Foraminal Endoscopic Treatment of Painful Degenerative Conditions of the Lumbar Spine: The YESS Technique1
Introduction
Endoscopic transforaminal spine surgery has evolved, but the methods taught can be confusing because different Champions of the approach are using different philosophies and instrumentation based on their individual experience. Recent endoscope and instrument designs reflect that change, and students of the technique are sometimes confused by the teachings of the various pioneers, and the companies that manufacture their systems. While improvements may move in different directions and with different emphasis on in endoscope design, instrumentation, and surgical techniques, the treatment of the patho-anatomy should remain the same; that is, to diagnose the pain generator and treat the patho-anatomy. The ability to visualize and treat painful pathology through the foramen with the endoscope has opened the door for transforaminal treatment of degenerative conditions of the lumbar spine from T-10 to S-1, regardless of the technique utilized. This Chapter is written to summarize the evolution of the YESS technique as evolved by Anthony Yeung, a student of Kambin's Transforaminal Arthroscopic Microdiscectomy.
Foraminal techniques for treating a painful disc was historically used for highly selective indications with exclusionary surgeons took on various disc herniations accessible through the foramen. When compared with traditional microdiscectomy, these procedures have not been statistically more effective than open discectomy but are better accepted by patients who have received benefit for the procedure because it is less invasive and have less surgical morbidity. The limitations of the surgical approach and the inability to expand the surgical exposure limited the spectrum of herniations attempted by each individual surgeon. Traditional approaches to the patho-anatomy by transcanal spinal decompression and fusion was the fall back procedure when nonsurgical treatment or discectomy failed to relieve sciatica and back pain. Now that minimally invasive techniques and spinal arthroplasty is the ultimate goal of motion preservation, foraminal endoscopic surgery may gain more interest as a desirable surgical approach to the lumbar spine that preserves motion because it can approach the spine without injury to normal anatomic structures such as the multifidus and longissimus muscle. This approach provides access to painful patho-anatomy that are due to degenerative conditions of the lumbar spine.
The YESS Technique: General Overview
The technique begins in the preliminary diagnostic phase with optimal placement of a spinal needle from the far lateral skin portal to perform a diagnostic epiduralgram, followed by a therapeutic steroid injection. Additional information obtained by the epidural pattern provides additional anatomic information of foraminal anatomy, such as the size and configuration of the annular protrusion or the space occupied by the disc herniation. In the surgical phase of the technique, needle placement is optimized to facilitate the placement of a tubular retractor and endoscopic instruments in the best position to reach the patho-anatomy. Special foraminoplasty trephines and burrs are used to enlarge the foramen by decompressing the ventral surface of the superior facet and cephalad portion of the pedicle to reach the patho-anatomy in the epidural space. With this approach, it is possible to reach the epidural space even at L5-S1 where the traversing nerve resides.
I used these techniques to facilitate the evolution of a transforaminal endoscopic surgical procedure that began as a foraminal disc decompression for contained disc herniations, (also known as percutaneous endoscopic lumbar discectomy (PELD). This methodology was originally used for contained and extruded disc herniations in the first 80 patients. Advancement of the technique, however, occurred when needle trajectory and placement was refined to better target each type of herniation with precise needle and cannula positioning directed at the herniation, including targeting some herniations in the epidural space. New hinged and flexible instrumentation and inclusion of a biportal technique led to the ability to remove extruded, migrated, and sequestered disc herniations. The further development of foraminoscopes with larger working channels and high speed burrs to remove bone more efficiently, along with recognition of foraminal patho-anatomy in the foramen also led to the identification and treatment of other painful degenerative conditions of the lumbar spine that included failed back surgery syndrome, recurrent HNP, lateral foraminal stenosis, degenerative spondylolisthesis, and isthmic spondylolisthesis.
Standardization of the YESS Technique
The YESS™ technique, also known as the “inside-out technique”, include: (1) a published protocol for optimal needle and instrument placement calculated by lines drawn on the skin from the C-Arm image; (2) evocative chromo-discography™ by the operating surgeon using non-ionic radiologic contrast and indigocarmine dye to confirm concordant or non-concordant pain production during discography, and to stain tissue having contact with the injectate; (3) selective endoscopic discectomy™, 5which targets the removal of loose degenerative nucleus stained differentially by indigocarmine dye; (4) Thermal annuloplasty, a visualized radiofrequency thermal modulation of disc and annuluar defects guided by vital tissue staining; (5) endoscopic foraminoplasty, a foraminal decompression of the lateral and subarticular recess causing stenosis that include decompression in degenerative and isthmic spondylolisthesis where fusion is not needed; (6) visually and radiologically guided exploration of the epidural space; (7) probing the hidden zone of MacNab, and identifying normal versus anomalous anatomy such as autonomic nerves, including anatomic branching of furcal nerves in the axilla of the foramen; (8) using a uniportal and biportal technique for inside-out removal of extruded and sequestered nucleus pulposus.
Indications/Relative Contraindications
Current indications for the use of an endoscopic posterolateral approach to the lumbar spine encompass a wide spectrum of degenerative conditions of the lumbar spine that include: contained central and paracentral disc herniations, foraminal and far-lateral disc herniations, recurrent herniations, small non-sequestered extruded disc herniations, symptomatic annular tears, synovial cysts, biopsy and debridement of diskitis, decompression of foraminal stenosis, visualized total nuclectomy (prior to nucleus replacement), visualized discectomy and endplate preparation prior to interbody fusion or total disk replacement (TDR) implantation. Since the technique utilizes local anesthesia with mild sedation, patients with the fore stated pathology that are considered “too high risk” for general anesthesia can receive treatment safely via this approach and are excellent candidates.
Relative contraindications include any pathology not thought to be accessible from the posterolateral endoscopic approach. This may include some extruded sequestered disc herniations, extruded migrated disc herniations that have obviously separated from the base of the herniated fragment accessible by removing the ventral aspect of the superior facet foramen (i.e. migrated > 50% of vertebral body superiorly or inferiorly), recurrent or virgin disc herniations with associated epidural scarring, moderate-severe central canal stenosis, and hard calcified herniations. These contraindications are considered relative contraindications dependent on the surgeons' technical experience and comfort level. More experienced endoscopic surgeons can gain greater access to pathology utilizing advanced techniques for bone removal of ostoephytes, stenosis, and the posterolateral corner of the vertebral body prior to addressing the pathology. Other relative contraindications include inadequate support staff or equipment to successfully perform procedure, and uncooperative patients. Contraindications are also relative dependent on the patients' co-morbidities. Sometimes the endoscopic procedure is attempted because the patient is too high risk for a traditional approach, such as an overweight patient with a severe respiratory or cardiac condition precluding the use of general anesthesia. In less developed countries where the facility infrastructure limits access, the fact that a less invasive endoscopic procedure can be performed in an out-patient setting may provide more options for a wider population of patients.
The YESS System vs Other Endoscopic Systems
There are several competing endoscopic systems available, but the most widely used and the authors' preferred system is the endoscopic spine surgery system by Richard Wolf Medical Instruments, Vernon Hills, IL, USA. The current outer diameter of the cannula is 7 mm. The original YESS scope rigid 2.7 mm working channel endoscope has two distal irrigation channels, but the smaller working channel require the use of more delicate endoscopic instruments. The two irrigation channels, however, provides faster and more efficient irrigation of the disc space to clear the disc space for bipolar cauterization of bleeding sources, and has been shown to be more durable than the newer designs that house a 3.1 mm working channel (the Vertebris System). The advantages of the Vertebris system is the more durable larger instruments (which is also capable of accepting more specialized hinged and flexible instruments). The Vertebris System has a single irrigation channel to make room for the larger working channel. There is also an endoscopic foraminoscope with a 4.2 mm working channel that will accommodate a shaver based cutting burr and a diamond burr. New instrumentation is being continuously tested to make transforaminal endoscopic surgery easier and more efficient. Specialized instruments that can go down the working channel include straight and hinged pituitary rongeurs and straight and flexible suction-irrigation shavers for mechanical tissue removal, a flexible bipolar radiofrequency probe (Ellman International trigger-flex bipolar probe) for hemostasis, tissue modulation and manual probing, and a side firing Holmium-YAG laser (Trimedyne) for precise tissue and boney ablation. A standard arthroscopic tower and monitor are also required to visualize the endoscopy. Recording equipment for capturing DVD, video and still pictures is optional, but highly desirable, not only for documentation, but if 6studied by the surgeon, will help shorten the learning curve and allow for more rapid and efficient assessment of each patient's clinical result, since the MRI, discogram, and epidural gram images are all incorporated in the operative report for easy review at the postoperative visit.
Clinical Presentation and Evaluation
A careful preoperative history, physical exam, and meticulous review of the plain radiographs and MRI are essential prior to attempting an endoscopic transforaminal approach regardless of the pathology being addressed. Attention to specific anatomic relationships is important to determine whether the approach is safe, feasible, and to assure that there are no contraindications. Note the level of the iliac crest in relation to the disc space being accessed to determining the optimum needle trajectory. We also recommend checking the axial MRI images with to evaluate the relationship of the lateral recess and the size and configuration of facets to the disc space, making sure the needle can pass into the disc space without significant bony obstruction. Access to the disc may or may not require partial resection of the lateral facet (especially @ L5/S1) prior to entering the disc but this can be anticipated by a detailed preoperative review of the patients'MRI and radiographs. In extreme cases, the lateral facet must be resected first, and the trajectory of the needle and cannula changed to provide a more optimal position of the cannula and surgical instruments. This technique is reserved, of course, for very experienced endoscopic surgeons and should not be attempted by novices.
The Operative Procedure
Anesthesia
While some experienced international endoscopic surgeons prefer general anesthesia, and the authors have also utilized general anesthesia, we recommend mild sedation and local anesthesia so that the patient is awake and responsive throughout the procedure. The patient can then provide real time feedback in case of nerve irritation from instrument pressure or retraction, adding a layer of safety and allowing the surgeon to adjust the instruments accordingly. The skin, needle tract, and annulus are anesthetized with half percent lidocaine. This allows generous use of the anesthetic agent without significant long acting motor block of the nerve roots. Throughout the procedure the patient can receive mild sedation and analgesia with versed and fentanyl. We recommend against using general anesthetics like propofol which can produce temporary total analgesia, and may cause airway concerns if the patient becomes overly sedated.
Position
The patient is prone on a hyperkyphotic frame with a radiolucent table. The endoscope is on one side and the fluoroscopic unit is on the opposite side of the patient. Occasionally, the lateral approach can be sued for patients who cannot lay on their stomach because of their size, but the prone position is the easiest and most efficient position.
Procedure
The instructions below are a step-by-step surgical technique and protocol for accessing the disc space using an endoscopic transforaminal approach. Optimal needle placement is the most crucial step of the procedure and is based on the type of pathology being addressed. Utilizing a thin metal rod as a radio-opaque marker and ruler, lines are drawn on the skin to mark surface topography for guidance using biplane C-arm needle placement. These surface markings help identify three key landmarks for needle placement: the anatomic disc center, the annular foraminal window (centered within the medial and lateral borders of the pedicles), and the skin window (needle entry point).
- Utilizing a metal rod as radio-opaque marker and ruler, draw a longitudinal line over the spinous processes to mark the midline on the PA view.
- Draw a transverse line bisecting the targeted disc space to mark the transverse disc plane on the PA view. The intersection of these 2 lines marks the anatomic disc center.
- On the lateral view draw the disc inclination plane from the lateral disc center to the posterior skin. This line should bisect the disc and be parallel to the endplates. This line determines the cephalad/caudal position of the needle entry point. In previous published articles on needle entry point, we have modified the technique of using the distance from the rod tip to the plane of the posterior skin because we have found that it is easier to use a far lateral projection from the spinous process using an angle of 10-20 degrees from the horizontal as the ideal reference trajectory to access the epidural space and the traversing nerve. It is easy to provide a steeper projection of the cannula by simply levering the obturator against the lateral facet to gain more lateral and ventral access to the disc.7
- The skin window's lateral location from the midline determines the trajectory angle into the foraminal annular window. A 20 degree needle trajectory to the disc should place the needle tip in the medial border of the pedicle.
- This is the desired trajectory to access posterior ¼ of the disk.
- This coordinate system of finding the optimal anatomical landmarks for instrument placement will help decrease the steep learning curve for needle placement and eliminate the less accurate “down the tunnel” method favored by radiologists and pain management physicians.
- The positive disc inclination plane of the L5-S1 disc is noteworthy. A steep positive inclination line (lordosis) will position the optimal skin window more cephalad from the transverse plane line, avoiding the “high iliac crest”. A flatly inclined L5-S1 disc will position the optimal skin window with the iliac crest obstructing the trajectory of the needle. The skin window will have to start more medial to avoid the iliac crest, and sometimes the lateral ¼ of the facet joint must be resected to allow for posterior needle placement in the disc.
- The first neutrally aligned disc inclination plane is usually at L4-L5 or L3-L4. A neutrally aligned disc inclination plane is in the same plane as the transverse plane line, thus the skin window is in line with the transverse plane line. A negatively inclined disc, often at L1-L2 and L2-L3, places the skin window caudal to the transverse plane line.
Needle Placement
Once the starting point and needle trajectory is determined, the skin window and subcutaneous tissue is infiltrated with one half percent lidocaine. A six inch long, 18 gauge needle is then inserted from the skin window at the desired trajectory (coronal plane) and passed anteromedially toward the anatomic disc center. Infiltrating the needle tract with one half percent lidocaine as you are advancing the needle will anesthetized the tissue tract avoiding pain when the dilator is passed later in the procedure. Tilt the c-arm beam parallel to the disc inclination plane (the Ferguson view) while advancing the needle toward the disc to avoid parallax error. At the first bony resistance or before the needle tip is advanced medial to the pedicle, turn the c-arm to the lateral projection. Avoid advancing the needle tip medial to the pedicle during the initial approach because doing so risks inadvertent traversing nerve root and dural puncture.
Most frequently (and ideally) the first bony resistance encountered is the lateral facet. Increase the trajectory angle to aim ventral to the facet and continue the approach toward the foraminal annular window. Turning the needle bevel to face dorsal helps the needle tip skive off the undersurface of the facet, but if the needle then deflects too much, reversing the bevel may allow the needle to fenestrate the ventral facet capsule and hug the bony facet when the exiting spinal nerve is irritated in the course of needle placement. If the trajectory is less than ideal by visualizing the trajectory angle, the skin window can be adjusted to approximate the ideal trajectory angle. The c-arm lateral projection should confirm the needle tip's correct annular location. In the lateral view the correct needle tip position should be just touching the posterior annulus surface. In the posteroanterior view the needle tip should be centered in the foraminal annular window. The above two views of the c-arm confirm that the needle tip has engaged, the safe zone, the center of the foraminal annular widow.
While monitoring the posteroanterior view, advance the needle tip through the annulus to the midline (anatomic disc center). Then check the lateral view. If the needle tip is in the center of the disc on the lateral view you have a central needle placement, which is good for a central nucleotomy. Ideally the needle tip will be in the posterior one-third of the disc indicating posterior needle placement if you are attempting to access herniations.
Instrument Placement
Insert a long thin guidewire through the 18 gauge needle channel. Advance the guidewire tip, one to two centimeters deep into the annulus, then remove the needle. Slide the bluntly tapered tissue dilating obturator over the guidewire until the tip of the obturator is firmly engaged in the annular window. An eccentric parallel channel in the obturator allows for four quadrant annular infiltration using small incremental volumes of one half percent lidocaine in each quadrant, enough to anesthetize the annulus, but not the nerves. Hold the obturator firmly against the annular window surface and remove the guidewire. Infiltrate the full thickness of the annulus through the obturator's center channel using lidocaine.
The next step is the through-and-through fenestration of the annular window by advancing the bluntly tapered obturator with a mallet. Annular fenestration is the most painful step of the entire procedure. Advise the anesthesiologist to heighten the sedation level just prior to annular fenestration. Advance the obturator tip deep into the annulus and confirm on the c-arm views. Now slide the beveled access cannula over the obturator toward the disc. Advance the cannula until the beveled tip is deep 8in the annular window. Remove the obturator and insert the endoscope to get a view of the disc, nucleus and annulus. The subsequent steps depend on the goal of the procedure and pathology being addressed. The basic endoscopic method to excise a non-contained paramedian extruded lumbar herniated disc via a uniportal technique is described here. Different steps are utilized for other pathology and are beyond the scope of this chapter.
Performing the Discectomy
First enlarge the annulotomy medially to the base of the herniation with a cutting forcep. The side-firing Holmium-YAG laser can also be utilized to enlarge and widen the annulotomy. This is performed to release the annular fibers at the herniation site that may pinch off or prevent the extruded portion of the herniation from being extracted. Directly under the herniation apex a large amount of blue stained nucleus is usually present, likened to the submerged portion of an iceberg. The nucleus here represents migrated and unstable nucleus. The endoscopic rongeurs are used to extract the blue-stained nucleus pulposus under direct visualization. The larger straight and hinged rongeurs are used directly through the cannula after the endoscope is removed. Fluoroscopy and surgeon feel guides this step. By grabbing the base of the herniated fragment, one can usually extract the extruded portion of the herniation. Initial medialization and widening of the annulotomy reduce the prospect of breaking off the apex of the herniation. The traversing nerve root is readily visualized after removal of the extruded herniation.
Next perform a bulk decompression by using a straight and flexible suction-irrigation shaver (Endius MDS). This step requires shaver head c-arm localization before power is activated to avoid nerve/dura injury and anterior annular penetration. The cavity thus created is called the working cavity. The debulking process serves two functions. First it decompresses the disc, reducing the risk for further acute herniation. Second it removes the unstable nucleus material to prevent future reherniation.
Inspect the working cavity. If a non-contained extruded disc fragment is still present by finding blue stained nucleus material posteriorly, then these fragments are teased into the working cavity with the endoscopic rongeurs and the flexible radio-frequency trigger-flex bipolar probe (Ellman) and removed. Creation of the working cavity allows the herniated disc tissue to follow the path of least resistance into the cavity. The flexible radio-frequency bipolar probe is used to contract the annular collagen at the herniation site. It is also used for hemostasis throughout the case.
The vast majority of herniations can be treated via the uniportal technique. Sometimes for a large central herniations the disc needs to be approached from both sides, biportal technique.
Postoperative Care
Since it is recommended that this technique be performed under local anesthesia, most procedures that use the approach can be performed as an outpatient procedure with same day patient discharge. Most patients require only brief postoperative monitoring depending on the amount of sedation given. The postoperative restrictions are dependent on the pathology being addressed. Small annulotomies are made during the scope insertion into the disc therefore postoperative activity restrictions should be similar to that of an open lumbar discectomy. This activity modification will allow adequate time for scar formation over the annulotomy defect and to prevent herniation/reherniation.
Complications and Avoidance
There is peer-reviewed literature on complication rates associated with spinal surgery performed via an endoscopic transforaminal approach.1-4 Potential complications of the endoscopic transforaminal approach include nerve dysesthesias (5-15%), transient (1.9%), persistent sensory deficit (1%), deep infection (0.65%), discitis (.05%), dural tear (0.3 %), thrombophlebitis (0.65), bowel injury (.004%), vascular injury (0%), respiratory distress requiring intubation (0%).4
Complications can be avoided by strictly adhering to the details in the keypoints section above and principles of the YESS technique listed in Table 1-2. Avoidance of complications is enhanced by the ability to clearly visualize normal and patho-anatomy, the use of local anesthesia and conscious sedation rather than general or spinal anesthesia, and the use of a standardized needle placement protocol. The entire procedure is usually accomplished with the patient remaining comfortable during the entire procedure and should be done without the patient feeling severe pain except when expected, such as during evocative discography, annular fenestration, or when instruments are manipulated past the exiting nerve. Local anesthesia using half percent xylocaine allows generous use of this dilute anesthetic for pain control and still allows the patient to feel pain when the nerve root is manipulated. Thus the awake and aware patient serves as the best indicator to avoid any nerve irritation/damage. Dural tears can be treated with a visualized blood patch and observation because there is no “dead space” for CSF collection/drainage.
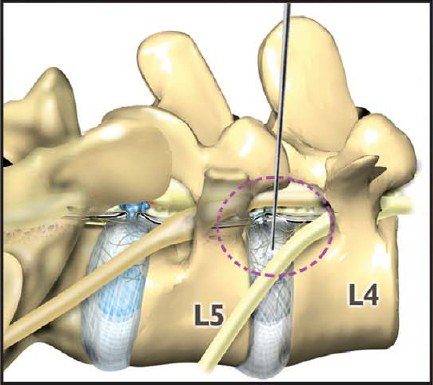
Figure 1-1: The foraminal portal is bordered by the superior facet dorsally, the exiting nerve ventrally and the superior end plate of the inferior vertebra.
|
Figure 1-3: The ‘Inside out” technique first decompresses and removes the nucleus from the base of the herniation. If the extruded fragment is large, medialize the annulus to release the annulus, to allow easier removal of the herniation.
Discussion/Conclusions
The endoscopic transforaminal approach is safe and efficacious but does require a unique combination of skills not typically used by spine surgeons. Prior experience with discography, epidural injections and arthroscopic experience is helpful in reducing the learning curve. Most spine surgeons are unfamiliar and uncomfortable with the endoscopic transforaminal approach therefore the learning curve is a major obstacle to more widespread use of this technique. Some surgeons feel that the potential for inferior outcomes that is associated with the learning curve of this approach may not be justified when open posterior approaches dictate high success rates and outcomes. Perhaps this is why this transforaminal approach is seldom utilized by the spinal surgeons despite the fact that the technique was first described by Kambin in 1991. New implants, instruments, and technological advances, however, have made this approach safer, easier to learn, and a versatile option for effective delivery of implants to the disc space. The benefits of using muscle spreading techniques under local anesthesia (avoiding general anesthesia) to access the foraminal anatomy and disc space cannot be denied.11
Future Considerations
Perhaps the best new indication for the use of this technique and approach is in the realm of motion preservation (nucleus replacement) or minimally invasive anterior stabilization. One advantage of this approach stems from its ability to approach the disc through the foramen avoiding the morbidity associated with dural scarring encountered in revision lumbar surgery. The presence of scar tissue makes traditional posterior lumbar interbody fusion techniques difficult or impossible but an interbody fusion via an endoscopic transforaminal approach would avoid this issue. A biportal endoscopic fusion technique can be used to perform a radical discectomy with burring of the endplates under direct visualization and subsequent delivery of a cage and bone graft. Transforaminal anatomy will limit size of implant that can be delivered, however this problem can be overcome by using expandable interbody devices.
This approach is also applicable as a vehicle for visualized nuclectomy and delivery of nucleus replacement. Endoscopic nuclectomy can be performed under direct visualization prior to implanting an expandable nucleus replacement or possibly a disc replacement. Although this would be a promising extension of the technique and approach, much work is necessary to assure that this is safe and efficacious.
References
- Yeung AT. Minimally Invasive Disc Surgery with the Yeung Endoscopic Spine System (YESS). Surg Technol Int 2000;VIII: 267–77.
- Yeung AT, Morrison P, Felts M, Carter J. Intradiscal thermal therapy for discogenic low back pain. In the practice of minimally invasive spinal technique, MH Savitz, J Chiu, AT Yeung (Eds) 2000; 237–48.
- Tsou PM, Yeung AT, Yeung CA. Selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: A minimal access visualized intradiscal procedure. The Spine Journal 2004(2):563–74.
- Yeung AT, Yeung CA. Microtherapy in low back pain. In Minimally Invasive Spine Surgery, M. Mayer (Ed) 2005, Springer Verlag.
- Yeung AT, Yeung CA, In vivo endoscopic visualization of patho-anatomy in painful Degenerative conditions of the lumbar spine. Surgical Technology International XV, 2006;243–56.
- Yeung AT, Yeung CA. Advances in endoscopic disc and spine surgery: The Foraminal Approach. Surgical Technology International XI, 2003; 253–61.
- Yeung AT, CA Yeung. Posterolateral Selective Endoscopic Discectomy: The YESS Technique, in Endoscopic Spine Surgery and Instrumentation: Percutaneous Procedures, D. Kim, R. Fessler, J. Regan (Eds), 2005, Thieme Medical Publishers: New York.
- Yeung AT, Savitz MH. Complications of Percutaneous Spinal Surgery, in Complications in Adult and Pediatric Spine Surgery, A Vacarro, (Ed), 2004.
- Yeung AT. Minimally invasive disc surgery with the Yeung Endoscopic Spine System (YESS). Surgical Technology International VIII: 1–11, June 1999.
- Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy. State of the art. Mt Sinai J Med 2000;67(4): 327–32.
- Yeung AT, Tsou, PM. Posterolateral endoscopic excision of lumbar disc herniation. The surgical technique, results and complications in 307 consecutive cases. Spine 2002;27(7):722–31.