INTRODUCTION
Radiation is small pockets of energy, which travels as waves and transfer energy from one point to another point. There are two types of radiation namely: (i) photons, e.g. X,γ, and (ii) particles, e.g. e, p, n and α. Radiation is a double edged weapon, analogous to fire, which possess both benefits and hazards. Radiation hazards were witnessed by the following events in early days:
- Uranium mine workers
- Watch dial painters-switzerland
- Atomic bomb explosion-Hiroshima and Nagasaki
- Radiobiology experiments.
Radiation was used in medicine immediately after the discovery of X-rays by W.C. Roentgen on November 15, 1895. It was used in India in 1898 within 3 years of its discovery. The Indian army employed hefty porters to carry the cargo,(100 bounds) on a pole for 200 miles in the Hyber pass region (Pakistan). That cargo had the first X-ray tube used in India. Major Bewoor used it effectively in the North-West frontiers. The civilian use of X-rays in India began in 1900 at the Government General Hospital, presently the Barnard institute of Radiology and Oncology, Chennai.
Radiation hazards were realized in the beginning of 20th century. The X-rays were used indiscriminately in the early years and have caused visible damage to several physicians and X-ray enthusiasts. Within 6 months of their use, several cases of erythema, dermatitis and alopecia were reported among X-ray operators and their patients. In 1902 the first X-ray induced skin cancer was reported. In 1921 Ironside Bruce, a pioneering radiologist in a London Hospital died of cancer at the age of 38. Similarly several lives were lost due to excessive X-ray exposures.
In 1915, the British Roentgen Society made the first radiation protection recommendations. To regulate the safe use of radiation the “British X-ray and Radium protection committee” was formed (1921). It was made as an International Committee in 1928 and later (1950) transformed as “International Commission on Radiological Protection”(ICRP). The ICRP is the first standard setting body formed, for the purpose of radiological safety. The similar organization at the USA is the National council on radiation protection and measurements (NCRP), which was formed in 1946. 2These bodies issue periodical reports on radiation safety aspects of various application of ionizing radiation. These concepts are explained in the following paragraphs and chapters.
RADIATION UNITS
Exposure – Roentgen
The term exposure (X) refers the radiation quantity measured in terms of ionization in air, in a small volume around a point. Exposure is a source related term. Exposure from an X-ray source obeys inverse square law. The unit of exposure is roentgen (R).
One roentgen shall be the quantity of x or gamma radiation such that the associated corpuscular emission per 0.001293 grams of air (1cc of dry air at NTP), produces in air, ions carrying 1 e.s.u. of quantity of electricity of either sign. The unit may also be defined in terms of SI unit as
There are some difficulties in the unit of roentgen. It is not a unit of dose, which is a measure of absorbed energy. It can be used only up to a photon energy of 3 MeV. It is defined only for x and gamma radiation in air.
Kerma
Kerma stands for kinetic energy released in the medium, which describes the initial interaction of the photon with an atom, that take place in the medium. When radiation interacts with matter, the uncharged particles (photons and neutrons) transfer kinetic energy to the charged particles (e and P). Kerma (K) is the measure of kinetic energy transferred to the charged particles. It is defined as the sum of the initial kinetic energy of all the charged ionizing particles, liberated by photons in a material of unit mass. The unit for kerma is Joul per kilogram (J/ kg). The SI unit is Gray and the special unit is rad.
Absorbed Dose—Rad/Gray
The term absorbed dose (D) refers the amount of energy absorbed per unit mass of the substance. The unit of absorbed dose is rad (r), which means radiation absorbed dose. 1 rad =100 ergs/gram. This unit is independent of type of radiation and the medium. The SI unit of absorbed dose is Gray (Gy).
Exposure Rate Constant
It is defined as the exposure per hour from 1 mCi point source at a distance of 1cm and it is expressed in R-cm2/mCi-h. For example, the exposure rate constant of cobalt, cesium and iridium radioisotopes are 13.07, 3.26 and 4.69 respectively.
RHM and RMM
If the exposure rate constant is defined for 1Ci source at 1m, then it is called RHM (Roentgen Hour Meter). It is defined as the exposure per hour from 1Ci point source at a distance of 1m and it is expressed in R-m2/Ci-h. In practice RHM of a given radioisotope can be obtained by dividing the exposure rate constant by a factor 10. Hence the RHM of cobalt, cesium and iridium radioisotopes are 1.307, 0.326, and 0.469 respectively. Mostly RHM is employed for calibration purposes in Brachytherapy and industrial radiography.
Instead of hour one can also express it for one minute, then it is called RMM (Roentgen Minute Meter). It is defined as the exposure per minute from 1 Ci point source at a distance of 1m and it is expressed in R-m2/Ci-min. For example, if the RHM of the cobalt radioisotope is 1.307, the corresponding RMM value is 1.307/60 = 0.0217. RMM is the most preferred and useful terminology in teletherapy source calibration.
RMM and CURIE
The unit of activity is curie and it is defined as the number of disintegration per second from 1 gram of radium and it is found to be 3.7 × 1010. In the case of cobalt, 0.0217 RMM corresponds to 1Ci, hence 1RMM = (1/0.0217)= 46.08 Ci. Similarly, it can be applied to different radioisotopes (Table 1.1).
Example 1: If a Cobalt teletherapy source is purchased with 200 RMM capacity, what is the corresponding activity of the source in Ci?
1 RMM = 46.08 Ci
Example 2: If a Cobalt teletherapy source is purchased with 10,000 Ci capacity, what is the corresponding RMM value?
46.08 Ci = 1RMM
10,000 Ci = (1/46.08) × 10,000 = 217 RMM.
EQUIVALENT DOSE
The biological effects of radiation depend not only on absorbed dose (D) but also on the type of radiation. Hence, the ICRP report 26 (1977) introduced the dosimetric quantity Equivalent dose (HT). It is the absorbed dose averaged over a tissue or organ and weighted for the radiation quality that is of interest, and is given as
Where WR is the weighting factor for the radiation type and it is analogous to RBE in radiobiology. Earlier the term quality factor (Q) was used to evolve dose equivalent (absorbed dose × quality factor). This is discontinued now and replaced with equivalent dose, which is an average dose and not a point dose. Table 1.2 gives the suitable weighting factors for various type of radiations.
|
Sievert (Rolf Sievert, Swedish Radiologist) is the SI unit of equivalent dose and one Sievert (Sv) =1 Joule/kilogram. Also 1 Sv=100 Rem (Radiation equivalent men), where Rem is the special unit of equivalent dose. In practice, milli sievert (mSv) unit is used.
1 Sv = 1000 mSv
1 mSv = 100 mRem.
EFFECTIVE DOSE OR EFFECTIVE DOSE EQUIVALENT
The whole body exposures are not uniform and dose equivalents for various tissues may differ markedly. Hence, the radiation induced effects vary with the sensitivity of the organ. To account these non uniform irradiation and organ sensitivity variation, the ICRP-26 introduced the term effective dose (E), which describes the dose to the whole body and is derived from equivalent dose. It is defined as 5
where WT is the weighting factor for the tissue T, HT is the mean equivalent dose received by the tissue and E is the summed organ or tissue doses as an overall whole body dose. This quantity expresses the overall measure of health detriment associated with each irradiated tissue or organ as a whole body dose and considers the radiosensitivity of each irradiated organ or tissue. It is used to evaluate the probability of stochastic effects at low doses.
The weighting factor of a particular tissue or organ is the risk of stochastic effects being induced in the organ when singly irradiated, compared to the total risk of inducing stochastic effects if the same radiation dose is received by the whole body.
The Table 1.3 gives the tissue weighting factors for various tissues. It is seen that testes and ovaries are the most radiosensitive tissues as they have the highest value of weighting factor as per ICRP 60. However, the radiosensitivity of the breast tissue and gonads are reassessed by the ICRP (2005) and the revised weighting factors are given the table. Organ of higher sensitivity carries a higher risk for a given dose. The sum of the weighting factors is unity. The unit of effective dose is Sievert (Sv).
|
Example 3: In a CT scan study the tissues breast, lung, bone marrow and thyroid receive dose of 21, 23.5, 5.17 and 2.30 mSv respectively. Calculate the effective dose with both old and revised tissue weighting factors. The effective dose:
E = ΣWT × HT
= (21 × 0.05+ 23.5 × 0.12+5.17 × 0.12+2.3 × 0.05) = 4.60 mSv(ICRP 60)
= (21 × 0.12+ 23.5 × 0.12+5.17 × 0.12+2.3 × 0.05) = 6.07 mSv (ICRP2005)
COMMITTED DOSE
If an individual is subjected to a radiation burden over a period of time, then committed dose is the term to be used. It is the absorbed dose the individual receives as a result of the intake of radioactive material. The individual will continue to receive a dose of radiation as long as the traces of radioactivity remain with in the body. The factor which determines the remaining activity in the body is the effective half life (T1/2 eff). It is related to the physical half life (T1/2 phys) and biological half life (T1/2 biol) as follows:
One can not alter the physical half life, which is a character of a given radionuclide. Whereas the biological half life can be reduced by increasing the rate of excretion of the radionuclide from the body. For example, a radio nuclide has a physical half-life of 6 hours and a biological half-life of 3 hours, then 1/ T1/2 eff = (1/6) + (1/ 3), and T1/2 eff = 2 hours. The effective half-life is always less than either the physical or biological half-life
The committed dose equivalent is the quantitative assessment of the effect of a particular intake of radioactivity over the whole of a individual's working life. It is defined as the dose equivalent accumulated over a period of 50 years following the intake of radioactive material. In the case of children the period is taken as 70 years. It is defined
where t is the period of time in years. If the committed organ or tissue equivalent dose is multiplied by the suitable tissue weighting factors then the sum of the products is called committed effective dose (E(t)).
The other factors which influences the dose equivalent are; (i) the concentration of the activity in the organ,(ii) whether the concentration is uniform or localized, (iii) decay system, (iv) radiation weighting factor, (v) size and shape of the organ,(vi) proximity of other organs and (vii) weighting factor of the organ.
COLLECTIVE DOSE
To assess the overall effect of radiation dose on a large group of people, the individual dose may be multiplied by the population number exposed and it is called the collective dose. If N is the number of population receiving a mean organ equivalent dose HT, over a period of time t, then the collective equivalent dose (ST) is given by7
Collective Effective Dose Equivalent
In a similar way the collective effective dose (S) can be defined. It is the whole body exposure to a population group exposed to radioactive materials in the environment and can cover successive generations of the populations being studied.
In a country, if a population of 10 million people are exposed to a background dose of 3 mSv, then the collective effective dose is 30,000 man-Sv.
The collective effective dose equivalent (CEDE), can be used as a method to assess the impact of human health from population radiation exposures and it is expressed in person-Sv. The CEDE values for different occupations are given in Table 1.4
|
The uranium miners CEDE is small due to relatively small size of the workforce involved in the occupation. The total annual CEDE for all occupationally exposed workers is about 2000 Person–Sv, for all occupations. Whereas the annual CEDE attributable to natural background radiation for the same population is about 3200 person-Sv. It means that the occupational workers getting an additional 63% (2000/3200) over the natural background.
In general the CEDE is decreasing in medicine due to small size of the exposed population and improved health physics practices.
GENETICALLY SIGNIFICANT DOSE
The genetically significant dose (GSD) is defined as that equivalent dose that, if received by every member of the population, would be expected to produce the same genetic injury to the population as do the actual doses received by the irradiated individuals. It is expressed in Sievert (Sv). It is 8used to assess the genetic risk or detriment to the whole population from radiation exposure, especially in medicine. It assumes a linear dose effect relationship. For example, the patients undergo X-ray examinations may receive a dose of about 10.0 mGy. If the same dose was received by every member of the population, it would be expected to produce the same total genetic effect on the population. The GSD accounts the child bearing potential of the patient population.
The genetically significant dose (GSD) is used to assess the genetic risk or detriment to the whole population from radiation exposure. In this the equivalent dose to the gonads of each exposed individual is weighted for the number of progeny expected for a person of that sex and age. Annual GSD from all radiation sources is about 1.3 mSv that includes 1.02 mSv (78%) from natural background and 0.28 mSv (22%) from technological sources (NCRP-report 93,1987). Among the technological sources, the major contributor is diagnostic X-rays, 0.20 mSv (15%). Among the 15 %, one-third is attributable to male and two-third to females. The higher proportion of female component is due to the location of the ovaries within the pelvis, which places them in the primary beam during most abdomino pelvic examinations.
DETRIMENT
Detriment is a measure of harm caused by exposure to radiation. It is the expectation of harm incurred from an exposure to radiation, taking into account not only the probability of each type of deleterious effect, but also the severity of the effect. Usually several parameters (e.g, probability of death and reduction of life expectancy) are considered to arrive the mean health detriment. Health detriment is an estimate of the risk of reducing in length and quality of life occurring in a population following exposure to ionizing radiations.
ANNUAL LIMIT ON INTAKE
The Annual limit on intake (ALI) is the that quantity of radionuclide which, taken into the body during 1 year, would lead to a committed effective dose equal to the occupational annual limit on effective dose.
ALARA
As Low As Reasonably Achievable (ALARA) term was introduced by ICRP-26. It states that doses to patients and staff should be kept as low as reasonably achievable. Every reasonable effort must be made to reduce radiation levels below the stated dose limits within economic and social limits.9
SOURCES OF RADIATION
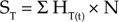
The sources of radiation are classified into (i) Natural radiation sources, (ii) Enhanced natural sources, (iii) Artificial radiation sources (man made) and (iv) Occupational exposures. The annual average per capita total effective dose equivalent is 3.6 mSv (NCRP-93,US data). About 82% of the above exposure (3 mSv) arise from naturally occurring sources, 18% (0.6 mSv) arise from technologic enhancements of naturally occurring sources and artificial radiation sources (diagnostic X-ray is the major contributor). Background radiation involves both natural and man made low level radiation exposure to all members of the public. This will vary with region and Kerala and Brazil have high background levels of radiation (100 mSv/year).
Natural Radiation Source
The natural radiation sources includes (i) Cosmic rays,(ii) Terrestrial (Primordial) radionuclides, and (iii) Internal Radioisotopes.
Cosmic Rays
Cosmic rays are extraterrestrial radiation that strikes the earth's atmosphere, that includes primary and secondary. Primary cosmic rays, in which protons accounts for 80%. The primary cosmic rays collide with atmosphere, producing showers of secondary particles (electrons, muons) and electromagnetic radiations. The average per capita equivalent dose is 270 μSv per year, which makes 8% of the natural background.
Cosmic exposures increase with altitudes. It is estimated that at 30,000 ft altitude the equivalent dose is about 5 mSv per hour and it is doubling in every 1500 feet. It is greater at the earth poles than the equator. Structures provide some protection against cosmic rays, and hence the indoor effective dose is 20% lesser than outdoor.
Air travel increases individual's cosmic ray exposures. Air crews and frequent fliers receive an additional annual equivalent dose of 1mSv. A 5 hr transcontinental jet aircraft travel result in 25 μSv equivalent dose. Apollo astronauts received an average equivalent dose of 2.75 mSv during the lunar mission. A part of secondary cosmic ray particles collide with stable atmospheric nuclei and produces cosmogenic radionuclides; e.g.147 N (n,p) 146 C, but their contribution to natural background is very little.
Terrestrial Radiations
Terrestrial radionuclides that have been present on earth since its formation are called primordial radionuclides. Their physical half lives are comparable to the age of the earth (4.5 billion yeras). Their decay products are the major contributors of terrestrial radiations. They mainly contribute in the form of external exposure, inhalation, and ingestion.10
External exposure: K-40,U-238, and Th-232 are mainly responsible for external exposure and they account an equivalent dose of 280 μSv per year. This may vary depending upon the local concentration of terrestrial radionuclides.
Inhalation: Rn-222 (U-238) is a noble gas, decays to polonium-218 by alpha emission with half life of 3.8 days. Its decay products are the most significant source of inhalation exposure. It is deposited in the tracheobronchial region of the lung. Radon concentration vary widely both seasonal and diurnal. It emanates from sail and is restricted by structures. Weatherproofing of homes, energy conservation techniques, decreased ventilation are resulting in higher indoor radon concentration. Radon inhalation accounts an equivalent dose of 2 mSv/year to the bronchial epithelium. It accounts for about 55% of natural background, which can be easily measured and reduced.
Ingestion: Ingestion of food and water is the second largest source of natural background in which K-40 is the most significant. It is a naturally occurring isotope of potassium having higher concentration at the skeletal muscle. It accounts an average equivalent dose rate of 400 μSv/year.
Internal Radionuclides
Internal radionuclides includes K-40 and C-14, which are present the in the human body. The main contributor is K-40, which emits β and γ rays and decays with a half life of 1.3 × 109 years.
Enhanced Natural Sources
Enhanced natural sources mainly consists of consumer products. The largest contributor is tobacco products, which burdens the bronchial epithelium. It produce an effective dose equivalent of 2.8μSv/year.
Radon gas dissolved in domestic water supply can contribute 10-60 μSv/ year. Building materials consists of uranium, thorium and potassium and these are present in brick, concrete, granite which may contribute an annual effective dose of 30 μSv /year.
Mining and agricultural activity contribute to a lesser level by fertilizers (uranium, thorium decay products and K-40).
Cumbustible fuels including coal, natural gas and consumer products includes smoke alarms (americium-241), gas lantern mantles (thorium), dental prostheses, certain ceramics, optical lenses (uranium) contribute <1% annual effective dose
Artificial Sources
The artificial sources of radiation includes medical exposure, radioactive fallout, nuclear power and occupational exposure.11
Medical Exposure
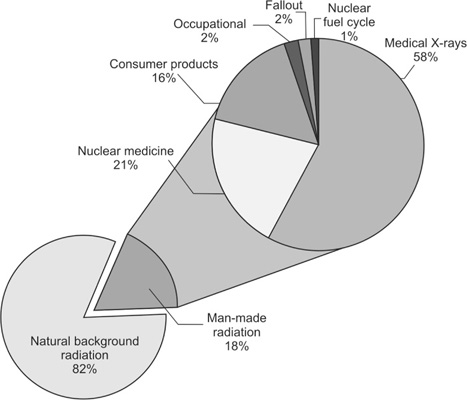
The majority of the exposure is from medical X-rays (Fluoroscopy & Computed tomography) which contribute to 58% of the artificial radiation exposure. Next contributor is the nuclear medicine which is 21%. Both produces an annual average effective dose equivalent of 540 μSv per year. It accounts for about 69% of artificial radiation.
Consumer Products
It accounts to 16% of the artificial radiation exposure. Substances in consumer products such as tobacco, the domestic water supply, building materials, and to a lesser extent, smoke detectors, televisions, and computer screens, account for the above exposures.
Radioactive Fallout
It arises from atmospheric testing of nuclear weapons and consists of Carbon-14 (70%) and other radionuclides including H-3, Mn-54, Cs-136, 137, Ba-140, Ce-144, plutonium and transplutonium elements. It results in an annual effective dose equivalent of <10 μSv. It contributes 2% of the manmade radiation exposures.
Nuclear Fuel Cycle
The contribution from nuclear power production is very minimal, which is about 1% of artificial radiation (Annual effective dose is <0.5 μSv). It involve all phases of fuel cycle; mining, manufacturing, reactor operations, and waste disposal. The most significant contributor is Carbon-14.
Occupational Exposure
The occupational exposures associates with uranium mining (12 mSv per year), nuclear power operations, medical diagnosis and therapy, aviation and research, non uranium mining, and application of phosphate fertilizers. It contributes about 2 % of the artificial radiation exposure.
Radiologist, X-ray technologist receive an average annual effective dose of 1 μSv. However special procedures involving fluoroscopy and cini-radiology (e.g. cardiac catheterization) may exceed 15 mSv. These are only partial body exposures (head & extremities), if lead apron is used during the procedure. The occupational exposures for various categories are listed in Table 1.5. The UNSCEAR and the NCRP have published the global annual dose contribution from various sources of radiations, which is presented in Table 1.6.
The average annual effective dose equivalent to a population from all radiation sources, is obtained by dividing the annual collective effective dose equivalent by the size of the population. The Fig. 1.1 shows the % contribution of various radiation sources to the total average effective dose equivalent in the US population, which is estimated as 3.0 mSv/year, excluding smoking.12
|
Smoking is the largest contributor (45%) to the average population effective dose equivalent. Hence, lung is the organ that receives highest dose equivalent from both smokers (polonium-210) and non smokers (radon-222). The Fig. 1.2 highlights the % contribution of various types of manmade radiation sources.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Fig. 1.1: The % contribution of various types of man-made sources to the total average effective dose equivalent to the US population
Fig. 1.2: The % contribution of various components of man-made radiation sources (Source BEIR VII Report)
Medical use of radiation warrant an optimal compromise between clinical utility and radiation dose to patients, staff and the public. The success of radiation protection mainly lies on the education of staff. They should be educated on radiobiology, genetics, risk analysis, methods of reducing radiation dose, decay patterns of radioactivity released in the environment and absorbing power of different materials to different radiation.
BIBLIOGRAPHY
- David JD, Patrick AK, Eugene RJ. The physics of diagnostic imaging (2nd edn.) Hodder Arnold, UK 2006.
- Donald TG, Paul C, Martin V. Principles of Radiological physics, (5th edn.) Churchill Livingstone 2007.
- International Commission on Radiological Protection ICRP 26 Annals of ICRP. Pergamon press 1997.
- Jerrold TB et al. The essential physics of medical imaging, (2nd edn.) Lippincott Williams & Wilkins 2002.
- Thayalan K. Basic radiological physics. Jaypee brothers Medical publishers (P) LTD, New Delhi 2001.