“The rate of the foetal heart is subject to considerable variations which affords us a fairly reliable means of judging as to the well-being of the child.”
—Dr J Whitridge Williams,
(2/e Williams
Obstetrics, 1908
INTRODUCTION
Throughout the period of gestation the main duty of the obstetrician is to ensure both foetal and maternal well being. Most methods which aim at ensuring foetal well being do so by detecting the foetal heart rate. Much has been learned regarding the various methods of assessing foetal heart rate over the past century since the previously mentioned statement was written by Dr. J. Whitridge Williams.
Presently the obstetricians still rely on the foetal condition in order to get an insight into its health. While in the past the clinicians mainly relied on clinical abdominal examination and intermittent auscultation using a foetoscope, stethoscope or hand foetal Doppler's device, good antenatal surveillance today involves a combination of patient education, clinical examination, sonographic assessment and electronic foetal monitoring. In the coming few chapters, I have tried to give the detailed description of the many more sophisticated methods used for evaluating the foetus. Some of these methods in the antenatal period, include, ultrasound examination, Doppler ultrasound, electronic foetal heart rate monitoring, etc. Antepartum foetal surveillance techniques are now routinely used to assess the risk of foetal death in pregnancies with complications. Some of these include real-time ultrasonography (chapter 3), Doppler velocimetry (chapter 4), electronic foetal monitoring (chapter 6), foetal assessment tests in early pregnancy (amniocentesis and CVS) (chapter 5), foetal assessment in late pregnancy, including tests like NST, CST, BPP, etc (chapter 7), amniotic fluid assessment (chapter 8), tests for foetal lung maturity (chapter 9). Most of these antepartum tests are noninvasive and are associated with 5minimum harm to the foetus. Since the developing baby derives its nourishment and protection from the placenta, it is important to understand the anatomy and physiology of placenta and uteroplacental circulation, which would be discussed in details in chapter 2.
Modern obstetrics provides us with tests that assess the health of the baby from conception through birth. While no test is fool-proof test and there are never guarantees that a baby will be perfect even if the tests are positive, foetal testing can definitely be sometimes lifesaving, particularly in high-risk pregnancies (PIH, IUGR, gestational diabetes, etc). Therefore it becomes a must for the obstetricians to learn about techniques of foetal assessment that may benefit the women as well as her baby. Some of the commonly performed antenatal tests are listed in Table 1.1.
With technological advancements, the foetal surveillance can also extend into the intrapartum period. Some of these tests, used for intrapartum monitoring have been mentioned in Table 1.2 and include tests for foetal well-being during labour like internal cardiotocographic monitoring, foetal blood sampling, etc. (chapter 10). Some of these tests may be invasive and may require observation of certain precautions in order to cause minimum harm to the foetus.
|
|
Some of the practical situations, commonly faced in obstetric practice, where intrapartum foetal monitoring may prove to be very helpful have been discussed in chapter 11 (management of foetal distress) and chapter 12 (management of meconium-stained amniotic fluid).
With the ever increasing advancements in the field of science and technology and discovery of fancy electronic equipment for foetal monitoring, the traditional methods of foetal assessment comprising of abdominal examination are often being sidelined. However it is essential for the obstetricians not to forget the importance of findings they encounter on clinical examination. This is particularly important in developing countries where the clinicians may not have an access to the fantastic modern gadgetry which is made available to their Western counterparts. Also none of these modern tests for foetal monitoring are totally fool proof. Nowadays the patients who have an access to internet may demand that their baby be monitored with help of modern machines, little realizing the significance of clinical examination by an experienced obstetrician. Failure to do so on part of the clinician can result in much bitterness and resultant legal litigations especially if the outcome of pregnancy is not good. Thus the obstetrician needs to be well-versed not only with the clinical examination but also with the various modern methods of electronic monitoring. The present chapter would provide a detailed review of clinical abdominal examination and brief mention of various modern methods of foetal monitoring.7
|
Other chapters in this book would be describing various tests for antenatal and intrapartum foetal monitoring in detail.
FOETAL HEART RATE
Heart Rate at Term
At term, the normal foetus (free from side-effects related to medicines) before labour has an average heart rate of 140 beats/minute (120-160 bpm). Preterm foetus (at 20 weeks gestational age) has a mean heart rate of 155 beats/minute.1 For practical purposes, baseline foetal heart rate (FHR) ranging from 120 to 160 beats/minute can be taken as normal at any period of gestation. The values of foetal heart rate indicative of tachycardia or bradycardia are shown in Table 1.3.
Measurement of Foetal Heart Rate
The embryonic heartbeat can usually be identified at prenatal ultrasonography (US) by 6 weeks gestation, and the heart rate can be measured via M mode.1 Later in development, with the conversion of embryo into the foetus, foetal heart rate (FHR) can also be measured using ultrasound Doppler techniques. Foetal heart sounds can also be detected by a fetoscope or even an ordinary stethoscope. The characteristic “lub-dup” sounds are associated with closing of heart valves. The first sound 8(lub) occurs due to the closure of atrioventricular valves and signifies beginning of systole (contraction). The second sound (dup) occurs due to the closure of semilunar valves and signifies the beginning of ventricular diastole (relaxation).
Changes in Foetal Heart Rate with Increasing Gestation
Heart rate (beats/minute) is a measurement that can be made from early in development (when the heart first starts) through embryonic and foetal stages into labour and birth. With increasing gestation as the foetal heart develops there is a gradual increase in FHR which parallels with the morphological development of the embryonic heart.2–5 According to Wisser and Dirchedl, maximum increase in foetal heart is observed until the embryo reaches a length of 22 mm and correlates with normal foetal well-being.6,7 Thereafter there occurs a steady decline in FHR, which can be interpreted as a functional adaptation to muscular development of the heart. Early ultrasonographic measurement of embryonic heart rate (EHR) shows a steady increase from 75 beats/minute) to 130 beats/minute, following which there is a gradual decrease in FHR.7 Presence of a low FHR with increasing gestation in early stages of development may be an indicator of developmental failure and may end up in an abortion.
Under normal circumstances, gestations having a sac diameter of 20 mm and 30 mm should contain at least a 2 mm and 5 mm embryo with embryonic heart rates of at least 75 and 100 beats per mm, respectively; and embryos measuring 10 mm and 15 mm in length should display embryonic heart rates of at least, 120 and 130 beats per minute respectively (Coulam, Britten and Soenksen)4 (Table 1.4).9
The human embryonic period proper is divided into 23 carnegie stages which are based on the external and/or internal morphological development of the embryo, and are not directly dependent on either age or size.8 Overall, it can be observed that the differences in the FHR vary significantly with changing gestational age of the foetus. Therefore while interpreting the FHR patterns, gestational age of the foetus must always be taken into consideration.
Significance of Low Embryonic Heart Rate
When a slow embryonic heart rate is detected at 6.0-7.0 weeks, the likelihood of subsequent first-trimester demise remains elevated (approximately 25%) even if the heart rate is normal at subsequent follow-up visits.9–15 In such pregnancies, at least one follow-up scan in late first trimester is warranted. An embryonic heart rate of 90 beats per minute or less early in the first trimester carries a dismal prognosis, with a very high likelihood 10of foetal demise before the end of the first trimester. Demise usually occurs in all embryos with heart rates less than 70 beats per minute.16 FHR decreases from 30-33 weeks to 34-35 weeks, and steadily falls from 36-37 weeks onwards within the range from 130 to 140 beats/minute at term. Druzin et al (1986) have reported a normal foetal heart rate of 132 beats/minute at term.17
Utero-placental insufficiency by causing inadequate delivery of nutrients and oxygen to the foetus can result in intrauterine stress (IUS). Some of these conditions include maternal caloric and protein restriction, exposure to hypoxia, etc. Hypoxia and malnutrition during foetal life have been reported to affect the renin-angiotensin system, the hypothalamic-pituitary-adrenal axis, vascular endothelial function and sympathetic innervation, and the development of organs like the kidney. As shown in animal studies hypoxic affect on the foetus can result in a permanent reduction in the number of glomeruli, abberent development of renal vascular system and defective adrenoceptor-mediated renovascular responses.18–22 This may contribute to the development of renal dysfunction and hypertension later in life. The study by Sanders et al demonstrates that hypoxia can result in long-lasting alteration of the β-adrenergic system.23
Heart Rate and Sex of the Embryo
In past, embryonic heart rate had been traditionally suggested as an indicator of sex (male/female), with female sex being associated with a lower foetal heart rate. It was believed that a foetal heart rate lower than 140 bpm towards the middle of third trimester was supposed to mean a girl child and a rate above 140 bpm was supposed to mean a boy child. However the scientific evidence 11available till date does not support any correlation between FHR and the sex of the embryo/foetus.17,24–26
History of Foetal Heart Monitoring
Analysis of the foetal heart sound has been used for over past 100 years to find out whether the foetus is alive or not. Pinard's version of the foetal stethoscope first appeared in 1876.27 Pinard's foetoscope (simple wooden or metallic funnel) placed over the mother's abdomen to hear the foetal heart can still be used for this purpose. Criteria for the normal FHR was set up in the latter part of the 19th Century. This criterion remained virtually unchanged until the 1950's. Electronic foetal monitoring was introduced during the 1970s with the advent of CTG (cardiotocography). By the beginning of the 20th century, electronic auscultation of the foetal heart had become an established practice in Europe.
CTG provides information on both foetal heart rate and the mother's labour. Electronic foetal monitoring (EFM) was first introduced at Yale University in 1958 by the physician-inventor, Dr Edward H. Hon.27 He had identified that foetal hypoxia could have an adverse effect on the foetal heart rate. Thus detection of foetal heart patterns would offer entirely new opportunities for the identification of oxygen deficiency and thus the prevention of brain damage through early identification of foetuses at risk.
With the advent of electronic foetal monitoring, it had now become possible to continuously monitor the foetal heart rate. Prior to this, mainly intermittent monitoring using a foetoscope (Figs 1.1A and B), stethoscope (Fig. 1.2) or a hand-held Doppler device (Figs 1.3A and B) was being done.12
This is a special type of stethoscope used for listening to the foetal heart. There are many types of foetoscopes available; however a regular stethoscope works as well. This can usually be used after about 18 weeks and is non-invasive and simple to use. Unlike the ordinary stethoscope, the foetoscope does not have ear pieces attached to it. One end of the foetoscope is applied over the maternal abdomen and a clinician is present at the other end, listening. The clinician requires to be trained to hear and interpret the foetal heart sounds. However this is usually not a problem since listening to the foetal heart is a standard procedure taught in every medical and nursing type institution. Hearing through human ear can help in preventing some of the mechanical errors related to the use of machines. Another advantage of foetal heart monitoring through foetoscope is that it gives mother the mobility to move about at her own wish, during the labour.13
Fig. 1.3B: The obstetrician listening to the foetal heart with the help of a hand held Doppler device
The main disadvantage of this method is that in the case of pregnancies at high risk or induced pregnancies (with medication with oxytocin, misoprostol, etc), it cannot provide continuous round the clock monitoring that may be necessary.
This is a handheld ultrasound device that transmits the sounds of the baby's heart rate either through a speaker or into ear pieces that are attached. This can generally pick up heart tones after 12 weeks gestation. A Doppler instrument, can detect the foetal heart sounds using sound 14waves. The advantages and disadvantages of measuring the foetal heart rate through hand held Doppler device is similar to that of foetoscope. In comparison to the EFM, the Doppler doesn't provide a written record of the heart rate. However similar to the use of foetoscope or stethoscope, it is a quick and simple way to listen to foetal heart rate without causing much maternal inconvenience and restriction of her movements. This method is also used for intermittent auscultation, requires little training to use, and has a live person on the other end. In comparison to intermittent auscultation using a foetoscope or a stethoscope, hand held Doppler is easier to use during a contraction, helps in detecting foetal heart rate earlier in gestation and helps in easy localisation of foetal heart.
Role of Amniotic Fluid Measurement in Foetal Well-being29
Since the foetus derives its nutrition from amniotic fluid, the volume of amniotic fluid serves as an indicator of foetal well-being. In clinical practice, the amount of amniotic fluid is measured using ultrasound scanning. An estimate about the adequacy of amniotic fluid can be made by an experienced obstetrician after conduction an abdominal examination. The chemical analysis of amniotic fluid helps in determining foetal maturity through tests like lecithin/sphingomyelin (L/S) ratio, levels of phosphatidyl glycerol, etc. (for details see chapter 8).
Even in the present time of technological advancements, the obstetricians must not underestimate the importance 15of clinical abdominal examination. In developing countries, many hospitals do not have facilities for electronic monitoring. When intermittent auscultation is used to monitor the baby, the contractions are not constantly monitored, as they would be with continuous electronic monitoring. In these cases, the clinician needs to assess the abdominal contractions through the method of abdominal palpation. The abdominal examination should comprise of the following:
- Estimation of height of uterine fundus
- Obstetric grips (Lepold's manoeuvres)
- Uterine contractions
- Estimation of foetal descent
- Auscultation of foetal heart
- Electronic monitoring
- Intermittent auscultation.
Fundal Height (Height of the Uterus)
After centralising the dextro-rotated uterus, the ulnar border of left hand is placed at the upper level of the fundus. The uterine height corresponds to the period of gestation. With increasing period of gestation the height of the uterus increases. The rough estimation of fundal height with increasing period of gestation is shown in Table 1.5 and Figure 1.4.
However estimation of period of gestation from the fundal height is not a fool proof method as there are certain conditions where height of the uterus can be more than the period of gestation (Table 1.6) as well as the conditions where height of the uterus is less than the period of gestation (Table 1.7).
Measurement of Symphysio Fundal Height (Fig. 1.5)
After centralizing the dextro-rotated uterus, the upper border of the fundus is located by the ulnar border of left hand and this point is marked by placing one finger there.16
|
|
|
The distance between the upper border of the symphysis and the marked point is measured in cm with help of a measuring tape. After 24 weeks, the symphysio fundal height measured in centimetres corresponds to the period of gestation up to 36 weeks. Though a variation of 2 cm (more or less) is regarded as normal, there are numerous conditions where the height of uterus may not correspond to the period of gestation (Tables 1.6 and 1.7).
Obstetric Grips or Lepold's Manoeuvres (Fig. 1.6)
These grips are also known as Lepold's manoeuvres. Obstetric grips must be conducted when the uterus is relaxed and not when the woman is experiencing contractions. The mother should be comfortable lying in supine poison and her abdomen is to be bared. She should be asked to semiflex her thighs in order to relax the abdominal muscles.18
These manoeuvres can be performed throughout the third trimester and between the contractions, when the patient is in labour. Besides estimating the foetal lie and presentation many an experienced obstetricians are also able to estimate foetal size and weight through these manoeuvres. These manoeuvres can be used by experienced clinicians as an effective screening tool for detecting foetal malpresentation, particularly in settings where ultrasound may not be readily available. A study by Lydon–Rochelle et al estimated the sensitivity of 88%, specificity of 94%, positive predictive value of 74%, and negative predictive value of 97%, using Lepold's maneuvers, in a population with a 17 percent frequency of foetal malpresentation.32 The following obstetric grips/Lepold's manoeuvres are carried out:19
Fundal Grip (Lepold's First Manoeuvre)
This is conducted while facing the patient's face. This grip helps the obstetrician identify which of the foetal poles (head or breech) is present at the fundus. The fundal area is palpated by placing both the hands over the fundal area. Palpation of broad, soft, irregular mass at the fundus is suggestive of foetal legs, thereby pointing towards head presentation. Palpation of a smooth, hard, globular, ballotable mass at the fundus is suggestive of foetal head and points towards breech presentation.20
Lateral Grip (Lepold's Second Manoeuvre)
This grip is also conducted while facing the patient's face. The hands are placed flat over the abdomen on the either side of the umbilicus. Lateral grip helps the clinician in identifying the position of foetal back, limbs and shoulder in case of vertex or breech presentation. The orientation of the foetus can be determined by noting whether the back is directed vertically (anteriorly, posteriorly) or transversely. In case of transverse lie, hard round globular mass suggestive of foetal head can be identified horizontally across the maternal abdomen. The foetal back can be identified as a smooth curved structure with a resistant feel. The foetal limbs would be present on the side opposite to the foetal back and present as small, round, knob like structures. After identifying the back, the clinician should try to identify the anterior shoulder, which forms a well-marked prominence just above the foetal head (in case of cephalic presentation).
Pelvic Grips
Second pelvic grip (pawlik's grip) (Third Leopold's) this examination is done facing the patient's face. The clinician places the outstretched thumb and index finger of the right hand keeping the ulnar border of the palm on the upper border of the pubic symphysis. If a hard globular mass is gripped, it implies vertex presentation. A soft broad part is suggestive of foetal legs. If the presenting part is not engaged, it would be freely blallotable between the two fingers. If the presenting part is deeply engaged, the findings of this manoeuvre simply indicate that the lower foetal pole is in the pelvis. Further details would be revealed by the next manoeuvre. In case of transverse presentation the pelvic grip is empty. Normally the size 21of head in a baby at term would fit in the hand of the examining clinician.
First pelvic grip (Fourth Leopold's): First pelvic grip is performed while facing the patient's feet. Tips of three fingers of each hand are placed on the either side of the midline in downwards and backwards direction in order to palpate the foetal parts present in the lower pole of the uterus. The fingers of both the hands should be placed parallel to the inguinal ligaments and the thumbs should be pointing towards the umbilicus on both the sides. In case of vertex presentation a hard smooth globular mass suggestive of foetal head can be palpated on pelvic grip. In case of breech presentation broad soft, irregular mass is palpated.
Uterine Contractions
Typically by placing hands on the patient's abdomen and feeling her uterus contract, the clinician will get an idea regarding her uterine contractions. The parameters to be assessed include, number of uterine contractions in a 10 minutes period, duration of contractions, regularity of contractions and intensity of contractions. Another important parameter to assess is whether the contractions result in dilatation of the cervix. One way to determine the intensity of a contraction is by comparing the firmness of the uterus to areas on the clinician's face. For example, the cheek could be considered as mild, the tip of the nose as moderate, and forehead as strong. In the early stages of labour the frequency of the uterine contractions may be after every 10-15 minutes, lasting for about 30-60 seconds. However as the labour progresses, the frequency and duration of uterine contractions greatly increases with contractions occurring after every 1-2 minutes and lasting for about 60-120 seconds.22
Foetal Descent
With the progress of second stage of labour there is progressive downwards movement of the foetal head in relation to pelvic cavity. Foetal descent is evident from abdominal and vaginal examination. Vaginal examination reveals the descent of foetal head in relation to the ischial spines (would be described with the vaginal examination).
The assessment of foetal descent through the abdominal examination is done by using the fifth's formula. In this method, number of fifths of foetal head above the pelvic brim is estimated. The amount of foetal head that can be palpated per abdominally is estimated in terms of finger breadth which is assessed by placing the radial margin of the index finger above the symphysis pubis successively. Depending upon the amount of foetal head palpated per abdominally, other fingers of the hand can be placed in succession, until all the five fingers cover the foetal head. A free floating head would be completely palpable per abdomen. This head accommodates full width of all the five fingers above the pubic symphysis and can be described as 5/5. A head which is fixing but not yet engaged may be three fifths palpable per abdominally and is known as 3/5. A recently engaged foetal head may be two fifths palpable per abdominally and is known as 2/5, while a deeply engaged foetal head may not be palpable at all per abdominally and may be described as 0/5.
Auscultation of Foetal Heart
The foetal well-being is usually assessed by listening to the foetal heart. The auscultation of foetal heart will also give some idea regarding the foetal presentation and position.23
The region of maternal abdomen where the heart sounds are most clearly heard would vary with the presentation and extent of descent of the presenting part. The foetal heart rate can be monitored in the following ways, which would be described below in details:
- Electronic foetal monitoring: Using an external foetal monitor (for details see chapter 6).
- Intermittent auscultation: This can be done with the help of a Doppler instrument or Pinard's foetoscope or even an ordinary stethoscope (described previously).
Usual Management of a Booked Patient at the Time of Labour (Flow chart 1.1)
In most of the tertiary health care centres at the time of beginning of labour (in the first stage), EFM is performed for 20-30 minutes. If the heart rate is within the normal range (100-160 bpm), shows good variability, shows presence of accelerations and provides no evidence of decelerations, it is said to be “reassuring.” This implies that the baby is in good condition and is tolerating labour well. If the woman has no associated risk factor (postmaturity, IUGR foetus, history of pre-eclampsia, gestational diabetes, etc) and her cardiotocograph trace is normal, continuous electronic foetal heart monitoring is usually not recommended. However the heart rate of the foetus is monitored intermittently at regular intervals using a stethoscope or a foetoscope or a hand held Doppler device. Whatever method of monitoring, the main aim of the obstetrician is to assess the foetal heart rate and to assess its relationship with the uterine contractions.25
Though methods like EFM and intermittent auscultation can be continued even as the labour progresses, it may become difficult to interpret the foetal heart rate properly in presence of strong uterine contractions and maternal bearing down efforts. If the obstetrician wants a more accurate assessment of foetal heart rate at this stage, she can restore to other techniques like internal foetal monitoring, etc (chapter 11), which give a more accurate assessment of foetal heart. Some of the tests for intrapartum foetal monitoring are enlisted in Table 1.2.26
|
Intermittent Auscultation
Intermittent auscultation implies listening to the baby's heart rate at preset regular time intervals. ACOG recommended auscultation intervals are shown in Table 1.8. Usually, this is done every 60 minutes in early labour, every 30 minutes in active labour, after every 15 minutes in the second stage and after every push or at least after every 5 minutes (or after every contraction) when the patient is pushing.31 Auscultation of FHR should be done for 60 seconds during and immediately following a contraction. ACOG has recommended a 1:1 nurse-patient ratio if intermittent auscultation is used as the primary technique of FHR surveillance.33 Generally, intermittent auscultation is a good choice for healthy mothers who have had low-risk pregnancies. Foetal heart sounds are usually audible with a Doppler from about 12 weeks or a stethoscope from 18th weeks onwards. Besides the foetal heart sounds, both the Doppler and the foetoscope can detect other sounds called soufflé which could be either uterine or funic. Soufflé is a soft blowing sound heard upon auscultation. Uterine soufflé is heard due to the passage of blood through the dilated uterine arteries in the third trimester of pregnancy and is synchronous with the maternal pulse. Funic soufflé is the sound produced by the flow of blood in the foetal umbilical vessels and is synchronous with foetal heart rate. If the technique of intermittent auscultation is used, the health care personnel must recognize its limitations. There 27are no evidence based guidelines available to detect foetal distress or foetal well-being using auscultation alone. Measurement of foetal heart rate through stethoscope identifies the characteristic “lub-dub” heart valve sounds and points towards a likely foetal compromise by demonstrating foetal tachycardia or bradycardia. FHR should be auscultated in relationship to uterine contractions to assess the affect of uterine contractions in reducing the blood flow, resulting in hypoxia.
If at any stage intermittent auscultation reveals any abnormality in the foetal heart pattern, external electronic foetal heart rate monitoring must be performed. One major benefit of monitoring through intermittent auscultation is that when the patient is not being monitored, she can move around as her will. In contrast, an electronic monitor would restrict her movements and she has to remain confined to the bed most of the time. Intermittent auscultation also may give the woman a feeling of more natural birth experience, since she would not be constantly connected to machines. Intermittent auscultation is believed to be as useful as electronic foetal heart rate monitoring in a low risk foetus. In a meta-analysis of all published randomised controlled trials by Vintzileos et al to compare the foetal outcomes by using continuous electronic foetal heart rate monitoring (EFM) as the main method of intrapartum foetal surveillance in comparison to intermittent auscultation, it was found that both groups showed the same APGAR scores at birth.34 However the use of intermittent auscultation was observed to actually reduce the rates of surgical intervention and caesarean sections.
The foetal heart sounds not only give information about the viability of the foetus, but the point of maximum intensity of foetal heart sounds also helps in confirmation of foetal lie, presentation and position.28
As a rule, the point is below the umbilicus in all cephalic presentations, above the umbilicus in all breech presentations, and at or just above the umbilicus in transverse or oblique presentations. The foetal heart is best audible through its left scapular region in vertex and breech presentation 29where the convex portion of the back is in contact with the uterine wall. However in face presentation, the heart sounds are heard through the foetal chest.
Depending on the position of foetal back towards left or right side, the foetal heart sounds would be heard on the same corresponding side. It is nearest the midline in anterior positions and further away from the midline in posterior positions. For example, in the left occipito-anterior position, the FHS is located in the middle of the spino-umbilical line of the left side, whereas in the right occipito-anterior position, the FHS is located in the middle of the spino-umbilical line of the right side. In occipito-lateral position, it is heard more laterally and in occipito-posterior positions, it is heard more posteriorly. In left occipito-posterior position, it is heard more posteriorly on the maternal flank on the left side whereas in the right occipito-posterior position, it is heard more posteriorly on the maternal flank on the right side. With the descent of foetal presenting part the point of maximum intensity also progressively shifts downwards.
Continuous Electronic Foetal Monitoring
In high risk pregnancies, there may be a requirement for continuous foetal heart rate monitoring. In these cases, the foetal heart rate is recorded continuously by Doppler ultrasound, while a tocodynameter records the uterine contraction pattern. These measurements are recorded on a moving strip of paper. This is known as external electronic foetal heart monitoring.35 Electronic foetal monitoring can be of two types either external (Fig. 1.9) or internal. While external monitoring can be used in both antepartum and intrapartum periods, internal monitoring can be used only in the intrapartum period after the membranes have ruptured. Internal electronic foetal heart rate monitoring would be discussed in details in chapter 10.30
According to Pattison and McCowan (2006)35 an electronic method of foetal monitoring can be defined as simultaneous measurement of foetal heart rate (FHR) and uterine contractions in order to identify the presence of foetal hypoxia. Reduced oxygen supply to the foetus during delivery is one of the important causes for neurological injury, including complications like cerebral palsy, perinatal death, neurodevelopmental disability in children (MacLennan 1999).36 The aim of foetal monitoring is to make it possible for the obstetrician to identify and quantify the risk of foetal injury. Timely identification of foetal hypoxia would help in improving foetal birth outcomes by taking timely steps to deal with foetal hypoxia before it could lead to perinatal mortality or foetal neurological injury. The interpretation and evaluation of the foetal heart rate pattern on the CTG trace is essential in the care of the obstetrical patient. Reassuring signs 31of foetal well-being on foetal heart monitoring will help to assure the obstetrician about the foetal well-being. Abnormal findings on foetal heart trace would guide the obstetrician either to expedite the delivery of the foetus or refer the patient to a higher centre in case adequate facilities for child birth and delivery are not available at the place of delivery.37
Electronic foetal monitoring has been controversial since years, with most health care professionals believing that it is an unnecessary intervention in childbirth, particularly in low-risk pregnancies. Some researchers believe that the electronic foetal monitoring devices can result in unnecessary caesarean sections because they can erroneously indicate foetal jeopardy.38 Another reason which questions the use of the EFM is that acceptable degrees of variation in the foetal heart rate have not been firmly established. Not uncommonly, even extreme fluctuations result in perfectly normal babies being born without technological intervention. Several studies have established that continuous external electronic monitoring is no more effective at identifying foetal heart rate patterns related to foetal distress in comparison to those identified by periodic manual auscultation.39–50
Until recently there had been rampant, routine use of electronic foetal heart monitoring (EFM) even in cases of low risk pregnancy. The overuse of EFM is now being challenged by both ACOG and RCOG as an iatrogenic, unscientific practice that increases the rate of caesarean section and consequent surgical risks to the mother without improving foetal outcomes.33,51 The use of continuous CTG in many hospitals in developing countries like India is not a standard procedure, where more commonly a combination of intermittent CTG, with intermittent auscultation using hand held Doppler devices or Pinard 32stethoscope between recording periods is accepted as standard practice.
When the woman arrives at the hospital in labour, the health care team will assess the maternal progress by monitoring her uterine contraction pattern and her cervical dilatation, effacement, foetal descent, position of presenting part, etc. by conducting an abdominal and vaginal examination. The parameters observed on vaginal examination are described below:
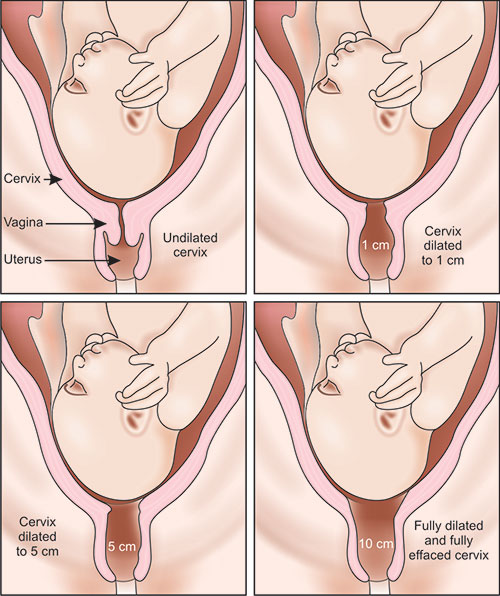
Cervical Dilatation (Fig. 1.10)
The force of uterine contractions exerts a centrifugal pull over the cervix resulting in its distension. This process is known as cervical dilatation. After the cervix is completely dilated (10 cm), the second stage of labour begins in which there is progressive descent of the foetal presenting part, which is used to assess the progress of labour. The cervical dilatation is usually described in terms of centimetres (1-10 cm). In the early stages the cervical dilatation can also be described in terms of fingers (one finger or two fingers dilated). The cervix is said to be fully dilated when it measures about 10 cm.
Cervical Effacement (Fig. 1.11)
Cervical effacement can be defined as obliteration or taking up of cervix resulting in conversion of cervical canal (about 2 cm in length) into a circular orifice with paper thin edges. This takes place from above down wards. The cervical effacement primarily results due to taking up or pulling upwards of the muscular fibres at the level of internal os into the lower uterine segment.33
As illustrated in Figure 1.12, the edges of internal os are drawn upwards several cm to become part of the lower uterine segment. When the cervix is reduced to one-half of its original length, it is 50% effaced. When the cervix becomes as thin as the corresponding lower uterine segment, it is known as 100% or completely effaced.34
Descent of Foetal Head (Station) (Fig. 1.12)
The level of the presenting part is described in terms of ischial spines (slight bony projections on the lateral pelvic wall), which are mid-way between the pelvic inlet and 35the outlet. The ischial spines are arbitrarily designated as zero station. The bispinous diameter between the two ischial spines (10.5 cm) is the shortest diameter of the pelvis in the transverse plane. The levels above and below the spine are divided into 5 parts (equal to 1cm each). The 5 stations above the ischial spine are known as minus stations (minus 1 to minus 5 from below to upwards) and the 5 stations below the ischial spines are known as plus stations (plus 1 to plus 5 from above to downwards).
Position of the Foetal Presenting Part
Since the cephalic presentation is the most common foetal presentation, with the presenting part most commonly being the vertex, the foetal position would be described for vertex presentation (Fig. 1.13).
The fingers are swept across the foetal presenting part, in order to determine the positions of the foetal sagittal suture and position of the anterior and posterior fontanelle (Fig. 1.14). The various positions of foetal head are shown in Figure 1.13 and represent the position of the occiput. In majority of cases the foetal head enters the pelvis with the saggital diameter lying in the transverse diameter of the pelvis. If the occiput is on the left side of maternal pelvis it is known as LOT position, where as if the occiput is on the right side, it is known as ROT position. LOT position is one of the commonest positions of foetal head, present in about 40% cases. At times, the head may enter the pelvis with the saggital diameter rotated at 45 degrees from the transverse plane. If the rotation is more towards the left side, it is known as LOA position, whereas if it more towards the right side, it is known as ROA position. In certain situations, the foetus may enter the pelvis in occipito-posterior position (occiput is directed posteriorly), which again may be LOP or ROP.37
Moulding of Foetal Head (Fig. 1.15)
Head moulding refers to changes in shape of forecoming head in response to external compression force. Since the contents of the foetal skull are incompressible there is very little change in the size of head. Moulding causes compression of the engaging diameter of the head with corresponding increase in the diameter at right angles to it. In the normal term labour with vertex presentation, the suboccipito-bregmatic diameter shortens and the mento-vertical diameter lengthens. The mechanism of moulding has yet not been delineated. It is still not clear whether this is due to unbending or straightening of the parietal bones or due to overlapping of sutures.52 The different grades of moulding are described in Table 1.9.38
|
Moulding of the foetal skull is a physiological process which disappears within few hours after birth. It is also a beneficial process which helps in the delivery of foetal skull.
Pelvic Assessment
Another important parameter which is assessed during the vaginal examination is the adequacy of the pelvis in relation to the foetal size. Various diameters of pelvis are assessed to evaluate if the foetus would be able to negotiate through the maternal pelvis resulting in normal foetal delivery. Detailed description of various diameters of maternal pelvis is beyond the scope of this chapter.
PARTOGRAM (Figs 1.16A and B)
Partogram is a graph devised by the WHO in 1987 for ensuring the active management of labour.53 The World Health Organisation partograph clearly differentiates normal from abnormal progress in labour and identifies those women likely to require intervention. Its use in all labour wards is recommended.54 It is not exactly used for monitoring the foetus, rather for monitoring the labour. However it is being discussed in this section as undue prolongation of the labour may result in increased perinatal morbidity and mortality. On the other hand, active management of labour helps in ensuring maternal and foetal well-being and improved pregnancy outcome.39
Active management of labour involves use of partogram, early amniotomy, early use of oxytocin, and continuous professional support, to prevent undue prolongation of labour and also helps in reducing the rates of caesarean sections and operative vaginal delivery.55
In a partogram, the normal progress in active labour is evaluated on the basis of various clinical parameters assessed with help of abdominal and vaginal examination. These include parameters like descent of the presenting part, dilatation of cervix, foetal heart rate, presence of moulding, pattern of uterine contractions, general condition of the mother, prescription of medicines to the mother, etc all of which are recorded on the graph (Figs 1.16A and B). As shown in the Figure 1.16 A, already two lines, the action line and the alert line have been plotted on the partogram. The idea of these two lines is that if progress was slow these lines would be crossed and intervention should follow. The alert line corresponds with onset of active phase of labour. When the cervix has dilated to about 3-4 cm, the clinician should expect it to progress at the rate of 1cm per hour in the primigravida and 1.5 cm per hour in the multigravida. In case the progress is slower than the ideal as indicated by the action line, the obstetrician may be required to take certain interventions for augmenting the labour including steps like using oxytocin, use of vacuum or forceps, etc.55 If nothing seems to work the obstetrician may have to resort to caesarean section as the last option. A four hour wait is recommended before resorting to any intervention when the active phase is slow. Figure 1.16 B shows a partogram in a 28 years old primi patient who was not showing sufficient progress despite of performing an ARM and starting oxytocin drip. After 4 hours of waiting period since the time of crossing the action line, a caesarean section was performed.
Normally the first stage of labour can be defined as onset of true labour pains and ends with the complete dilatation of cervix.42
| |||||||||||||||||||
It lasts for an average of 12 hours in the primigravida and 6 hours in multigravida (Table 1.10). Second stage begins with the dilatation of cervix and ends with the foetal expulsion. The second stage lasts for about two hours in the primipara and half an hour in the multipara. Cervical dilatation in the first stage of labour has two phases: a latent phase and an active phase. The latent phase with the cervical dilatation of about 2.5-3 cm lasts for about 8 hours in the primipara and for about four hours in the multipara. The active phase has three components: an acceleration phase with cervical dilatation of 2.5-4 cm, phase of maximum slope (4-9 cm) and phase of deceleration (9-10 cm). In primigravidae the cervical effacement primarily occurs in the latent phase while in the multipara, effacement and dilatation occur simultaneously.
In a multicentric trial by Thornton, and Lilford it was shown that the use of the partograph with an agreed labour-management protocol caused a significant reduction in the rates of both prolonged labour (from 6.4% to 3.4% of labours) and the proportion of labours requiring augmentation (from 20.7% to 9.1%).56 This led to a significant reduction in rates of emergency caesarean sections and intrapartum stillbirths.43
SUMMARY
Foetal monitoring is an important aspect of management of pregnancy and labour. Despite of increasing advancements in the field of science and technology which has provided us with novel methods, abdominal examination still forms a trusted and time-tested method of foetal monitoring. Though electronic foetal monitoring provides reassurance to the mother and extra information to the clinicians and midwives, it is a device that requires training and experience to make it a source of reliable information. There are many incidences of misinterpretation from these devices and it is important that users are aware of the limitations involved when using these devices.
REFERENCES
- Williams Obstetrics Antepartum and Intrapartum assessment. In: Cunningham FG, leveno KJ, Bloom SL, Hauth JC, Gilstrap L, Wenstrom KD (eds). 22 nd edition. McGraw-Hill: London; 2005. pp 373–88, 443-72.
- Howe RS, Isaacson KJ, Albert JL, Couifaris CB. Embryonic heart rate in human pregnancy. J Ultrasound Med. 1991 Jul;10 (7): 367–71.
- Schats R, Jansen CA, Wladimiroff JW. Embryonic heart activity: appearance and development in early human pregnancy. Br J Obstet Gynaecol. 1990 Nov;97 (11): 989–94.
- Coulam CB, Britten S and Soenksen DM. Pregnancy: Early (34-56 days from last menstrual period) ultrasonographic measurements in normal pregnancies. Hum Reprod 1996 Aug;11 (8): 1771–74.
- Tezuka N, Sato S, Kanasugi H, Hiroi M. Embryonic heart rates: development in early first trimester and clinical evaluation. Gynecol Obstet Invest. 1991;32(4):210–12.
- Wisser J, Dirchedl P. Embryonic heart rate in dated human embryos. Early Hum Dev. 1994 May;37 (2): 107–15.
- Harkness LM, Baird DT. Morphological and molecular characteristics of living human foetuses between Carnegie stages 7 and 23: developmental stages in the post-implantation embryo. Hum Reprod Update. 1997 Jan-Feb;3 (1): 3–23.
- Achiron R, Tadmor O, Mashiach S. Heart rate as a predictor of first-trimester spontaneous abortion after ultrasound-proven viability. Obstet Gynecol. 1991 Sep;78(3 Pt 1): 330–34.
- Benson CB and Doubilet PM. Slow embryonic heart rate in early first trimester: indicator of poor pregnancy outcome. Radiology. 1994 Aug;192 (2): 343–44.
- May DA Sturtevant NV. Embryonal heart rate as a predictor of pregnancy outcome: a prospective analysis. J Ultrasound Med. 1991 Oct;10 (10): 591–93.
- Stefos TI, Lolis DE, Sotiriadis AJ, Zinkas GV. Embryonic heart rate in early pregnancy. J Clin Ultrasound. 1998 Jan;26 (1): 33–36.
- Golstein SR. Embryonic death in early pregnancy: a new look at the first trimester. Obstet Gynecol. 1994 Aug;84 (2): 294–97.
- Ikegawa A. Prediction of first-trimester miscarriage from embryonic bradycardia and embryonic growth delay. J Obstet Gynaecol. 1995 Dec;21 (6): 537–44.
- Sherer DM, D Amico ML, Arnold C, Ron M, Abramowicz JS. Physiology of isolated long-term variability of the foetal heart rate. Am J Obstet Gynecol. 1993 Jul;169 (1): 113–15.
- Doubilet PM, Benson CB. Outcome of first-trimester pregnancies with slow embryonic heart rate at 6-7 weeks gestation and normal heart rate by 8 weeks at US. Radiology. 2005 Aug;236 (2): 643–46.
- Druzin ML, Hutson JM, Edersheim TG. Relationship of baseline foetal heart rate to gestational age and foetal sex. Am J Obstet Gynecol. 1986 May;154 (5): 1102–03.
- Jansson T, Lambert GW. Effect of intrauterine growth restriction on blood pressure, glucose tolerance and sympathetic nervous system activity in the rat at 3-4 months of age. J Hypertens. 1999;17:1239–48.
- Green LR. Programming of endocrine mechanisms of the cardiovascular control and growth. J Soc Gynecol Invest. 2001;8:57–68.
- Holemans K, Gerber R, Meurrens K, De Clerck F, Poston L, Van Assche FA. Maternal food restriction in the second half of pregnancy affects vascular function but not blood pressure of rat female offspring. Br J Nutr. 1999; 81:73–79.
- Slotkin TA, Auman JT, Seidler FJ. Ontogenesis of beta-adrenoceptor signaling: implications for perinatal physiology and for foetal effects of tocolytic drugs. J Pharmacol Exp Ther. 2003;306:1–7.
- Sanders MW, Fazzi GE, Janssen GMJ, et al. Reduced Uteroplacental Blood Flow Alters Renal Arterial Reactivity and Glomerular Properties in the Rat Offspring. Hypertension 2004;43: 1283.
- Glahn RP et al. Evaluation of sex differences in embryonic heart rates. Poult Sci. 1987 Aug;66 (8): 1398–401.
- DuBose TG et al. Foetal heart rate (FHR) is not an indicator of the baby's sex. J Ultrasound Med. 1988 Apr;7 (4): 237–38.
- Hall S, King K, Cox SM. Foetal sex prediction: the heart of the matter. J Ky Med Assoc. 1993 Sep;91 (9): 409–10.
- Hon EH. The electronic evaluation of the foetal heart rate. Am J Obstet Gynecol 1958;75: 1215.
- Rachel Hale. Monitoring foetal and maternal well being. British Journal of Midwifery 01 Feb 2007;15 (2): 107–09.
- Kurjak A and Chervenak FA. Donald School textbook of ultrasound in Obstetrics and Gynecology. 2nd edition. 2008. Jaypee Brothers: New Delhi.
- Antenatal complications: Foetal. Evidence based Obstetrics. In; Luesley DM, Baker PN (Eds). Arnold: London; 2004. Pp. 205–72.
- Lydon–Rochelle M, Albers L, Gorwoda J, Craig E, Qualls C.Accuracy of Leopold maneuvers in screening for malpresentation: a prospective study. Birth 1993 Sep;20 (3): 132–35.
- ACOG Committee on Practice Bulletins. ACOG Practice Bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists. Number 62, May 2005. Intrapartum foetal heart rate monitoring. Obstet Gynecol. 2005 May; 10 5(5 Pt 1):1161–69.
- Vintzileos AM, Nochimson DJ, Guzman ER, Knuppel RA, Lake M, Schifrin BS. Intrapartum electronic foetal heart rate monitoring versus intermittent auscultation: a meta-analysis. Obstet Gynecol 1995;85:149–55.
- Pattison N, McCowan L. Cardiotocography for antepartum foetal assessment. Cochrane Database of Systematic Reviews 1999, Issue 1. Art. No.: CD001068. DOI: 10.1002/14651858.CD001068.
- MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: international consensus statement. BMJ. 1999 Oct 16;319 (7216): 1054–59.
- Gimovsky ML. Electronic foetal heart rate monitoring. J Perinatol. 1994 May-Jun;14 (3): 173.
- Sawers RS. Foetal monitoring during labour. Br Med J (Clin Res Ed). 1983 December 3; 287 (6406): 1649–50.
- Anonymous. Is foetal monitoring worthwhile? Br MedJr 1971 Mar 6;1 (5748): 515–16.
- Haverkamp AD, Thompson HE, McFee JG, Cetrulo C. The evaluation of continuous foetal heart rate monitoring in high-risk pregnancy. Am J Obstet Gynecol 1976 Jun 1;125 (3): 310–20.
- Haverkamp AD, Orleans M, Langendoerfer S, McFee J, Murphy J, Thompson HE. A controlled trial of the differential effects of intrapartum foetal monitoring. Am J Obstet Gynecol 1979 Jun 15;134 (4): 399–412.
- Kelso IM, Parsons RJ, Lawrence GF, Aroroa SS, Edmonds DK, Cooke ID. An assessment of continuous foetal heart rate monitoring in labor. A randomized trial. Am J Obstet Gynecol 1978 Jul 1;131 (5): 526–32.
- Wood C, Renou P, Oats J, Farrell E, Beischer N, Anderson I. A controlled trial of foetal heart rate monitoring in a low-risk obstetric population. Am J Obstet Gynecol 1981 Nov1;141 (5): 527–34.
- Edington PT, Sibanda J, Beard RW. Influence on clinical practice of routine intrapartum foetal monitoring. BMJ 1975 Aug 9;3 (5979): 341–43.
- Quilligan EJ, Paul RH. Foetal monitoring: is it worth it? Obstet Gynecol 1975 Jan;45 (1): 96–100.
- Beard RW, Filshie GM, Knight CA, Roberts GM. The significance of the changes in the continuous foetal heart rate in the first stage of labour. Journal of Obstetrics and Gynaecology of the British Commonwealth 1971 Oct; 78 (10): 865–81.
- Pearce JM, Willson K. Foetal heart rate monitors-some clinical and technical aspects. Br J Hosp Med 1983 Aug;30 (2): 123–31.
- Shelley T, Tipton RH. Dip area. A quantitative measure of foetal heart rate patterns. Journal of Obstetrics and Gynaecology of the British Commonwealth 1971 Aug;78 (8): 694–701.
- Beguin F, Yeh SY, Forsythe A, Hon EH. A study of foetal heart rate deceleration areas. II. Correlation between deceleration areas and foetal pH during labor. Obstet Gynecol 1975 Mar;45 (3): 292–98.
- Carlan SJ, Wyble L, Lense J, Mastrogiannis DS, Parsons MT. Foetal head molding. Diagnosis by ultrasound and a review of the literature. J Perinatol 1991 Jun;11 (2): 105–11.
- World Health Organisation. The application of the WHO partograph in the management of labour. WHO, Geneva: 1994.(WHO/IHE/MSM 94.4.).
- O'Driscoll K, Meagher D. Active management of labour. Saunders, London: 1980. 3. O'Driscoll K, Foley M. Correlation of decrease in perinatal mortality and increase in caesarean section rates. Obstet Gynecol 1983 Jan;61 (1): 1–5.
- Lennox C. WHO partogram helps. BMJ 1994;309:1016 Thornton JG, Lilford RJ. Active management of labour: current knowledge and research issues. BMJ 1994 Aug 6;309 (6951): 366–69.