HEALTH AND DISEASE
Health in its broadest sense is a dynamic state in which the individual adapts to changes in internal and external environments to maintain a state of well-being. The internal environment includes many factors that influence health, including genetic and psychological variables, intellectual and spiritual dimensions and disease processes. The external environment includes factors outside the person that may influence health, the physical environment, social relationships, and economic variables. Because both environments continuously change, the person must have to maintain a state of well-being. Health and illness therefore must be defined in terms of individual. Health can include conditions that the client or nurse may have previously considered to be illness. Health is also closely related to an individual's work place and home life; and stressors can be the result of those environments.
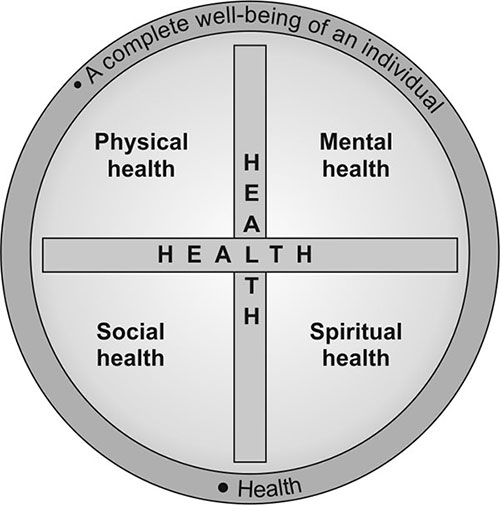
Health Definition by WHO (Fig. 1.1)
Concepts of Health, Illness and Sick Behaviors
- It is useful for the nurse to be aware of the behavioral components of health, illness and sick-role behavior.
- Every person develops a system of health belief and attitudes, and these tend to fall within the framework provided by society or cultural heritage.
- Health behavior activities of a person engage in, when feeling well, to take measures to prevent disease and illness, to detect them before symptoms occur.
- Illness behavior activities of person changes when feeling ill, that will lead to the defining of the state of health and that will gain help.
- Sick-role behavior activities of a person engages in believing himself ill. For any individual the level of health behavior is determined by the significance of symptoms—danger value, visibility, ambiguity, fear of unknown, the expectations of those from whom help is sought, feeling about dependence and fear of loss of control, the expectations of the illness position, including past experiences with illness.
Impact of Illness on Family
Behavioral and Emotional Changes
- People react differently to illness. Individual behavioral and emotional reactions depend on the nature of the illness, the client's attitude towards it, the reaction of others to it, and the variables of illness behavior.
- Severe illness, particularly one that is life threatening, can lead to more extensive emotional and behavioral change such as anxiety, shock, denial, anger and withdrawal.
Impact of Family Roles
- When an illness occurs, the roles of client and family may change. Such a change may be suitable and short-term or drastic and long-term.
- An individual and family generally adjust more easily to suitable, short-term changes. In most cases they know that the role change is only temporary.
- Long-term changes, however, require an adjustment process similar to the grief process. The client and family often require specific counseling and guidance to assist them in coping with role changes.
Impact on Body Changes
- Some illnesses result in changes in physical appearance; clients and families react differently to these changes.
- When changes in body image occur, such as results from a leg amputation, the client generally adjusts in the following phases: shock, withdrawal, acknowledgment, acceptance and rehabilitation.
- Withdrawal is an adaptive coping mechanism that can assist the client in making the adjustments.
Impact of Self-concepts
- Self-concept is individual's mental image of themselves, including how they view their strength and weaknesses in all aspects of their personalities.
- Self-concepts depend in part of body image and roles but also include other aspects of the psychological and spiritual self.
- Self-concept changes because of illness may no longer meet the expectations of the family, leading to tension or conflict.
Impact of Family Dynamics
- Family dynamics is the process by which the family functions, makes decisions, give support to individual members, and copes with everyday changes and challenges.
- If a parent in a family becomes ill, family activities and decision making often come to a habit that the other family members wait for the illness to pass, or they delay action because they are reluctant to assume the ill person's roles or responsibilities.
Health-illness Continuum
- According to Neuman (1990), health on a continuum is the degree of client wellness that exist at any point in time ranging from an optimal wellness condition, with available energy at its maximum, to death, which represents total energy depletion.
- According to health-illness continuum model (Fig. 1.2), health is a dynamic state that continuously alters as a person adapts to changes in the internal and external environments to maintain a state of physical, emotional, intellectual, social, developmental and spiritual well-being.
- The continuum is thought of a complex, dynamic process that includes physical, psychological and social components. There are adaptive or maladaptive behavioral responses to internal and external stimuli.
- Health and illness tend to merge but may represent pattern of adaptive change along the continuum. The direction of change may be reversible, depending on the quality of the individual's adaptive efforts.
- The individual at the illness end of the continuum is characterized by feeling of uncertainty, helplessness, loss of control, loss of identity and incapacity for problem solving (Fig. 1.3).
- As the patient is in the sick role, there is incapacity to meet other social roles, the person has sought diagnosis and get treatment.
- Less far along the illness end of the continuum, as illness behavior are brought into play, the person may be tired, rundown and irritable with complains of loss of sleep, appetite, dependence, self-absorpter, minor illnesses such as colds, infections, headaches and backaches.
- Between illness and wellness there is the ambiguous area where no symptoms are present and the person is neither especially well nor especially ill.
- At the health end of the continuum, as health behaviors are utilized, the person is not only unaware of disease and without pain, fatigue or somatic complications but also tends to be resistant to infections. The person tends to be industrious, vigorous and physically able, with a strong sense of identity and autonomy, carrying out usual social roles and needing no health care.
- The goal in preventive health care is to maintain equilibrium between health and illness, with balance in favor of maximum wellness for the individual.
Symptoms Experience
- During the initial stage, a person is aware that some thing is wrong. A person usually recognizes a physical sensation or a limitation in functioning, but does not suspect a specific diagnosis.
- The person's perception of symptoms includes awareness of a physical change such as pain, a rash, or a lump.
Assumption of the Sick Role
- The assumption of the sick role results in emotional changes, such as withdrawal or depression, and physical changes.
- Emotional changes may be simple or complex, depending on the severity of the illness, the degree of disability and anticipated length of the illness.
Medical Care Contact
- If symptoms persist despite home remedies, become severe or require emergency care, the person is motivated to seek professional health services.
- In this stage, the client seeks expect acknowledgment of the illness, as well as treatment. In addition, the client seeks an explanation of the symptoms, the cause of the symptoms, the course of the illness for future health.
- Client's illness can be validated at any point on the health-illness continuum. A health professional may determine that they do not have an illness or that illnesses are present and may belief threatening.
Dependent Client Role
- After accepting the illness and seeking treatment, the client enters the fourth stage of illness behavior.
- In this stage, the client depends on health care professionals for relief of symptoms. The client accepts care, sympathy and protection from the demands and stresses of life.
- It is socially permissible for clients in the dependent role to be relieved of normal obligations and tasks.
Recovery Stage
- The final stage of illness behavior—recovery and rehabilitation can arrive suddenly, such as a fever subsides.
- The recovery is not prompt; long-term care may be required before the client is able to resume an optimal level of functioning.
- In the case of chronic illness, the final stage may involve an adjustment to a prolonged reduction in health and functioning.
COMMUNITY, COMMUNITY HEALTH AND COMMUNITY HEALTH NURSING
Community
Community can be defined in numerous ways, depending on the application. The variety of individuals, families and cultural groups represented in a community contributes to the overall character of the community. Community-based nursing need to understand the community within which they practice. Knowledge of the community helps nurses to maintain quality of care.
Characteristics of Community
- Distinctiveness: Each community has defined as geographical boundaries having its beginning and end. These boundaries are more remarkable in smaller communities than in larger communities.
- Homogeneity: There is similarity in psychological characteristics of people living in the defined boundaries of the community, e.g. similarity in language, lifestyle, customs, tradition, etc.
- Closeness: The people in the community have face-to-face interaction and free communication. The extent of closeness varies. The community people frequently participate in common activities, etc.
- Sense of belongingness: The degree and intensity of this feeling may vary among members in the community.
- Sense of togetherness: There is unity and cohesiveness among the members in the community, which is based on their interaction and sense of belongingness to community.
- Self-sufficiency: The community provides all such means and facilities which help in meeting the basic needs of its people, i.e. space to live, education, protection and security, etc.
Functions of Community
- It provides space for housing, shelter, for socialization and recreation.
- It provides safety and security by protecting the community members.
- Linkages with social system outside the community for meeting needs of its members.
- Provides opportunity for employment and sustenance.
- Protection, distribution and consumption of goods and services.
- Socialization and education for its members.
- Provides opportunities for interaction amongst members, transmits information, ideas and beliefs and provides support system.
Community Health
Community health is defined more broadly and encompasses the entire gamut of community organized efforts for maintaining protection and improves the health of the people. Community health postulates a unified and balanced integration of curative, preventive and promotive health services. The primary motto is promotion of well being (physical, mental and social).
Definition
- According WHO, community health refers to the health status of the members of the community to the problems affecting their health and to the totality of health care provided for the community.
- Community health refers to the health status of the members of the community, to the problems affecting their health and to the totality of health care provided to the community.
- Community health implies, in a broad sense, integration of curative, preventive and promotive health services. The traditional and important responsibilities of public health are now included in the concept of community health.
The community health demands are placed on the nurse and the nursing profession as a result of changes in society, especially changes in modern technology, social consciousness, and the quality, type and financing of health care. Emphasis has shifted from acute hospitalized-based care to preventive community health care. All changes that affect the health care delivery system affect nursing.
- It is concerned with motivating individuals and group, to learn healthy life styles and to achieve optimum health.
- It involves co-ordinated group activities on the part of a team, representively a number of disciplines. For example demography, epidemiology, statistics, sociology, etc.
- There is a traditional role assigned to the nurses in community diagnosis and treatment. It is one of the important milestones in the nursing profession because health problems have been, and still are the basis for planning for providing health services.
According to CEA Winslow (1920), community health is the science and art of preventing disease, prolonging life, and promoting health and efficiency through organized efforts for:
- The sanitation of the environment.
- The control of communicable diseases.
- The education of the individual through personal hygiene.
- Early diagnosis and preventive care of disease.
- The development of social machinery so as to enable every citizen to realize his/her birth right of health and longevity, to ensure every individual a standard of living, adequate enough for the maintenance of good health.
Community Health Nursing
Definitions
- “Community health refers to the health status of the members of the community, the problems affecting their health and the totality of health care provided for the community”—Blum.
- Community health or public health is defined as “the art and science of maintaining, protecting and improving health of people through organized effects”—American Association of Public Health.
Nature of Community Health Nursing
The community is responsible for providing all facilities and total care to all. Such changes have led to the placement of the term public health with community health. Hence ‘community health’ encompasses all those process of prevention of disease, promotion and protection of health of all people.
Community health nursing (Fig. 1.4) implies making systematic assessment and diagnosis of health status of people and their problems, planning and implementing 7comprehensive health care services for the entire community with their active co-operation and participation. In community health nursing, the major emphasis is laid on primary level prevention through community approaches.
The community health nursing implies sound preparation of community health personnel so that they are knowledgable and skillful. They need to acquire knowledge about community structure, community dynamics, community approaches, population statistics, community health indicators, epidemiological aspects of health problems, health planning, administration and delivery system.
DIMENSIONS OF HEALTH
The WHO definition envisages three dimensions —the physical, the mental and the social (Fig. 1.5). Many more may be cited, viz. spiritual, emotional, vocational and political dimensions.
Physical Dimension
The state of physical health implies the notion of ‘perfect functioning’ of the body. It conceptualizes health biologically as a state in which every cell and organ is functioning at optimum capacity and in perfect harmony with the rest of the body.
Mental Dimension
Mental health is the ability to respond to the many and varied experiences of life with flexibility and a sense of purpose. More recently, mental health has been defined as, “a state of balance between the individual and surrounding world, a state of harmony between oneself and others, a coexistence between realities of self and other people of the environment”. Mind and body were considered independent entities.
Social Dimension
It has been defined as the “quantity and quality of an individual's interpersonal ties and extent of involvement with the community”.
Social health takes into account that every individual is a part of a family and of wider community; focuses on social and economic conditions and well-being of the ‘whole person’ in context of his social network.
Spiritual Dimension
It refers to that part of individual which reaches out and strives for meaning and purpose in life. It is intangible—“something that transcends physiology and psychology. It includes integrity, principles of ethics, the purpose in life, commitment to some higher being and belief in concepts that are not subject to ‘state of art’ explanation”.
Emotional Dimension
Emotional health relates to ‘feeling’. Experts in psychology have been relatively successful in isolating these two separate dimensions. With this new data, mental and emotional aspects of humanness may have to be viewed as two separate dimensions of human health.
Vocational Dimension
It is a part of human existence. When work is fully adapted to human goals, capacities and limitations, work often plays a role in promoting both physical and mental health. Physical work is usually associated with an improvement in physical capacity, while goal achievement and self realization in work are sources of satisfaction and enhanced self-esteem.
HEALTH DETERMINANTS
Community health is influenced by various factors which interact with each other and determine the health status of many individuals families and communities at large, at any given point of time (Fig. 1.6).
Human Biology
Genetic Inheritance
Hereditary or genetic predisposition to specific illness is a major physical risk factor. For example, a person with a family history of diabetes mellitus is at risk for developing the disease later in life. Other documented genetic risk factors include family history of cancer, coronary disease and renal disease.
Age
Age increases susceptibility to certain illness. For example, the risk of cardiovascular disease increases with age, for both sexes. The risk of birth defects and complications of pregnancy increase in childbearing women after the age of 35. Age risk factors are often closely associated with other risk factors such as family history and personal habits.
Race
Race increases susceptibility to certain illness. For example, the risk of sickle cell anemia is more common in Africans and Mediterranean people.
Self-concept
Self-concept implies individual's perception of his/her physical, intellectual and social abilities.
Environment
Physical Environment
The physical environment includes atmospheric pressures, gravity, light and sound waves, temperature, humidity, wind velocity, solar radiation, electromagnetic fields and seasonal variations, etc. The variety of pollutants is found to pollute air, water, food and soil and is the cause of various acute and chronic diseases, e.g. gastrointestinal, respiratory, skin cancer, cardiovascular diseases, etc.
Biological Environment
Most of the plants and animals are useful to human being to promote health, but at the same time, they produce diseases like malaria, insect bites and allergic reactions.
Social Environment
The social environments include other people and social institutions, socio-cultural events, religious beliefs, moral and ethical values, and social rules and regulations pertaining to living society, socioeconomic support system, etc.
Lifestyle
Many activities, habits and practices involve risk factors; the stress of life crisis and frequent life changes also increase risk factors. Health practices and behaviors can have positive or negative effects in health. Practices with potential negative effects are risk factors. These include overeating or poor nutrition, insufficient rest and sleep and poor personal hygiene. Other habits that put a person at risk for illness include smoking, alcohol or drug abuse, and activities involving a threat of injury such as skydiving or mountain climbing. Prolonged emotional stress may increase the chance of illness. Emotional stress may occur with events such as divorce, pregnancy and arguments. Job-related stresses, for example, may overtax a person's cognitive skills and decision making ability leading to mental overload or burnout.
Health and Allied Health Resources
Health Services
Health services are directly concerned with improvement of health status of people. Health services can also contribute on socioeconomic development of people because sound health can improve and increase the physical, intellectual and emotional capacity of people to get educated, work and earn for their livelihood, improve their life style which will further reinforce their health.
Socioeconomic Conditions
Socioeconomic conditions have significant influence on community health. In developed countries like America, UK and Canada, there has been significant reduction in the morbidity and mortality rates, and increases in longevity at birth because of socioeconomic developments. Socioeconomic conditions include economic status, education, occupation and living standards.
Political System
The political system has a very strong role in health promotion of people in the country. The health care delivery system is determined by the political system though there is constitutional control. Decisions pertaining to health policy, allocation of funds, programmes, manpower development, infrastructure, health technology and delivery of health services are made by the ruling party within the parliament system.
Health-related Services
The health-related services include education, governmental policies, social welfare, developmental programs, food and agriculture, industry, communication and broadcasting, rural and urban 10development, and transportation facilities. The health-related services needs to have balanced approach with National Health Policy and voluntary health promotes active participation.
INDICATORS OF HEALTH
Indicators help to measure the extent to which the objectives and targets of a program are being attained.
Characteristics
- Indicators should be valid: They are actually measures, what they are supposed to measure.
- It should be reliable and objective: The answer should be the same if measured by different people in similar circumstances.
- It should be sensitive: They should be sensitive to changes in the situation concerned.
- It should be specific: They should reflect changes only in the situation concerned.
- It should be feasible: They should have the ability to obtain data need.
- It should be relevant: They should contribute to the understanding of the phenomenon of interest.
Uses
- To measure the health status of a country.
- To compare the health status of one country with that of another country.
- To assess the health care needs.
- To plan and implement health care services.
- To evaluate the health care services.
Since, health is not defined in measurable terms and is multidimensional and never static, health is measured multidimensionally, indirectly.
Classification
These indicators are classified as follows:
- Mortality indicators (Table 1.1).
- Morbidity indicators (Table 1.2).
- Disability rates.
- Nutritional status indicators.
- Health care delivery indicators.
- Utilization rates.
- Indicators of social and mental health.
- Socioeconomic indicators.
- Health policy indicators.
- Environmental indicators.
- Indicators of quality of life.
- Other indicators (Table 1.3).
|
|
LEVELS OF HEALTH CARE
Health services are usually organized at three levels, each level supported by a higher level to which the patient is referred. These levels are described in Table 1.4.
|
PRIMARY HEALTH CARE: ELEMENTS AND PRINCIPLES, NURSE'S ROLE IN PRIMARY HEALTH CARE
Definition
Primary health care (Fig. 1.7) is essential health care, made universally accessible to individuals and families in the community, by means acceptable to them, through their full participation, and at a cost that the community and country can afford. It forms an integral part both of the country's health system of which it is the nucleus, and the overall social and economic development of the community (Alma Ata 1978).
Highlights of this Definition
This definition highlights several attributes of primary health care. It stresses on:
- Its essentiality by observing that primary health is essential health care.
- Its ‘accessibility’ by observing that health care is “made universally accessible to individuals and families in the community.
- Its ‘acceptability’ by observing the means acceptable to them.
- Its ‘patricianly’ by observing that health care acts a cost that the community and country can afford.
- Its ‘affordability’ and integrating by observing that it forms an integral part both of the country's health system of which it is the nucleus and the overall social and economic development of the community.
Attributes of Primary Health Care
Accessibility
Primary health care permeates uniformly to reach equitably to all segments of population.
Acceptability
Primary health care achieves acceptability through cultural assimilation of its policies and programs.
Adaptability
Primary health care system is highly flexible and adaptable. It believes in ‘adaptation’ rather than ‘adoption’.
Affordability
Primary health care is affordable to consumers as well as providers.
Availability
Primary health care is always ready to respond to any demand at any time.
Appropriateness
Primary health care system evolves from the socioeconomic conditions, social values and health situation of a community, it is quite appropriate from all angles.
Closeness
Primary health center is close at hand to people at their door steps.
Continuity
Primary health service is a continuous service, which extends from ‘womb’ to tomb and addresses the changing needs of an individual in all situations of health and disease.
Comprehensiveness
Primary health care is comprehensive and the curative need of the community.
Co-ordinativeness
Primary health care is dependent on intersectoral co-ordination and community participation.
Elements of Primary Health Care
As per Alma Ata declaration primary health care includes:
- Education on prevailing health problems and methods of identifying, preventing and controlling them.
- Promotion of food supply and proper nutrition.
- An adequate supply of water and basic sanitation.
- Maternal and child health care including family planning.
- Immunization against the major infectious disease.
- Prevention and control of locally endemic diseases.
- Appropriate treatment of common diseases and injuries.
- Promotion of mental health.
- Provision of essential drugs.
Principles of Primary Health Care
Equitable Distribution
Primary health care services must be shared equally by all people irrespective of their ability to pay (rich, poor, urban or rural).
Community Participation
Primary health care must be a continuing effort to secure meaningful involvement of the community in the planning, implementation and maintenance of health services.
Coverage and Accessibility
Primary health care implies providing health care services to all, who required them. The care has to be appropriate, adequate in content and in amount to satisfy the essential health needs of the people and has to be provided by methods acceptable to them.
Intersectoral Co-ordination
Primary health care requires joint efforts of other health-related sectors such as agriculture, animal husbandry, food, industry, housing, social welfare, public works, communication and other sectors.
Appropriate Health Technology
The technology that is scientific, adaptable to local need and socially acceptable instead of costly methods, equipment and technology.
Human Resource
Health resource is very essential to make full use of all the available resources including the human potential of the entire community.
Referral System
Referral system would be desirable to develop a methodology for referring from one level to another with laid down procedures and policies.
Logistics of Supply
The logistics of supply include planning and budgeting for the supplies, required procurement or manufacture, storage distribution and control.
Physical Facilities
The physical facilities for primary health care need to be simple and clean. It should have a spacious waiting area with toilet facility.
Control and Evaluation
A process of evaluation has to be built to assess the relevance, progress, efficiency, effectiveness and impact of the services.
Role of Community Health Nurse in Primary Health Care
An extent committee on community health nursing was concerned by WHO executive board in July 1974 to recommend ways through which nursing could have critical impact on the urgent health problems throughout the world. The committee made specific recommendations, which are as follows:
- The development of community health nursing services, responsive to community health needs that would assure primary health care coverage for all.
- The reformulation of basic and post-basic nursing education as to prepare all nurses for community health nursing.
- The inclusion of nursing in national development plans in a way that would ensure the rational distribution, appropriate utilization and support of nursing personnel.
HEALTH FOR ALL BY 2000 AD
- The World Health Assembly in its 30th meeting, in 1977, decided the goal of Health for all (HFA) and defined that main social targets of Governments and WHO in the coming decades should be the attainment of a level of health for all citizens of the world by the year 2000, that will permit them to lead socially and economically productive life.
- Attainment of a level of health that will enable every individual to lead a socially and economically productive life.
Health for All Goals
- Realization of highest possibility of health, which includes physical, mental and social well-being.
- Attainment of minimum level of health that would enable to the economically productive and participate actively in social life of community, in which they live.
- Removal of obstacles to health such as unemployment, ignorance, poor living conditions, standards and malnutrition, etc.
- Health care services are within the reach of all in the country.
Strategies for Health for All
The Alma Ata declaration called for global strategy to provide guidelines for member countries to refer. In 1981, the WHO after consultation with member countries developed a global strategy for health for all. The global strategy provides common broad frame work, which can be modified and adopted by countries according to their needs. The global strategy for HFA is based on the following principles.
- Health is a fundamental human right, a worldwide social goal and an integral part of social and economic development of the communities.
- People have the right and the duty to participate individually and collectively, in the planning and implementation of their health care.
- The existing gross inequality, in the health strategies, is of common concern of all countries and must be drastically reduced.
- Government has responsibility for the health of their people.
- Countries and people must become self-reliant in health matters.
- Governments and health professionals have the responsibility of providing health information to people.
- There should be equitable distribution of resources within and among the countries, but should be allocated most to those who need most.
- Primary health care would be the key to the success of HFA and it has to be the integral part of the country's health system.
- Development and application of appropriate technology according to health care system of the nation.
- Research in the field of biomedical and health services must be conducted and findings should be applied soon.
The National Health Policy echoes the WHO, a call for HFA and the Alma – Ata declaration. It had laid down specific goals with respect of various health indicators by different dates such as 1990 and 2000 AD. Some of the goals are:
- Reduction of infant mortality from the level of 125 (1978) to below 60.
- To raise the expectation of life at birth from the level of 5 years to 64.
- To reduce the crude death rate from the level of 14 per 1000 population to 21.
- To reduce the crude birthrate from the level of 33 per 1000 population to 21.
- To achieve a net reproduction rate of one by rural population.
COMMUNITY HEALTH TEAM
Community health nursing is concerned with the people who are sick as well as the healthy, young and old, male and female. Community health and community health nursing draw knowledge and practices from other disciplines such as medicine, surgery, pediatrics, obstetrics, gynecology, dentistry, health education and vital statistics.
The community center may refer a patient directly to the state level hospital or the nearest medical college hospital. The community health center has the following staffs and collectively called community health team (Fig. 1.8).
Functions of Community Health Team Members
Medical Officer
- Medical officer is the planner, promoter, organizer, supervisor, co-ordinator and evaluator of all functions in PHC.
- Medical officer monitor the OP patients in the morning and afternoon he does field visit.
- Visit subcenter on fixed days and hours. He gives guidance to team.
- He conducts staff meeting once every month and discuss problems, reviews the progress of health activities.
- He ensures that National Health Programs are implemented properly.
Female Health Worker
- Registration and care of prenatal and postnatal mothers at home.
- Registration and follow-up of all eligible couples.
- Provide nutrition advice and immunization to mothers and children.
- Refer mothers and children at the time of need, to hospitals and follow them up after discharge.
- Carryout family planning services including the distribution of contraceptives.
- Provide treatment for minor ailments.
- Notify communicable diseases.
- Maintenance of records and register of all the services provided and also of vital events such as births and deaths.
Male Health Worker
- Conduct survey of the subcenter area and maintain record of all families.
- Maintain information of all vital events.
- Participation in Malaria Control Program.
- Participate in family planning services by keeping a list of all eligible couples; provide information on the family planning acceptors.
- Participate in nutritional program.
- Promote health education activities.
- Identifying and reporting about communicable diseases.
- Co-ordinating the activities with female health worker and block staff.
- Maintaining records.
A qualified community health nurse is prepared to give a generalized or multipurpose service in home, school and in industry. She functions in the field of administration and supervision, education, training personnel, health services and research.
PHILOSOPHY, GOALS, OBJECTIVES AND PRINCIPLES OF COMMUNITY HEALTH NURSING PRACTICE
Philosophy
Nursing contributes to the health services in a vital and significant way, in the health care delivery system. It recognizes national health goals and is committed to participate in the implementation of National Health Policies and Programs. It aims at identifying health needs of the people, planning and providing quality care in collaboration with other health professionals and community groups. It focus on the following:
- The essential dignity and worth of the individual.
- The right of an individual for basic necessities.
- The right of the individual to help in times of need and crisis.
- The great capacity for growth within all social beings.
- The possession of potentialities and resources by individuals for managing their own lives.
- The need for individuals to struggle and strive to improve their life and environment.
- The importance of freedom to express one's individuality.
Objectives
Nursing seeks to help people understand the importance of all segments of their life and the environment in their well-being (Fig. 1.9). Nursing uses scientific knowledge to perform activities to prevent illness and to help those with health problems to regain vigor and joy of living. Social changes taking place in the community must be considered while planning health care.
Nurses are key persons in providing health care in our changing society. Health education has for a long time been considered as a major nursing responsibility. That responsibility is increasing with our social trends. Because nurses live in the community and have their own families, they are accessible to the people of the community. They are often called for help in emergencies or to give advice.
Goals
- To increase the capacity of families, groups and communities to cope with health and illness problems.
- To support and supplement the efforts of other professionals, restoration and preservation of health.
- To control or counteract, as much as possible the physical and social environmental conditions that threaten health or decrease the enjoyment of life.
- To contribute to the reinforcement and improvement of nursing practice, public health practice and service.
Principles
The following are some main principles, which may be used to guide for the community health nurse.
- Effective health workers, irrespective of position or place of work, function as a team.
- The community nurse should be a qualified person by a recognized school or college.
- Health services should be based on the felt-needs of an individual, family and community.
- Health services should be made available to all people, irrespective of their age, sex and status.
- Community health nurses are held accountable/responsible as authorized health authority for their services.
- Health services should be realistic in terms of available personnel and facilities.
- Professional relationship and etiquette are essential in community health services.
- Community health nurse must be a non-political and non-sectarian, in her relationship with people.
- Evaluation and follow-up services are important aspects in community health programs.
- Facilities for further training and continuing education should be provided by the health authority.
- Community health nurse should organize periodical in-service education programs.
- Community health nurse should organize and lead a team effectively and efficiently to provide best service to the community.
- The family and community are the units of work. There should be adequate and accurate baseline data of the community which is essential.
- Supervision and guidance are needed to help the worker to produce a high quality of work.
- Records and reports are essential in community health services.
- The community health nurse should prepare updated records and reports, and sent to their higher level promptly.
- The public health worker must never accept gifts or bribes.
- Professional interest should be developed and maintained.
- Job condition should be conducive to optimum satisfaction.
QUALITIES AND FUNCTIONS OF A COMMUNITY HEALTH NURSE
Community health nurse is a personnel, serving at the community level, who provide basic promotive, preventive, curative and rehabilitative services directly to the community. The specific nursing activities which are performed by the nurse will vary according to community needs and the structure of the primary health care system.
Qualities
- A qualified community health nurse is one who has undergone basic general nursing, midwifery training and post-basic education in community health nursing.
- A community health nurse must have interest in people and in understanding human behavior.
- Sincerity and ability to empathize are basic qualities required for a nurse.
- A well-poised nurse has a friendly disposition, will be honest, charitable, resourceful and co-operative and takes responsibilities with initiative.
- Minimum essential skills of a nurse are observation, communication, interviewing, and bedside supportive and technical skills.
- She must have abilities to make interpretations, make judgments and take decisions.
Functions
Community health nursing functions (Fig. 1.10) vary according to the designation for which the nurse is employed and according to her education and experience. Some community health nurses 21function on the staff level, while others serve in the capacity of administrator, supervisor or instructor in health organizations.
- Community health nurse provides comprehensive health care to individuals, families and groups by teaching, counseling and providing guidance.
- Community health nurse develop goals to meet the need. She develops an action program, evaluates progress and plans again as needed.
- Provide assistance to the family in improving environmental conditions that affect health; she helps to plan a safe environment in the home, school and industry.
- Providing supportive services to doctor such as early symptom detection and giving technical help.
- Demonstration and teaching of skilled nursing care of the sick in the home.
- Supervision of work of midwives, dais and other nursing personnel.
- Helping in the adjustment of social and emotional conditions that affect health.
- Co-ordination of her work with other members of the health team, working in the community.
- Revising and revitalizing plan and programs.
- Epidemiologic investigation in the field of communicable diseases such as tuberculosis, sexually transmitted diseases, leprosy, etc.
- Organizing planned group classes in health with emphasis on applied nutrition, sanitation, child care, parent craft and family welfare services.
- Development and utilization of facilities such as other branches of health and welfare services for making referrals and for promotion of sound and adequate health programs.
- She is responsible for planning, implementation and evaluation of a practical plan of nursing administration within the primary center and its associated subcenters.
- The community health nurse involves in nursing research and collection of vital statistics.
- Evolution and development of community health nursing in India and its present concept.
- Evaluating the differences between institutional and community health nursing.
CONCLUSION
Nursing, in the minds of many people, is associated with medicine and hospitals, because most nurses work for hospitals caring sick people. The major purpose of the hospital is to support the medical regimen in treating disease and dysfunction. The public image of what nursing is and what nurses do has been influenced by medical definition of health as a ‘absence of disease.’
A community health nurse need to know about a community, of which importance is the composition, character, role and capabilities of population group and agencies that exist in the community. The community health nurse needs to have a development perspective on the community: The trends, patterns of change, and a problem-orientation in which the needs and demands of groups are viewed, against the real and potential resources available to address the needs and demand.
BIBLIOGRAPHY
- Craven R, Himle C. Fundamentals of Nursing, 2nd edition. Lippincott; Philadelphia: 1996.
- Harkness Hood G, Dincher JR. Total Patient Care: Foundations and Practice of Adult Health Nursing, 8th edition. Mosby-Year Book, mc; St. Louis: 1992.
- Lindberg JB, et al. Introduction to Nursing Concepts, Issues and Opportunities. JB Lippincott Co; Philadelphia: 1990.
- Potter PA, Perry AG. Fundamentals of Nursing: Concepts, Process and Practice, 3rd edition. Mosby Year Book, mc; St. Louis: 1993.
- Purtilo R. Health Professional and Patient Interaction, 4th edition. WB Saunders; Philadelphia: 1990.
- Timby BK, Lewis LW. Fundamental Skills and Concepts in Patient Care, 5th edition. JB Lippincott; Co, Philadelphia: 1992.