1.1 CHEST OVERVIEW
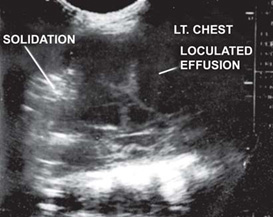
Ultrasound is a noninvasive, relatively inexpensive and most rewarding imaging modality, carries no radiation burden, but not much exploited for evaluation of chest disease because of basic (inherent) properties of US waves not to pass through bony cage and air filled lungs. However, over a couple of years, US has emerged as a useful tool in evaluating wide range of perplexing clinical problems of chest due to presence of fluid in pleural space, consolidating or atelectatic lung or even tumor, provide window for US to penetrate and this has helped in diagnosis of certain conditions or limit the DD of conditions under consideration.
- Chest wall: It has helped in diagnosing soft tissue abscesses, masses, osteomyelitis, rib tumors and even fracture where plain X-ray gives only soft tissue swelling or obliteration of costophrenic angle (may be due to pleural fluid or sometimes by rib tumor) and also where rib erosion is due to underlying carcinoma. Sometimes, when clinically mass is suspected with fractures, US can be used as a first modality particularly in children to avoid radiation by getting an X-ray chest
- Mediastinum: Anterior mediastinum can be very well evaluated by US through suprasternal route by elevating shoulders and extending the neck. This will avoid radiation particularly in children where it is due to thymus. Even paratracheal and hilar adenopathy can be diagnosed especially in tubercular patients where it is not only helpful in diagnosis but also in follow-up when child is on anti-tubercular therapy, thus avoiding unnecessary radiation and getting repeated X-rays.
- Lung parenchyma: It is also helpful in differentiating consolidation, collapse and tumor of lung. A tumor 3on US gives heterogeneous shadows, consolidation gives fluid bronchogram and collapse will give homogeneous shadow. Also it is helpful in differentiating solid vs cystic that is whether it is a hydatid cyst/thoracic kidney, etc. or a lung consolidation. Also it is helpful when X-ray chest PA view shows a homogeneous shadow in right lower zone—may be due to consolidation/hiatus hernia.
- It is also a good screening modality in opaque hemithorax—due to collapse, large consolidation, tumor of lung or even tumour from bony cage because of different US spectrum.
- It is also a good modality for diagnosing diaphragmatic pathologies and lesions above (pleural fluid/consolidation) or below (subpulmonic effusion).
- Pleura: US is a good modality to differentiate pleural lesions from parenchymal ones.It is also helpful in diagnosing minimal amount of fluid in pleural cavity, even 5–10 ml of fluid, thus avoiding need of lateral decubitus film/lateral chest film.
- It also gives the etiology of pleural fluid due to its appearance as anechoic, hypoechoic, echogenic, presence of debris, nodules and types of septa.
- Anechoic—all transudates are anechoic, however all anechoic collections are not transudates. About one-third of exudative collection tends to be anechoic in the beginning.
- Hypoechoic—usually exudative effusions, empyema and later stages of hemothorax.
- Echogenic—hemothorax or empyema.
- Debris—represents settled down pus cell, blood cells, etc.
- Septations—usually represent process of loculation and fibrosis occurring in pleural effusion. Thin clean septa with no or very minimal debris— tubercular pleural effusion.Fig. 1.1.7: Longitudinal intercostal view in a patient with pleural effusion showing echogenic surface of visceral and perietal pleuraFig. 1.1.9: Loculated multiseptated fluid collection seen in the pleural cavity with associated pleural thickeningHowever, thick, shaggy irregular septations with debris—pyogenic effusion.
- Pleural nodule/masses—represent mesothelioma, metastatic nodule and tuberculomata. In addition to characteristics septations the thickness of parietal pleura and combined (parietal + visceral) also give etiological diagnosis. As tubercular pleural effusion—parietal pleural thickness varies 2–8 mm and combined pleural varies from 4–10 mm. In pyogenic pleural effusion—parietal pleural thickness varies from 5–22 mm and combined 8–27 mm. In hemothoraces (post-traumatic) thick irregular mantle of pleura around hypoechoic pleural collection is seen, pleural thickness varies from 12–18 mm.
- Intervention—US is very helpful in fine needle aspiration biopsy, pleural tapping, guided pleural aspiration and tube placement.
- ICU—US is very helpful in critically ill-patients that is trauma and ICU—needs serial X-rays to see day to day changes in lesions—particularly when there is inability to position the patient as required and usually substandard quality of X-rays.
Limitations
- Pneumothoraces/hydropneumothorax
- Limited information about mediastinum, hilar and proximal airways
- Restricted field of view
- Familiarity of clinician
- Operator dependent
Other Advantages
- Lower cost
- Increase flexibility
- No radiation
- Good guidance tool
- Repeated evaluation with no radiation cost.
Ability to detect abdominal lesions associated with causative of chest lesion as liver abscesses leading to pleural effusion.
1.2 PLEURAL EFFUSION
Pleural effusion can be transudative or exudative.
Signs of pleural fluid on USG—transudative effusion—
Pleural (fluid) that changes shape with respiration.
Exudative effusion—
Fluid with floating echodensities
Septations—thick and shaggy
Fibrin strands
May be anechoic fluid
Echogenic fluid
Pleural nodules
Thickened pleura
Causes of Transudative Pleural Effusion
- Increased hydrostatic pressure
- Congestive heart failure
- SVC obstruction
- Constrictive pericarditis
- Decreased osmotic pressure
- Cirrhosis with ascites
- Peritoneal dialysis
- Acute glomerulonephritis
- Nephrotic syndrome
- Urinary tract obstruction
- Hypoalbuminemia
- Overhydration
- Hypothyroidism
Causes of Exudative Pleural Effusion
- Infection
- Parapneumonic effusion
- Empyema
- Tuberculosis
- Fungi (Nocardia, actinomycosis)
- Neoplasm
- Pleural metastasis
- Pleural mesothelioma
- Bronchogenic carcinoma
- Lymphoma
- Vascular
- Pulmonary emboli
- Collagen Vascular Disease
- SLE
- Rheumatoid arthritis
- Abdominal Disease
- Subphrenic abscess
- Pancreatitis
- Trauma
- Hydrothorax
- Miscellaneous
- Drug induced effusion
1.3 PLEURAL PLAQUE
Common causes of pleural plaque includes:
- Pneumonia
- Asbestos exposure
- Pulmonary infarction
- Trauma
- Chemical pleurodesis
- Drug related pleural disease
Plaques resulting from asbestos exposure are usually confined to the parietal pleura. Ultrasound demonstrates pleural plaques as smooth, elliptical, hypoechoic pleural thickening.
Visceral pleural plaques are differentiated from parietal pleura by observing the ‘gliding sign’ during respiration.
Calcified pleural plaques are irregular, echogenic and produce acoustic shadowing and comet tail artifact.
1.4 PLEURAL MASSES
- Loculated pleural effusion
- Metastasis
- Malignant mesothelioma
- Pleural fibroma
- Fibrin balls
Loculated Pleural Effusion
Anechoic collection seen within the pleural cavity.
Metastasis
Pleural effusion associated with malignant disease may result from:
Malignant cell implantation on the pleura (common causes: lung, breast and GIT cancers).
Obstruction of pleura or pulmonary lymphatics (common causes: lymphoma, breast cancer).
Obstruction of pulmonary veins usually by lung cancers.
Malignant cells shed freely into pleural space
Obstruction of thoracic ducts, resulting in chylous effusion. (usually due to lymphoma)
Sonographic findings favoring malignant etiology.
- Solid nodules in the pleural space
- Circumferential pleural thickening
- Nodular pleural thickening or >1 cm pleural thickening.
- Pleural thickening involving the mediastinal pleura.
Pleural Mesothelioma
Malignant mesothelioma is a rare and usually fatal pleural tumors associated with asbestos exposure.
Imaging Findings
Diffuse pleural thickening, often nodular and irregular (86%)
Calcification in pleura (74%)
Focal pleural mass (25%)
Rib destruction occurs with advanced disease.
Pleural Fibroma (Local Benign Mesothelioma)
A smooth lobular mass, 2–15 cm diameter arising more frequently from the visceral pleura.
Pedunculated mass changes shape with respiration (30-50%).
Forms an obtuse angle with the chest wall.
Fibrin Balls
These develop in serofibrinous pleural effusion and become visible following absorption of fluid.
Small and tend to be situated near the lung base.
- May disappear spontaneously or remain unchanged for many years.
1.5 MEDIASTINAL LYMPHADENOPATHY
Tuberculosis | Sarcoidosis | Lymphoma |
Unilateral | Bilateral | Bilateral |
— | Symmetric | Asymmetric |
Right paratracheal and tracheobron-chial nodes are most commonly involved | — Bilateral hilar with or without window lymph-adenopathy. | Superior media-stinum most right paratracheal, common site with aortopulmonary or without unilateral or bilateral hilar nodes |
— Mediastinal LN with or without hilar LN—unusual. — Characteristic involvement of bronchopulmonary nodes. | — in NHL involvement of other nodal groups (cardiophrenic, posterior media-stinal) also seen more commonly than HD | |
Low attenuation | Isodense | Isodense |
Mild homogeneous enhancement to rim enhancement | Homogeneous mild to moderate enhancement | Mild homogeneous enhancement |
May show calcification | May show rim Calcification | calcification unusual without treatment |
More likely to be confluent | Discrete | Usually discrete May be confluent with large nodal masses |
1.6 VASCULAR LESIONS OF MEDIASTINUM
Ultrasound is an excellent, noninvasive method of diagnosing masses of vascular origin in the mediastinum.
Vascular nature of a suspected mass can be confirmed by ultrasound using imaging supplemented by color flow and spectral Doppler effect—
- Tortuous brachiocephalic artery
- Aneurysm of the aorta
- Aneurysm of the sinus of Valsalva
- Right sided aortic arch
- Double aortic arch
- Dilated superior vena cava.
1.7 CYSTIC MASSES OF MEDIASTINUM
- Congenital cyst (Benign)
- Bronchogenic cyst
- Pericardial cyst
- Esophageal duplication cyst
- Neuroenteric cyst
- Thymic cyst
- Mature cystic teratoma
- Meningocele (Lateral)
- Lymphangioma
- Cystic degeneration
- Hodgkin's disease
- Metastasis to lymph nodes
- Nerve root tumors
- Mediastinal abscess
- Pancreatic pseudocyst
Ultrasonography can be useful in evaluating a mass adjacent to pleural surface or cardiophrenic angle. At US, the benign cysts typically appear as anechoic thin walled masses with increased through transmission.
- Ultrasound is used to characterize wall thickness, septations, vascularity, appearance of internal fluid, location and relationship to adjacent structures.
Pericardial cyst—results from aberrations in the formation of celomic cavities. Pericardial cysts are invariably connected to the pericardium but only a 18few cases unable to show communication with the pericardial sac.
The majority of pericardial cysts arise in anterior cardiophrenic, more commonly on the right side. Occasionally cysts are pedunculated.
Mature Cystic Teratoma
These are cystic tumors composed of well differentiated derivations from at least two of the three germ layers.
Majority of dermoid cysts are in the anterior mediastinum.
Most cystic teratoma are multilocular but unilocular cystic lesions also occur.
They may contain four types of tissues-including fluid, fat, soft tissues, calcium but fluid containing cystic component are usually prominent.
A fat fluid level within the mass is highly specific finding but is seen less frequently.
Cystic Degeneration
Many tumors and lymph nodes can undergo cystic degeneration and demonstrate mixed solid and cystic elements. If degeneration is extensive, the appearance of the lesion is indistinguishable from those of a congenital cyst. Cystic degeneration of a solid mass is more likely to occur after radiation therapy or chemotherapy but may be seen prior to treatment.
- A mediastinal abscess or pancreatic pseudocyst appears as a fluid containing mediastinal cystic mass, but clinical features usually permit differentiation from true cysts or neoplasms.
1.8 DIAPHRAGM
Bilateral Diaphragmatic Elevation
- Shallow inspiration (most common).
- Abdominal cause (USG useful by showing fluid, fetus or an abdominal mass as the cause)
- Obesity
- Pregnancy
- Ascites
- Any large abdominal mass.
- Pulmonary causes-USG little use
- Chext X-ray/CT required making the diagnosis.
- Neuromuscular disorders
- Myasthenia gravis—chest CT may show thymoma.
- Amyotropic lateral sclerosis—USG is of little use.
- MRI required for diagnosis.
Unilateral Diaphragmatic Elevation
Subpulmonic Pleural Effusion
- Ultrasound confirmatory
- Shows the presence of fluid is pleural cavity with normal relative position of bothdomes of diaphragm.
Pulmonary Causes
- USG may show the presence of elevation of one dome of diaphragm as compared to other dome. However underlying lung is usually not evaluated by ultrasound.
- Chest X-ray/CT will confirm the cause for diaphragmatic elevation.
Phrenic Nerve Paralysis (Diaphragmatic Paralysis)
- May occur due to
- Primary lung tumor
- Malignant mediastinal
- Iatrogenic
- Idiopathic
- Diagnosis is made on USG by observing the absent or paradoxical movement on the affected side with usual or exaggerated excursion on the opposite side. Paradoxical movement can be elicited by the coughing or sniffing tests.
Abdominal Causes
- Subphrenic abscesses.
- In appropriate clinical setting usually H/o surgery
- USG shows—elevated hemidiaphragm
- Reduced or absent movement of the ipsilateral diaphragm
- Subdiaphragmatic anechoic or hypoechoic collection
- Usually ipsilateral pleural effusion present.Fig. 1.8.4: Amebic liver abscess—a hypoechoic SOL is seen in the posterosuperior aspect of liver with evidence of posterior enhancement. It is extending into subdiaphragmatic space
- Liver mass: (tumor, echinococcal cyst, abscess)
- Distended stomach or colon.Interposition of colon.
Diaphragmatic Hernia
- USG may show the discontinuity of the dome of diaphragm
- Bowel, spleen, kidney may be visualized inside thorax above dome of diaphragm
- Contralateral displacement of heart is visualised
- In congenital diaphragmatic hernia, polyhydramnios may be associated after 25 weeks.
Eventration of Diaphragm
- Complete—more commonly on left
- Partial—more commonly on right
- Complete eventration of diaphragm can be diagnosed by ultrasound
- Ultrasound in focal eventration shows evidence of typical focal diaphragmatic bulge filled by liver.
Diaphragmatic Rupture
- Traumatic—blunt or penetrating trauma
- Infection—ruptured amoebic liver abscess
- In post-traumatic rupture in large, usually over 10 cm, defects ultrasound may detect–disruption of diaphragmatic echoes. Herniation of abdominal viscera into thorax—associated pleural effusion. Sometimes—small diaphragmatic rents may be difficult to detect, but due to availability of high 24frequency transducers, it is now possible to detect small disruption of diaphragmatic contour.
Neoplasms
- Very rarely diaphragmatic neoplasms
- Primary—various types of sarcomas
- Fibroma
- Secondary—Local invasion by adjacent pleural, peritoneal, thoracic and abdominal wall malignancies
- Distant metastasis from bronchogenic or ovarian cercinoma
- Wilms' tumor and osteogenic sarcoma are less common.
DIAPHRAGMATIC INVERSION
Normally diaphragm is convex towards thorax, but reverse occurs in inversion with convexity towards abdomen.
Fig. 1.8.6: Transverse view—a large pleural effusion inverting the diaphragm can look like a large cyst
Fig. 1.8.7: Free fluid seen in right pleural cavity with collapsed lung inside—note the inverted diaphragm
- More common on left side, due to protective effect of liver on right side
- Part of diaphragm or entire diaphragm may be affected
- May occur due to large pleural effusion or neoplasm, pushing the diaphragm downwards
- May show little or asynchronous motion with respiration.