DEVELOPMENTAL DISTURBANCES OF THE JAWS
Developmental disturbances are diverse group of deformities in the embryonic development of the head and facial structures. Anomaly as a medical term which means irregularity or deviation from normal. These abnormalities may be present as congenital (Present at bunt) or inherited (transmitted genetically). Developmental disturbances may be mild or severe. Numerous factors contribute to their development.
AGNATHIA
(Otocephaly, Holoprosencephaly Agnathia)
- Extremely rare congenital defect characterized by absence of the maxilla or mandible.
- Only a portion of jaw is missing.
- In maxilla there may be one maxillary process or even the premaxilla is involved.
- In mandible the entire mandible of one side may be missing, or only the condyle or entire ramus will be missing.
- There may be bilateral agenesis of the condyles and of the rami.
MICROGNATHIA
- Means a small jaw.
- Either the maxilla or mandible may be affected.
- Associated with congenital heart disease and Pierre Robin syndrome.
- Micrognathia of the maxilla is frequently due to a deficiency in the premaxillary area and patients with this deformity appear to have middle third of face retracted.
- Micrognathia may be one of the predisposing factors in mouth breathing owing to associated with maldevelopment of the nasal and nasopharyngeal structures.
- Acquired type of micrognathia is of postnatal origin and usually results from a disturbance in the area of the temporomandibular joint.
MACROGNATHIA
- Refers to the condition of abnormally large jaws.
- Increase in size of both jaws is frequently proportional to a generalized increase in size of the captive skeleton.
- General factors which conceivably influence and find to favor mandibular prognathism are.
- Increased height of the ramus.
- Increased mandibular body length.
- Increased gonial angle.
- Anterior positioning of the glenoid fossa.
- Decreased maxillary length.
- Prominent chin button.
- Varying soft tissue contours.
e.g. Pituitary gigantism, Paget's disease leontiasis osseae, acromegaly.
FACIAL HEMIHYPERTROPHY
It is a rare developmental anomaly characterized by asymmetric overgrowth of one or more body parts.3
More commonly known as hemihypertrophy.
Can be an isolated condition, but also may be associated with a variety of malformation syndromes.
Malformation syndromes associated with hemihyperplasia:
- Beckwith-Wiedemann syndrome
- Neurofibromatosis syndrome
- Klippel-Trenaunay-Weber syndrome
- Proteus syndrome
- McCune-Albright syndrome
- Epidermal nevus syndrome
- Triploid/diploid mixoploidy
- Langer-Giedion syndrome
- Multiple exostoses syndrome
- Maffucci's syndrome
- Ollier syndrome
- Segmental odontomaxillary dysplasia
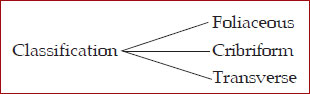
Classification
- Complex hemihyperplasia
- Simple hemihyperplasia
- Hemihyperplasia involving one side of the face.
Etiology
Unknown. May be vascular or lymphatic abnormalities, CNS disturbances and chromosomal abnormalities.
Clinical Features
Enlargement of face confined to one side of the body. Unilateral macroglossia, premature development, eruption, increased size of the dentition.
Familial occurrence is also seen.
Oral Manifestations
Alteration in the crown size, root size and shape and rate of development.
Most commonly cuspids, premolars and first molars are involved.
Bone of the maxilla and mandible are enlarged. Sometimes altered trabecular pattern.
Buccal mucosa appears velvety, seem to hang in soft, pendulous folds on the affected side.
• Treatment and Prognosis
No specific treatment.
FACIAL HEMIATROPHY
(Parry Romberg syndrome, Romberg Parry syndrome, progressive facial hemiatrophy, progressive hemifacial atrophy)
First reported by Romberg in 1846.
Characterized by slowly progressive atrophy of the soft tissue of half of the face. It is manifested as progressive wasting of subcutaneous fat, atrophy of the skin, cartilage, bone and muscle.
Etiology
Primary factor is cerebral disturbance leading to increased and unregulated sympathetic nervous system.
Local trauma, infection
Genetic alterations.
Clinical Features
Painless cleft on the midline of the face or forehead.
Atrophy of the skin, subcutaneous fat, muscle, bone, cartilage, alveolar bone. Neurological disturbances may be seen.
Oral Manifestations
Incomplete root formation
Delayed eruption
Difficulty in mastication
Treatment and Prognosis
DEVELOPMENTAL DISTURBANCES OF THE LIPS AND PALATE
VAN DER WOUDE'S SYNDROME
(Cleft lip syndrome, lip pit syndrome, dimpled papillae of the lip)
It is an autosomal dominant syndrome consisting of a cleft lip or cleft palate and distinctive pits of the lower lips.
Etiology
Prominent feature of this syndrome is orofacial anomalies. This is due to abnormal fusion of palate and lips at days 30-50 postconception.
Clinical Features
- Incidence is 1 in 100,000 people.
- Affects both generation equally.
- Cleft lip and cleft palate is commonly seen. Unilateral or bilateral involvement is seen.
- Hypernasal voice and cleft or bifid uvula is the clue for diagnosis.
- Lower lip pits are quite distinctive and medial on the vermilion portion of the lower lip.
- Extraoral manifestations
- Rare but include limb anomalies, popliteal webs, brain anomalies, accessory nipples, congenital heart diseases can be seen.
Treatment and Prognosis
- Surgical repair of the cleft lip and palate in cases of cosmetic reasons.
CONGENITAL LIP AND COMMISSURAL PITS AND FISTULAS
Etiology
- May result from notching of the lip at an early stage of development.
- Fixation of the tissue at the base of the notch.
- Failure of complete union of the embryonic lateral sulci of the lip.
Clinical Features
- Unilateral or bilateral depression or pit that occurs on the vermilon surface of lip.
- Sparse mucus secretion may exude from the base of the pit.
- Lip appears swollen, accentuating the appearance of the pits.
Treatment
- Surgical excision has been recommended.
DOUBLE LIP
- It is an anomaly characterized by a fold of excess tissue on the inner mucosal aspect of the lip.
Clinical Features
- Both upper and lower lips are involved.
- When the upper lip is sensed, the double lip resembles a cupids bow.
- Occurrence of acquired double lip in association with blepharo-chalasis and nontoxic thyroid enlargement is known as “Ascher's syndrome”.
- Blepharochalasis is drooping of tissue between the eyebrow and the edge of upper eyelid so that it hangs loosely over margin of the lid.
Treatment
- No treatment is necessary except for cosmetic purposes or functions involving speech and mastication.
CLEFT LIP AND CLEFT PALATE
- Classification of cleft lip
- Unilateral incomplete.
- Unilateral complete.
- Bilateral incomplete.
- Mandibular cleft lip is an extremely rare condition that occurs in the midline of the lowerlip.
- It is due either failure of the copula to give rise to mandibular arch or to persistence of the central groove of the mandibular process.
- Maxillary cleft lip is thought to be due to failure of the globular portion of the median nasal process to unite properly with the lateral nasal and maxillary process.
- Cleft may also be due not to an actual lack of union of the processes but rather to a failure of mesodermal penetration and the obliteration of the ectodermal grooves separating these mesodermal masses that actually constitute the facial processes.
- Cleft palate appears to represent a disturbance in the normal fusion of the palatal shelves.
- Failure to unite due to lack of forceful interference by the tongue, disparity in the size of the parts involved.
Etiology
- Heredity is undoubtedly one of the most important factors to be considered.
Environmental Factors
- Genetic in origin.
- Physiologic, emotional or traumatic stress may play a significant role.
Other Factors
- A defective vascular supply to the area involved.
- A mechanical disturbance in which the size of the tongue may present the union of parts.
- Circulating substances such as alcohol and certain drugs.
- Infections.
Clinical Features
- Unilateral cleft lip involves only one side of the lip or both sides of the lip.
- The latter type has given rise to term harelip.
- Cleft lip and cleft palate are somewhat more common in boys than in girls.
- Cleft occurs about three times more frequently on the left side than on the right.
- Cleft of the hard palate extends anteriorly through the alveolar ridge and lip, producing a complete cleft in the lip, ridge and palate.
- Isolated cleft palate is associated with congenital heart diseases, polydactylism and syndactylism, hydrocephalus, microcephalus, club foot, supernumerary ear, hypospadias, spina bifida, hypertelorism and mental deficiency.
- A median maxillary anterior alveolar cleft might be due to precocious limitation of the growth of the primary ossification centers on either side of the midline at the primary palate or to their subsequent failure to fuse.
Clinical Significance
- Eating and drinking are difficult because of regurgitation of food and liquid through nose.
Treatment
- Surgery can correct cleft palate. Operation to close the cleft is not usually carried out until the patient is 18 months old.
CHEILITIS GLANDULARIS
- Occurs mostly in adult, the lower lip becomes enlarged, firm and finally everted.
Etiology
- Unknown etiology, but it can be due to:
- Chronic exposure to sun, wind and dust.
- Use of tobacco.
Clinical Features
- Labial salivary glands become enlarged and sometimes nodular.
- Orifices of the secretory ducts are inflamed and dilated appearing as small red macules on the mucosa three basic types of cheilitis glandularis are seen:
- Simple type
- Superficial suppurative type
- Deep suppurative type.
- Simple type is characterized by multiple painless pinhead sized lesions with central depressions and dilated canals.
- This type may be transformed into superficial suppurative type characterized by painless swelling, induration, crusting, superficial and deep ulcerations of the lip. (Baelz's disease).
- Deep suppurative type (Cheilitis glandularis apostematosa, myxadenitis labialis) is a deep seated infection with abscesses and fistulous tracts that eventually form scars.
Treatment
- Because of relatively high incidence of associated malignancy, a vermilionectomy or surgical stripping of the lip has been recommended.
CHEILITIS GRANULOMATOSA
(Mieschers-Melkersson-Rosenthal syndrome)
Clinical Features
- There is a diffuse swelling of the lips, especially lower lip. Swelling is usually soft and exhibits no pitting upon pressure.
- Scaling, fissuring, erythematous vesicles or pustules present.
- Appears in association with facial paralysis and scrotal tongue called Melkersson-Rosenthal syndrome
Histologic Features
- Chronic inflammatory cell infiltrate particularly peri and paravascular aggregations of lymphocytes, plasma cells and histiocytes and focal noncaseating granuloma formation with epitheloid cells and Langhans’ type of giant cells.
HEREDITARY INTESTINAL POLYPOSIS SYNDROME
(Peutz-Jeghers syndrome)
- Pigmented spots on the face, oral cavity and sometimes the hands and sometimes the hands and feet.
Clinical Features
- Melanin pigmentation of the lips and oral mucosa is present from birth and appears as small brown macules measuring 1-5 mm in diameter.
- Buccal mucosa is frequently involved.
- On the face the spots tend to be grouped around the eyes, nostrils and lips,
- Lower lip is almost involved.
- Facial pigmentation tends to fade later in life.
- Oromucosal pigmentation includes melanin pigmentation such as:
- Local and ethnic pigmentation.
- Oral pigmentary manifestations of systemic diseases.
- Pigmentary disturbances associated with pharmaceuticals and other chemicals.
- Benign and malignant pigmented neoplasms.
- Intestinal polyps are distributed through the entire intestine.
- Patients have frequent episodes of abdominal pain and signs of minor obstruction.
- Role of dentist in detecting this syndrome is important through a tentative diagnosis based on the oral and paraoral manifestations.
DEVELOPMENTAL DISTURBANCES OF ORAL MUCOSA
FOCAL EPITHELIAL HYPERPLASIA
(Heck's Disease)
It is the one of the most contagious oral papillary lesions caused by HPV (human papilloma virus).
Clinical Features
- No gender predilection.
- Involves the labial, buccal and lingual mucosa mainly but gingiva and soft palate can be affected.
- Characterized by broad based or slightly elevated, well demarcated plaques. Frequently papillary in nature, relatively smooth surfaced, flat topped lesions.
- Appears as cobblestone or fissured appearance.
Histologic Features
- Considerable focal acanthosis of the oral epithelium.
- The thickened mucosa extends upward, not down into underlying connective tissues, hence the adjacent normal rete ridges.
- Ridges are widened and club shaped.
Treatment and Prognosis
Conservative excisional biopsy
FORDYCE'S GRANULES
(Fordyce's Disease)
- Also called Fordyce's disease and sebaceous nevi.
- Not a disease of oral mucosa. It is a developmental anomaly characterized by heterotopic collections of sebaceous glands at various sites in the oral cavity.
- This occurs due to inclusion of sebaceous glands in the oral cavity of ectoderm during development of the maxillary and mandibular processes of embryonic life.
Clinical Features
- Appears as small yellow spots, either seen individually or forming a large plaques, often projecting slightly above the surface of the tissue.
- Most frequently seen as a bilaterally symmetrical pattern. On the cheek mucosa, opposite the molar teeth.
Other Sites
- Inner surface of the lips.
- Retromolar region lateral to the anterior faucial pillar.
- Current research states that it can be seen in esophagus, the female genitalia including the uterine cervix, the nipples, the palms and soles, the parotid glands, the larynx and the orbit.
- Incidence of oral condition is 80%.
- No significant difference in occurrence between the genders or races.
Histologic Features
- Glands are usually superficial and may consist of only a few or a great lobules, all grouped around one or more ducts which open on the surface of the mucosa.
- Ducts may show keratin plugging.
Treatment
- No treatment required.
- Very rarely a benign sebaceous gland adenoma and keratin filled pseudocyst develops.
DEVELOPMENTAL DISTURBANCES OF THE TONGUE
MICROGLOSSIA
- Is a rare congenital anomaly manifested by the presence of a small or rudimentary tongue.
- When tongue is completely absent at birth, the condition is known as aglossia.
MACROGLOSSIA
- Congenital macroglossia is due to an overdevelopment of the musculature which may or may not be associated with generalized muscular hypertrophy or hemihypertrophy.
- Secondary macroglossia may occur as tumor of the tongue such as diffuse lymphangioma or hemangioma, from neurofibromatosis, blockage of efferent lymphatic vessels, in cases of malignant neoplasms.
- In cases of acromegaly it is due to hyperpituitarism in the adult, cretinism, congenital hypothyroidism; Beckwith's hypoglycemic syndrome.
- Macroglossia may produce displacement of teeth malocclusion.
Treatment
- Removal of the primary cause.
- Surgical trimming.
ANKYLOGLOSSIA
(Tongue tie)
- Fusion between the tongue and floor of the mouth.
- Usually result of a short lingual frenum of one which is attached too near the tip of the tongue.
- There is restricting movement of tongue, exhibit speech difficulties in pronunciation of certain consonants and diphthongia.
Treatment
- Treated surgically by clipping the frenum.
CLEFT TONGUE OR BIFID TONGUE
- Manifested as a lay groove in the midline of the dorsal surface.
- Results because of incomplete merging and failure of groove obliteration by underlying mesenchymal proliferation.
- It is found in association with orofacial digital syndrome.
FISSURED TONGUE
(Scrotal tongue, Lingua plicata)
- Malformation manifested clinically by numerous small furrows or grooves on the dorsal surface, radiating out from a central groove along the midline of the tongue.
- It is not a developmental malformation, the incidence of this condition increases with age.
- Associated with some extrinsic factor such as chronic trauma or vitamin deficiencies.
Treatment
- It is usually painless except in occasional cases in which food debris tends to collect in the grooves and produce irritation.
- Material may be removed by stretching and flattening the fissures and using a tooth brush or gauze sponge to cleanse the surface.
MEDIAN RHOMBOID GLOSSITIS
(Central papillary atrophy of the tongue)
- Congenital abnormality which is presumable due to failure of the fusion of tuberculum impair to retract or withdraw before fusion of the lateral halves of the tongue, so that a structure devoid of papillae is interposed between them.
- An etiologic relationship between median rhomboid glossitis and a localized chronic fungal infection specifically Candida albicans.
- Presence of fungal hyphae in histology sections of biopsies.
- Common among diabetes.
Clinical Features
- Clinically as an ovoid, diamond or rhomboid shaped reddish patch or plaque on the dorsal surface of tongue anterior to circumvallate papillae.
- A flat or slightly raised area and mamelonated. It has no filiform papillae.
- Occurs three times more frequently in men than women.
Histologic Features
- Loss of papillae with varying degrees of hyperparakeratosis.
- Proliferation of spinous layer with elongation of the rete ridges which may branch and anastomose.
- Lymphocytic infiltration within connective tissue.
- Numerous blood vessels and lymphatics.
- Degeneration and hyaline formation within the underlying muscle.
- Fungal hyphae are found in the parakeratin or in superficial spinous layer of epithelium.
- Best visualized by Periodic acid schiff (PAS) stain.
Treatment
- Antifungal agents like nystatin and amphotericin B can be used.
BENIGN MIGRATORY GLOSSITIS
(Geographic tongue, wandering rash, glossitis areata exfoliativa, erythema migrans)
- May be related to emotional stress.
Clinical Features
- Multiple areas of desquamation of the filiform papillae of the tongue in an irregular circinate pattern.
- Central portion of the lesion appears inflamed while the border is outlined by a thin, yellowish while line or band.
- Fungiform papillae persist in the desquamated areas small, elevated red dots.
- Areas of desquamation remains for a short time in one location and heal and appear in another thus giving rise to the idea of migration.
- “Ectopic geographic tongue” or erythema circinate is located at other sites in the oral cavity, like buccal mucosa, gingiva, palate, lips and floor of the mouth.
Histologic Features
- Filiform papillae are lost. Hyperparakeratosis and acanthosis seen.
- Migration of (PMNL) polymorphonuclear leukocytes and lymphocytes into the epithelium producing degeneration of epithelial cells and microabscess formation near the surface.
- Inflammatory cell infiltration of underlying connective tissue chiefly neutrophils, lymphocytes and plasma cells are seen.
Treatment
- Heavy therapeutic doses of vitamins have been used.
HAIRY TONGUE
(Lingua nigra, Black hairy tongue)
Clinical Features
- Condition is characterized by hypertrophy of filiform papillae of the tongue, with lack of normal desquamation which is extensive and form a thick matted layer on dorsal surface.
- Color of papillae may vary from yellowish white to brown or even black depending upon staining by extrinsic factors as tobacco, foods, medicines, chromogenic organisms.
Etiology
- Unknown etiology.
- Certain microorganisms particularly fungi might be exciting factor.
- Many different types of organisms including Candida albicans may be cultured from scrapings of the papillae.
- Systemic disturbances like anemia, gastric upsets are responsible for hairy tongue.
- Oral use of certain drugs (sodium perborate, sodium peroxide, antibiotics such as penicillin and aureomycin), heavy smoking.
- Development of hairy tongue is frequently seen in patients who have had extensive X-ray radiation of head and neck.
Treatment
- Benign condition. So, treatment is empirical because of unknown etiology.
- Tongue may be brushed with a toothbrush to promote desquamation and remove the debris.
DEVELOPMENT DISTURBANCES OF SALIVARY GLAND
ATRESIA
It is defined as congenital occlusion or absence of one more of the major salivary gland ducts is an exceedingly rare condition. When it occurs it may result in the formation of a retention cyst or produce a relatively severe xerostomia.18
ABERRANCY
Because of widespread distribution of accessory salivary gland it is very difficult to define the condition of aberrancy.
As these salivary glands are common in lips, palate buccal mucosa floor of the mouth, aberrancy can be construed as simply that condition in which these glands are found farther from their own usual location.
No clinical significance to be attached in any event other than they may be the site of development of a retention cyst or neoplasm. Occasional cases have been reported with salivary gland tissue present within the body of the mandible.
It has been found that this glandular tissue anatomically communicated with the normal submaxillary or sublingual gland through a stalk or pedicle of tissue which perforate the lingual cortical plate.
For this reason this aberrancy represents only an extreme example of the condition known as the developmental lingual mandibular salivary gland depression.
APLASIA
(Agenesis)
- Glands or groups of glands may be missing unilaterally or bilaterally.
Classical Features
- Xerostomia or dry mouth.
- Oral mucosa appears dry, smooth, pebbly, cracking of the lips and fissuring of the corners of the mouth.
- Collection and stagnation of food debris around the teeth resulting in rampant dental caries and early loss of deciduous and permanent teeth.
Treatment
- Institution of oral hygiene to prevent dental caries.
XEROSTOMIA
(Dryness of the Mouth)
- Is a clinical manifestation of salivary gland diseases.
Clinical Features
- Patient complains of a dry or burning sensation.
- Severe alterations in mucous membranes and the patient have extreme discomfort.
- Mucosa appears dry atrophic, inflamed, pale and translucent.
- Soreness, burning and pain of the mucous membrane and tongue.
Etiology
- Associated with an emotional reaction; with blockage of duct by calculus.
- With acute or chronic infection of the salivary glands.
- Administration of various drugs such as atropine or various antihistamine drugs, causes transient or partial chronic obstruction.
- Salivary gland aplasia.
- X-ray radiation.
- Administered in the treatment of a tumor, induces prompt xerostomia.
- Vitamin deficiency
- Affects specialized epithelium.
- Results in squamous metaplasia of the ductal epithelium with retention of salivary secretion.
- Sicca syndrome or keratoconjunctivitis sicca is caused by vitamin A deficiency.
- Riboflavin and nicotinic acid deficiencies causes xerostomia.
- Sjögren's syndrome
- Xerostomia occurs because of distinction and atrophy of acinar tissue of the salivary glands.
- Miscellaneous
- Pernicious anemia, iron deficiency anemias.
- Hemorrhage, excessive sweating, diarrhea, vomiting, polyuria, organic lesions of the nervous system.
Clinical Significance
- Rampant dental caries and subsequent loss of teeth.
- Have difficulty with artificial dentures.
- Dental appliances are disagreeable.
Treatment
- Depends upon the nature of the disease. Etiology should be removed. Symptomatic treatment given.
DEVELOPMENTAL LINGUAL MANDIBULAR SALIVARY GLAND DEPRESSION
(Static bone cavity, static bone cyst, latent bone cyst, Stafne cyst or defect)
- First recognized by Stafne in 1942.
- Developmental inclusion of glandular tissue within or adjacent to the lingual surface of the body of mandible in a deep, well circumscribed depression.
Radiological Features
- Appears as an ovoid radiolucency situated between mandibular canal and the inferior border of the mandible. Commonly seen in the second or third molar area just anterior to the angle.
- Occasionally bilateral.
- Depression may be due to actual presence of salivary gland anthion the mandible during embryonic development or may be an indentation on the lingual surface.
DEVELOPMENTAL DISTURBANCES OF TEETH
(Disturbances in Size of Teeth)
MICRODONTIA
- It is used to describe teeth which are smaller than normal.
- In true generalized microdontia, all the teeth are smaller than normal. e.g.: Pituitary dwarfism.
- In relative generalized microdontia, normal or slightly smaller than normal teeth are present in jaws that are somewhat larger than normal.
- Microdontia involving a single tooth, affects mostly the maxillary lateral incisor and the third molar, e.g. Peg lateral.
MACRODONTIA
- Refers to teeth larger than normal.
- True generalized: All teeth are larger than normal, e.g.: pituitary gigantism.
- Relative generalized: Presence of slightly larger than normal teeth in small jaws.
- Macrodontia involving single tooth is common.
- In hemihypertrophy of the face it can be seen but its not a true type.
DEVELOPMENTAL DISTURBANCES IN SHAPE OF TEETH
GEMINATION
- Anomalies which arise from an attempt at division of a single tooth germ by an invagination, with resultant incomplete formation of two teeth.
- The structure is usually one with two completely or incompletely separated crowns that have a single root and root canal.
- Seen in deciduous as well as permanent dentition.
- The term “twinning” is used to designate the production of equal structures by division resulting in one normal and one supernumerary tooth.
FUSION
- Arise through union of two normally separated tooth germs.
- Depending on stage of development of teeth at the time of union, fusion may be complete or incomplete.
- Some physical force or pressure produces contact of the developing teeth and their subsequent fusion occurs.
- If contact occurs early before calcification begins, the two teeth may be completely united to form a single large tooth.
- If contact of teeth occur when a portion of the tooth crown has completed its formation there may be union of roots.
- Possible clinical problems related to appearance, spacing and periodontal conditions have been noticed.
CONCRESCENCE
- A form of fusion which occurs after root formation has been completed.
- The teeth are united by cementum only.
- Thought to arise as a result of traumatic injury a crowding of teeth with resorption of interdental bone so that the two roots are in approximate contact and become pushed by deposition of cementum between them.
- May occur before or after teeth have erupted.
- Diagnosis is by roentgenographic examination.
- With fused teeth the extraction of one may result in extraction of the other.
DILACERATION
- Refers to an angulation or a sharp bend or curve in the root or crown of a formed tooth.
- It is thought to be due to trauma during the period in which the tooth is forming with result that the position of calcified portion of the tooth is changed and the remainder of the tooth is formed at an angle.
- Curve or bend may occur anywhere along the length of the tooth, at the cervical portion, at other times midway along the root or own just at the apex of the root, depending upon the amount of root formed when the injury occurred.
- Dilacerated teeth present difficult problems at the time of extraction.
TALON CUSP
- An anomalous structure resembling an eagles talon projects lingually from the cingulum areas of a maxillary and mandibular permanent incisor.
- The cusp blends smoothy with the tooth except that there is a deep developmental groove where the cusp blends with the sloping lingual tooth surface.
- It poses problems for the patient in terms of esthetics, caries control and occlusal accommodation.
- Prevalent in persons with Rubinstein-Taybi syndrome.
DENS IN DENTE
(Dens invaginatus, dilated composite odontome)
- Is a developmental variation which is thought to arise as a result of an invagination in the surface of a tooth crown before calcification has occurred.
Causes
- Increased localized external pressure, focal growth retardation and focal growth stimulation in certain areas of tooth bud.
- Permanent maxillary lateral incisors are mostly involved.
- Maxillary central incisor are sometimes involved.
Radiological Features
- It is recognized as a pear shaped invagination of enamel and dentin with a narrow constriction at the opening on the surface of the tooth and closely approximating, the pulp in its depth. Food debris may become packed in this area with resultant caries and infection of the pulp.
- Dens in dente may exhibit an invagination that extends nearly to the apex of the root.
DENS EVAGINATUS
(Occlusal tuberculated premolar, Leong's premolar, evaginated odontome, occlusal enamel pearl)
- Is a developmental condition that appears clinically as an accessor cusp or a globule of enamel on the occlusal surface between the buccal and lingual cusps of premolars, unilaterally or bilaterally.
- Pathogenesis of the lesion is thought to be proliferation and evagination of an area of the inner enamel epithelium and subjacent odontogenic mesenchyme into the dental organ during early tooth development.
- This extra cusp may contribute to incomplete eruption, displacement of teeth or pulp exposure with subsequent infection following occlusal wear off.
TAURODONTISM
(Bull like teeth)
- Dental anomaly in which the body of the tooth is enlarged at the expense of the roots.
• Shaw classified taurodont into | – Hypotaurodont – Mesotaurodont – Hypertaurodont |
Causes of Taurodontism
- Failure of epithelial sheath to invaginate at the proper horizontal level.
- Specialized or retrograde character.
- Primitive pattern.
- Mendelian recessive trait.
- Atavistic feature.
- Mutation resulting from odontoblastic deficiency during dentinogenesis of the roots.
- It is associated with Klinefelter's syndrome (males whose sex chromosome constitution includes one or more extra X chromosomes).
Clinical Features
- May affect either deciduous or permanent dentition.
- Teeth involved are molars.
- It may be unilateral/bilateral.
Radiological Features
- Involved teeth are rectangular in shape.
- Pulp chamber is extremely large with greater apico-occlusal height.
- Pulp lacks the usual constriction at the cervical of the tooth and roots are short.
- Bifurcation or trifurcation is only a few mm above the apices of roots.
DEVELOPMENTAL DISTURBANCES IN NUMBER OF TEETH
ANODONTIA
- Total anodontia in which all teeth are missing may involve both deciduous and permanent dentition. It is associated with hereditary ectodermal dysplasia.
- Induced or false anodontia occurs as result of extraction of all teeth.
- Pseudoanodontia is applied to multiple unerupted teeth.
- True partial anodontia (hypodontia or oligodontia).
- All four first molars are missing.
- Congenitally missing deciduous teeth usually involve the maxillary lateral incisor.
- The etiology of missing teeth is that it is actually the result of one or more point mutations in a closely linked polygenic system transmitted as an autosomal dominant pattern with incomplete penetrance and variable expressivity.
SUPERNUMERARY TEETH
- Develop from a fluid tooth bud arising from the dental lamina near permanent tooth bud or from splitting of the permanent but itself.
- Most common tooth is mesiodens.
- Maxillary 4th molar is the second most supernumerary tooth.
- Other supernumerary teeth are maxillary paramolars, mandibular premolars and maxillary lateral incisors.
- It may be erupted or impacted.
- Frequently cause malposition of adjacent teeth or present their eruption.
- Found in cleidocranical dysplasia, Gardner syndrome.
DEVELOPMENTAL DISTURBANCES OF STRUCTURE OF TEETH
ENVIRONMENTAL ENAMEL HYPOPLASIA
Caused by environmental factors.
Either primary or permanent dentition is involved.
Both enamel and dentin are affected.
Causes
Nutritional deficiencies
Exanthematous diseases
Congenital syphilis
Hypocalcemia
Birth injury, prematurity, Rh incompatibility
Local infection/trauma
Ingestion of chemicals
Types
- Mild – few small grooves, pits or fissures in enamel surface.
- Moderate – rows of deep pits arranged horizontally across the tooth.
- Severe – considerable portion of enamel may be lost.
Clinical Features
Due to nutritional deficiency
Mainly deficiency of vitamin A, C and D during tooth formation.
Usually pitting type of hypoplasia is seen.
Involve those teeth that form within the 1st year after birth.
Due to exanthematous fevers
Measles, chickenpox, scarlet fever are the common causes.
Ameloblasts being one of the most sensitive group of cells in terms of metabolic function are easily affected by any systemic diseases.
Due to congenital syphilis
Pathognomonic appearance is seen.
Involves maxillary and mandibular permanent incisors and 1st molars.
Incisors shows “Hutchinson's teeth” characterized by screw driver shaped, mesial and distal surfaces of crown taper towards the notched incisal edge.
Molars show “Mulberry molars” characterized by irregular crowns and enamel of the occlusal 1/3rd arranged in an agglomerate mass.
Due to hypocalcemia
When serum calcium level falls below 6 mg/100 ml, pitting variety of enamel hypoplasia is seen.
Due to birth injuries
Hypoplasia is common in prematurely born children.
Children suffering from Rh hemolytic diseases at birth showed recognized staining of teeth.
Generally seen in the enamel formed after deciduous dentition
Due to local infections
Turner's teeth – any degree of hypoplasia (mild, moderate and severe).
Infection of periapical region of deciduous teeth affect the ameloblastic layer of secondary dentition resulting in hypoplastic crowns.
Due to chemicals
Mainly due to fluorides
Mottled enamel is seen characterized by ingestion of fluoride in drinking water during the tooth formation.
Disturbance of the ameloblasts during formative stage results in defective or deficient enamel matrix.
Clinical features varies from occasional white flecking or spotting to white opaque areas involving more of tooth surface, pitting and brownish staining of surface and corroded appearance of the teeth.
Due to idiopathic factors
Ameloblast being a sensitive cell gets affected easily by even illness or some mild systemic disturbances, which is not significantly remembered by the patients.
AMELOGENESIS IMPERFECTA
(Hereditary enamel dysplasia, hereditary brown enamel, hereditary brown opalescent teeth)
- It is an ectodermal disturbance since the mesodermal components of the teeth are normal.
- Three basic types of amelogenesis imperfecta are recognized:
- Hypoplastic type in which there is defective formation of matrix.
- Hypocalcification (hypomineralization) in which there is defective mineralization of the formed matrix.
- Hypomaturation type in which enamel crystallites remain immature.
Clinical Features
- Hypoplastic type
- Enamel has not formed to full normal thickness on newly erupted teeth.
- Hypocalcified type
- Enamel is so soft that it can be removed by prophylaxis instrument.
- Hypomaturation type
- Enamel can be pierced by an explorer point under firm pressure of can be lost by chipping away from the underlying normal appearing dentin.
- Crowns of the teeth may or may not show discoloration. If present it varies between yellow to dark brown.
- It may have a chalky texture or a cheesy consistency. It may be chipped or show depressions.
Histologic Features
- There is a disturbance in the differentiation or viability of ameloblasts in the hypoplastic type and this is reflected in defects in matrix formation up to and including total absence of matrix.
- In hypocalcification type there are defects of matrix structure and mineral deposition.
- In hypomaturation type there are alterations in enamel rod and rod sheath structure.
Treatment
- Improvement of cosmetic appearance.
DENTINOGENESIS IMPERFECTA
(Hereditary opalescent dentin)
- Here the mesodermal portion of the odontogenic apparatus is disturbed.
Classification
- Type I: Occurs in families with osteogenesis imperfecta.It is an autosomal dominant trait with variable expressivity.
- Type II: Never occurs in association with osteogenesis imperfecta. Referred to as hereditary opalescent dentin.
- Type III: It is of Brandywine type. This is a racial isolate in Maryland.There is multiple pulp exposures in deciduous teeth.It is an autosomal dominant.
Clinical Features
- Color of teeth may range from a gray to brownish-violet or yellowish-brown.
- Exhibits a characteristic translucent or opalescent hue.
- There is an abnormal dentinoenamel junction and the scalloping is absent.
- Dentin undergoes rapid attrition and occlusal surfaces are severally flattened.
Radiological Features
- There is partial or total precocious obliteration of the pulp chambers and root canals by continued formation of dentin.
- Enamel is normal while dentin is thin and pulp chambers are enormous. This is shell teeth.
- Most of the teeth exhibit short roots.
Histologic Features
- There is purely a mesodermal disturbance.
- Dentin is composed of irregular tubules often with large areas of uncalcified matrix.
- Tubules tend to be larger in diameter.
- Pulp chamber is obliterated by the continued deposition of dentin.
- Odontoblasts degenerate readily becoming entrapped in the matrix.
Chemical and Physical Features
- Water content is greatly increased (60% above normal). Inorganic content is less than that of normal dentin.
Treatment
- Cast metal crowns on posterior teeth and jacket crowns on anterior teeth have been used.
DENTIN DYSPLASIA
(Rootless teeth)
- Rare disturbance of dentin formation characterized by normal pulpal morphology.Type I – Radicular dentin dysplasiaType II – Coronal dentin dysplasia.
Etiology
- Hereditary disease transmitted as an autosomal dominant characteristic.
Clinical Features
- Type I (Radicular): Both dentitions are affected. Teeth exhibit extreme mobility and are commonly exfoliated prematurely or after minor trauma.
- Type II (Coronal): Both dentitions are affected. Deciduous teeth have brown or bluish grey opalescent appearance.
Radiological Features
- Type I (Radicular): In both dentitions roots are short, blunt, conical and malformed, root canals are obliterated. Crescent shaped pulpal remanents may be seen in pulp chamber.
- Type II (Coronal): Exhibit an abnormally large pulp chamber in the coronal portion of the tooth offer described as thistle tube in shape.
Histologic Features
- Type I (Radicular): Apical to the coronal dentin is tubular dentin, most of which obliterates the pulp is calcified tubular dentin, osteodentin and fused denticles. New dentin forms around obstacles and shows an characteristic appearance as lava flowing around boulders.
- Type II (Coronal): Deciduous teeth exhibit amorphous and atubular dentin in the radicular portion. Coronal dentin is normal. Pulp has multiple pulp stones or denticles.
REGIONAL ODONTODYSPLASIA
(Odontogenesis imperfecta, ghost teeth, odontodysplasia, odontogenic dysplasia)
Etiology
- Local vascular defects are involved in the pathogenesis of the condition.
Clinical Features
- Delay or total failure in eruption.
- Shape is markedly altered, irregular in appearance with evidence of defective mineralization.
Radiological Features
- Marked reduction in radiodensity so that the teeth assume “ghost appearance”
- Enamel and dentin are thin and pulp chamber is large.
Histologic Features
- Marked reduction in amount of dentin, widening of predentin layer, presence of large areas of interglobular dentin and an irregular tubular pattern of dentin.
Treatment
- Extraction with restoration by prosthetic appliance.
DISTURBANCES OF GROWTH OF TEETH
- Deciduous teeth erupted into oral cavity seen in infants at birth. These are called natal teeth.
- Neonatal teeth are those teeth erupting prematurely in the first 30 days of life.
- Only 1 or 2 teeth erupt early most often deciduous and mandibular central incisors.
- In cases of endocine dysfunction (hyperthyroidism) cases it involves the entire dentition.
PREMATURE ERUPTION
- Deciduous teeth that have erupted into the oral cavity are occasionally seen in the infants at birth.
- These are called natal teeth in contrast with neonatal teeth which have been defined as those teeth erupting prematurely in the first 30 days of life.
- Most often the deciduous and mandibular central incisors are involved.
- Etiology of this phenomenon is unknown, although in some instances it follows a familial pattern. In case of the adrenogenital syndrome developing early in life, premature eruption of teeth is sometime seen.
- It has been pointed that premature erupted teeth are often well formed and normal in all respect except that they may be somewhat mobile. The premature eruption of permanent teeth is usually sequelae of the premature loss of deciduous teeth this is best demonstrated in the situation of single deciduous tooth has been loss, with subsequent of permanent tooth.
EMBEDDED AND IMPACTED TEETH
- Individual teeth which are unerupted usually because of lack of eruption force is called embedded teeth.
- Impacted teeth are those prevented from erupting by some physical barrier in the eruption teeth.
- Lack of space due to crowding of dental arches or the premature loss of deciduous teeth with subsequent partial closure of the area.
- Maxillary and mandibular third molars and maxillary cuspids are frequently impacted.
Winter's Classification of Mandibular third Molars
- Mesioangular impaction: Third molar lies obliquely in bone, crown pointing in a mesial direction, usually in contact with distal surface of the root or crown of the second molar.
- Vertical impaction: There is lack of space for eruption. It is prevented from erupting by impingement on the distal surface of IInd molar or the anterior border of ramus.
- Horizontal impaction: It is in horizontal position with respect to body of mandible.
- Crown may or may not be in contact with the distal surface of second molar.
- Completely impacted tooth is one which lies completely within the bone.
- Partially impacted tooth is not completely encased in bone but lies partially in soft tissue.
- This tooth creates an ideal situation for infection and even dental caries.
ANKYLOSED DECIDUOUS TEETH
(Submerged teeth)
- Are deciduous teeth, most commonly mandibular second molars that have a variable degree of root resorption and then have become ankyloses to the bone.
- This process presents exfoliation and subsequent replacement by permanent teeth.
- After the adjacent permanent teeth have erupted, the ankylosed tooth appears to have submerged below level of occlusion.
- Teeth affected lack mobility even though root resorption is far advanced.
- Upon percussion ankylosed tooth imparts characteristic solid sound in comparison to dull cushioned sound of normal tooth.
- Trauma, infection, disturbed local metabolism, or a genetic influence have been considered.
DEVELOPMENTAL CYST OF ORAL REGION
Nasolabial Cyst
Clinical Features
This may cause swelling in the mucolabial fold as well as in the floor of the nose, being located near the attachment of the ala over the maxilla.
Bilateral cases are rare.
This cyst probably originates from the lower anterior part of the nasolacrimal duct rather than from epithelium entrapped in the naso-optic furrow.
Histologic Features
May be lined by pseudostratified columnar epithelium which is sometimes ciliated, often with goblet cells or by stratified squamous epithelium.
Treatment
The cyst should be surgically excised although care must be taken to prevent perforation and collapse of the lesion.
Median Anterior Maxillary Cyst
(Nasopalatine duct cyst, incisive canal cyst)
- Most common type of maxillary developmental cyst.
- Arises from proliferation of epithelial remnants of the nasopalatine duct, an embryologic structure consisting of a duct or cord of epithelial cells lying within in the incisive canal.
Clinical Features
- Can occur at any age, even in the fetus.
- Discovered in the 4-6th decade.
- They are asymptomatic but become infected and produce pain and swelling and open by a tiny fistula on or near the palatine papilla.
Radiological Features
- Area appears to lie in the midline between the roots of maxillary central incisors and may cause separation or divergence of roots.
Histologic Features
- Lined by stratified squamous epithelium pseudostratified ciliated columnar epithelium, cuboidal epithelium or any combination.
- Connective tissue wall shows inflammatory cell infiltration.
Treatment
- Surgical excision not necessary.
Globulomaxillary Cyst
- The cyst actually forms in the bone suture between premaxilla and maxilla.
Clinical Features
- Cyst does become infected and the patient may complain of local discomfort or pain in the area.
Radiological Features
- Appears as an inverted pear shaped radiolucent area between the roots of lateral incisor and cuspid causing divergence of roots of these teeth.
Histologic Features
- Is lined by pseudostratified ciliated columnar epithelium remainder of wall is made up of fibrous connective tissue showing inflammatory cell infiltration.
Treatment
- Should be surgically removed, preserving adjacent teeth.
Palatal Cysts of the Neonate (Palatal and alveolar cysts of newborn)
(Epstein pearls, Bohn's nodules, gingival cyst of the newborn)
- Derived from epithelial remnants of developing palatal salivary glands.
- Found along the median raphae of the hard palate and appeared to be derived from entrapped epithelial remnants along the line of fusion.
- It may be found on alveolar ridges and is derived from remnants of dental lamina and is thus odontogenic in origin. This type is known as dental lamina cyst of newborn.
Clinical Features
- Appear as small, white, raised nodules, usually multiple measuring a fraction of a millimeter to 2 to 3 mm in diameter.
- They find to cluster along junction of hard and soft palate.
Histologic Features
- Lined by a thin, compressed layer of stratified squamous epithelium with the lumen generally packed with orthokeratin or parakeratin.
Treatment
- No treatment is necessary.
Thyroglossal Tract Cyst
- It is a developmental cyst which may form along the embryonic thyroglossal tract between foramen caecum of tongue and thyroid glands.
- Arises from remnants of this to act that do not become obliterated.
Clinical Features
- Usually occurs in young persons.
- Appears clinically as a firm, cystic, midline mass, varying in size from a few mm to several cm.
- Swelling develops slowly and is asymptomatic.
- If it is present high in the tract it causes dysphagia.
- Cyst may be present in the floor of the mouth near for a foramen caecum, in the floor of the mouth or inferiorly near thyroid or cricoid cartilage.
Histologic Features
- Thyroglossal tract cyst may be lined by stratified squamous epithelium ciliated type.
- The increased intracystic pressure causes cells become flattened.
- Connective tissue wall of the cyst contain small patches of lymphoid tissue, thyroid tissue and mucous glands.
Treatment
- Complete surgical excision.
EPIDERMOID AND DERMOID CYST
- It is a form of cyst, derived principally from embryonic germinal epithelium.
- These cysts are noted at the floor of the mouth and submaxillary and sublingual areas were common sites.
- Presumed to be derived from enclavement of epithelial debris in the midline during closure of the mandibular and hyoid branchial arches.
Clinical Features
- Arise in the floor of the mouth occur in young adulthood.
- Produces a bulge in the floor of the mouth often causing elevation of the tongue and ensuing difficulty in eating and talking if the cyst occurs above geniohyoid muscle.
- If the cyst is situated deeper between geniohyoid and mylohyoid muscles, bulging in submental area is common.
- The cyst has “doughlike” feel to palpation but may be more fluctuant.
- The cyst sometimes becomes infected and develops sinus tracts opening intraorally.
- They may undergo malignant transformation.
Histologic Features
- These cysts are composed only of connective tissue wall lined on the inner surface by a thin layer of stratified squamous epithelium usually showing keratinization.
- Lumen may actually be filled with keratin.
- There may be numerous sebaceous glands and even hair follicles in addition to sweat glands.
- Lumen contains sebaceous material as well as keratin.
Treatment
- Should be removed surgically.
Benign Cervical Lymphoepithelial Cyst
(branchial cleft cyst, lateral cervical cyst, benign cystic lymph node)
- Is a cyst which occurs on the lateral aspect of the neck and is originating from remnants of the branchial arches or pharyngeal pouches.
- This cyst originates through cystic transformation of epithelium entrapped in cervical lymph nodes.
Clinical Features
- Occur in young adult.
- Many cysts occur in neck, angle of mandible, submandibular area and even in preauricular and parotid areas.
Histologic Features
- Lined by stratified squamous epithelium may contain some pseudostratified columnar epithelium.
- Wall of the cyst exhibits lymphoid tissue with a typical lymphnode pattern.
- Cyst may contain thin watery fluid or a thick gelatinous, mucoid material.
Treatment
- Treated by surgical removal.
- Recurrence results, if residual remnants are left or if the lesion is simply aspirated.
- It might develop into a carcinoma.