (superiorly). The floor of the femoral triangle is formed by the iliopsoas laterally and pectineus medially. Important structures passing through the femoral triangle include the femoral nerve, artery and vein (Figure 1.4).
- A Inferior glutealGluteus maximus:Origin: posterior gluteal line of inner upper ilium, posterior surface of lower sacrum, lumbodorsal fascia and sacrotuberous ligamentInsertion: iliotibial band, ischial tuberosityNerve: inferior glutealArtery: superior and inferior gluteal arteriesAction: extension and external rotation of hip
- E Transversalis fascia lies directly below the rectus sheathThe rectus sheath is formed from the aponeuroses of three muscles: transversus abdominis, external and internal oblique muscles.Above the arcuate line, the aponeurosis of the external oblique passes in front of the rectus abdominis and the transversus abdominis passes behind; the aponeurosis of the internal oblique divides into two at the lateral margin, with the anterior lamellae passing in front of the rectus abdominis and the posterior lamellae passing behind. Scarpa's fascia is deep to the Camper's fascia and superficial to external oblique muscle. See Figure 1.5 for the anatomy of the rectus sheath above and below the arcuate line. The transversalis fascia forms the layer below the rectus sheath.
-
The ureters leave the kidney and travel inferiorly and medially along the psoas muscle. They run along the posterior pelvic brim and cross anteriorly to the bifurcation of the common iliac vessels. They continue posteroinferiorly and turn medially at the ischial spines. They then run in the base of the broad ligament where they are crossed by the uterine artery (water under the bridge). The ureter passes the lateral vaginal fornix and enters the bladder.
- B Inferior vena cavaThe right ovarian vein empties directly into the inferior vena cava. The left ovarian vein empties into the left renal vein before reaching the inferior vena cava.
- E Pudendal nerveThe pudendal nerve provides sensory innervation to the vagina. The pudendal nerve passes into the urogenital region at the end of its course and gives off the perineal branches, which supply the vagina and posterior two-thirds of the vulva. It also branches off the dorsal nerve to the clitoris.
- A Coeliac trunkThe embryonic foregut is the part which forms the mouth to the duodenum. The coeliac trunk is the first branch of the aorta once it has passed through the diaphragm. The coeliac trunk then branches into three: to the left gastric artery, the splenic artery and the common hepatic arteries.The superior mesenteric artery provides blood supply to the embryonic midgut and the inferior mesenteric to the embryonic hindgut.
- D Left ovarian arteryBoth ovaries receive their arterial supply from the ovarian arteries, which are direct branches of the abdominal aorta. Venous drainage of the right ovary is supplied by the right ovarian vein, a branch of the inferior vena cava (IVC). The left ovary's venous supply is from the left renal vein, which then drains into the IVC. The differing blood supply of the ovaries, in comparison to the other pelvic viscera, reflects the embryonic origin and subsequent descent of the ovaries from near the kidneys, down into the pelvis.
- B Is a branch of the abdominal aortaThe ovarian arteries both arise from the abdominal aorta. The paired arteries, which sit below the renal arteries and above the inferior mesenteric artery, descend along the posterior abdominal wall. These arteries cross the external iliac vessels at the 25 level of the pelvic brim. Each artery supplies its respective ovary and fallopian tube, anastomosing with the uterine arteries. Arterial and venous supply to the ovaries follow a similar course, however, the right ovary receives its venous supply from the right ovarian vein, which reaches the inferior vena cava and the left ovary is supplied by the left renal vein.
- B Median sacralThe aorta enters the abdomen through the aortic hiatus of the diaphragm at the level of T12. At the level of L4 the abdominal aorta bifurcates into the common iliac vessels, which in turn divide to form the external and iliac vessels. The abdominal aorta has three terminal branches which are: right and left common iliac arteries and the median sacral artery. There are another four paired branches which are: phrenic, suprarenal, renal and gonadal arteries.
- C IschiocavernosusThe perineal body (or central tendon of the perineum) is a midline structure formed of fibromuscular tissue found between the vagina and the anus in females. The external anal sphincter, transverse perineal muscles, bulbocavernosus muscle and the levator ani muscles all insert into the perineal body. The ischiocavernosus muscle is a muscle of the superficial pouch of the perineum. Lying between the perineal membrane and the subcutaneous tissue, it arises from the inferior ischial ramus and compresses the crus clitoris, hence promoting clitoral erection. See Figure 1.6 for the anatomy of the perineum.
- E Uterine artery, anterior division of the internal iliacThe uterine artery is a branch of the anterior division of internal iliac artery (the main artery to supply the pelvic viscera). Ovarian arterial supply comes from the ovary arteries which are direct branches of the abdominal arteries. Equivalent to the female ovarian arteries is the testicular artery, which is a branch of the abdominal aorta and supplies the testes. The internal pudendal artery, which supplies the perineum, is a branch of the anterior division of the internal iliac artery.
-
The bony pelvis consists of the innominate bone, which is formed from the ilium, ischium and the pubis, together with the sacrum and the fifth lumbar vertebrae. The sacrum is actually formed from the five sacral vertebrae. The sacrum articulates with the fifth lumbar vertebrae. Figure 1.7 shows the structure of the bony pelvis.
- E The superficial inguinal ring transmits the round ligamentThe deep inguinal ring is situated at the midpoint of the inguinal ligament. It can be located by finding the midpoint between the anterior superior iliac spine and the pubic tubercle. The superficial inguinal ring lies just above, and lateral to the pubic tubercle. The deep and superficial rings mark the entrance (deep ring) and exit (superficial ring) to the inguinal canal.The canal's boundaries are:
- Anterior wall: external oblique aponeurosis, with lateral reinforcement from the internal oblique
- Posterior wall: transversalis fascia, with the conjoint tendon (internal oblique and transversus abdominis) providing medially
- Superiorly: internal oblique
- Inferiorly: inguinal ligament
Running through the canal is the round ligament in females and the spermatic cord in males. The ilioinguinal nerve passes through the superficial inguinal ring only, having travelled down the lateral abdominal wall between the internal and external oblique muscles. See Figure 1.8 for the anatomy of the inguinal canal. - C Ilioinguinal nerve