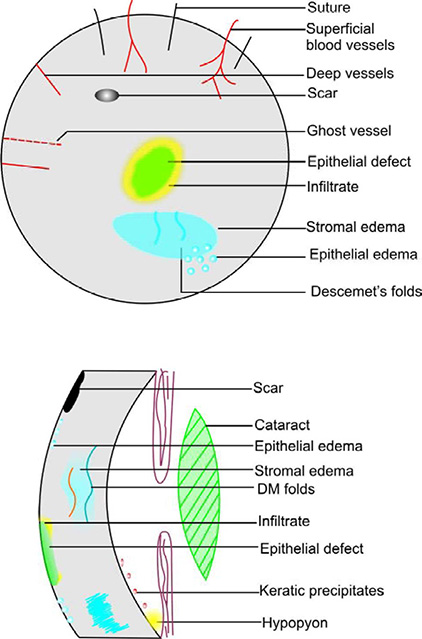
CORNEAL COLOR CODING
Scars | Black |
Degenerations | Black |
Contact lens | Black dotted circle |
Sutures | Black straight lines |
Cornea! outline | Black |
IOL | Black |
Guttata | Black shade |
Deep blood vessels | Dark red, straight lines ending at limbus |
Superficial blood vessels | Bright red, wavy branching lines crossing limbus |
Ghost vessels | Red dotted straight lines |
Hyphema | Red |
Rose Bengal stain | Red |
Pterygium | Red |
Epithelial edema | Blue circles |
Descemet's folds | Blue wavy lines |
Stromal edema | Blue shadows |
Lens | Green |
Vitreous | Green |
Corneal filaments | Green |
Fluorescein stain | Green |
Epithelial defect | Green |
Infiltrates | Yellow |
Hypopyon | Yellow |
Iris | Brown |
Pigment | Brown |
Keratic precipitates | Brown |
BACTERIAL KERATITIS
PREDISPOSING FACTORS
- Contact lens wear may cause epithelial defects; predispose to Pseudomonas aeruginosa infection
- Pre-existing corneal disease - trauma, bullous keratopathy, exposure keratopathy, decreased corneal sensation
- Chronic blepharitis; chronic dacryocystitis
- Tear film deficiency; topical steroid usage; Vitamin A deficiency.
CLINICAL FEATURES
- Pain, photophobia, redness, foreign body sensation, lid edema, discharge
- Circum-corneal congestion
- Sharp epithelial demarcation with underlying dense suppurative stromal inflammation, surrounded by stromal edema
- Epithelial defect surrounded by infiltrate
- Endothelial inflammatory plaque
- Anterior uveitis with hypopyon
- P. aeruginosa produces stromal necrosis with a shaggy surface and adherent mucopurulent exudate
- Corneal perforation is a complication.
The pneumonic PEDAL is used for infectious keratitis; P – pain; E – epithelial defects; D – discharge; A–AC reaction; L – location.
Stains & culture media for microbial keratitis
SUSPECTED ORGANISM | STAIN | MEDIA |
|---|---|---|
Aerobic bacteria | 1. Gram 2. Acridine orange | 1. Blood agar 2. Chocolate agar 3. Thioglycollate broth |
Anaerobic bacteria | 1. Gram stain 2. Acridine orange | 1. Anaerobic blood agar 2. Phenylethyl alcohol agar in anaerobic chamber |
Mycobacteria | 1. Gram 2. Acid fast 3. Lectin | 1. Blood agar 2. Lowenstein-Jensen medium |
Fungi | 1. Gram 2. Acridine orange 3. Calcofluor white | 1. Blood agar (25°) 2. Sabouraud agar 3. Brain-heart infusion (25°) |
Acanthamoeba | 1. Acridine orange 2. Calcofluor white | 1. Non-nutrient agar with E. coli overlay 2. Blood agar 3. Buffered charcoal-yeast extract agar |
GRAM's STAINING
[Gram +ve stains purple; gram -ve stains pink]
1. Heat fix the slide ® 2. flood with crystal violet [1 min]
6. Decolorize with Acetone: Alcohol sol. [in 1:1 ratio]
GIEMSA STAINING
ACID FAST STAINING
[stains typical and atypical mycobacteria]
KOH MOUNT
A drop of 10% KOH is placed on the slide with the corneal scraping; a cover slip is placed over it; Fungal elements are looked for under the microscope.
TREATMENT
- In the form of broad spectrum topical antibiotics
- Oral ciprofloxacin 750 mg BD in juxta-limbal keratitis
- Atropine 3% ointment BD - to prevent posterior synechiae and decrease pain from ciliary spasm.
Antibiotics used in bacterial keratitis
ORGANISM | ANTIBIOTIC | TOPICAL DOSE |
|---|---|---|
GP cocci | Cefazolin Vancomycin | 50 mg/ml 50 mg/ml |
GN rods | Tobramycin Gentamicin Ceftazidime Fluoroquinolones | 9-14 mg/ml 15 mg/ml 50 mg/ml 3 mg/ml |
No/multiple organisms | Cefazolin + Gentamicin (or) Fluoroquinolones | 50 mg/ml 15 mg/ml 3 mg/ml |
GN cocci | Ceftriaxone Ceftazidime | 50 mg/ml 50 mg/ml |
Mycobacteria | Amikacin | 20 mg/ml |
* GP = gram positive | ||
* GN = gram negative | ||
Preparation of fortified topical medication
DRUG | VIAL STRENGTH | HOW TO PREPARE |
|---|---|---|
Cefazolin [50 rag/ml] | 1 vial = 500 mg | Add 10 ml of AT to vial |
Ceftazidime [50 rag/ml] | 1 vial = 500 mg | Add 10 ml of AT to vial |
Vancomycin [50 rag/ml] | 1 vial = 500 mg | Add 10 ml of AT to vial |
Gentamicin [15 mg/ml] | 1 vial = 2 ml [40 mg/ml] | Add 2 ml from vial to 5 ml of 0.3% gentamicin eye drops |
* AT = preservative free artificial tears | ||
KERATOMYCOSIS
CAUSED BY
- Filamentary fungi - Fusarium sp., Aspergillus sp
- Yeasts - Candida species (immunocompromised individuals; pre-existing corneal disease).
PATHOGENECITY
- Hyphae grow along stromal collagen fibers
- Ineffective phagocytosis by host immune system because hyphae are large - instead digestion of host cells occurs
- Immunosuppression increases fungal growth
- Fungi enter anterior chamber by penetrating intact Descemet's membrane.
EPIDEMIOLOGY
- Trivial injury with organic matter
- Windy and dry season; rural areas
- Agriculturists are more prone.
CLINICAL FEATURES
- Signs >>> symptoms
- Gradual onset, foreign body sensation, photophobia, blurred vision, discharge
- Slow progression, less painful.
Candida keratitis
- Yellow-white ulcer with dense suppuration
Filamentous Keratitis
- Gray stromal infiltrate with a dry texture and indistinct margins
- Surrounding satellite lesions
- Feathery finger-like lesions
- Immune ring infiltrates (Wessely ring)
- Endothelial plaque
- Hypopyon - thick and immobile - due to direct invasion of hyphae enmeshed in thick exudatesRx:
- Topical natamycin 5%,
- Topical amphotericin B 0.15%
- Oral ketoconazole 200 – 600 mg/day if severe
INVESTIGATIONS
- KOH mount – KOH dissolves epithelial cell walls; hyphae become visible
- Culture media – Sabouraud's dextrose agar, Potato dextrose agar
TREATMENT
- Topical antifungals up to 6 weeks
- Cycloplegics
- Hypotensive agents
- Systemic antifungals [oral fluconazole 150 mg BD; if severe or if endophthalmitis occurs]
ACANTHAMOEBA KERATITIS
- Caused by a ubiquitous free-living protozoan
- Cysts become trophozoites which produce enzymes ♦ tissue penetration and destruction
- Contact lens wearers at particular risk.
CLINICAL FEATURES
- Severe pain, blurred vision
- Symptoms >> signs
- Photophobia, foreign body sensation
- Conjunctival injection, chemosis
- Stromal ring infiltrate ♦ ring abscess - may be central/ paracentral
- Radial keratoneuritis - perineural infiltrates
- Sub-epithelial keratopathy
- Endothelial plaque, hypopyon
- Frank corneal necrosis
- Pseudo-dendritic keratitis
- Small white satellite lesions
- Slowly progressive stromal opacification; descemetocele
- Scleritis
INVESTIGATIONS
- 10% KOH mount - amebic cysts are seen
- Calcofluor white - a chemofluorescent dye with special affinity for acanthamoeba cysts
- Gram's stain, Giemsa stain, Periodic Acid Schiff
- Culture on non-nutrient agar with E. coli overlay; buffered charcoal yeast extract.
TREATMENT
TOPICAL
- PHMB (polyhexamethylene biguanide) 0.02% + Propamidine isothionate (brolene) 0.1%
- Chlorhexidine [monotherapy]
- Neomycin + broleneAlso used are:
- Miconazole 1%
- Clotrimazole 1%
- Dipropamidine isothionate 0.15%
ORAL: Ketoconazole [optional]
SURGERY: Therapeutic penetrating keratoplasty
INTERSTITIAL KERATITIS
- Non-ulcerative, non-suppurative inflammation of corneal stroma, often with subsequent vascularization
CAUSES
- Congenital/acquired syphilis (90%)
- TB, leprosy, Lyme disease
- HSV, HZV, mumps, influenza, rubella
- Chromium deficiency, gold toxicity
- Onchocercariasis, cysticercosis, infectious mononucleosis
- Malaria, leishmaniasis, trypanosomiasis
CLINICAL FEATURES
- PROGRESSIVE STAGE [from 1-2 weeks]
- Pain, photophobia, lacrimation, blepharospasm
- Circum-corneal congestion, cloudy cornea
- Superficial peripheral vascularization
- Anterior uveitis, choroiditis
- Limbitis - raised inflamed sector of limbus from which deep blood vessels invade
- FLORID STAGE [from 2-4 months]
- increased inflammation, DM folds
- deep vascularization
- ground glass cornea - diffuse stromal cellular infiltration
- Salmon patch - corneal clouding obscures the outline of the vessels — looks dull, pinkish red
- REGRESSIVE STAGE [from 1-2 years]
- clearing starts
- blood vessels become non-perfused ♦ GHOST VESSELS - may refill later following inflammation - bleeding occurs
- stromal thinning, scarring, flattening
COMPLICATIONS
- corneal decompensation, corneal guttata
- band keratopathy, lipid keratopathy
- Salzmann nodular degeneration, astigmatism
- glaucoma
TREATMENT
- Topical steroids - to reduce corneal inflammation and iritis
- Penicillin G given in ♦
- Primary and secondary syphilis ♦ 1.2 million units i.m
- Tertiary syphilis ♦ 2.4 million units i.m weekly × 3 wks
- Penetrating keratoplasty - for corneal scarring
HERPES SIMPLEX KERATITIS
EPITHELIAL KERATITIS
- present with watering, discomfort, decreased vision, pain
- opaque epithelial cells break down to form linear, branching, dendritic ulcer with terminal bulbs (ulcer bed stains with fluorescein; margin stains with Rose Bengal)
- centrifugal enlargement ♦ geographical/ameboid ulcer
- decreased corneal sensation
Rx:
- debridement of dendritic (not geographic) ulcer
- acyclovir ointment 3% (5 times per day); check for response in a week; if no response, change the antiviral agent to -
- trifluorothymidine 1% (6 X/day) or
- ganciclovir gel 0.15% (5 X/day) [5 times per day]
* Low dose oral acyclovir [400 mg bd for 1 yr] reduces the rate of recurrent herpetic eye disease; this is indicated in patients prone to frequent recurrences
DISCIFORM KERATITIS
Possible Etiologies
- exaggerated hypersensitivity reaction to viral antigens
- infection of keratocytes and endothelium
Clinical Features
- gradual onset of blurred vision and haloes; no pain
- central, disc-like zone of epithelial edema overlying an area of stromal thickening, with KPs and DM folds
- ring of stromal precipitates - WESSELY RING ♦ marks the junction between viral antigen and host antibody
- mild anterior uveitis; raised IOP
- decreased corneal sensation
- Topical prednisolone acetate 1% + antiviral cover initially [if steroids used > 4 times/day]
- If topical prednisolone acetate 0.25% used - no need for antiviral cover
- Gradually taper steroids over several weeks
STROMAL NECROTIC KERATITIS
- active viral invasion and tissue necrosis
- can have an intact epithelium or epithelial disease
- cheesy/necrotic stroma
- profound interstitial opacification
- anterior uveitis, KPs
- scarring, vascularization, lipid keratopathy, perforation
Eye disease caused by Herpes simplex virus and Varicella zoster virus
HERPES SIMPLEX | VARICELLA-ZOSTER | |
|---|---|---|
Dermatomal distribution | Incomplete | Complete |
Pain | Less | More |
Dendrites | Large with central ulceration and terminal bulbs | Small, medusa-like dendrites without central ulceration or terminal bulbs |
Dendritic mucous plaques | Don't occur | Occur late |
Skin scarring | Rare | Frequent |
Postherpetic neuralgia | Rare | Common |
Iris atrophy | Patchy | Sectoral |
Bilateral involvement | Rare | Never |
Recurrent lyric epithelial keratitis | Common | Never |
Corneal hypoesthesia | Sectoral/diffuse | Frequent |
KERATOCONUS
- Non-inflammatory ectasia of cornea resulting in visual impairment, owing to a high degree of irregular myopic astigmatism
- Adolescence; bilateral/unilateral
THEORIES
- Developmental delay in separation of lens fibers from cornea
- Degeneration of elastic fibers
- Secondary to disease process or malnutrition
- Endocrinological - because of association with hypothyroidism and pregnancy
SYMPTOMS
- Decreased visual acuity; ghost images; glare
- Can present with irritation and frequent rubbing of the eye
SIGNS
- Central/eccentric cone
- Fleischer ring - a line running along the base of the cone due to iron deposition superficial to the Bowman's membrane (complete/incomplete; pigmented/yellow/brown)
- Prominent corneal nerves
- Stromal thinning increases gradually from base of the cone to the apex
- Vogt's striae - thin vertical stress lines in the deeper stroma which disappear on digital pressure
- Endothelial reflex because of increased concavity
- Acute Hydrops - in the center of the cone due to rupture of the descemet's membrane and influx of fluid into the stroma
- Scarring following rupture
- Munson sign - on looking down, the angular curve is assumed by the lower lid margin
- Axenfeld sign - loss of sensitivity at the apex of the cone
- Benedict sign - conical reflection on the nasal cornea when torch light thrown from temporal side
INVESTIGATIONS
- Keratometry - non-alignment of the mires
- breaking/doubling of the right lower circle.
- Placido's disc - irregularities in reflection of illuminated rings near the corneal center; distortion of the horizontal axis
- Direct ophthalmoscopy - oil drop sign
- Retinoscopy - scissors reflex; 2 shadows move in opposite direction
- Orbscan detects early keratoconus; bow-tie pattern; called Forme Frustae keratoconus
OCULAR ASSOCIATIONS
- Vernal keratoconjunctivitis, atopic keratoconjunctivitis [due to constant rubbing of eye]
- Retinitis pigmentosa; Leber's congenital amaurosis
- Retrolental fibroplasia
- Macular coloboma
- Ectopia lentis, blue sclera
- Cataract, retinal detachment, optic atrophy
- Xeroderma pigmentosa
- Addison's disease
- Syndromes - Down's, Ehlers-Danlos, Marian's, Crouzon's, Apert's.
DIFFERENTIAL DIAGNOSIS
KERATOCONUS | KERATOGLOBUS | PELLUCID MARGINAL DEGN |
|---|---|---|
Most common | Rare | Less common |
Bilateral [usually] | Bilateral | Bilateral |
Onset at puberty | Onset at birth | 20 – 40 years |
Inferior paracentral thinning | Thinning greatest in periphery | 1-2 mm band of thinning inferiorly |
Protrusion at apex | Generalized protrusion | Protrusion superior to band of thinning |
Fleischer ring present | Absent | Sometimes present |
Scarring common | Mild scarring | Only after hydrops |
Striae are common | Sometimes | Sometimes |
* DEGN - degeneration | ||
TREATMENT
- Spectacles
- Contact lenses - RGP [rigid gas permeable]
- Gas-permeable with large diameter - for oval/globus cones
- Aspherical - for nipple cones
- Small, steep lenses - for severe nipple cones
- Semi-rigid/hard - for steep oval cones
- Piggy bag lenses
- Scleral contact lenses [Boston lenses]
- Surgery -
- Anterior lamellar keratoplasty
- Epikeratoplasty
- Deep lamellar keratoplasty
- Penetrating keratoplasty (use same sized donor button)
- Thermokeratoplasty - heat is applied to the tip of the cornea for 1 min which causes shrinkage of collagen and flattening of the cornea
- Intacts [intra-stromal rings]
- Rx of acute hydrops:
- hypertonic saline drops
- C3F8 (14%) injection into the anterior chamber
POSTERIOR KERATOCONUS
- Increased curvature of the posterior corneal surface with normal curvature of the anterior corneal surface
- May be focal/generalized; central/eccentric
- Unilateral; present from birth
- Associated with posterior corneal opacity, anterior lenticonus, aniridia, iris atrophy, ectropion uveae
- Amblyopia and strabismus may be present
- Associated features: hypertelorism, webbed neck, short stature, mental retardation, abnormal development of bridge of the nose
CORNEAL DYSTROPHIES
- A dystrophy is a bilateral, symmetric, inherited condition that appears to have little or no relationship to environmental or systemic factors.DegenerationDystrophyOpacity often peripheralCentral opacityMay be asymmetricBilateral and symmetricPresents later in lifePresents early in lifeAssociated with agingHereditaryProgression can he very slow or rapidProgression usually slow
- Cogan microcystic/epithelial basement membrane/map-dot-fingerprint dystrophy
- dot-like opacities; epithelial microcysts
- map-like patterns; whorled fingerprint-like lines
- not familial/progressive
- cause recurrent bilateral corneal erosions
- Meesmann dystrophy - tiny intraepithelial cysts in the interpalpebral area; do not reach limbus
- Reis-Buckler dystrophy - gray-white, round and polygonal opacities in the center of the cornea; decreased corneal sensation; visual disturbance due to scarring
- Thiel Behnke dystrophy - similar to Reis-Buckler type; opacities for a honey-comb pattern
- Crystalline dystrophy - scintillating subepithelial crystalline opacities in the center of a generally hazy cornea
- Lattice type 1 - fine, spidery, branching lattice lines spreading outward, sparing the periphery
- Lattice type 2 - short, fine, sparse lattice lines; associated with progressive bilateral cranial and peripheral neuropathies
- Lattice type 3 - thick ropy lines from limbus to limbus with minimal intervening haze
- Granular - small, white, crumb-like deposits in the central anterior stroma; not reaching limbus
- Avellino - fine ring /disc-like opacities [dense centrally] with deep linear opacities
- Macular - grey-white, dense, focal, poorly delineated spots with diffuse stromal clouding; eventually full thickness stroma is involved with stromal thinning
- Gelatinous - in familial sub-epithelial amyloidosis; grey sub-epithelial nodules giving a mulberry - like appearance; presents with photophobia, watering, decreased vision
- Fuch's endothelial dystrophy–
- Middle-aged women
- Increased incidence of POAG
- Central corneal guttata which spread to the periphery
- Blurred vision especially in the morning which clears during the dayStage I - cornea has a beaten metal appearanceStage II - endothelial decompensation leads to stromal edemaStage III - epithelial edema leading to bullous KeratopathyRx - Topical NaCl; bandage contact lens; PKP
- Posterior polymorphous dystrophy–
- Endothelium displays features of epithelium
- Vesicular/band-like/geographical endothelial patterns
- Associated with peripheral anterior synechiae, glaucoma, ectropion uveae
- Congenital Hereditary Endothelial Dystrophy
- Focal/generalized absence of endothelium
- Diffuse bilateral comeal edema
- Blue grey/ground glass appearance/total opacification
- D/D - birth trauma, buphthalmos, sclerocornea.
TREATMENT
- Observation till asymptomatic or manageable vision
- PKP when vision deteriorates
THERAPEUTIC CONTACT LENS
USES
- Optical -
- irregular astigmatism e.g. Keratoconus
- superficial corneal irregularities
- anisometropia for binocular single vision
- Promote epithelial healing -
- persistent epithelial defects
- recurrent corneal erosions
- Pain relief -
- bullous keratopathy
- wet filamentary keratitis
- trichiasis
- Thygeson's SPK
- Preservation of corneal integrity -
- descemetocele
- corneal wound apposition
- Miscellaneous -
- ptosis props to support the upper lid in patients with ocular myopathies
- prevent symblepharon in eyes with cicatrizing conjunctivitis
- drug delivery [hydrogel lenses soaked in topical medication]
COMPLICATIONS OF CONTACT LENS USE
- Conjunctival -
- Allergic conjunctivitis - perilimbal injection, fine papillary conjunctival reaction
- Giant papillary conjunctivitis - increased mucus, Trantas dots, limbitis
CORNEAL DEGENERATIONS
Degeneration of a tissue is a physiological decomposition of tissue elements and deterioration of tissue functions; it is distinguished from dystrophies in being non-hereditary and usually unilateral
- AGE RELATED:
- Arcus senilis -
- occurs hi elderly individuals
- a ring of lipid deposition in the peripheral cornea [1 mm band]
- separated from the limbus by a clear zone
- also seen in Type II hyperlipoproteinemia [presents early]
- usually bilateral; unilateral in ocular hypotony and carotid artery disease
- Vogt white limbal girdle -
- narrow bilateral crescentic lines
- chalk-like flecks in the interpalpebral fissure along the nasal and temporal limbus
- Cornea farinata -
- bilateral minute flour-like deposits in the deep stroma
- Crocodile shagreen -
- grayish white, polygonal stromal opacities separated by relatively clear spaces
- in the anterior 1/3 or posterior 2/3
- Corneal guttata -
- focal accumulation of collagen on the posterior surface of the descemet's membrane
- warts or excrescences in the center of the cornea
- called Hassal-Henle bodies if in the periphery
- LIPID KERATOPATHY:
- Primary - occurs spontaneously in an avascular cornea
- Secondary - occurs following previous ocular disease/ injury which results in vascularization
- Yellowish stromal deposits of cholesterol, fats, Phospholipids occurs
- If associated with corneal vascularization, it is progressiveRx-
- control underlying disease [inflammation or vascularization]
- argon laser photocoagulation to arterial feeder vessels
- needle point cautery to feeder vessels
- PKP if severe
- BAND KERATOPATHY:
- Deposition of calcium salts in the sub-epithelial space and anterior portion of the Bowman membrane
Causes:- Ocular
- chronic anterior uveitis
- interstitial keratitis, severe superficial keratitis
- phthisis bulbi
- silicon oil instillation in an aphakic eye
- Age related band keratopathy
- Metabolic
- hypercalcemia caused by hyperparathyroidism, Vitamin D toxicity, milk-alkali syndrome, sarcoidosis
- hyperphosphatemia with normal serum calcium [in some renal failure patients]
- Hereditary transmission ♦ primary hereditary band keratopathy
Clinical Features- Peripheral interpalpebral calcification separated from the limbus by a clear zone
- Gradual central spread ♦ band like chalky plaque
- Nodular elevated lesions in advanced stages
- Discomfort due to epithelial breakdownRx-
- Chelation with a neutral solution of EDTA (sodium edetate) 150 mg/ml after large chips of calcium are removed with forceps and the epithelium is scraped off [mix a 20 ml vial with 100 ml of sterile ophthalmic irrigation solution and warm it]
- Excimer laser keratectomy
- SPHEROIDAL DEGENERATION
- Also called corneal elastosis; Labrador keratopathy; climatic droplet keratopathy [due to increased exposure to UV light]
- Amber-colored spheroidal granules in the superficial stroma, in the interpalpebral strip
Rx-- corneal epithelial debridement
- superficial keratectomy
- SALZMANN NODULAR DEGENERATION
- Secondary to chronic keratitis as in trachoma, phlyctenulosis
- discrete, elevated, gray superficial lesions
- stromal opacities form nodules which elevate the epithelium
- located over scarred cornea or at the edge of a scar in a clear cornea
Rx-- superficial keratectomy or debridement
CORNEAL VASCULARIZATION
ETIOPATHOGENESIS
- Traumatic/inflammatory/toxic/nutritional insult ♦ causes blood vessels to gain access into a swollen and edematous tissue
- The normally present vasoinhibitory factors are abolished in pathological state
CLASSIFICATION
- Superficial vascularization–
- Originates from the superficial limbal plexus
- From branches of anterior ciliary arteries
- Confined to a segment or extend around the limbus
- Preceded by edema, exudation or epithelial disturbance
- When extensive - called pannus
- Interstitial vascularization–
- Straight non-anastomozing blood vessels from anterior ciliary arteries
- Seem to disappear from view
- Invade the cornea at the level of the pathological process
- Deep vascularization–
- Retrocorneal pannus
- Proliferation of deep blood vessels by budding from anterior ciliary arteries
TREATMENT
- Radiation ♦ given at the onset of superficial vascularization; obliterative end arteries develop due to trauma to the endothelium
- Peritomy is done 3-4 mm from limbus
- Argon laser photocoagulation
- Sodium chromoglycate 4% drops
- Superficial keratectomy or PKP
PANNUS
- Inflammatory or degenerative in growth of fibrovascular tissue from the limbus
- Growth of tissue between epithelium and Bowman's layer
- An inflammatory pannus disrupts the Bowman's layer; a degenerative pannus leaves it intact
STAGES OF PANNUS
- Infiltration - superficial corneal layers are infiltrated by polymorphonuclear leucocytes (PMNs) and lymphocytes
- Progressive - new vessels emerge from the limbal plexus to form a grey vascular mass beneath the epithelium
- Stationary - resolution of exudates followed by shrinkage of blood vessels
- Sclerotic - cicatricial tissue or obliterated remnants of blood vessels
TYPES OF PANNUS
- Progressive - a leash of vessels in front of which there is a zone of infiltration and haziness
- Regressive - vessels extend beyond the area of infiltrated cornea
DIFFERENTIAL DIAGNOSIS
- Superior limbic keratoconjunctivitis; phlyctenulosis
- Vernal keratoconjunctivitis; atopic conjunctivitis
- Herpes simplex keratitis; trachoma
- Contact lens wear; toxic/chemical keratitis
MOOREN'S ULCER
- Chronic painful peripheral corneal ulceration (serpigenous ulcer) progressing circumferentially and centrally
- Infection or collagen vascular disease is absent
POSSIBLE ETIOLOGY
- autoimmune reaction
- helminthiasis
- chronic hepatitis C
- corneal injury; surgery; burns
- HSV/HZV
CLINICAL FEATURES
- Pain, photophobia, lacrimation
- Decreased vision, blepharospasm
- Starts as a peripheral infiltration in the interpalpebral fissure area near the limbus
- Marginal furrow ulcer with overhanging edge and sloping peripheral border
- The infiltration breaks into a circumferential ulcer
TYPES
Type 1 | Type 2 | |
|---|---|---|
Prevalence | Common form | Atypical form |
Pathogenic factors | Trauma | Trauma, helminthiasis |
Age | > 40 years | 20-30 years |
Sex | Female > male | Male > female |
Pain | Moderate - severe | Variable |
Course | Slowly progressive | Rapid |
Response to treatment | Moderate | Poor |
Perforation | Rare | In 1/3 of cases |
Laterality | 75% unilateral | 75% bilateral |
INVESTIGATIONS
To rule out systemic association
- Total count/differential count; platelet count; ESR; Hemoglobin%
- Rheumatoid factor; ANA; pANCA; cANCA
TREATMENT
- Topical steroids; oral steroids
- Topical cycloplegics
- Bandage contact lens
- Peritomy - resection of 4 mm perilimbal conjunctiva adjacent to the ulcer
- Lamellar corneal transplant and conjunctival flaps
- Systemic immunosuppressives
- Glue if corneal perforation
- PKP - if extreme peripheral corneal thinning
BULLOUS KERATOPATHY
SYMPTOMS
Poor vision, haloes around light bulbs, pain, photophobia, foreign body sensation
CAUSES
- Endothelial damage during cataract surgery
- Pseudophakic bullous keratopathy due to AC IOL touching endothelium or raised IOP following surgery
- Aphakic bullous keratopathy due to vitreous in anterior chamber, which touches the endothelium
- Congenital Hereditary Endothelial Dystrophy (CHED)
- Fuch's endothelial dystrophy
- Posterior polymorphous dystrophy
- Chandler syndrome (ICE syndrome)
- Acute angle closure glaucoma
- Herpetic disciform keratitis
- Corneal transplant rejection
Prevention of corneal edema following cataract surgery:
- Choose the type of cataract surgery depending on the type of cataract (phacoemulsification for a hard cataract will cause more endothelial damage)
- Use viscoelastics liberally during surgery - to protect endothelium from instrument touch
- Wash out all viscoelastic at the end of surgery to prevent post-operative rise of IOP
- Try to avoid the use of AC lOLs if there already is endothelial compromise
- Look for cornea guttata and Fuch's endothelial dystrophy in pre-operative evaluation ♦ in which case use BSS (balanced salt solution) or sodium hyaluronate
TREATMENT OF BULLOUS KERATOPATHY
- Hypertonic saline 5% eye drops or 6% eye ointment [draw out water from the cornea by osmosis]
- A thin, high water content bandage contact lens - for pain relief
- Control IOP if it is high
- Remove AC lOLs and iris-clipped if they are the cause for bullous keratopathy
- Anterior stromal puncture ♦ with a 25-g needle, multiple small superficial punctures are made in the cornea, at/below Bowman's layer; place bandage contact lens for 1-2 weeks to allow the epithelium to adhere to cornea
- Excimer laser phototherapeutic keratectomy
- Penetrating keratoplasty
CORNEAL TRANSPLANT
TYPES
- Optical - for visual rehabilitation
- Tectonic - for re-enforcing altered corneal structure (descemetocele)
- Therapeutic - tissue substitution for refractory corneal disease (corneal ulcer)
COMMON INDICATIONS
- Keratoconus with apical scarring; rapid progression
- Aphakic/pseudophakic bullous keratopathy
- Corneal scarring
- Fuch's endothelial dystrophy
- Failed graft ♦ primary graft failure; graft rejection/infection
- Herpes simplex keratitis causing stromal necrosis
- Ocular trauma - normal posterior segment
- Congenital corneal opacities — Peter's anomaly, sclerocornea
- Stevens-Johnson syndrome
- Corneal dystrophies
- Chemical burns
CONTRAINDICATIONS: (Donor Cornea)
ABSOLUTE | RELATIVE |
|---|---|
– Death of unknown cause – AIDS, rabies – Hepatitis, septicemia – CMV encephalitis – Congenital rubella – Reye's syndrome – Leukemia – Hodgkin's disease – Intrinsic eye disease – Creutzfeldt-Jakob disease | – Multiple sclerosis – Parkinsonism – Syphilis – Chronic lymphocytic leukemia – Chronic immunosuppression |
DONOR TISSUE EVALUATION
- Epithelium - edema, abrasions, foreign body
- Stroma - edema, DM folds
- Breaks in DM
- Endothelium - specular microscopy
DONOR CORNEA PRESERVATION
- Short term storage - Moist chamber technique
- Whole globe preservation at 4°C with saline humidification for up to 48 hrs
- Disadvantages: endothelium undergoes autolysis; difficult to screen for HIV and HBsAg; HLA typing can't be done in aqueous environment
- Intermediate term storage media (2 wks)MKMCSEMCSMDMOMK-SOLTC199++--++HEPES+-++++Dextran+--++-Chondroitin sulphate-+++++Gentamicin sulphate--++++NEAA--+++-MEM--+++-Mercaptoethanol--++--Sodium bicarbonate----+-Sodium pyruvate----+-
- Storage up to 2 weeks
- MKM = Mc-Carey Kaufman Medium
- In modified MK medium, 0.025 M of HEPES is used instead of bicarbonate buffer
- CSEM = chondroitin sulphate enriched medium
- CSM = corneal storage medium
- DM = dexsol medium
- OM = optisol medium
- K-SOL = K sol medium
- NEAA = non-essential amino acids
- MEM = minimum essential medium
- TC 99 = Technichium 99
- Long Term Storage1. Organ Culture MethodEagle's MEM + Earle's Salts + L-Glutamine + Decomplemented Calf Serum is used
- Stored at 34°C for 35 days, endothelial side up
- If no growth after 10 days in any microbiological medium - cornea is fit for transplant
2. Cryopreservation- Can preserve indefinitely
- Corneo-scleral button passed through a series of solutions containing increasing concentration of DSMO (Dimethyl sulphoxide) up to 7.5%
- Placed in each solution for 10 min.
- Frozen up to −80°C; stored at −160°C
- Disadvantages are - Intracellular microcrystal formation; number of endothelial cells decreases
- Used for lamellar transplant
COMPLICATIONS OF PENETRATING KERATOPLASTY
EARLY COMPLICATIONS
- PRIMARY GRAFT FAILURE
- Irreversible graft edema in immediate post-op period
- No period of graft clarity
- Due to endothelial damage
- Donor tissue with endothelial cell count < 1500/mm3
- Improper preservation
- Trauma during surgery, stretching of cornea; shallowing of AC; instrument touch
- GLAUCOMA
- Acute rise in IOP, with/without optic nerve damage or field loss
Causes:- retention of visco-elastic
- angle closure
- distortion of Trabecular Meshwork
- inflammation
- steroid induced
- EPITHELIAL DEFECTS
- Increased chance of rejection, infection, ulceration, perforation
Causes:- Storage
- Injury during surgery
- Post-operative lid movement
- Trichiasis
INTERMEDIATE COMPLICATIONS
- GRAFT REJECTION
- Epithelial rejection:
- elevated rejection line which stains with fluorescein/Rose Bengal
- represents zone of destruction of donor epithelial cells
- occurs usually 3 months following surgery
- Stromal rejection:
- sudden onset of peripheral full thickness haze with circum-corneal congestion
- Associated with endothelial rejection
- Endothelial rejection:
- Khoudadoust line
- diffuse KPs
- linear arrangement of endothelial precipitates
- edematous cornea
Risk factors for rejection -- Vascularization
- Previous graft failure
- Large, eccentric, bilateral grafts
- Younger patients
Treatment of graft rejection -- Topical hourly steroids
- Systemic steroids
- In severe rejection, pulsed I.V. methyl prednisolone followed by oral prednisolone
- GRAFT INFECTION:
- bacterial, viral, fungal, acanthamoebic infection
- due to steroid usage
- Infectious crystalline keratopathy - caused by Streptococcus viridans
- WOUND DEHISCENCE:
- following high IOP, early suture removal or trauma
LATE COMPLICATIONS
- recurrence of disease - especially herpetic keratitis and corneal dystrophies
- late graft failure ♦ decompensation due to decreased endothelial cells
- astigmatism if donor button is slightly larger
LAMELLAR KERATOPLASTY
- Partial thickness graft of cornea
- Anterior lamellar and deep lamellar keratoplasty
INDICATIONS
- Corneal opacity involving superficial 1/3 of stroma, not caused by recurrent disease
- Marginal corneal thinning e.g. pterygium, Terrien marginal degeneration, limbal dermoids
- Localized thinning or descemetocele
- Keratoconus
DEEP LAMELLAR KERATOPLASTY
- All opaque corneal tissue is removed to the descemet's membrane level
- Endothelium is not transplanted – so less chances of rejection
Indications:
- Disease involving anterior 95% of corneal thickness with endothelium being normal and no breaks/scars in descemet's membrane
- Chronic inflammatory disease like atopic keratoconjunctivitis
Advantages:
- Less astigmatism
- Structurally stronger globe
- No risk of endothelial rejection
- Increased availability of graft material
Complications:
- Corneal perforation during dissection
REFRACTIVE SURGERY
CORNEA | LENS | |
|---|---|---|
MYOPIA | – PRK – LASIK – Radial keratotomy – Intrastromal plastic rings | – Clear lens extraction – Phakic IOL: iris clipped lenses and implantable contact lenses |
HYPEROPIA | – PRK – LASIK – Laser thermo-keratoplasty | – Clear lens extraction – Phakic IOL |
ASTIGMATISM | – Arcuate keratotomy | – Toric IOL implantation |
PRESBYOPIA | – Conductive keratoplasty | – Multifocal IOL |