Teaching is only demonstrating that it is possible, Learning is making it possible for yourself.
ANATOMY OF FEMALE GENITAL TRACT
An understanding of the anatomy of the female pelvis, internal and external genitalia and related structure is crucial to have clear concept of the subject of obstetrics and gynecology. It is also important to appreciate that while the basic facts of anatomy remains the same. Our understanding of specific anatomic relationship and the development of new clinical and surgical correlation continues to evolve.
Anatomy of External Genitalia
Urogenital triangle includes the external genital structure and the urethral opening. These external structures cover the superficial and deep perineal compartments and are known as vulva.
Vulva
Vulva is an ill defined area which comprises the whole of the external genitalia and conveniently includes the perineum. It is bounded anteriorly by the mons veneris (Pubis), laterally by the mons pubis and posteriorly by the perineum (Fig. 1.1).
Mons pubis: It is a traingular eminence in front of pubic bones that consist of adipose tissues covered by hair bearing skin up to its junction with the abdominal wall.
Labia majora: Labia majora is a pair of fibroadipose folds of skin that extend from mons pubis, downward and backward to meet in midline in front of the anus at the posterior fourchette. They are best developed in child-bearing period of life. In prepubertal children and in postmenopausal women the amount of subcutaneous fat in the labia majora is relatively small and the cleft between labia is prominent.
They include the terminal extension of the round ligament and occasionally a peritoneal diverticulum—the canal of Nuck. Labia majora are covered by skin with scattered hairs and are rich in sebaceous, apocrine and exocrine glands which produces a characteristic aroma and from which the rare tumor of hidreadenoma of the vulva is probably derived.
The adipose tissue is richly supported with venous plexus which may produce hematoma, if injured during childbirth. The labia majora are homologous with the scrotum in the male.
Labia minora: The labia minora are the folds of skin which lie on the inner aspect of the labia majora with which they merge posteriorly to form fourchette and are separated into two folds as they approach the clitoris anteriorly. The anterior folds unite to form the prepuce or hood of the clitoris and posterior fold form the frenulum of the clitoris as they attach to its inferior surface. Fourchette is a thin fold of skin, indented on separation of labia and is often torn during childbirth. Labia minora are covered by hairless skin overlying a fibroelastic stroma rich in neural and vascular elements. The area between the posterior labia minora forms the vestibule of the vagina.
4Clitoris: It is a small cylindrical erectile organ measuring 2–3 cm in length. It consists of two crura and two corpora cavernosa and is covered by sensitive rounded tubercle (the glans). It is attached to undersurface of the symphysis pubis by the suspensory ligaments. It is an analog to penis in the male.
Vestibule: Vestibule is the space lying between the anterior and inner aspects of the labia minora and is bounded posteriorly by the vaginal introitus.
Vaginal orifice: Vaginal orifice is surrounded by the hymen, a variable crescentic mucous membrane that is replaced by rounded caruncle after its rupture. The opening of the duct of greater vestibular (Bartholin) gland is located on each side of the vestibule.
Urethral orifice: It is situated in the midline just in front of the vaginal orifice about 2–3 cm beneath the clitoris. The Skene (Paraurethral) gland duct presents an opening on its posterior surface.
Bartholin's gland: Bartholin's glands are two in number and are homologous to Cowper's gland in the male. They lie posterolaterally to the vaginal orifice embedded in the posterior part of the vestibular bulb, one on either side.
The gland measures about 10 mm in diameter and lies near the junction of the middle and posterior thirds of the labia majora. The duct of the gland is about 25 mm long and runs downwards and inwards to open at the introitus below hymen but above the attachment of the posterior end of labium minor.
It is normally impalpable when healthy but can be readily palpated between finger and thumb when enlarged by inflammation. The gland is lobulated and racemose, the acini being lined by a single layer of low columnar or cuboidal cells. The duct is lined by multilayered columnar cells but near its opening by stratified squamous epithelium (Fig. 1.2). The function of the gland is to secrete lubricating mucus during coitus. The Bartholin's gland corresponds to the bulbourethral glands of male.
Vestibular bulb: There are bilateral elongated masses of erectile tissue situated beneath the mucous membrane of the vestibule. They are homologous to the single bulb of the penis and corpus spongiosum in male. Each bulb lies on either side of the vaginal orifice in front of the Bartholin's gland and is incorporated with the bulbocavernosus muscle. They are likely to be injured during childbirth with brisk hemorrhage.
Vascular Connexion of Vulva
All the tissues of the vulva are highly vascular so even a minor operation in that area should not be attempted except in well-equipped settings:
- Arterial: The vulva is mainly supplied by branches of internal pudendal artery—labial, transverse perineal artery to the vestibular bulb and deep and dorsal arteries to the clitoris. Internal pudendal artery is one of the terminal branches of the internal iliac artery. Its four parts are also served by the superficial and deep pudendal arteries which are branches of femoral artery.
- Veins: Some veins accompany corresponding arteries to the internal pudendal veins, those of the clitoris and bulb link with the vesical and vaginal plexus. The long saphenous vein also takes a share of venous return so its ligation can improve vulvar varicosities.
- Lymphatics: Lymphatic drainage is mainly to the superficial inguinal nodes and hence to the deep inguinal and external iliac nodes. Lymphatics from the deep tissues accompany the internal pudendal vessels to the internal iliac nodes.
Nerve Supply of Vulva
The skin of the mons veneris and the foreparts of the vulva are supplied by ilioinguinal nerve and the genital branch of the genitocrural nerve and the posteroinferior part by the pudendal branch from the posterior cutaneous nerve of thigh. Between these two groups the vulva is supplied by the labial and perineal branches of the pudendal nerve. The pudendal nerve supplies sensory fibers to the skin of the vulva, external urethral meatus, clitoris, perineum and lower vagina. It provides motor fibers to all the voluntary muscles including the compressor urethra, sphincter vaginae, levator ani and external anal sphincter. The skin of vulva is very sensitive and perineal injuries are especially painful. The discomfort which results from perineorrhaphy or episiotomy is mostly due to spasm in the underlying muscle.
Internal Genital Organs
The internal genital organs in female include vagina, uterus, fallopian tubes and ovaries.
Vagina
The vagina is a hollow fibromuscular tube extending from the vulvar vestibule to the uterus. In the dorsal lithotomy position the vagina is directed posteriorly toward the sacrum but its axis is almost horizontal in the upright position. Vagina communicates interiorly with the uterine cavity and exteriorly with the vulva. It constitutes the excretory channel for the uterine secretion and menstrual blood. It is organ of copulation and for birth canal at parturition.
Vagina has anterior, posterior and two lateral walls. Vagina is attached at higher point posteriorly than anteriorly, the anterior wall measures 7 cm. The vaginal portion of the cervix projects into its upper end and forms the anterior, posterior and lateral fornices. The depth of fornices depends upon the development of the portio vaginalis of the cervix. In prepubertal girls and in elderly women where uterus is small the fornices are shallow, while in women with congenital elongation of the portio vaginalis of the cervix, the fornices are deep.
Posterior vaginal fornix is separated from the posterior cul de sac and peritoneal cavity by the vaginal wall and peritoneum. This proximity is clinically useful for diagnostic procedure of culdocentesis* and therapeutic procedure of posterior colpotomy (Fig. 1.3).**
The vagina is attached to the lateral pelvic wall with endopelvic fascial connection to the arcus tendinous (white line) which extends from the pubic bone to the ischial spine. This connection converts the vaginal lumen into the transverse slit with the anterior and posterior walls in opposition and lateral space where the two walls meet in the vaginal sulcus.
The opening of the vagina may be covered by a membrane or surrounded by a fold of connective tissue called hymen. This tissue is usually replaced by irregular tissue tags later in life after resumption of sexual activity and childbirth.
Vagina is not of uniform caliber. The lower vagina is a little constricted as it passes through the urogenital hiatus in the pelvic diaphragm. The upper vagina is more spacious. However, the entire vagina is characterized by its distensibility which is most evident during child- birth.
Relations of vagina: Vagina is closely applied anteriorly from below upward to—urethra, bladder neck and trigonal region. Posteriorly, the vagina is in relationship with perineal body, anal canal, lower rectum and posterior cul de sac from below upward.
Vagina is separated anteriorly from the lower urinary tract and posteriorly from gastrointestinal tract by their investing layers of fibromuscular elements known as the endopelvic fascia. Laterally, vagina is related from below upward—cavernous tissue of the vestibule, the superficial muscles of the perineum, the triangular ligament, and at about 2.5 cm from the introitus—the levator ani, lateral to which is the ischiorectal fossa. Above the levator lies the condensation of endopelvic fascia called Mackenrodt's ligament on either side. The ureter traverses this tissue in the ureteric canal and is about 12 mm anterolateral to the lateral fornix.
Superior relation: The cervix has its four fornices—anterior, posterior and two lateral. Lateral fornices are related to the uterine vessels, Mackenrodt's ligament, and the ureter. Posteriorly surrounds the pouch of Douglas where lie the uterosacral ligaments, which can be identified on vaginal examination especially if thickened by disease, as endometriosis and cancer cervix.
Histology of Vagina
- Mucosa: It is nonkeratinized stratified squamous epithelium without glands, which consist of a basal layer of cuboidal cells, a middle layer of prickle cell and a superficial layer of cornified cells. Vaginal serration is derived primarily by transudation with contribution from cervical and Bartholin's gland secretions. Mucosa has a characteristic pattern of transverse ridges and furrows known as rugae. It is hormonally sensitive, responding to stimulation by estrogen with proliferation and maturation. The mucosa is colonized by mixed bacterial flora with lactobacilli predominant.Normal pH of vagina is 3.5-4.5 during reproductive life which is due to presence of lactic acid. This acidity inhibits the growth of pathogenic organism (Fig. 1.4). Doderlein bacilli is a gram-positive, rod shaped bacilli, which grows anaerobically on acid media. Its presence is dependent on estrogen. Its function is to convert the glycogen present in the vaginal mucosa into the lactic acid. Before puberty and after menopause due to estrogen deficiency, vaginal pH become alkaline and with deficiency of Doderlein bacilli, there is tendency for development of mixed organism infection in these age groups.
- Subepithelial layer is vascular and contains much erectile tissue.
- A muscle layer consist of a complex interlacing lattice of plain muscle which is external to subepithelial layer, loosely arranged in inner circular and outer longitudinal layers.
- Adventitia is endopelvic fascia, adherent to the underlying muscularis.
Blood Supply
Blood supply of vagina is from the vaginal artery and branches from the uterus, middle rectal and internal pudendal arteries.
Innervation
The upper vagina is innervated from the uterovaginal plexus and distal vagina from the pudendal nerve.
Uterus
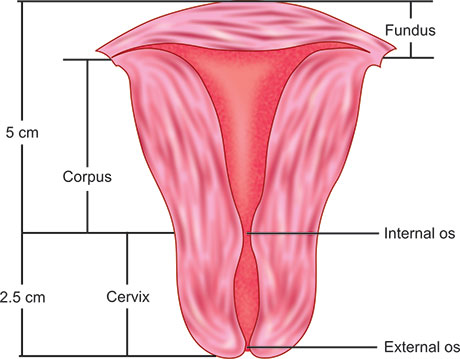
Uterus is a pear shaped fibromuscular hollow organ usually divided into a lower cervix and an upper corpus or uterine body.
Corpus (Body of Uterus)
The body of uterus varies in size and shape depending on hormonal and childbearing status. At birth the cervix and corpus are approximately equal while in adult women, the corpus is 2–3 times the size of cervix (Fig. 1.5). Before puberty the cervix to corpus ratio is 2:1. At puberty this ratio is reversed to 1:2 and during reproductive year, cervix to corpus ratio is 1:3 or even 1:4, after menopause, the organ atrophies and portio vaginalis may eventually disappear.
The position of the uterus in relation to other pelvic structure is variable and is generally described in terms of positioning—Anterior, Mid position or Posterior.
Flexion and Version
Flexion Flexion is the angle between the long axis of uterus corpus and the cervix. It is about 120°.
Version Version is the angle of junction of uterus with the upper vagina. It is about 90°. Normal position is one of the anteversion and anteflexion. In 15–20% of women uterus normally remains in retroverted position.
Body of uterus has got following parts (Fig. 1.6):
- Isthmus or lower uterine segment: It is the area where endocervical canal opens into the endometrial cavity. It is annular zone, measuring 0.1-0.5 cm from top to bottom in the nonpregnant uterus. It is limited above by the anatomical internal os and below by the histological internal os.The area between uterine cavity and cervical canal is anatomical internal os and the isthmus is below this. The junction between isthmus and cervical canal can only be recognized microscopically and termed as histological internal os.
- Uterine cornu: On each side of the upper uterine body a funnel shaped area receives the insertion of the fallopian tube, which is called cornu.
- Fundus of uterus: The part of body of uterus above the cornua is called fundus.
Endometrial cavity: Endometrial cavity is triangular in shape and represents the mucosal surface of uterine corpus. Endometrium of the body of uterus is divided into two zones:
- Superficial epithelium which is functional layer,
- Deeper basal layer which lies adjacent to myometrium.
The surface epithelium is a single layer of ciliated columnar epithelium and with endometrial gland, vessels and nerves forms a specialized stroma. It undergoes cyclic structural and functional changes during the reproductive years with regular shedding of the superficial endometrium and regeneration from basal layer.
Muscular layer: Muscular layer of uterus is called myometrium, which consist of interlacing smooth muscle fibers held by connective tissues, which range in thickness from 1.5 to 2.5 cm or some other fibers of myometrium are continuous with those of fallopian tube and round ligament.
During pregnancy, three distinct layer of myometrium can be identified—outer longitudinal, middle interlacing and inner circular.
Peritoneum: It is termed serosa which covers most of corpus of uterus and the posterior cervix. The perineum is reflected onto the bladder at the level of the internal os. So the cervix of the uterus has no peritoneal covering anteriorly. Posteriorly the whole of the body of uterus and supravaginal portion of the cervix is covered by peritoneum. The peritoneum is reflected from the supravaginal portion of the cervix onto the posterior vaginal wall in the region of the posterior fornix.
Laterally, the peritoneal layer is incomplete because of the insertion of the fallopian tube, round and ovarian ligament into the uterus and below this level, the double layer of peritoneum covering the neurovascular supply to the uterus inserts into the cervix and corpus (Fig. 1.7).
Cervix
Cervix is spindle shaped, measuring 2–3 cm in length bounded above by the internal os and below by the external os. The position of cervix exposed to vagina is the Exocervix or Portio Vaginalis. It has a convex round surface with a circular (in nulliparous) or slit like (in multipara) opening (the external os) into the endocervical canal. The endocervical canal is about 2.3 cm in length and opens proximally into the endometrial cavity at the internal os. The mucosal lining of cervix differs from that of the corpus by the absence of a submucosa. The endocervix is lined by high columnar ciliated epithelium with spindle shaped nuclei lying adjunct to the basement membrane.
The glands are racemose in type; secrete mucus of alkaline pH with high fructose content. The direction of cilia of columnar epithelium is downwards, towards external os, so secretion collects as a plug in the cervical canal which helps against ascending infections. It is under hormonal influence. The mucous membrane lining the endocervix is thrown into folds which consist of anterior and posterior column from which radiate circumferential folds to give the appearance of true trunk and branches, so called ‘arbor vitae’.
Exocervix and portio vaginalis of cervix: It is covered by stratified squamous epithelium which extends right up to external os, where there is abrupt change to columnar type.
Transformation zone: The intersection where the stratified squamous epithelium of exocervix and mucous secreting columnar epithelium of endocervical canal meet is called squamocolumnar junction or transformation zone. This zone is geographically variable, dependent on hormonal stimulation as well constantly effected by infection and trauma. This dynamic interface is most vulnerable to development of squamous neoplasia. In early childhood, during pregnancy or with oral contraceptive use, columnar epithelium may extend from the endocervical canal onto the exocervix, a condition known as eversion or ectopy.
After menopause the transformation zone usually recedes entirely into the endocervical canal. Deep in the mucosa and submucosa the cervix is composed of fibrous connective tissue and a small amount of smooth muscle in circular arrangement.
Blood supply: Blood supply to the uterus is via uterine artery which anastomoses with the ovarian and vaginal arteries one on each side. Uterine artery arises directly from the anterior division of the internal iliac artery or in common with superior vesical artery.
The uterine artery cross the ureter anteriorly about 1.5 cm away at the level of internal os before it ascends up along the lateral border of the uterus in between the leaves of broad ligament (Fig. 1.8).
Nerve supply: The nerve supply to the uterus is the uterovaginal plexus:
Uterine Appendages
The uterus projects upwards from the pelvic floor into the peritoneal cavity. It carries on each side of it two folds of peritoneum which pass laterally to the pelvic wall and form the broad ligament. The fallopian tube passes outwards from the uterine cornua and lie in the upper border of the broad ligaments. The ovarian ligaments passes posteriorly and round ligament anteriorly into the uterine cornu but at a slightly lower level than fallopian tube. Round and ovarian ligament, as well the fallopian tubes are covered with peritoneum. Fallopian tubes and ovaries collectively are referred to as the adnexa.
Fallopian Tube
The fallopian tubes are paired hollow structure representing the proximal unfused ends of the Müllerian duct. They lie in upper margin of the broad ligament and are approximately 10 cm long (vary from 7 to 12 cm) and approximately 8 mm in diameter but the diameter diminishes near the cornu of the uterus. Each fallopian tube has got two openings—one communicates with the lateral angle of the uterine cavity called uterine opening and measure 1 mm in diameter, the other on the lateral end of the tube called pelvic opening or abdominal ostium which measures 2 mm in diameter.
The fallopian tube is divided into several portions (Fig. 1.9):
- Interstitial portion (Intramural, uterine Syn): It is the narrowest portion of the tube, 1 cm in length, lies within the uterine wall and form the tubal ostia at the endometrial cavity. There are no longitudinal muscle fibers here but the circular fibers are well developed. Its internal diameter is 1 mm or less, so that only finest cannula can be passed into it during salpingostomy operation.
- Isthmus: It is narrow cord tube segment closest to the uterine wall, represent 1/3rd of total length of fallopian tube, i.e. 35 mm. It is narrow but a little wider than interstitial part and its lumen has a diameter of 2 mm. It's muscle wall contain both longitudinal and circular fibers. It is covered by peritoneum except for a small inferior base area related to broad ligament.
- Ampulla: It is the lateral, widest, tortuous part of tube which comprises half of length of fallopian tube (5 cm).
- Fimbria (Infundibulum): It is a funnel-shaped abdominal ostia of the tube, opening into the peritoneal cavity.This opening is fringed with numerous fingers like projection that provide a wide surface for ovum pickup. One fimbria is Fimbria ovarica which is larger and longer than the others and is attached to the beginning of the ovary.
Histology
It consist of three layers:
- Serous layer: It consists of the mesothelium of the peritoneum which covers on all sides except all along the line of attachment of mesosalpinx. Intervening between the mesothelium and the muscle layer is a well defined subserous layer in which numerous small blood vessels and lymphatics can be demonstrated.
- Muscle layer: It consists of an inner circular and outer longitudinal layer of smooth muscles. The circular fibers are best developed in isthmus. Muscular activity in the infundibulum draws the fimbria close to the ovary at the time of ovulation. The tube displays high frequency/low amplitudes and low frequency/high amplitudes contraction. The former are more characteristic of the ampulla, while the low frequency/high amplitude occur in isthmus and may propagate in either direction. Ovum transport is fast in the ampullary region but a physiological sphincter at the isthmus delays passage into the uterus for three days. Ampullary area also contains numerous (excitatory and inhibitory) adrenergic receptors.
- Mucosa of fallopian tube: The fallopian tube is lined by a single layer of columnar epithelium with three types of cells: (i) Ciliated, (ii) Secretory, (iii) Resting.
- Function of ciliated epithelium is to propel a fluid current towards the uterus which plays some part in transport of inert ovum, which unlike sperm, has no motile power of its own. The cilia beat asynchronously at about 7 beat per second.
- Secretory, nonciliated cells are found throughout the tube, but are most numerous at the isthmic end. They develop microvilli and become secretory at the mid cycle.
- A cell intermediate in type to ciliated and secretory cells are small rod shaped resting or peg cell, whose purpose is not known.
Function of Fallopian Tube
Function of fallopian tube is ovum pickup, provision of physical environment for conception and transport and nourishment of fertilized ovum. Fallopian tube secretion contains pyruvate, which is an important substrate for the embryo. They contain less glucose, protein and potassium than serum.
Blood Supply
Vascular supply to the fallopian tube is the tubal branch of uterine and ovarian arteries. A anastomosing branch of uterine artery supplies the inner part and tubal branch of ovarian artery supply the main fallopian tube. Unlike the vermiform appendix, the fallopian tube does not become gangrenous when acutely inflamed, as it has two sources of blood supply, which reach it at opposite ends. Venous drainage is through the pampiniform plexus into the ovarian veins.
Innervation
The innervation to the fallopian tube is via uterovaginal plexus and ovarian plexus.
Lymphatics
The lymphatics of the fallopian tube communicate with the lymphatic of the fundus of the uterus and with those of ovary and they drain along the infundibulopelvic ligament to the aortic glands near the origin of the ovarian artery from the aorta.
Ovaries
The ovaries are paired gonadal structure that lie suspended between the pelvic walls and the uterus by the infundibulopelvic ligament laterally and uterovesical ligament medially. The ovary measures 3 cm × 1.5 cm, almond shaped, pearl grey due to a compact tunica albuginea and surface is slightly corrugated (Fig. 1.10).
The ovaries are intraperitoneal structure and not normally palpable during bimanual examination.
Relation
Ovary is attached to the posterior surface of the broad ligament by the mesovarium and occupies the ovarian fossa on the wall of the pelvis.
This fossa is bounded anteriorly by the obliterated umbilical artery and posteriorly by the ureter and the internal iliac artery and laterally to the peritoneum separating the obturator vessels and nerves.
Primary neurovascular structure reaches the ovary through the infundibulopelvic ligaments and enters through mesovarium.
Histology
The surface of the ovary is covered with a layer of cuboidal cells known as germinal epithelium which is continuous with the peritoneum at the mesovarium. Beneath this is the thin layer of condensed connective tissue, the tunica albuginea. It has a thick cortex which is composed of a specialized stroma and follicles in various stage of development or attrition (Fig. 1.11).
The medulla is highly vascular, occupies a small portion of ovary in its hilar region and is composed of fibromuscular tissue, blood vessels and nerves. There are small collections of cells called ‘hilus cells’ which are homologous to the interstitial cells of the testes.
Blood Supply
The blood supply to the ovary is the ovarian artery—a branch of abdominal aorta, which anastomoses with uterine artery. Venous drainage is through pampiniform plexus, which form ovarian vein which drain into inferior vena cava on the right side and left renal veins on the left side. Part of the venous blood from the placental site drains into the ovarian vein and thus may become the site of thrombophlebitis in puerperium.
Nerve Supply
The nerve supply of the ovarian plexus includes parasympathetic, postganglionic sympathetic and autonomic afferent fibers from T10 segment. Ovary is sensitive to touch.
Epoophoron (Organ of Russell Miller)
It represents the cranial end of the Wolffian body. It consists of series of vertical tubules in the mesovarium and mesosalpinx between the fallopian tube above and ovary below.
Each tubule is surrounded by plain muscles and is lined by cubical cells.
Paroophoron
It represents the caudal end of the Wolffian body and contains vertical tubules.
Wolffian Duct
It is an imperfect duct which runs parallel to but below the fallopian tube in the mesosalpinx, which passes downward by the side of uterus to the level of internal os, where it passes into the tissues of the cervix. From where it runs forward to reach anterior lateral aspect of the vaginal walls and may reach down up to hymen. The duct sometimes from a cyst, called Gartner's cyst in the broad ligament in the vagina and require surgical enucleation sometimes.
FEMALE UROLOGICAL SYSTEM
Ureter
The ureter forms as an outgrowth (metanephric diverticulum) from the lower end of the mesonephric duct. The cranial end of the diverticulum gives rise to the pelvis, calices and collecting tubules of the kidney.
The ureter is the urinary conduit, leading from the kidney to the bladder. It measures about 25 cm in length and is totally retroperitoneal in location. The abdominal part lies on the Psoas major, crosses in front of genitofemoral nerve and is crossed by the ovarian vessels. The lower half of each ureter traverses the pelvis after crossing the common iliac vessels at their bifurcation, just medial to the ovarian vessel.
The pelvic part follows the anterior border of the greater sciatic notch, turns medially at the ischial spine and runs above the levator ani in the base of broad ligament (Parametrium) to the base of the bladder. The ureter pierces the Mackenrodt's ligament (Parametrium) where a canal—ureteric canal is developed. It is obvious that the ureter must have a room in which its peristaltic movements can be carried out without pressure from surrounding structure and for that ureteric canal is present. In its passage through the ureteric canal, the ureter is crossed by the uterine artery and the uterine plexus of veins.
After leaving the ureteric canal, the ureter passes forwards and medially to reach the bladder, being separated from the cervix by a distance of 1–2 cm, ureter follows an oblique course through the bladder wall.
Applied Anatomy
- The course of ureter in the pelvis is important as it is liable to get injured in gynecological surgery. The common sites of injury may be:
- The infundibulopelvic ligament
- By side of cervix
- Vaginal angle
- During pelvic peritonization
The chances of injury are more in cases of endometriosis, pelvic inflammation or broad ligament tumors. - The course of ureter through the pelvis is not always constant and there is a variation also in origin of uterine artery.
- During surgery the ureter is recognized by its pale glistening appearance and by a fine longitudinal plexus of vessels on its surface but more particularly by the peristaltic movements. It can be readily recognized by palpation between finger and thumb as a firm cord, which as it escapes gives a characteristic snap.
- Ureter is sometimes duplicated.
- In malignancies of the cervix with extensive involvement of the parametrium, dilatation of ureter is frequently present.
Histology
The ureter has fibrous, muscular and mucosal coats. Fibrous coat is derived from the visceral layer of the pelvic fascia. Muscularis consist of an inner longitudinal and outer circular layer of smooth muscles. The mucosa consists of the transitional epithelium.
Blood Supply
The blood supply comes from the abdominal aorta, variable with contribution from the renal, ovarian, common and internal iliac, uterine and vesical arteries.
Nerve Supply
Nerve supply is both sympathetic and parasympathetic and arises from the renal, aortic and superior and inferior hypogastric plexus (T10 to S4).
Urinary Bladder
The urinary bladder is derived in part from the urogenital sinus and in part from the ends of the mesonephric ducts. It is continuous with the allantoic duct, which persist as a partly canalized fibromuscular band—the urachus, joining the apex of the bladder to the umbilicus. The bladder is a hollow organ, spherically shaped when full that stores urine.
Relations
The bladder is positioned posterior to the pubis and lower abdominal wall and anterior to the cervix, upper vagina and part of the cardinal ligament. Laterally, it is bounded by the pelvic diaphragm and obturator internus muscle.
Structure
The urinary bladder is often divided into two areas which are of physiologic significance:
12The base of the bladder: Consist of urinary trigone posteriorly and a thickened area of detrusor anteriorly. The three corners of the trigone are formed by the two ureteral orifice and opening of urethra into the bladder. Base of the bladder receives alpha-adrenergic sympathetic innervation and responsible for maintaining continence.
The dome of the bladder: It is the remaining bladder area above the bladder base. It has parasympathetic innervation and is responsible for micturition.
Histology
The bladder wall has three layers: (a) Serous, (b) Muscular, (c) Mucosal. Serous layer is the peritoneal covering of the superior surface. The smooth muscle (Detrusor) has internal and external longitudinal layers and a middle circular layer. Fibers from the external layer pass with the pubovesical ligament to the pubic bones. Rather than being arranged in layers, it is composed of intermeshing muscle fibers.
The bladder mucosa is transitional cell epithelium which is loosely attached to the muscle except over the trigone where it is firmly attached.
Blood Supply
The blood supply to bladder is from the superior, middle and inferior vesical arteries and from small branches from the obturator, inferior gluteal, uterine and vaginal arteries. The veins form a plexus on inferolateral surface which drain to internal iliac veins.
Innervation
The parasympathetic nerves convey motor fibers to the detrusor (S2-S4 nervi erigentes). The sympathetic nerves (T11, T12, L1, L2) may have the opposite effect, but their main function is vasomotor control.
Urethra
Urethra is the vesical neck in the region of the bladder that receives and incorporates the urethral lumen. The female urethra is 4 cm long and is embedded in the anterior wall of the vagina. Its diameter is about 6 mm.
The bladder base forms an angle with the posterior wall of the urethra called Posterior Urethrovesical (PUV) angle, which normally measures 100°. The urethra runs downwards and forwards in close proximity of the anterior vaginal wall. About 1 cm from the lower end it pierces the triangular ligament. It ultimately opens into the vestibule about 2.5 cm below the clitoris.
Relation
The lower urinary tract and genital tracts are intimately connected anatomically and functionally. Posteriorly it is related to anterior vaginal wall to which it is loosely separated in the upper 2/3rd but firmly adherent in lower third.
Anteriorly urethra is related to posterior aspect of symphysis pubis. The upper 2/3rd is separated by loose areolar tissues, the lower 1/3rd is attached on each side of the pubic rami by fibrous tissue called pubourethral ligament.
Laterally as urethra passes through the triangular ligament, it is surrounded by compressor urethra.
Applied Anatomy
In gynecological surgery the bladder and proximal urethra can be dissected easily in midline from underlying lower uterine segment, cervix and vagina through a loose avascular plane. The distal urethra is essentially inseparable from the vagina. Unrecognized injury to the bladder during pelvic surgery may result in the development of a vesicovaginal fistula.
Histology
The urethral mucosa has a transitional epithelium near the bladder neck, grading to a nonkeratinized stratified squamous epithelium near the external orifice. On the posterior wall is an epithelial fold—the urethral crest.
There are numerous mucosal glands, near the lower end. The ducts of these join to form the two paraurethral (Skene's duct). Skene's glands are homologous to prostrate in the male, which end in an aperture lateral to the external orifice.
Chronic infection of Skene's glands, with obstruction of their ducts and cystic dilatation is believed to be an inciting factor in the development of suburethral diverticulum.
The urethra contains an inner longitudinal layer of smooth muscles and outer circularly oriented smooth muscle fibers. The smooth muscle layer is continuous with that of the bladder and there is no separate internal sphincter at the junction with the bladder. The urethra is surrounded by two layers of striated voluntary muscles. The intramural layer (external sphincter) consists of slow twitch muscle fibers which exhibit tonic activity at rest.
Blood Supply
The arterial and venous blood supply to the upper third of the urethra is associated with that of the bladder and lower two-third with that of the anterior vaginal wall and clitoris. It is from the vesical and vaginal arteries and the internal pundendal branches.
Nerve Supply
The nerve supply is direct from S2-S4. Together with the bladder neck, this layer is responsible for urethral continence at rest. The periurethral striated muscle is supplied by the perineal branch of the pudendal nerve 13and is responsible for augmenting urethral closure during stress events.
Physiology of Micturition and Continence
Micturition: The normal urinary bladder fills without a rise in intravesical pressure. This is the result of progressive relaxation of the detrusor smooth muscle, which occurs partly under the influence of the sympathetic nervous system. Sensation of bladder filling occur when urinary volume of 350 ml is reached with maximum capacity of 500–600 ml. Voluntary voiding is controlled by the pontine micturition center, which produces contraction of the detrusor muscle and simultaneous urethral relaxation, which continue, until the contents of the bladder have been completely expelled, leaving a negligible residual volume.
Continence
Continence of urine depends on the urethral pressure being maintained at the higher level than intravascular pressure. This is achieved by active contraction of both smooth and striated muscles of the urethral wall, with some contribution from the pelvic floor (Fig. 1.12).
When abdominal pressure rises suddenly during coughing, sneezing or straining, urethral pressure also rises to exceed abdominal pressure and prevent urine loss.
LOWER GASTROINTESTINAL TRACT
Sigmoid Colon
The sigmoid colon begins its characteristic S-shaped curve as it enters the pelvis at the left pelvic brim. The columnar mucosa and richly vascularized submucosa are surrounded by an inner circular layer of smooth muscles and their overlying longitudinal bands of muscle called tenia coli. A mesentery of varying length attach to the sigmoid to the posterior abdominal wall.
Blood Supply
Blood supply to sigmoid colon is from sigmoid arteries.
Innervation
The nerves to the sigmoid colon are derived from the inferior mesenteric plexus.
Rectum
The sigmoid colon loses its mesentery in the midsacral region and become the rectum about 15–20 cm above the anal opening. The rectum follows the course of the lower sacrum and coccyx and becomes entirely retroperitoneal at the level of rectouterine pouch or posterior cul-de-sac.
It continues along the pelvic curve, just posterior to the vagina until the level of anal hiatus of the pelvic diaphragm, where it takes a sharp 90° turn posteriorly and become the anal canal, separated from the vagina by the perineal body. The rectum curves twice to the left and once to the right before it passes down to continue as anal canal.
Peritoneal Covering and Relation
Rectum is covered anteriorly and laterally in its upper and one-third, only anteriorly in the middle third while whole of the posterior surface and entire lower one-third remain uncovered.
Anteriorly: From above downwards —(i) The part of rectum covered by peritoneum is related to the posterior wall of the pouch of Douglas which often contains loop of small or large bowel, (ii) The ampulla is related to posterior vaginal wall separated by rectovaginal septum, (iii) The lower part is related to perineal body.
Posteriorly: Rectum is related to the sacrum and coccyx intervened by loose areolar tissues, sacral nerve trunks and middle sacral vessels.
Laterally: From above downwards—(i) Rectum is related to uterosacral ligament, pelvic plexus of nerve and ureter, (ii) Near anorectal junction it is related to puborectalis part of levator ani, (iii) Below the muscle it is related to ischiorectal fossa.
Histology
The rectal mucosa is lined by a columnar epithelium and characterized by three transverse folds that contain mucosa, submucosa and the inner circular layer of smooth muscles.
The tenia of the sigmoid wall broadens and fuses over the rectum to form a continuous longitudinal external layer of smooth muscles to the level of the anal canal.
Anal Canal
Anal canal begins at the level of the sharp turn in the direction of the distal colon, measures 2–3 cm in length, and ends at the anal orifice.
At the anorectal junction the mucosa changes to stratified squamous epithelium which is called pectinate line (or white line, Hilton's line synonym) which continues until the termination of the anus at the anal verge, where there is transition to perineal skin with typical skin appendages.
Relation
Anteriorly rectum is related to perineal body and posteriorly to the anococcygeal body.
Anal Sphincter
Mucosa of anal canal is surrounded by a thickened ring of circular muscle fibers that is a continuation of the circular muscles of the rectum, which is termed: (a) Internal anal sphincter—it is involuntary, (b) Voluntary external anal sphincter—it is formed by bundle of striated muscle in lower part of anal canal, it consist of three parts:
- Subcutaneous part which is attached to skin.
- Superficial part which starts from the perineal body and is inserted posteriorly to tip of the coccyx.
- Deep part which is separated from the internal sphincter ani by levator ani.
Fecal continence is primarily provided by the puborectalis muscle and the internal and external anal sphincters. The puborectalis muscle surrounds the anal hiatus in the pelvic diaphragm and interdigitates posterior to the rectum to form a rectal sling. The external anal sphincter surrounds the terminal anal canal below the level of the levator ani (Fig. 1.13).
Blood Supply
The vascular supply to the rectum and anal canal is from the superior (branches of inferior mesenteric artery), middle and inferior rectal (branch of internal iliac artery). The rectum and upper one-third of anal canal has venous drainage into portal circulation via superior rectal veins. The lower one-third of the anal canal drains on both sides into inferior rectal veins.
The venous drainage is a complex submucosal plexus of vessels, that under condition of increased intra-abdominal pressure like pregnancy, ascites may dilate and become symptomatic with rectal bleeding and present as hemorrhoids.
Nerve Supply
The rectum and upper two-third of the anal canal are supplied by autonomic middle rectal plexus and inferior mesenteric plexus while the lower third of anal canal is innervated by pudendal nerve.
Applied Anatomy
Anatomic proximity of the lower gastrointestinal tract to lower genital tract makes the rectum and sphincter ani liable to injury during repair of vaginal laceration and surgery of vulva and vagina. Because of avascular nature of the rectovaginal space, it is relatively easy to dissect the rectum from the vagina in the midline.
Pelvic Floor
The pelvic floor includes all of the structure closing the pelvic outlet from the skin inferiorly to the peritoneum superiorly. It includes: (i) Pelvic peritoneum, (ii) Extraperitoneal fat and cellular tissue, (iii) Levator Ani (Pelvic diaphragm) and their fascial coats, (iv) Urogenital diaphragm (triangular coats), (v) The muscles of peritoneum and their aponeuroses, (vi) Subcutaneous fascia, (vii) Fat, (viii) Skin.
The most important of these structures are the levator ani muscles and these together with fascia which covers their upper and lower surface are collectively called the ‘Pelvic Diaphragm’. Pelvic diaphragm divides pelvic floor into a pelvic and perineal portion.
Levator Ani (Pelvic Diaphragm)
The pelvic diaphragm is spread transversely in a hammock like fashion across the true pelvis, with a central hiatus for origin the urethra, vagina and rectum. From this extensive origin the fibers sweep inferiorly and posteriorly to interdigitate in the midline and insert into:
- Perineal raphe: Perineal body
- Wall of anal canal: Deep external sphincter
- Anococcygeal raphe
- Lower part of the coccyx.
Origin
Each levator ani muscle arises from: (i) Back of the pubic rami, (ii) From the condensed fascia covering the obturator internus (white line, tendinous arch), (iii) Inner surface of ischial spine.
- External component: Which originate from the arcus tendinous, extending from the pubic bone to ischial spine. It gives rise to fibers of differing directions and includes: (a) Pubococcygeus, (b) Iliococcygeus, (c) Coccygeus
- Internal component: It originates from the pubic bones above and medial to origin of the pubococcygeus and is smaller but thicker and stronger. These can be considered inner fiber of pubococcygeus. These fibers run in a sagittal direction and are divided into two portions
- Pubovaginalis: These fibers run in a perpendicular direction to the urethra, crossing the lateral vaginal wall at junction of its lower 1/3rd and upper 2/3rd to insert into the perineal body.
- Puborectalis: Superior fibers of puborectalis sling around the rectum to the symphysis pubis, as inferior fibers insert into the lateral rectal wall between the internal and external sphincter.
Thus, these internal components of levator ani, divide the space between the two levator ani muscles into an anterior portion—the hiatus urogenitalis through which pass urethra and vagina and the hiatus rectalis, through which pass the rectum (Fig. 1.14).
The dimension of the hiatus urogenitalis depends on the two main factors: (a) Tone of levator ani muscle, (b) Existence of the decussating fibers of the puborectalis.
Fascia of Pelvic Diaphragm
The pelvic diaphragm is covered superiorly by fascia which includes a parietal and visceral component and is a continuation of the transversalis fascia. Parietal fascia has area of thickening and forms ligament, septa and gives strength and fixation for the pelvic floor (Fig. 1.15).
The endopelvic fascia (visceral) extends medially to invest the pelvic viscera resulting in a fascial covering to the bladder, vagina, uterus and rectum. It continues laterally with the pelvic cellular tissue and neurovascular pedicles.
Nerve Supply
The muscle is supplied by 3rd and 4th sacral nerve, inferior rectal nerve and a perineal branch of pudendal nerve (S2,3,4).
Perineal Muscles and Urogenital Diaphragm (Triangular Ligament Syn)
At a lower level in the pelvis is the urogenital diaphragm (Triangular ligament) with its two layers stretching between and attached to the inferior pubic rami. It is pierced by the dorsal vein of the clitoris which joins the retropubic urethrovesical plexus, by the urethra and the vagina. Between its fascial layers lie the: (a) Compressor urethrae, (b) The deep transverse perineal muscles, (c) Branches of internal pudendal vessel and pudendal nerve. Deep transverse perineal muscles arise from the ramus of the ischium, and are inserted partly into the sidewalls of the vagina and partly into the perineal body.
On the undersurface of the urogenital diaphragm are vestibule and Bartholin's gland and immediately superficial to these are: (a) Sphincter vaginae (bulbocavernosus), (b) Ischiocavernosus, (c) Superficial transverse perineal muscle followed by fascia and skin.
Perineal Body (Central Tendon of Perineum)
It is fibromuscular mass into which levator ani, bulbocavernosus, superficial and deep transverse perineal muscle, sphincter vaginae and external sphincter ani muscle are inserted which represent three layers of muscles of pelvic floor.
Urogenital Triangle
It contains the: (a) Termination of vagina and urethra, (b) Crura of clitoris surrounded by the ischiocavernosus muscle, (c) Bulb of the vestibule surrounded by the bulbocavernosus muscle, (d) Bartholin's gland, (e) Urogenital diaphragm, (f) Superficial and deep perineal pouches (Fig. 1.15).
Superficial perineal pouches: It is a potential space between the inferior fascia of the urogenital diaphragm and fascia of Colles. It contains the Bartholin's gland and superficial transverse perineal muscles.
Perineum
It is pyramidical in shape with its apex on a level with the junction of middle and lower third of the posterior vaginal wall.
Deep perineal pouches: It is a potential space between the two fascial layers of the urogenital diaphragm and contains the membranous urethra surrounded by the external sphincter and deep transverse perineal muscles.
Perineum is situated at the lower end of trunk between the buttocks. Its bony boundaries include the lower margin of the pubic symphysis anteriorly, the tip of coccyx posteriorly and ischial tuberosity laterally. These landmarks correspond to the boundaries of the pelvic outlet. The diamond shape of the perineum is customarily divided by an imaginary line, joining the ischial tuberosities immediately in front of the anus, at the level of perineal body into an anterior urogenital and a posterior anal triangle. Perineal tear during childbirth may divide the muscles of perineal body leading to a tendency to prolapse.
The contraction of levator muscle pulls the rectum and vagina towards the symphysis pubis, the rectum is thereby kinked and closed and vaginae narrowed anteroposteriorly. The origin of levator ani is fixed from bone or white line, while insertion is movable into anococcygeal raphe and coccyx. So the contraction of the levator muscles lead to the posterior attachments being pulled towards the symphysis pubis.
During childbirth the movement of internal rotation of the presenting part is assisted by this property of the levator muscles. Uterine contraction push the presenting part down upon the levator ani (Pelvic floor) and cause the muscle to contract as a result of direct pressure of the presenting part. The lowest part of the fetus is carried forwards during the contraction of the levator muscles and because the anterior fibers of the levator ani muscles are directed inwards as well forward, the presenting part becomes rotated forwards and inwards.
Peritoneum and Ligaments of the Pelvis
- Peritoneal reflection (Done with anatomy of uterus): Peritoneum covers the uterus with the exception of the anterior part of the supravaginal cervix and intravaginal cervix. From the anterior surface of the uterus the peritoneum is reflected onto the superior surface of the bladder, forming the uterovesical pouch. From the posterior surface of the uterus the peritoneum continues onto the anterior rectal surface forming the rectovaginal pouch (or pouch of Douglas). The lower extremity of this pouch is attached to the perineal body by connective tissue of the rectovaginal septum.
Ligament of Uterus
- Broad ligaments: From the lateral borders of the uterus two layers of peritoneum on each side are reflected to the lateral pelvic walls forming the broad ligaments. These peritoneal folds include loose connective tissue referred to as parametrium, which merges inferiorly with extraperitoneal connective tissues.The upper lateral border of the broad ligament forms the infundibulopelvic fold and contains the ovarian vessels in their course from the side wall of the pelvis. The ovary 17is attached to the posterior layer of the broad ligament by a short double fold of peritoneum (the mesovarium) and the portion of the broad ligaments above this is the mesosalpinx.The top of the broad ligament envelops the fallopian tubes. Below and in front of the fallopian tube is the round ligament and below and behind it is the ovarian ligament, all enclosed in the broad ligament. Vestigial remnants of the mesonephric bodies and ducts (Wolffian duct, duct of Gartner's) are contained within the broad ligament.Remnants of the mesonephric body lie above and lateral to the ovary (epoophoron and hydatid of Morgagni) and between the ovary and uterus (paroophoron).The uterus is held in position by the following structures:
- Round ligament: It is attached to uterine body below and in front of the fallopian tube. It is 12 cm long and passes through the broad ligament inferolaterally towards the lateral wall of the pelvis, where it crosses the psoas muscle and external iliac vessels. It hooks round the inferior epigastric arteries to the deep inguinal ring, passes through the inguinal canal and fans out into labium majus. It is composed mainly of fibrous tissues, with some smooth muscle at the uterus and some striated muscle at the labial end.
- Ligaments from the pelvic fascia: The connective tissue covering the levator ani is condensed into musculofibrous bands at 3 areas (Fig. 1.16):
- Transverse cervical ligament (cardinal ligament) arising from the arcuate line on the side wall of the pelvis. It provides support to the cervix and upper vagina and contributes to the support of the bladder.
- Pubocervical ligament arising from fascia over the pubic bone and passing around the bladder neck.
- Uterosacral ligament (posterior part of the cardinal ligament) arising from the sacral promontory, providing support to the cervix and upper vagina.
BLOOD VESSELS OF PELVIS
The aorta divides at the level of fourth lumbar vertebra into two common iliac arteries and the common iliac artery divides at the level of lumbosacral intervertebral disk. Internal iliac artery arises from the bifurcation of the common iliac artery and in the fetus is the hypogastric (umbilical) artery.
From its origin the internal iliac artery descends into the pelvis as far as the greater sciatic foramen where it divides into anterior and posterior trunks. The ureter runs down its front aspect and behind it are the internal iliac veins, the lumbosacral nerve trunk and the piriformis muscle. On its outer side is the external iliac vein and lower down the obturator nerve (Fig. 1.17).
Posterior division passes through the greater sciatic foramen to supply the muscles of the buttock. While the anterior division supplies the internal pelvic organs and terminates as the internal pudendal artery. The branches of the anterior division of the internal iliac artery are following: (i) Superior vesical, (ii) Inferior vesical, (iii) Middle hemorrhoidal (rectal), (iv) Uterine, (v) Vaginal, (vi) Obturator, (vii) Internal pudendal, (viii) Inferior gluteal (sciatic). Last two are terminal branches.
Uterine Arteries
It arises from anterior division of internal iliac or hypogastric artery. It runs downwards and forwards along the lateral pelvic wall almost in the same direction—as ureter until it reaches the base of broad ligament.
It then turns medially and crosses the uterus anteriorly from above and at right angle to it, about 1.5–2 cm lateral to at the level of internal os. It then ascends in a tortuous course between the two layers of the broad ligament on the lateral border of the uterus giving out branches to the myometrium and anastomosing at the superior angle with the terminal portion of the ovarian artery (Fig. 1.17).
Branches to the uterus penetrate the myometrium and then turn to run parallel with the surface and divide into anterior and posterior arcuate arteries which are disposed circumferentially in the myometrium and anastomose with those from the opposite side. The uterus is therefore least vascular in the middle line which becomes the natural site for an incision.
The arcuate arteries give off the serosal branch and radial arteries which penetrate the myometrium to end as basal arteries (spiral arteries), which supply the endometrium (Fig. 1.18). Arcuate and radial arteries are coiled and the purpose of this is to reduce arterial pressure without reducing the flow, which plays important role in pregnancy.
The uterine artery also gives off branches to:
- Ureter while crossing
- To uterine ligaments
- Circular artery to the cervix which is formed by anterior and posterior branches of the artery to the cervix on both side
- Ovarian anastomotic branch
- Ovarian portion of arcade gives off branches to the fallopian tube.
During pregnancy the uterine arteries hypertrophy (the luminal area increase by five times) and their course is straightened. The vaginal and ovarian arteries do not enlarge but the ovarian veins are greatly dilated.
Vaginal Arteries
The vaginal artery is usually a separate branch (or branches) of the internal iliac artery, but may come off the first part of uterine artery. It passes forwards and inwards low in the broad ligament to reach the lateral vaginal fornix. In the vaginal wall it anastomoses with the azygous branches of the circular artery to the cervix. The lower vagina is supplied from the middle and inferior rectal (hemorrhoidal) vessels and by branches from the internal pudendal artery.
Internal Pudendal Artery
Internal pudendal artery is the terminal branch of the internal iliac artery which passes out of the pelvis through the greater sciatic notch, curls round the ischial spine and returns to the lateral wall of ischial rectal fossa through the lesser sciatic notch, 4 cm above ischial tuberosity.
Together with pudendal nerve, it run forward in Alcock's canal under the lee of inferior pubic ramus and then enters between the layers of the triangular ligament to give branches to the labia, vagina, and bulb of the vestibule, perineum and various muscles. It ends as dorsal artery of the clitoris.
Superficial and Deep External Pudendal Arteries
These are branches of the femoral artery which come off just below the inguinal ligament and turn inward to supply the foreparts of the vulva.
Ovarian Artery
The ovarian artery arises from the aorta approximately at the level of renal artery. It run downwards and slightly outwards retroperitoneally and crosses the ureter to reach the brim of the pelvis where it enters the infundibulopelvic ligament.
The ovarian artery sends branches to the ovaries and to the outer part of the fallopian tube. It ends by anastomosing with the terminal part of the uterine artery after giving off a branch to cornu and the round ligament. Thus, a continuous arterial arch is formed and it is impossible to define the limits of ovarian and uterine contribution.
Pelvic Veins
The left ovarian vein ends by passing into the left renal vein. The right ovarian vein terminates into inferior vena cava. The peculiarities of the pelvic veins are that there is tendency to form plexus and plexus anastomose freely with each other and they have no valves.
In the broad ligament near the mesovarium there is a pampiniform plexus of veins which drains into the uterine and ovarian trunks. Pampiniform plexus can sometime become varicose and give rise to broad ligament varicocele.
The uterine plexus is found around the uterine artery near the uterus, the vaginal plexus around the lateral fornix of vagina, and at anorectal junction. All ultimately drain into the internal iliac veins.
The venous return from the rectum and pelvic colon enters the portal system by way of the inferior mesenteric veins. The uterine veins also communicate with the vaginal plexus and this account for low vaginal metastasis in cancer of body uterus. The vessels of bulb and clitoris link with vesical and vaginal plexus.
The pelvic plexus and veins also have communication with the presacral and lumbar channels of the vertebral plexus and thus it is possible for blood, tissue cells, emboli and organism to travel to remote parts of the body without passing through the heart and lungs. This explains the occurrence of metastatic growth in the spine and brain, when the primary is in the uterus.
The collateral pathways are especially significant in late pregnancy, when the large uterus always obstructs the inferior vena cava of the woman lying on her back. It is mainly when this alternative route is inadequate and woman can have the supine hypotension syndrome.
Salient Features of Pelvic Blood Vessels
- The pelvic vessels play an important role in pelvic support—they provide condensation of endopelvic fascia that act to reinforce the normal position of pelvic organs.
- There is significant anatomic variation between individuals in the branching pattern of the internal iliac vessels.
- The pelvic vasculature is a high volume, high flow system with enormous expensive capabilities throughout reproductive life.
- The pelvic vasculature is supplied with an extensive network of collateral connection that provides a rich anastomotic communication between different major vessels system.
LYMPHATIC DRAINAGE OF PELVIS
The lymphatic drainage of the pelvis begins as plexus in the individual organs and generally follows the line of blood vessels. After which they are named and generally arranged in groups or chain (Fig. 1.19).
Lymph nodes in pelvis receive afferent lymphatic vessels from pelvic, peripheral, visceral and parietal structure and send efferent lymphatic to more proximal node groups.
The number of lymph nodes and their exact location though varies but major and constant group of lymph nodes are as follows:
- Nodes at junction of internal and external iliac vein (common iliac).
- External iliac (collecting from inguinal group of lymph nodes).
- Internal iliac.
- Obturator node in the obturator foramen, close to obturator vessels and nerve.
- Ureteral node in the broad ligament near the cervix, where the uterine artery crosses over the ureter.
- The Cloquet or Rosenmüller node—highest of deep inguinal nodes that lie within the opening of femoral canal.
- Median and lateral sacral.
- Superficial (horizontal)
- Deep femoral gland (vertical group): The horizontal group lies superficially parallel to inguinal ligament (Poupart's ligament syn) and vertical group follow the course of saphenoid and femoral veins. The Cloquet or Rosenmüller node lies beneath the inner end of Poupart's ligament in the femoral canal between Gimbernat's ligament and the femoral vein. Inconstant deep inguinal nodes are 5 – 6 in numbers and lie on the medial side of the femoral vein, along the course of round ligament and in the tissue of mons veneris. The communication from the superficial to deep gland occurs through fossa ovalis.
The glands of the parametrium: It is of small size, inconsistently present in the parametrium, near the crossing of the ureter with the uterine artery.
Hypogastric gland (bifurcation nodes): These glands are situated below the bifurcation of the common iliac. This group contains all the regional glands for the cervix, the bladder, the upper one-third of the vagina and also for greater part of the body of the uterus. These glands may be extensively involved in carcinoma of cervix and of vagina. A further group of these glands situated in the obturator fossa often called the obturator glands, which is most obviously involved in carcinoma of cervix.
External iliac glands: This group of gland has three groups: (a) Lateral—lateral to external iliac artery, (b) Middle in between artery and vein, (c) Medial—medial to the vein.
These glands receive drainage from the obturator and hypogastric glands and are always involved in late cervical cancer.
Common Iliac Glands
This group is the upward continuation of the external and hypogastric group and therefore involved next after these glands.
Sacral Group
Two groups of sacral glands can be recognized—a lateral group, lying lateral to the rectum and a medial group lying in front of the promontory of the sacrum. They receive lymphatics from the cervix of the uterus and from the upper third of the vagina. The lymphatic from these glands pass directly either to inferior lumbar group or to the common iliac group.
Lumbar Group
These lymphatic glands are divided into an inferior group which lies in front of the aorta below the origin of the inferior mesenteric artery and a superior lumbar group which lies near the origin of the ovarian arteries.
The superior group of lumbar glands receive lymphatics from the ovaries and fallopian tubes as well from the inferior lumbar glands. The lymphatics from the fundus of the uterus join the ovarian lymphatics to pass to the same group.
The above group of lymphatic glands receives lymphatics ‘direct’ from the female generative organs and are known as the ‘regional lymphatic glands’ of the female genital system.
Thereafter, the lymph from the superior lumbar group of lymph nodes, passes up to cisterna chyli situated over the body of 12th thoracic vertebra. The lymph is finally carried upwards via the thoracic duct which opens into the left subclavian vein at its junction with left internal jugular vein.
Organ-wise Lymphatic Drainage of Female Reproductive System
Vulva and Perineum
The lymphatics of each side of the vulva communicate freely with each other, so for malignant disease of one labium it is proper to excise the whole vulva. Without encroaching on the inner aspect of the thigh, channels pass forward to the mons veneris and the subcutaneous tissue of the lower abdominal wall to enter the medial group of superficial inguinal nodes.
These connect with the deep inguinal (femoral) groups from which lymphatics pass to the external and ultimately to the common iliac lymph nodes.*
Vagina
The lymphatic plexus are situated in the mucosal and muscle layers. Lower vagina drains to the inguinal and femoral nodes in the same way as the vulva. The drainage of the middle and upper vagina is the same as that of cervix.
Cervix
Lymphatics from the cervix run in the broad and uterosacral ligaments and in the cellular tissue beneath these to the external and internal iliac, the obturator and sacral nodes. There is a plexus of lymphatic vessels and rarely use node in the broad ligament near the cervix.
The hypogastric and external iliac nodes communicate with those around the common iliac vessels and ultimately with the para-aortic group.
Fallopian Tube and Ovary
The intrinsic plexus of the fallopian tube are situated in the mucosal and subperitoneal layers. The fallopian tube drains in part with the fundus of uterus but mainly with the ovary. Lymphatics from the ovary accompany the ovarian vessels to reach the aortic nodes (lumbar nodes).
There are free anastomoses between the ovarian lymphatics of each side across the uterosacral ligament and via the subperitoneal lymphatic plexus of the fundus of uterus.
Urethra and Bladder
The external urethral meatus drains with the vulva to the inguinal nodes. The remainder of the urethra together with bladder has lymph vessels which go to external, internal and common iliac nodes.
Pelvic Colon
Lymphatic accompany the inferior mesenteric vessels to the preaortic nodes.
Anus and Rectum
The anal orifice drains to the superficial inguinal nodes and anal canal to the internal iliac group. The lymphatic drainage of lower rectum is also to the internal inguinal nodes, the lymph channels accompanying the inferior rectal and internal pudendal vessels. That of upper rectum is to the preaortic nodes, the lymph channels being associated with superior rectal vessels.
PELVIC NERVES
These are somatic and autonomic pelvic nerves.
Somatic Nerves
- The skin of mons veneris and the foreparts of the vulva are supplied by the ilioinguinal nerve and genital branch of genitofemoral nerve both arising from L1 and L2 roots of the lumbar plexus.
- The outer parts of the labia posteriorly and the perineum receive some sensory fibers from the perineal branch of posterior cutaneous nerve of the thigh.
- The main somatic supply to the pelvic organ is pudendal nerve, which is both motor and sensory and is formed from the S2, S3 and S4 roots of the sacral plexus.
Pudendal nerve leaves the pelvis through the greater sciatic notch, curls round the ischial spine and with internal pudendal vessels re-enters through lesser sciatic notch to lie on the outer wall of the ischiorectal fossa in Alcock's canal (Pudendal canal syn). Pudendal nerve supplies sensory fibers to the skin of vulva, external urethral meatus, clitoris, perineum and the lower vagina.
It provides motor fibers to all the voluntary muscles, including the compressor urethrae, sphincter vaginae, levator ani and external and sphincter.
Except in its lower part, the vagina is remarkably insensitive to ordinary stimuli. Disease such as vaginitis, ulcer with cancer and injuries including burn do not cause pain. Vaginal surgery can be carried out with minimum infiltration of local anesthetic provided the perineum and introitus are avoided, because most of the vagina is supplied by autonomic and not somatic nerves.
Autonomic Nerves
All the internal reproductive organs including the upper vagina together with urinary apparatus, rectum, and colon have only autonomic innervations. The blood vessels are controlled by their own intrinsic nerves. The autonomic nerves to these carry both sensory and motor fibers—principally adrenergic and partly cholinergic.
Sympathetic
Motor sympathetic nerves arise from D5 and D6 and sensory nerves arise from D10 to L1 in case of sensory nerves. They pass down from the celiac plexus through intermesenteric plexus, lying retroperitoneally in front of abdominal aorta. Over the bifurcation of the aorta and promontory of the sacrum is complicated network just beneath the peritoneum, called presacral nerve or superior hypogastric plexus.
From superior hypogastric plexus two main chain hypogastric nerves run outwards and downwards, on each side wall of the pelvis to terminate in the inferior hypogastric plexus, which lie on either side of ampulla of rectum extending forward beneath the uterosacral and broad ligament.
It also receives fibers from the parasympathetic system, consisting of sacral fibers S2,3,4, from here the nerve fibers pass to all the pelvic organs. The forward extension of the pelvic plexus is called the Lee Frankenhausser plexus. The parasympathetic fibers (nerve erigentis) are derived from the S2, S3 and S4 nerves and join the hypogastric nerve of the corresponding side to form pelvic plexus. These parasympathetic fibers are mainly sensory to the cervix and lower uterus (Fig. 1.20).
From vaginal plexus the nerve fibers pass onto the uterus, upper 1/3rd of vagina, urinary bladder, ureter and rectum.
Ovarian Plexus
The fallopian tubes and ovaries are supplied by parasympathetic and sympathetic nerves which accompany the ovarian vessels and come directly from the preaortic plexus. They are both motor and sensory. The segmental supply is D10 and D11 for the ovary and D11 and D12 for the fallopian tube.
ANTERIOR ABDOMINAL WALL
It is relevant for student to know the anatomy of abdominal wall beside female reproductive system, which from the basis for different abdominal incision in obstetrical and gynecological surgery and endoscopy.
The anterior abdominal wall includes skin, superficial fascia, a muscle/aponeurosis layer, transversalis fascia and peritoneum.
The four main muscles are: (a) Internal oblique, (b) External oblique, (c) Transversus, (d) Rectus abdominis. All muscles are supplied by T6 to T12 and L1 (Fig. 1.21).
Muscles of Anterior Abdominal Wall
External oblique (Obliqus externus syn): It arises from the lower eight ribs. Some muscle fibers terminate on the iliac crest, the rest form an aponeurosis which ends medially in the linea alba, which is a tendinous structure extending from the xiphoid process to the pubic symphysis.
Aponeurosis ends below the pubic symphysis and pubic crest. Between the pubic tubercle and the anterior superior iliac spine the thickened margin of the aponeurosis form the inguinal ligament.
Inguinal Rings and Canal
Just above the pubic crest is a triangular aperture which is called superficial inguinal ring. The deep inguinal ring in the transversalis fascia lies above and lateral to superficial inguinal ring. The inguinal canal runs between these two rings and contains the round ligament (spermatic cord in the male) and the ilioinguinal nerve.
Oblique Internus Muscle
It arises from the lateral 2/3rd of the inguinal ligament, from the iliac crest, and from the thoracolumbar fascia. It inserts to the lower three to four ribs. Some fibers from the inguinal ligament arch around the round ligament of the uterus and join the aponeurosis of the transverse abdominis to form the conjoint tendon inserting into the pubic.
Transverses Abdominis
This muscle arises from the lateral third of the inguinal ligament, iliac crest, the thoracolumbar fascia and the internal aspect of the lower six cartilages. It forms an aponeurosis, the lower fibers of which contributes to the conjoint tendon, while rest of fibers blends with the linea alba in the midline.
Rectus Abdominis
Rectus abdominis arises by tendons from the pubis and is attached to the 5th to 7th costal cartilages. It has three tendinous intersections and is enclosed by the fibrous rectus sheath.
Rectus Sheath
The aponeurosis of the external and internal oblique and the transverses abdominis combines to form a sheath for the rectus abdominis and pyramidalis which fuse medially in the midline at the linea alba and laterally at the semilunar line. Above the arcuate line, the aponeurosis of the internal oblique muscle splits into anterior and posterior lamellae.
Below this line, all three layers are anterior to the body of the rectus muscle. The rectus is then curved posteriorly by the transversalis fascia, providing access to the muscles for the inferior epigastric vessels. Pyramidalis is a triangular muscle in front of the lower part of the rectus abdominis.
Nerve and Vessels
The tissues of the abdominal wall are innervated by the continuation of the inferior intercostals nerve T4 to T11 and the subcostal nerve T12. The inferior part of the abdominal wall is supplied by the first lumbar nerve through the iliohypogastric and ilioinguinal nerve. The primary blood supply to the anterior abdominal wall includes the following:
- Inferior epigastric and deep circumflex iliac arteries branches of the external iliac artery.
- The superior epigastric artery—a terminal branch of the internal thoracic artery.
The inferior epigastric artery runs superiorly in the transversalis fascia to reach the arcuate line where it enters the rectus sheath. It is vulnerable to damage by the abdominal incision in which the rectus muscle is completely or partially transected or by excessive lateral traction on the rectus. The superior epigastric vessels enters the rectus sheath superiorly just below the 7th costal cartilage.
Concluding Remark
Clear concepts of anatomical details lay the foundation steps of differential diagnosis, surgical approaches and techniques. Today new surgical approaches are being developed to solve old problem and new interpretation of old anatomical knowledge is being done. Surgeon has to revisit and reapply its familiar anatomy from different perspective with wide use of endoscopy or disturbed anatomic relationship in various diseases, so a clinician as well surgeons should be a perpetual students of anatomy.
PELVIC SKELETON
The skeleton of the pelvis is formed by the sacrum and coccyx, and the paired hip bones (Coxal, Innominate syn) which fuse anteriorly to form the symphysis pubis.
The Innominate Bone
The innominate bone consists of: (a) Ilium, (b) Ischium, (c) Pubis. These components meet to form the acetabulum, a cup shaped cavity that accommodates the femoral head.
While studying for pelvic skeleton, it is mandatory that student have hip bone with them for understanding the different landmarks which are of great clinical, imaging and surgical importance (Fig. 1.22).
- Ilium: Iliac crest is the most prominent feature which provides attachment to iliac fascia, abdominal muscle and fascia lata. Projections at each end of iliac crest are the anterior and posterior superior iliac spines. The medial surface presents the iliac fossa, the iliac tuberosity and auricular surface, which articulates with the sacrum.
- Ischium: This consists of a body and a ramus—the body forms part of the acetabulum and the ramus fuses with the ramus of the pubis to complete the obturator foramen. Ischial spine delineates the greater and lesser sciatic notch above and below it. It has following significance:
- It is important clinical landmark on pervaginal examination for detection of progressive fetal descent.
- It is landmark in performance of pudendal nerve block and sacrospinous ligament vaginal suspension.
Ischial tuberosity is the rounded bony prominence upon which the body rest in the sitting position. - Pubis: This consist of a body and two rami. The superior ramus joins the ilium and ischium to form the acetabulum. The inferior ramus joins the ramus of the ischium to complete the obturator foramen. The upper part of the body forms the pubic crest and pubic tubercle and the medial surface forms a cartilaginous joint with the opposite pubis (the pubic symphysis). These three 24parts of the innominate bones is joined by bone in the adult and cartilage in the young.
Sacrum: It consists of five sacral vertebra joined by bone in the adult and cartilage in the young. There are four sacral foramina communicating with the sacral canal. The upper border of the pelvic surface is the sacral promontory. The sacrum articulates above with the fifth lumbar vertebra, laterally with the ilium and below the coccyx, which are 3–5 fused coccygeal vertebrae.
Foramina and Canals in the Pelvis
Obturator foramina: This is bordered by ischium and pubis and is occupied by fibrous sheet—the obturator membrane. Superiorly there is a small gap (canal) which communicates between the pelvis and the thigh and carries the obturator artery, vein and nerve.
Greater sciatic foramen: This is formed by the greater sciatic notch (ilium and ischium), the sacrotuberous and sacrospinous ligaments and ischial spine. It transmits the (a) Piriformis muscles, (b) Superior and inferior gluteal nerve and vessels, (c) Internal pudendal vessels and nerve, (d) The sciatic nerve, (e) Posterior femoral cutaneous nerves, (f) Nerve to the quadratus femoris.
Lesser sciatic foramen: This is bounded by the ischium and ischial spine and by the sacrotuberous and sacrospinous ligaments. It transmits—tendon of obturator internus, internal pudendal vessel and nerve. The nerve to the obturator internus passes lateral to the internal pudendal vessels and nerve, and innervates the obturator internus on the wall of the ischiorectal fossa.
Pudendal canal: This is a sheath of fascia on the lateral wall of the ischiorectal fossa, transmitting the internal pudendal vessel and nerves.
Sacral foramina: There are four pairs of these on each of the dorsal and ventral surface of the sacrum. They communicate with the sacral canal through the intervertebral foramina and transmit the dorsal and ventral rami of the first four sacral spinal nerves.
Sacral canal: The sacral canal is formed by the vertebral foramina of the sacral vertebrae, the lower opening is the sacral hiatus. As the spinal cord ends at the first lumbar vertebrae, the sacral canal contains only nerve roots (cauda equina) and the filum terminale.
The subarachnoid space extends to the lower border of 2nd sacral vertebrae and below this the dura mater and arachnoid form a closely applied covering of the filum terminale as it descends to its attachment on the first coccygeal segment.
General Feature of the Bony Pelvis
From obstetrical point of view, it is useful to consider the bony pelvis as a whole rather than separate two bones. In both women and men the pelvis form the bony ring through which the body weight is transmitted to lower extremities but in women it has a special form that adapt the childbearing or parturition. The sex differences in the pelvis are listed in Table 1.1.
The false pelvis lies above the linea terminalis and bounded posteriorly by the lumbar vertebra and laterally by the iliac fossa. In front the boundary is formed by the lower portion of the anterior abdominal wall. The true (or lesser) pelvis consists of a cavity with upper and lower openings. The cavity of true pelvis is like obliquely truncated bent cylinder with its greatest height posteriorly. Its anterior wall at the symphysis pubis measures about 5 cm and its posterior wall about 10 cm. It is divided for systemic description into three parts: (a) The brim, (b) The cavity, (c) The outlet (Fig. 1.23).
The Pelvic Brim (Inlet, Upper Pelvic Strait Syn)
The pelvic brim is bounded from anteriorly to posteriorly from center of upper border of pubic symphysis, along the pubic crest, part the pubic spine to the iliopectineal eminence, thence along the iliac portion of iliopectineal line to the sacroiliac articulation, thence along the lower border of the ala of the sacrum to the center of the sacral promontory (Fig. 1.24) (students are advised to have bony pelvis or model in hand). Shape of inlet of female pelvis is typically near round.
Fig. 1.24: The female pelvis—diameters of inlet (ab—Anteroposterior diameter, cd—Right oblique diameter, ef—Left oblique diameter, gh—Transverse diameter)
Caldwell and Moloy (1934) identified radiographically a nearly round or gynecoid pelvic inlet in approximately 50% of women).
Plane of pelvic brim is an imaginary flat surface bounded by the limits of pelvic brim. It is not strictly a mathematical plane and is therefore referred to as superior strait.
Inclination
Due to oblique articulation of the pelvis with the femora, the plane of pelvic brim is inclined at an acute angle of approximately 55 degrees to the horizontal surface, which is called angle of inclination of pelvic brim (Figs 1.25A and B).
The posterior border of the pelvic brim stands at a higher level than anterior, the sacral promontory being about 3¾ inch (9.4 cm) higher than upper border of symphysis pubis in the erect position. The fact plays an important basic for certain obstetric maneuver in breech delivery and shoulder dystocia.
When there is lumbarization of first piece of sacral vertebra there is low inclination, which has no obstetrical significance.
When there is sacralization of 5th lumbar vertebra, it is called high inclination. It has got following obstetrical significance – (a) There is delay in engagement because uterine axis fails to coincide with that of inlet, (b) It favors occipitoposterior position, (c) There is difficulty in descent of head due to long birth canal and flat sacrum which interferes in internal rotation.
Axis of Pelvic Brim
It is an imaginary straight line drawn perpendicular to the plane of the brim at its center. If it is extended upwards and downwards, this line passes through the umbilicus to coccyx. This line or axis of brim indicates the direction in which fetus passing through pelvic brim passes. It is also important that the uterine axis should coincide with the axis of the inlet so that force of uterine contraction will coincide in right direction for passage of baby through the brim (Fig. 1.25B).
Figs 1.25A and B: The female pelvis—inclination and axis: (A) AB—Horizontal line, CD—Axis of brim, EF—Plane of obstetrical outlet, GH—Axix of obstetrical outlet; (B) Obstetrical axis
Diameters of Pelvic Brim
Anteroposterior Diameter (Syn: True Conjugate, Anatomical Conjugate, Conjugate Vera):
It is the distance between the midpoints of the sacral promontory to the inner margin of upper border of symphysis pubis. It measures 11 cm (4 ¼ inch).
Obstetric Conjugate
It is the distance between the midpoints of the sacral promontory to prominent bony projection in the midline on the inner surface of the symphysis pubis. The point is somewhat below its upper border. It is the shortest anteroposterior diameter in the anteroposterior plane of the inlet. It measures 10 cm (4 inch).
Diagonal Conjugate
It is the distance between the lower border of symphysis pubis to the midpoint on the sacral promontory. It measures 12 cm (4 ¾ inch). Diagonal conjugate is important as it can be measured clinically during per vaginal pelvic assessment in late pregnancy or labor. Obstetric conjugate is computed by subtracting 1.2 cm from the diagonal conjugate (Fig. 1.26).
For practical purpose if the middle finger fails to reach the promontory or touches it with difficulty, it is considered that conjugate is adequate for average size fetal head to pass through.
Transverse Diameter
It is the distance between the two farthest apart points of the pelvic brim. This line crosses the true conjugate in its middle third and divides the brim into anterior and posterior segment. Strictly speaking it is not a diameter, since it does not usually pass through center.
Oblique Diameter
There are right and left oblique diameters which are measured from the right sacroiliac articulation behind to left iliopectineal eminence on the opposite side in the front and from left sacroiliac articulation to right iliopectineal eminence irrespectively. It measures 12 cm (4 ¾ inch).
Mid Pelvis (Pelvic Cavity)
It is the segment of the pelvis bounded above by the inlet and below by plane of least pelvic dimension (obstetrical outlet). It forms a curved canal with a shallow anterior wall measuring 3.75 cm (1½ inch), deep posterior wall measuring 11.25 cm (4 ½ inch), and lateral walls measuring 7.5 cm (3 inch). Shape of the mid cavity is almost round in typical gynecoid pelvis.
Plane of Mid Cavity
Usually a single mid plane of cavity is described which is bounded in front by the center of the symphysis pubis and behind by the junction of 2nd and 3rd sacral vertebra. It is the plane of greatest pelvic dimensions and represents the roomiest part of the pelvic cavity.
Diameters of Mid Cavity
Anteroposterior diameter: It measures from the midpoint on the posterior surface of the symphysis pubis to the junction of 2nd and 3rd sacral vertebrae. It measures 12 cm (4 ¾ inch).
Transverse diameter: It cannot be precisely measured as the points lie over the soft tissues covering the sacrosciatic notches and obturator foramina. It measures 12 cm (4 ¾ inch).
Oblique diameter: It cannot be precisely defined. Axis of the mid plane of the cavity is represented by a line the direction of which is intermediate between those of brim and the outlet.
Outlet of Pelvis
From obstetrical point of view it is useful to consider the outlet of the pelvis as its constricted lower portion and not merely as its lower bony limit. Bony limit or bone outlet is known as Anatomical outlet. It is Lozenge shaped space, bounded from anterior to posterior—lower border of symphysis pubis, laterally by ischiopubic rami, the ischial tuberosities, sacrotuberous ligaments, tip of coccyx (Fig. 1.27A). These boundaries of anatomical outlet are not in a single line, they form two triangular planes, which have a common base formed by a line joining the ischial tuberosities. Apex of anterior triangle is formed by the inferior border of the pubic arch and that of posterior triangle by the tip of coccyx.
Obstetrical Outlet
It forms a shallow bony segment which is bounded above at the level of ischial spine, which is known as narrow pelvic plane and below by the anatomical outlet (Fig. 1.27B).
Diameter of Anatomical Outlet
- Anteroposterior: It extends from the lower border of the pubic symphysis to tip of coccyx. It measures 11.5 cm when coccyx is in normal position and 13 cm (5 ¼ inch) when coccyx is pushed back by the head in second stage of labor.
- Transverse (Intertuberous diameter syn): It measures between inner border of two ischial tuberosity measuring 11 cm (4 ¼ inch). Oblique diameter cannot be defined as between ischial tuberosity and the coccygeal border the pelvic outlet is filled in with the soft structure only and these diameters are skeletal.
- Posterior sagittal diameter: It is the anteroposterior distance between the sacrococcygeal joint and midpoint of transverse diameter of anatomical outlet. It measures 8.5 cm (3 ½ inch). It is clinically measured by the distance between sacrococcygeal joint and anterior margin of anus.
So the obstetrical outlet must be clearly distinguished from anatomical outlet. Its anterior wall is defective at pubic arch, its lateral walls are formed by ischial bones and the posterior wall is made up of whole of coccyx.
Narrow Pelvic Plane (Plane of Least Pelvic Dimension Syn)
It is an imaginary flat surface bounded in front by the lower border of the symphysis pubis, laterally by the tips of ischial spines and posteriorly by the lower border of the last sacral vertebra.
Figs 1.27A and B: The female pelvis—anatomical and obstetrical outlet (PS—Pubic symphysis, IT—Ischial tuberosity, LSV—Last sacral vertebra, IS—Ischial spine)
Its shape is anteroposteriorly oval and measures 10.7 cm (4.3 inch).
It is general agreement to refer it as plane of outlet. Axis of narrow pelvic plane is represented by a line joining the center of its plane with the sacral promontory, the direction of which is nearly vertical than the axis of brim.
Diameter of Narrow Pelvic Plane
Anteroposterior diameter: It extends from the inferior border of pubic symphysis to the tip of sacrum, measuring 11 cm (4 ¼ inch).
Transverse diameter (bispinous): It is the distance between two ischial spines measuring 10.5 cm (4 1/5 inch).
Posterior sagittal: It is the distance between the tip of sacrum and the midpoint of bispinous diameter, measure 5 cm (2 inch).
Obstetrical Significance of Narrow Pelvic Plane
Narrow pelvic plane is the useful landmark for following reasons:
- It corresponds to the site of origin of levator ani muscles (Pelvic diaphragm).
- It marks the beginning of forward curve of pelvic axis.
- Ischial spines are easily felt on pervaginal examination. So it is an important landmark for clinical documentation of descent of presenting part in assessment of progress of labor. For example, if head has reached up to ischial spine, it is certain that head is engaged in the pelvic brim.
- At this level completion of internal rotation of head takes place.
- It is a landmark used for pudendal nerve block.
Other Obstetrical Significant Landmarks
- Subpubic angle: It is formed by the approximation of the two descending pubic rami. In gynecoid pelvis, it measures approximately 85°.
- Pubic arch: It is formed by descending rami of both the sides. At the level of 2 cm below the apex of subpubic arch it measures 6 cm. Clinically, it is assessed by placing the finger of hand side by side.
Waste Space of Morris
In gynecoid pelvis the subpubic arch is rounded and fetal head is well placed under the pubic arch. But in narrow pubic arch as found in android pelvis, the fetal head is displaced backwards and there is less room available for head. This distance between the lower border of symphysis pubis and the circumferences of the head is termed—waste space of Morris, which should not exceed 1 cm in proportionate pelvis.
When waste space of Morris is more than 1 cm, the anterior point of the anteroposterior diameter of the outlet extends below the symphysis pubis on the pubic rami for distance equivalent to the waste space of Morris. The distance between above point and the sacrum is called available anteroposterior diameter of the outlet. Through this available anteroposterior diameter the fetal head escapes out of the bony outlet (Figs 1.28A to C).
Axis of Pelvis
By uniting the axis of the three planes of pelvic brim, mid cavity and the outlet, a line is formed which traverse the center of the canal of the bony pelvis. It is uniformly curved, with anterior concavity. It is directed at first downwards and backwards (corresponding to axis of brim) than gradually more and more forwards (corresponding to axis of cavity and then outlet) until it reaches the axis of the outlet, where it has anterior concavity.
Figs 1.28A to C: Diagrammatic representation of: (A) Normal pubic arch; (B) Waste space of Morris; (C) Available anteroposterior diameter of the outlet
This line is known as anatomical axis of the pelvis or curve of Carus (Figs 1.25A and B).
Obstetrical Axis
Fetus passing through the pelvis does not follow the anatomical axis because pelvic cavity is almost cylindrical in its upper three fourth parts, so head descends in axis of pelvic inlet till level of ischial spines and than curves forward near the narrow pelvic plane.
This line represents obstetrical pelvic axis, which represent the real path of head through the pelvis. This line is straight in upper part and curved only in its lower portion.
Pelvic Shapes
Coldwell and Molloy (1933, 34) used special methods of stereoradiography which enabled them to study the architecture of pelvic in life size accurately. Coldwell and Molloy classification is still considered the gold standard for obstetrics and anticipating various difficulties and complications in different types of pelvis.
This classification is based on measurement of the greatest transverse diameter of the inlet and its division into anterior and posterior segment. The character of posterior segment determines the type of pelvis and the characters of anterior segment determines the tendency of pelvis.
| |||||||||||||||||||||
Both type as well tendency are not pure but determined because many pelvis are not pure but mixed type.
However, the four parent types of pelvis are:
- Gynecoid
- Anthropoid
- Android
- Platypelloid
Gynecoid pelvis is found in approximately 50% of women and intuitively suited for delivery of most fetuses. In contrast in android pelvis the posterior sagittal diameter at the inlet is much shorter than the anterior sagittal diameter, which limits the use of the posterior space by the fetal head. Beside, the anterior portion is narrow and triangular. So the extreme android pelvic passage has a poor prognosis for vaginal delivery.
In the anthropoid pelvis the anteroposterior diameter of the inlet is greater than transverse, which results in a narrow and somewhat pointed anterior segment. Anthropoid pelvis and its variant are found in approximately one third of the women.
The platypelloid pelvis has a flattened gynecoid shape with short anteroposterior and wide transverse diameter.
Table 1.3 summarizes the different characteristics of four types of pelvis.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
MULTIPLE CHOICE QUESTIONS
- Lymphatics from clitoris drain into
- Superficial inguinal lymph node
- Deep inguinal lymph node
- Lymph node of cloquet
- Obturator lymph node
Ans. a, b, c
- All of the following pelvic structure support the vagina except:
- Perineal body
- Pelvic diaphragm
- Levator ani
- Infundibulopelvic
Ans. d
- All of the following are classified as primary supports of uterus except:
- Transcervical ligament
- Pubocervical ligament
- Uterosacral ligament
- Broad ligament
Ans. d
- Peg cells are seen in:
- Vagina
- Fallopian tube
- Vulva
- Uterus
Ans. b
- Epithelial lining of Bartholin's duct is:
- Columnar
- Transitional
- Cuboidal
- Squamous
Ans. a
- The mucosal lining of vagina is composed of:
- Ciliated columnar
- Pseudostratified columnar
- Stratified squamous keratinized
- Transitional
Ans. c
- Bartholin's duct opens into:
- Labia majora
- Labia minora
- Lower vagina
- Groove between labia minora and hymen
- Corpus cervix ratio up to 10 years of age:
- 3:2
- 2:1
- 3:1
- 1:2
Ans. d
- The length of fallopian tube is:
- 8–10 cm
- 10–12 cm
- 15 cm
- None
Ans. b