The introduction of laser photocoagulation to treat ocular disorders was a major advance in ophthalmology. Proper use of lasers in ophthalmic practice starts with a good understanding of how laser works.
LASER refers to Light Amplification by Stimulated Emission of Radiation. As the term denotes, a laser derives from the excitation by a photon of light, of the atoms falling back to a lower level and thereby emitting energy in the form of radiation.
The matter, composed of the atoms and molecules, at low temperatures is in the lowest and thereby the most stable level or “ground state”. As the temperature increases, more and more atoms jump to the higher energy levels. This is described as the Boltzmann's energy distribution, according to which the higher energy level always has fewer molecules populating it than a lower level. Now if a light beam of a suitable wavelength is introduced into the medium, the beam will become attenuated and the photons will get absorbed by the atoms which get excited to a higher energy level. From here, the atoms spontaneously decay to the lower level and emit photons in random direction.
Here, it is essential to understand a phenomenon which is reverse of the Boltzmann's distribution: “population inversion”, i.e. more atoms are in the higher energy levels than in a lower level. It can be achieved by introduction of: (i) electrical discharge, and (ii) optical pump using a xenon arc lamp or another laser. In a medium with a population inversion, the introduction of a beam of light leads to subsequent emission of photons which are in phase and coherent with each other and also with the exciting light beam. So, the two prerequisites for the emission of a laser beam are:
- Population inversion of the medium, and
- A light beam of correct wavelength introduced to stimulate the excited atom into emitting light that is coherent with the exciting light beam.
Population inversion occurs when the proportion of pumping atoms in the higher energy level is larger than the decay into the lower energy level. This increases the rate of stimulated emission and is a prerequisite for laser emission. This chain reaction is amplified by surrounding the medium with two mirrors, one of which is totally reflective and the other one typically partially reflective. To constrain the direction of radiation release, the excited atoms are contained in a laser cavity.
Properties of the laser: It is monochromatic, therefore eliminates chromatic aberration, in phase, i.e. all the photons produced are in phase with each other unlike normal light beam where photons exist in random phases, is coherent, is collinear and with limited divergence. The resultant beam of light is easy to focus to a small spot. The total amount of light produced depends on the volume of the optical cavity, not the surface area.4
Different types of laser materials are available. They include solid state and gas lasers. In many lasers used in ophthalmology, noble gases, such as krypton and argon, are ionized within a tube. Other lasers are formed from crystals containing rare earths, such as Nd:YAG laser, which uses neodymium in an yttrium-aluminium-garnet crystal.
Lasers allow precise treatment of a variety of eye problems without risk of infection. Most laser procedures are also relatively painless and can be done on an outpatient basis. This combination of safety, precision, convenience, and reduced cost make lasers one of the most successful medical tools available to ophthalmologists.
Continuous Wave Lasers: Gas Ion Lasers
Most lasers used for photocoagulation are of this type and include argon and krypton ion lasers. Low pressure gas is pumped with a high electrical current that excites the gas. An integral cooling system is required for gas discharge lasers. A shutter mechanism is used to allow a selected duration of light to reach the desired tissue.
Semiconductor Lasers
These are made by joining a p-type (atom with a relative deficiency of electrons) material with n-type (atom with an excess electron) material to produce p-n junction. Heat built-up is very detrimental to semiconductors and this limits the output. Only a limited number of wavelengths are available for such lasers; most of these are in the infrared and deep red wavelengths.
Photodisruptive Lasers
Energy is used to raise electrons to a higher energy metastable state in photodisruptive lasers, just as in continuous wave lasers. There are two main ways the laser cavity can be switched, using either Q-switching or lock mode methods. The functional difference between these two modes is not important for clinical use. These lasers concentrate energy used to pump electrons into a light pulse that lasts on the order of 10−8 seconds or less. Even though the total energy delivered may be only 1mJ, the concentrating effect of the short duration creates an irradiance of millions of watts. This produces an optical breakdown and formation of plasma from molecules in tissue in a region confined to the focus point of the laser. This can be used to cut or perforate without coagulating tissue.
The most common photodisruptive laser used in ophthalmic practice is the Nd:YAG laser. Because of the extremely high energy densities produced, photodisruptive lasers do not depend on absorbing pigments to produce optical breakdown. This allows us to cut clear tissue such as vitreous fibers, lens capsule, and posterior hyaloid phase.
Choice of Wavelength
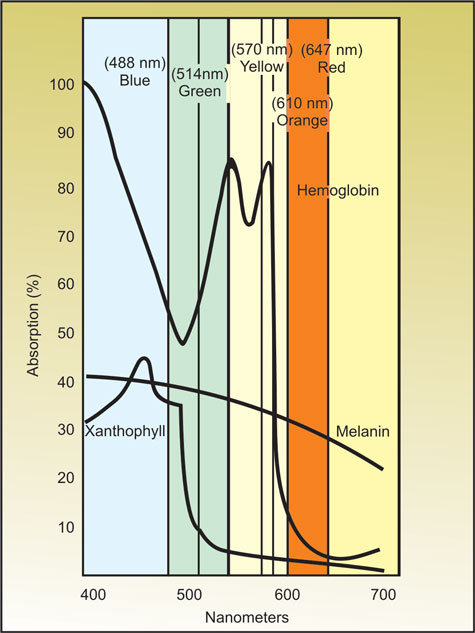
A number of wavelengths are available to the surgeon. The reasons to pick one wavelength over another are mostly theoretical, but the overriding concern is an attempt to increase the therapeutic index. One wavelength, argon blue, should not be used as blue light is more likely to be scattered and has the potential to be absorbed by the xanthophyll in the macula causing unintended macular damage.5
Diode | 810 nm |
Krypton red | 647 nm |
Krypton yellow | 568 nm |
Frequency doubled NdYAG | 532 nm |
Argon green | 514 nm |
Argon blue | 485 nm |
Xanthophyll pigment of the retina absorbs blue light, but passes green, yellow and red. Hemoglobin in blood vessels absorbs blue, green and yellow light, but does not absorb red as well. Melanin in RPE and the choroid absorb all visible wavelengths.
Longer (towards red) wavelengths are scattered less and therefore penetrate the cloudy media better. Longer wavelengths (like diode), owing to their increased penetrance, are frequently more painful.
Yellow laser has among its advantages, minimal scatter through nuclear sclerotic lenses, low xanthophyll absorption, and little potential for photochemical damage. It is useful for destroying vascular structures with little damage to adjacent pigmented tissue.
The key pigments found in ocular tissues are (Fig. 1.1):
- Melanin: Excellent absorption by green, yellow, red and infra-red wavelengths.
- Macular xanthophyll absorbs blue but minimally absorbs yellow or red wavelengths.
- Hemoglobin easily absorbs blue, green and yellow with minimal absorption of red wavelength.
SUGGESTED READING
- Esperance FA Jr. Photocoagulation of ocular disease: Application and technique in: L' Esperance FA Jr. ed. Ophthalmic lasers 3rd Ed. Mosby: St. Louis: 1989.
- Mainster MA. Laser light interactions and clinical systems. In: L' Esperance FA Jr. Ed: Ophthalmic lasers 3rd Ed. Mosby: St. Louis: 1989.