- 1.1 The bony pelvis
- 1.1.1 The ligaments of the bony pelvis
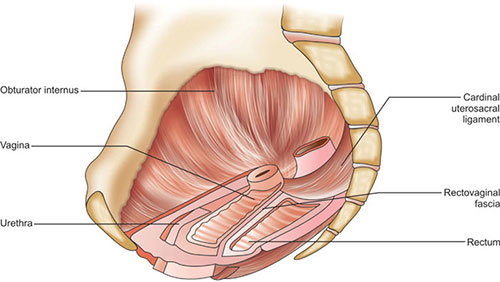
- 1.2 The visceral fascia and ligaments
- 1.2.1 Pelvic connective tissue
- 1.2.2 Muscles
- 1.3 Urogenital diaphragm
- 1.4 The perineum
- 1.4.1 The superficial perineal space
- 1.4.2 Deep perineal space
- 1.4.3 Perineal body (Central tendon of the perineum)
- 1.4.4 Blood supply
- 1.4.5 Lymphatic drainage
- 1.4.6 Nerve supply
- 1.4.7 Imaging of the pelvic floor
- 1.5 The pelvic ureter
- 1.6 The pelvic viscera
- 1.6.1 Uterus
- 1.6.2 Fallopian tube
- 1.6.3 Ovaries
- 1.6.4 Urinary bladder
- 1.7 Blood vessels of the pelvis
- 1.8 Nerve supply to the pelvic viscera
- 1.9 Lymphatic drainage of the pelvis and the perineum
- 1.10 Anterior abdominal wall
- 1.11 Conclusion
Surgical procedures in gynecology are continuously evolving, demanding knowledge of the anatomy of unfamiliar areas. Understanding anatomy, especially of the pelvis, perineum, abdominal wall and thigh is crucial to the gynecologic surgeon not only for performing difficult surgical procedures like Wertheim's hysterectomy, radical vulvectomy etc but also for routine surgical procedures. The traditionally described anatomy may have individual variations. There can be differing patterns of blood vessels between individuals. Knowledge of congenital anomalies of the genitourinary system which occur in 10% of individuals would prove beneficial in diagnosing and managing them as well as in preventing complications while encountering them during surgical procedures. Distortion of pelvic anatomy associated with endometriosis, pelvic inflammatory disease, previous pelvic surgery as well as adnexal and uterine masses predispose to injuries to ureter, bladder, rectum, pelvic vessels and nerves. Delineating anatomy in these situations helps in preventing visceral injuries to a great extent. Evolution of newer surgical techniques like laparoscopic surgery demands understanding anatomy in a different perspective.
1.1 THE BONY PELVIS
The bony pelvis protects the pelvic viscera as well as provides support by its connections with the muscles and connective tissues of the pelvis. The bony pelvis is formed by the sacrum and coccyx posteriorly and the two innominate bones anterolaterally. The ilium, ischium and pubis together form the hip bone. These three meet at the acetabulum, which is a cup shaped structure into which the femoral head fits. The ischial spine separates the greater sciatic notch from the lesser sciatic notch. In the normal position, the cervix is 2suspended at the level of the ischial spine. The bony pelvis is divided into an upper false pelvis and a lower true pelvis by the plane of the pelvic brim. The pelvic organs occupy the true pelvis. The pelvic brim is formed by the upper margin of the pubic symphysis anteriorly, iliopectineal line (arcuate line) laterally and the sacral promontory posteriorly. The pelvic cavity is a curved canal like the joint of a drainpipe, the anterior wall being much shorter than the posterior wall. In the standing position, the pelvic inlet is at about 60° with the horizontal plane while the plane of the outlet is almost horizontal (15-20° with the horizontal).
The sacrum is formed by the fusion of 5 sacral vertebrae and 4 coccygeal vertebrae. The sacral promontory has surgical importance to the gynecologist. The anterior longitudinal ligament is a thick ligament made of dense connective tissue seen in the anterior aspect of the 1st sacral vertebra. In sacral colpopexy, the vaginal apex is fixed to the anterior longitudinal ligament of the first sacral vertebra. It should be kept in mind that the middle sacral artery, a branch of the aorta and the pelvic plexus are encountered in this site. The aortic bifurcation takes place above the sacral promontory at the lower border of the 4th lumbar vertebra. Even though the level of umbilicus can have individual variation, the aortic bifurcation is usually at the level of umbilicus which should be remembered while introducing the primary trochar during laparoscopy.
Through the anterior sacral foramina exits the anterior rami of the corresponding sacral nerves and vessels. The lumbo-sacral plexus lies over the piriformis, which is seen in the posterolateral aspect of the pelvic cavity.
Striated muscles within the investing fascia cover the posterolateral and inferior walls of the pelvis. Posterolaterally, the muscles are the piriformis which arises from the ventral surface of the sacrum. Its tendon exits through the greater sciatic foramen to get inserted to the greater trochanter. It is a lateral rotator of the thigh. Laterally, the obturator internus muscle overlies the ilium, ischium and obturator membrane. Its tendon exits from the pelvis through the lesser sciatic foramen and gets inserted on to the greater trochanter. It is also an external rotator of the thigh. Parietal fascia which is a part of endopelvic fascia covers these muscles. Through its fascial connection to the visceral fascia, the pelvic viscera are indirectly attached to the bony pelvis.
1.1.1 The Ligaments of the Bony Pelvis (Fig. 1.1)
The sacrotuberous ligament stretches from the sacrum to the ischial tuberosity. The sacrospinous ligament extends from the ischial spine to the lower anterior aspect of the sacrum. The ligament is closely related to the coccygeus muscle which also stretches from the spine to the sacrum. In sacrospinous colpopexy, the vaginal wall is fixed to this ligament. The ligament is approached by dissecting between the rectum and the vagina upwards and backwards. Palpation of the ischial spine helps in identifying the ligament.
The ligament can be felt stretching from the spine medially and is widened as it goes medially. Bites from this ligament should be taken at about 2 finger breadths medial to the ischial spine in order to avoid injuries to the pudendal vessels and nerve which passes from behind the ligament and the spine. The inferior gluteal artery which goes posteriorly between the coccygeus muscle and the piriformis can also get injured.
Inguinal ligament: The inguinal ligament is formed by the folded lower edge of the aponeurosis of the external oblique muscle. It stretches between the anterior superior iliac spine and the pubic tubercle. Inferiorly it fuses with the fascia lata. Medially it forms the lacunar ligament. Below the inguinal ligament, the femoral vein, artery and the femoral nerve emerges into the thigh. The femoral vessels carry along with it an extension of the fascia, the femoral sheath. Medial to the vein is the femoral canal and lateral to the femoral vein is the femoral artery. The femoral nerve escapes to the thigh and lies outside the femoral sheath.
Lacunar ligament: Lacunar ligament is a triangular ligament which is formed by the deep fibres of the medial end of the inguinal ligament. The sharp lateral edges of the lacunar ligament lies in close apposition to the femoral canal.
Cooper's ligament: The Cooper's ligament is also known as the pectineal ligament. This is the fibrous tissue which stretches along the pectineal line. It is a thickening of the periosteum of the pubic bone. Medially it merges with the lacunar ligament. In Burch colposuspension, the paravaginal and the paraurethral fascia are attached to the Cooper's ligament.
1.2 THE VISCERAL FASCIA AND LIGAMENTS
1.2.1 Pelvic Connective Tissue
Pelvic cellular tissue fills the space between the peritoneum above and the pelvic diaphragm below. This extraperitoneal pelvic cellular tissue condensation forms the ligaments which has a role in supporting the pelvic viscera especially the uterus. Even though visceral connective tissue is continuous and interdependent, De Lancey described three levels of connective tissue support (Fig. 1.2).
Level I—Cervical and upper vaginal support: The cervix and the upper vagina are attached to the pelvic side wall by condensations of visceral pelvic connective tissue called uterosacral and cardinal ligaments (Mackenrodt's ligament).
The Mackenrodt's ligament (Cardinal ligament) primarily consists of perivascular connective tissue. It extends from the cervix and the upper vagina to the pelvic side wall. The ureter passes through a tunnel in this ligament during its course from behind forwards to the bladder. At this point the ureter is 1.5–2 cm lateral to the cervix. While clamping the ligament during hysterectomy, injury to the ureter should be avoided by applying the clamp close to the cervix. In type III hysterectomy the ureter is dissected from the ureteric tunnel and the Mackenrodts ligament is clamped and cut lateral to the ureter.
Fig. 1.2: Sagittal view of female pelvis showing the relation of pelvic viscera to endopelvic fascial attachments
Uterosacral ligaments attach the cervix to a broad area of the second and third piece of the sacrum and form the lateral boundaries of the posterior cul-de-sac.
Pelvic cellular tissue on either side of the cervix which harbors the uterosacral and the cardinal ligaments is called the parametrium. The parametrium continues caudally as paracolpos around the vagina.
Level II—Mid-vaginal support: Arcus Tendineus Fascia Pelvis (ATFP) stretches from the pubis to the ischial spine. The anterior vaginal wall is supported by the attachment of the pubovesicocervical fascia to the ATFP. The so called pubovesicocervical fascia is actually the adventitia of the vaginal wall which is made of collagen and elastin and separates the vagina from the bladder and urethra. It should be correctly named as vaginal adventitia. Laterally, this vaginal adventitia is attached to the ATFP and levator ani. The attachment to the levator ani is responsible for bladder neck elevation during increased intra-abdominal pressure. Failure of midvaginal support results in cystocele, rectocele and stress urinary incontinence. Detachment of the fascia from the ATFP results in lateral cystocele. Defects in the middle portion of the fascia results in midline cystocele. Fascial defect at the level of the urethro-vesical junction results in descent of the bladder neck and stress urinary incontinence. The layer of connective tissue intervening between the rectum and vagina is the rectovaginal septum originally described as Denonvillier's fascia. This fascia is attached inferiorly to the perineal body.
Level III—Distal vaginal support: Anteriorly the vagina is attached to the urethra. Laterally it is attached to the pubovaginalis muscle and perineal membrane and posteriorly to the perineal body. In women where perineal body is deficient due to previous obstetric trauma, it can result in gaping introitus and fecal incontinence.
1.2.2 Muscles
The muscles of the pelvis (Figs 1.3 to 1.5) include those of the lateral wall of the pelvis and the pelvic floor. The pelvic floor muscles form an important support for the pelvic viscera. The pelvic diaphragm is the most important structure supporting the pelvic contents. This is a funnel shaped fibromuscular structure composed of the levator ani and the coccygeus muscles along with its covering fasciae.
Levator Ani
The levator ani is the most important support for the pelvic viscera. The muscle complex with its superior and inferior fascial coverings forms the pelvic diaphragm. The urethra, vagina and the anal canal passes through the levator ani which supports these structures. Levator ani is in a constant state of contraction. The tone of contraction will be adjusted depending upon the changes in the intra-abdominal pressure. This helps in reducing the strain on the ligaments which support the pelvic viscera. The muscle originates from the posterior wall of the pubic bone and the tendinous arch (white line) which extends from the pubis to the ischial spine, on the medial side of the obturator internus muscle. The levator ani muscle ends in the vaginal wall, wall of the anal canal, central tendon of the perineum, anococcygeal ligament and coccyx. The muscle includes the pubococcygeus, puborectalis and the iliococcygeus.
The iliococcygeus arise from the arcus tendineus fascia and the ischial spine. The muscle of one side joins that of the other side in the anococcygeal raphi and thus the coccyx.
The puborectalis is the portion of levator ani which arises from either side of pubic bone and form a U-shaped sling behind the ano-rectal junction. It aids in defecation and maintains fecal continence.
Fig. 1.3: View of the pelvic floor from above showing the relation of the muscles of the pelvic floor to the pelvic viscera and pelvic bone
By contracting it compresses the anal canal and obliterates it. The nerve supply is by separate branches of S3 and S4. This is called the inferior rectal nerve. In posterior colpoperineorrhaphy, the muscle is plicated in the midline. This procedure is criticized recently as it is alleged to cause dyspareunia.
The pubococcygeus can be divided into pubovaginalis, puboperinealis and puboanalis. Pubovaginalis elevates the vagina during increased intra-abdominal pressure. There is no direct attachment to the urethra, but contractions of pubovaginalis during increase in intra-abdominal pressure elevate the urethra and helps maintain continence. The puboperinealis are the fibres which are attached to the perineal body. The puboanalis is attached to the anal canal between the external and the internal anal sphincter. Contraction of this portion of the muscle causes elevation of the anal canal and helps to close it during increased intra-abdominal pressure and keeps the urogenital hiatus closed.
The Levator Plate
The levator plate lies between the anus and the coccyx and is formed by the tendinous portion of the iliococcygeus muscle. The rectum, upper vagina and the uterus rest on this. When the levator plate is normally supported, it lies in 6a horizontal position. When the woman is standing, the upper vagina and rectum rests on it. Injuries to levator plate, the commonest cause being child birth, leads to sagging of levator plate and widening of the genital hiatus (Refer Pelvic Organ Prolapse). The levator muscle is supplied by separate branches of S2,4 and 5 whereas the external anal sphincter and the urethral sphincter are supplied by the pudendal nerve. This explains the reason why several women with significant prolapse do not have incontinence and vice versa.
Coccygeus
The coccygeus muscle originates from the ischial spine and the sacrospinous ligament to get inserted to the lateral margin of the 5th sacral vertebra and the coccyx.
1.3 UROGENITAL DIAPHRAGM (PERINEAL MEMBRANE)
The perineal membrane is the fibromuscular connective tissue sheet that stretches between the ischiopubic rami to the distal urethra and vagina. Thus it supports the distal vagina and urethra by indirectly attaching to the bony pelvis. Above this sheet of fibromuscular tissue lies the urogenital sphincter complex. The urogenital sphincter complex consists of the rhabdosphincter and two strap muscles,- the compressor urethrae and urethrovaginal sphincter. The compressor urethrae and the urethrovaginal sphincter were originally named as the deep transverse perineal muscle. The muscle originates from the ischiopubic rami and is supplied by S2,3,4 (pudendal nerve).
Sphincter urethrae (rhabdosphincter) also arise from the medial aspect of ischiopubic rami and get attached to the lower half of the urethra and the vagina. It is a voluntary compressor of the urethra. It is also supplied by the pudendal nerve. The urogenital diaphragm reinforces the pelvic diaphragm. It is intimately related to the vagina and urethra below the level of the levator ani.
1.4 THE PERINEUM
The perineum is the lower most part of the trunk between the buttocks. It is diamond shaped and it extends from the lower margin of the pubic symphysis anteriorly, to the tip of the coccyx posteriorly and the ischial tuberosities laterally. This space can be divided into an anterior urogenital triangle and a posterior anal triangle by an imaginary line extending between the ischial tuberosities which pass across the perineal body.
The Urogenital Triangle
The external genital structures, the vulva and the urethral openings are situated in the urogenital triangle. Behind these external structures lie the superficial and the deep perineal spaces.
1.4.1 The Superficial Perineal Space
This space lies between the deep fascia of the perineum and the perineal membrane. The superficial perineal muscles, the bulb of the vestibule and the vestibular glands occupy this space. The bulbospongiosus muscle extends from the perineal body posteriorly to the dorsal aspect of the clitoris. It is a sphincter of the vagina. The bulb of the vestibule is a 3 cm long highly vascular structure surrounding the vestibule and located under the bulbocavernosus muscle. The muscle compresses the vestibular bulb (Fig. 1.6).
The ischiocavernosus muscle originates from the ischial tuberosity and gets inserted to the ischiopubic rami.
The superficial transverse perineal muscle originates from the ischial tuberosity and is inserted to the perineal body. Pudendal nerve supplies all these muscles.
Fig. 1.6: Pelvic diaphragm viewed from below showing superficial perineal muscles and the perineal membrane
Laterally the ischiorectal fossa intervenes between the pelvic diaphragm and the bony pelvis. The fossa on one side is continuous with that of the other side through the posterior aspect. Hence pus from one ischiorectal fossa can track to the opposite side.
The Greater Vestibular Glands (Bartholin's Gland)
These glands are situated one on either side of the vestibule behind the posterior end of the bulb of the vestibule. The glands drain through a duct into the vestibule at a point which corresponds to the junction of the posterior 1/3rd and the anterior 2/3rd of the labia minora. The opening is situated between the hymen and the labia minora. Mediolateral episiotomy should always start from the midline and proceed laterally. If the initial cut is a bit lateral, it may injure the Bartholin's gland duct and the bulb of the vestibule which can cause primary hemorrhage, hematoma formation, gaping of episiotomy wound as well as infection.
1.4.2 Deep Perineal Space
The deep perineal space lies above the level of the urogenital diaphragm. Urogenital sphincter complex which lies above the perineal membrane consists of
- The external urethral sphincter which surrounds the middle 1/3rd of the urethra
- The compressor urethrae which arches across the ventral aspect of the urethra
- The urethrovaginal sphincter which surrounds the ventral aspect of the urethra and terminate in the lateral wall of the vagina.
1.4.3 Perineal Body (Central Tendon of the Perineum)
The perineal body is a pyramidal structure which lies posterior to the lower 1/3rd of the vagina with its apex cephalad. It is formed by the decussation of the superficial muscles of the perineum, the bulbospongiosus, the external anal sphincter, the anterior fibres of levator ani and the superficial transverse perineal muscle. Tearing or stretching of the perineal body during child birth interferes with the support of the lower part of the posterior vaginal wall leading to prolapse and/or fecal incontinence. Hence, tearing of muscles of the perineal body during child birth should be properly repaired.
1.4.4 Blood Supply
The perineum is supplied by the pudendal artery which is the terminal branch of the internal iliac artery. The venous drainage is by the corresponding vein to the internal iliac vein.
1.4.5 Lymphatic Drainage
Superficial and deep compartments drain to the internal iliac group of nodes. Lymphatics of the perineal structures including the lower part of anal canal, vagina and urethra drain to the inguinal lymph nodes. Lymph from the upper part of these viscera drains superiorly into the pelvis.
1.4.6 Nerve Supply
The cutaneous innervation of the vulva is by the branches of the ilioinguinal, genital branch of the genitofemoral and perineal branch of the lateral femoral cutaneous nerve of thigh. The pudendal nerve supplies the muscles of the superficial and deep perineal compartments.
1.4.7 Imaging of the Pelvic Floor
Magnetic resonance imaging can image the levator ani muscle. But the recent introduction of 4D imaging of the pelvic floor muscles has largely replaced MRI.
1.5 THE PELVIC URETER
The gynecologic surgeon should be thorough with the anatomy of the urinary tract due to its close proximity with the ovary, uterus and vagina.
The ureter is 25–30 cm long half of which is in the abdomen and the rest in the pelvis. After emerging from the renal pelvis it courses downward retroperitoneally over the psoas muscle. It enters the pelvis over the bifurcation of the common iliac vessels (Fig.1.7). It then passes posteromedially along the anterior border of the greater sciatic notch in the ovarian fossa and then anteriorly and forwards below the uterine artery. During its course anteromedially, the ureter lies in the substance of the Mackenrodt's ligament (ureteric tunnel) which is about 1.5–2 cm lateral to the cervix. Emerging from the ligament it is in relation to the anterolateral aspect of the vagina (vaginal vault).
The left ureter is more extensively related to the vault than the right due to the dextrorotation of the uterus; the reverse can also happen when the uterus is levorotated. On entering the bladder the ureter courses for about 1.5 cm in the muscular wall of the bladder. The two ureteric openings are about 5 cm apart in a distended bladder and 2.5 cm apart in a non-distended bladder. The blood vessels supplying the ureter are branches from the common iliac, internal iliac, uterine and the vesical arteries which form a plexus in the connective tissue covering of the ureter.8
During pelvic surgery the ureter can be identified as it crosses the pelvic brim over the bifurcation of the common iliac. The presence of peristalsis, absence of pulsations and the characteristic feel of quill help in identification of the ureter. When the ureter is caught with the finger and thumb and slipped, it will go with a snap sound which is characteristic. During internal iliac artery ligation the ureter should be identified at the pelvic brim and peritoneum lateral to the ureter should be incised at the level of bifurcation of the common iliac vessels. The ureter with the attached peritoneum should be reflected medially to expose the internal iliac vessels. This will help preserve the blood supply to the ureter.
The ureter is at risk of injury while clamping the infundibulo-pelvic ligament and while clamping and cutting uterine vessels during hysterectomy. The risk of injury is more especially when the anatomy is distorted. In severe endometriosis and in situations where ovarian tumor or fibroid burrows retroperitoneally, the ureter will not be seen in its normal position. In these instances the ureter should be identified by palpation. In severe endometriosis with extensive pelvic adhesions, difficulty in identification of the ureter should be anticipated. Preoperative stenting of the ureter preferably with an illuminated stent would help in identification.
During uterosacral ligament fixation of the vault, the sutures taken higher up are likely to involve the pelvic ureter. Hence cystoscopy should be performed during the procedure to exclude ureter ligation by looking for the ureteric reflux.
Wertheim's hysterectomy necessitates extensive dissection of the ureter predisposing to direct injury, avascular necrosis and fistula formation later on. To avoid this, the ureter should be identified from the pelvic brim and the attachment of the ureter to the medial peritoneal flap should be maintained up to the level of the uterosacral ligament. Afterwards, the ureter needs to be dissected from the Mackenrodt's ligament by opening the roof of the ureteric tunnel. Bleeding from vessels at this point should be meticulously controlled and inadvertent attempts to arrest hemorrhage by blind clamping should be avoided.
During hysterectomy for cervical fibroid, the ureter is likely to be injured because of its close proximity. Identification of the ureter would be easy if hysterectomy is preceded by myomectomy. Broad ligament fibroids will also displace the ureter laterally and can be very close to the tumor. Opening the leaf of the broad ligament will help removal of the fibroid without injuring the ureter.
During vaginal hysterectomy, bladder injury can occur while separating the bladder from the cervix. The portion injured will be near the trigonal area where the ureters traverse through the bladder wall. Suturing should be done after inserting ureteric catheters, lest the portion of the ureter in the bladder wall be likely to be incorporated in the suture.
1.6 THE PELVIC VISCERA
The relations of the pelvic viscera can be understood in the sagittal and coronal sections of the pelvis (Figs 1.8 and 1.9). The vagina extends from the vestibule to the uterus.9
The upper vagina is almost horizontal in the standing position and rests on the levator plate. The vaginal wall is composed of the following three layers:
- Vaginal epithelium: The vaginal epithelium is composed of non-stratified squamous epithelium without glands and hence the term vaginal mucosa is a misnomer. The epithelium has transverse ridges formed by the underlying muscular layer. The epithelium is sensitive to estrogen. Under estrogenic influence it undergoes proliferation and maturation in the reproductive period and later atrophy in the post menopausal period with absent or marked reduction of rugae.
- Muscle wall: Outer to the epithelium is the muscular wall of the vagina constituted by the inner circular and outer longitudinal layer.
- Adventitia: The portion of the endopelvic fascia covering the muscular wall of the vagina is the outermost covering of the vagina. Anteriorly, there is no definite supporting layer of endopelvic fascia between the vagina and bladder or urethra. However, thickening of the fascia, the Denonvillier's fascia is seen between the vagina and the rectum above the level of the perineal body.
The upper vagina is supplied by the cervical branches of the uterine; the midvagina by the vaginal artery, a branch of the internal iliac artery and the lower 1/3rd by the pudendal artery and the middle rectal artery. There is a rich anastamosis of vessels supplying the vagina. Multiple vaginal lacerations with uncontrolled bleeding, can be tackled by ligating the internal iliac arteries, as all the vessels supplying the vagina originate from the internal iliac artery.
The upper vagina is innervated by the presacral plexus and the lower vagina by the pudendal nerve.
1.6.1 Uterus
The uterus consists of the uterine body (corpus) and the cervix. The portion of the corpus above the attachment of the round ligament is the fundus. Between the body of the uterus and the cervix is the isthmus. The uterine corpus is covered by peritoneum which is closely adherent to the underlying myometrium of the body of the uterus. Anteriorly, it covers the isthmus and gets reflected (Fig. 1.10) on to the dome of the bladder—uterovesical fold of peritoneum. The uterovesical fold of peritoneum is loosely attached to the isthmus of the uterus with intervening areolar tissue. In abdominal hysterectomy, this loose fold of peritoneum is incised and the urinary bladder with the peritoneum is separated from the cervix before clamping the uterine arteries. Posteriorly, the peritoneum is closely attached to the lower uterine segment, the cervix and the upper vagina and then gets reflected on to the rectosigmoid.
The size of the uterus depends upon the age and reproductive status. The body to cervix ratio is 1:1 in childhood; after puberty, the size of the uterine body increases and the corpus to cervix ratio become 3:1 in the child bearing age group. After menopause the cervix atrophies and become flushed with the vaginal vault.
The corpus and cervix are not usually in the same vertical plane. When the corpus is anteriorly angled with the cervix, it is anteflexion and when it is posteriorly angled, it is retroflexion. The long axis of the vagina and the long axis of the uterus are also not in the same vertical plane. When the long axis of uterus is directed anteriorly, it is anteversion and when it is posteriorly directed, it is retroversion.
1.6.2 Fallopian Tube
The fallopian tubes are tubular structures extending from the cornua laterally. It represents the unfused ends of the Mullerian duct. They usually measure about 10cms in length. The fallopian tube can be differentiated into four regions:
- Interstitium: This is the narrowest portion of the tube and the lumen measures <1 mm in diameter. It is the intramuscular portion of the fallopian tube and starts from the tubal ostia.The direction of the interstitial portion of the tube varies in different individuals.
- Isthmus: This is the narrow segment of the tube which is close to the uterine wall. In female sterilization, the fallope ring or the Hulka clip should be inserted in this region of the tube as failure rate will be less and the chance of successful recanalisation better. This is because recanalisation can be done without luminal disparity if tubotubal anastamosis is done in the isthmial region of the tube.
- Ampulla: This is the longest portion of the tube and is broader than the isthmial region. Fertilization usually takes place in the ampullary region of the tube. This is a common site for ectopic pregnancies.
- Infundibulum/fimbrial region: This is the funnel shaped portion of the tube which opens into the peritoneal cavity. It has numerous finger-like projections which aid in ovum pick up. One fimbria, the fimbria ovarica, is longer and extends to the ovary.
The tube is lined by ciliated columnar epithelium which, along with the peristaltic movement helps in the transport of ovum, sperm and zygote. The muscular wall of the tube consists of inner circular and outer longitudinal layers. The peritoneum of the broad ligaments covers the fallopian tube and is called the mesosalpinx.
The fallopian tube is supplied by uterine and ovarian arteries which form an arterial arcade in the mesosalpinx parallel and below the tube.
1.6.3 Ovaries
The ovaries are situated between the pelvic side wall and the uterus in the ovarian fossa. The double fold of peritoneum which attaches the ovary to the pelvic side wall is the infundibulopelvic ligament. The ovarian artery, which is a branch of the aorta enters the ovary through this ligament. Hence while doing ovariotomy, the pedicle should be carefully ligated especially in the presence of an ovarian tumor where the vessel will be enlarged. The fold of peritoneum which attaches the ovary to the posterior leaf of the broad ligament is called the mesovarium. The medial end of the ovary is attached to the upper and posterolateral aspects of the uterus with the help of the ovarian ligament which is developed from the gubernaculum of the ovary.
The size of the ovary varies with age and functional status. The ovarian size is less in women who are on medication for ovulation suppression and more in those who are on ovulation induction. The normal ovary in the child bearing age group measures 4 × 3 × 2 cm. On cut section the ovarian substance can be differentiated into outer cortex and inner medulla. The cortex harbors the follicles. The medulla which is only a small portion of the ovary near the hilar region is composed of fibromuscular tissue and blood vessels. The peritoneum of the mesovarium is continuous with the outer covering of the ovary which is made up of cuboidal low columnar epithelium.
1.6.4 Urinary Bladder
The urinary bladder occupies the anterior compartment of the pelvis. It is located behind the pubic bone anterior to the cervix and the vagina. The parietal peritoneum gets reflected from the anterior abdominal wall to the dome of the bladder. From the dome of the bladder the peritoneum is reflected on to the isthmus of the uterus. The wall of the bladder which is close to the vagina and cervix is called the trigone of the bladder. During vaginal hysterectomy, the bladder can get injured while separating it from the cervix. Since the portion injured can be near to the ureteral orifice, suturing the bladder defect can occlude the intramuscular portion of the ureter. Hence ureteric stenting is mandatory during the repair of such defects (Figs 1.11 and 1.12).
Retroperitoneal Spaces
The space between the peritoneum of the pelvis above, the pelvic diaphragm below and the bony pelvis on the sides can be divided into potential spaces by the pelvic viscera and the ligaments. These are described below.
Fig. 1.11: Diagram showing speculum retracting the bladder from the cervix after cutting the vesicocervical ligament during vaginal hysterectomy. As the bladder is pushed and retracted, the ureter will be away from the uterine artery which can be clamped close to the cervix to avoid injury to the ureter
Prevesical Space (Cave of Retzius)
This is the space between the anterior surface of the bladder and pelvic surface of the pubic bone. It is filled with loose fatty tissue- the retropubic pad of fat. The space is limited inferiorly by the pubourethral ligaments which pass to the lower part of the bladder. Superiorly the space is continuous with the loose extra peritoneal tissue which extends up to the anterior abdominal wall to the level of the umbilicus. Because of this anatomy, the bladder can expand superiorly between the anterior abdominal wall and its peritoneum, up to the level of umbilicus.
In Burch colposuspension the cave of Retzius is entered by separating the bladder and urethra from the pubic symphysis. The medial part of the inguinal ligament, the lacunar ligament and the iliopectineal ligament are identified. The lateral fornix of the vagina is pushed from below and three series of bites are taken from the vaginal adventitia lateral to the bladder, urethrovesical junction and upper urethra and anchored to the iliopectineal ligament with non absorbable or delayed absorbable sutures. Lateral to the lacunar ligament the femoral canal and the femoral vein will be seen and care should be taken not to injure the vein.
While doing TVT insertion for stress urinary incontinence, the ends of the tape are inserted on either side of the mid urethra and traversed through the retropubic space upwards to emerge on either side of the midline about 2.5 cm apart. As the tape is passed through the retropubic space the urinary bladder can be inadvertently injured. However keeping close to the pubic bone will avoid such occurrence. While the tape emerges through the lower abdomen, the inferior epigastric vessels are likely to be injured, which can be avoided by keeping the distance between the emergences of the tape at 2.5 cm.
The trans-obturator tape is maneuvered to emerge through the obturator membrane lateral to the ischio-pubic rami. More lateral and upward steering of the tape can injure the obturator neurovascular bundle.
Paravesical Space
Paravesical space lies between the pelvic diaphragm laterally, the bladder pillar medially, endopelvic fascia inferiorly and the lateral umbilical ligament superiorly.
Vesicovaginal Space
Vesicovaginal space is the space lying between the bladder anteriorly and vagina posteriorly.
Rectovaginal Space
Rectovaginal space lies between the rectum and the vagina and extends from the superior border of the perineal body to the peritoneum of the pouch of Douglas. The rectovaginal septum forms the upper and anterior wall of the space. The rectal wall forms the posterior boundary.
Para-rectal Space
Pararectal space is bound by the levator ani laterally and medially by the fascia covering the rectum (rectal pillar).
Retro-rectal Space
This space lies between the rectum anteriorly and the anterior aspect of the sacrum posteriorly.
Presacral Space
Presacral space is the superior extension of the retrorectal space. The middle sacral vessels and hypogastric plexus lies in the loose areolar tissue of the space. In presacral neurectomy, the space is opened. Care should be taken not to injure the presacral vessels during the procedure.
1.7 BLOOD VESSELS OF THE PELVIS
The blood vessels supplying the pelvis are shown in Figure 1.13. The pelvic organs are supplied by the branches of the internal iliac artery. The common iliac artery bifurcates into external and internal iliac arteries over the sacroiliac joint. The external iliac artery courses over the psoas muscle, into the thigh behind the inguinal ligament and is in line with the common iliac artery. The internal iliac artery turns sharply medially and downwards and divides into anterior and posterior branches.13
The posterior division escapes through the greater sciatic foramen into the gluteal region to supply the gluteus muscle. The anterior division supplies the pelvic viscera and gives off the following branches.
The obturator is the initial branch of the anterior division. It courses through the pelvic side wall along with the obturator nerve and escapes through the obturator fossa. The obturator group of nodes are in relation to the vessel in the obturator fossa. During pelvic lymphadenectomy the obturator node should be removed carefully since serious hemorrhage can be encountered at this site.
The other branches are the uterine, vesical, vaginal, inferior gluteal and the internal pudendal.
Uterine Artery
The uterine artery arises as a branch of the anterior division of the internal iliac artery. It supplies the uterine body, the uterine cervix, the fallopian tubes, and the upper part of the vagina. It gives off two main branches as it crosses anterior to the ureter (Fig. 1.14). From its origin, the uterine artery crosses the ureter anteriorly in the broad ligament before branching at the level of the uterus. One of the major branches passes superiorly over the uterus in a tortuous manner within the broad ligament until it reaches the region of the ovarian hilum where it anastomoses with branches of the ovarian artery. Another branch descends over the uterus to supply the cervix and anastomoses with the branches of the vaginal artery to form two median longitudinal vessels, the azygos arteries of the vagina, which descend anterior and posterior to the vagina. Although there are anastomoses with the ovarian and vaginal arteries, the dominance of the uterine artery is indicated by its marked hypertrophy during pregnancy.
Each uterine artery gives off numerous branches which are also tortuous. These enter the uterine wall, divide and run circumferentially as groups of anterior and posterior arcuate arteries. The branches narrow as they approach the midline and hence the midline of the uterus is less vascular. The left and right arterial arteries anastomose across the midline and unilateral ligation can be performed without serious effects. The arcuate arteries give off radial branches, which pass centripetally through the deeper myometrial layers to reach the endometrium. Terminal branches in the uterine muscle called helicine arterioles are also tortuous. From the arcuate arteries many helical arteriolar rami pass into the endometrium. In the proliferative phase of menstrual cycle, helical arterioles are less prominent, whereas they grow in length and caliber, becoming even more tortuous in the secretory phase.
1.8 NERVE SUPPLY TO THE PELVIC VISCERA
Fig. 1.14: Relation of uterine artery to the ureter. Note the tortuosity typical of the uterine artery
The ovaries and fallopian tubes are supplied by the ovarian plexus which originate from the aortic plexus and accompany the ovarian vessels. Thus the parasympathetic supply to the ovary and lateral part of the fallopian tube is from the vagus nerve. The uterine nerve supply comes from the superior hypogastric plexus which lies in the areolar tissue over the 5th lumbar vertebra and sacral promontory. The plexus is in close relation to the presacral artery and is constituted by 2–3 incompletely fused nerve trunks. It is formed of post ganglionic fibres from higher sympathetic ganglia and sacral sympathetic trunk along with visceral afferents. The superior hypogastric plexus thus formed divides into two nerve trunks named as the hypogastric nerves. These nerves proceed to the inferior hypogastric plexus which are located in the pelvic side wall in relation to the internal iliac vessels. The parasympathetic supply to the pelvic organs is from S2,3,4 segments which joins the inferior hypogastric plexus. Thus the inferior hypogastric plexus carries both sympathetic and parasympathetic nerves to the bladder, urethra, rectum, uterus, vagina, clitoris and vestibular bulbs. These nerve fibers are distributed along the blood vessels which supply these organs. The sensory afferent fibers from these organs course through the same pathway.
In presacral neurectomy, a portion of the presacral nerve is dissected and removed at the region of the sacral promontory. Care should be taken to avoid injury to the presacral artery. Presacral neurectomy can interfere with bladder and bowel function as the nerve supplies these organs as well. Hence the alternative procedure advocated is resection of a portion of uterosacral ligament so that interference with bladder and bowel function can be prevented.
1.9 LYMPHATIC DRAINAGE OF THE PELVIS AND THE PERINEUM
Lymphatic Drainage of the Uterus and Cervix
The important group of nodes draining the uterus and adnexa are:
- Internal iliac
- External iliac
- Common iliac
- Sacral group
- Inguinal group
- Pre and para-aortic group
The internal iliac group of nodes: These are found surrounding the internal iliac artery and its branches. They lie in the adipose tissue in between its main branches. The largest and most numerous lie on the lateral pelvic wall, but may be found adjacent to the viscera.
The external iliac group of nodes: They are around 8–10 nodes usually arranged in lateral, anterior and medial groups. The medial group drains the upper vagina and cervix uteri.
Common iliac nodes: Four to six nodes arranged in medial, lateral and intermediate group. Grouped around the artery one or two are found inferior to the aortic bifurcation, anterior to the fifth lumbar vertebra and sacral promontory.
Sacral nodes: This group of nodes found along the medial and lateral sacral vessels, one group in the obturator canal along the obturator artery.
Pre aortic nodes: Lies anterior to the abdominal aorta and receive efferents from the common iliac group of nodes.
1.10 ANTERIOR ABDOMINAL WALL
The muscles of the abdominal wall are:
- Rectus abdominis: The muscle arises from the pubic symphysis and its superior ramus and gets inserted on to the anterior surface of the xiphisternum and the cartilage of 5th-7th ribs.
- External oblique muscles: It originates from the outer surface of 5th-12th rib and is directed downwards, forwards and medially to get inserted on to the iliac crest and pubic tubercle and the free inferior border forms the inguinal ligament.
- Internal oblique muscles: Originates from the anterior 2/3rd of iliac crest and inguinal ligament and gets inserted on to the inferior border of the 10th-12th rib.
- Transversus abdominis: Originate from the lower 6 ribs, thoracolumbar fascia, iliac crest and lateral 1/3rd of inguinal ligament. It joins the aponeurosis of the internal oblique and forms the linea alba. The inferior fibres join with the internal oblique forming the conjoint tendon which forms the roof and posterior wall of inguinal canal.
- Pyramidalis: It is a small triangular muscle seen medial and anterior to the lower part of the rectus muscle above the pubic symphysis.
The Rectus Sheath (Figs 1.15A and B)
The aponeuroses of the external oblique, internal oblique and the transverses abdominis join together at the lateral border of rectus muscle and splits into anterior and posterior sheath to enclose the rectus muscle. The two layers fuse in the midline to form the linea alba. Below the arcuate line, all three layers are anterior to the rectus muscle. Hence below the arcuate line the rectus sheath is applied to the transversalis fascia and the peritoneum.
The inferior epigastric vessel (Fig. 1.16) which originates from the external iliac runs superiorly between the peritoneum and the muscle layers of the abdominal wall. It is vulnerable to damage by accessory trocar while performing laparoscopic surgery. Because of its deeper location it cannot be trans-illuminated, but can be identified by locating the lateral umbilical ligament intra-abdominally. The artery will be seen lateral to the lateral umbilical ligament. Hence the accessory trocar entry should be either medial to the lateral umbilical ligament or far lateral to it. In low transverse incisions, it can be injured if the extent of the incision goes far laterally.
Fig. 1.16: Laparoscopic view of inferolateral anterior abdominal wall showing the relation of inguinal canal, inferior epigastric artery and lateral umbilical ligament. The lateral umbilical ligament is formed by the obliterated umbilical artery which lies medial to the inferior epigastric artery
1.11 CONCLUSION
Understanding relevant anatomy is a must for all gynecologic surgeons. Learning anatomy should be an ongoing process which should begin while assisting experienced surgeons and should be periodically reviewed by dissecting cadaveric specimens when newer techniques are adopted. The surgeon should be able to identify the different structures by their characteristic appearance and feel because distortion of anatomy can be encountered very often. Complications of surgery can be prevented to a great extent if the surgeon is thorough with the anatomy and is able to identify the different structures by their nature.