ANSWERS
1. The answer is d. (Bailey 25th edition) Testicular torsion is a surgical emergency that occurs commonly in adolescents. The underlying pathology is secondary to an abnormally narrowed testicular mesentery with tunica vaginalis surrounding the testis and epididymis in a bell clapper deformity. As the testis twists, it comes to lie in a higher position within the scrotum. Urinalysis is usually negative. Elevation will not provide a decrease in pain (negative Prehn sign); a positive
Prehn sign might indicate epididymitis. Angel's sign (testis which has undergone torsion lies at a higher level) is also suggestive of testicular torsion.
Torsion is a clinical diagnosis and one should not wait for a Doppler to operate on the patient. This patient's pre-sentation warrants immediate operation. Both the affected and the unaffected testes should undergo orchiopexy. The differential diagnosis between torsion of the testicle and epididymitis is sometimes quite difficult. On occasion, the physician has to explore a patient with epididymitis just to rule out a torsion of the testicle.
Epididymitis usually occurs in sexually active males. Urinalysis is usually positive for inflammatory cells, and urethral discharge is often present.
2. The answer is b. (Devita 9th edition) Patient has an early breast cancer with a negative axilla. She has no contraindications for BCS and is an ideal candidate for the surgery. To address her axilla she will require a sentinel lymph node biopsy. Radiotherapy to the chest wall is mandatory after breast conservation surgery. As the size of the lesion is more than 1cm, it is an indication for adjuvant chemotherapy as well. On account of ER and PR positivity, patient with require hormonal therapy as well.
Contraindications to Breast Conservation Surgery
Absolute Contraindications
- Pregnancy is an absolute contraindication to the use of breast irradiation.
- Women with two or more primary tumors in separate quadrants of the breast or with diffuse malignant-appearing microcalcifications are not considered candidates for breast conservation treatment.
- A history of prior therapeutic irradiation to the breast region.
- Persistent positive margins after two surgical attempts.
Relative Contraindications
- Collagen vascular disease is a relative contraindication to breast conservation treatment because published reports indicate that such patients tolerate irradiation poorly
- Large tumor to breast ratio
3. The answer is b. (Bailey 25th edition) Buerger's disease (Thromboangiitis obliterans)
- Age – young men below 40 years of age, with history of smoking.
- It characteristically involves small and medium sized arteries (plantars, tibial, radial). Both upper and lower extremities are affected. Lower extremity is more commonly involved
- It is the inflammatory reaction in arterial wall with involvement of neighboring vein and nerve.
- Patient complains of claudication and presents with dry gangrene
- Management involves smoking cessation and conservative amputation. Sympathectomy provides temporary relief and is contraindicated in intermittent claudication.
4. The answer is c. This is a classic description of nodular basal cell carcinoma (BCC). BCC is usually described as a pearly, telangiectatic nodular lesion with rolled borders.
- Major risk factors are childhood sun exposure, fair skin, chronic dermatitis, and xeroderma pigmentosum.
- BCC is usually very slow-growing, but can result in extensive destruction of local tissues and extension into the central nervous system if untreated.
- Basal cell nevus syndrome, a genetic form of BCC, is associated with mutation in the PTCH gene.
- Moh's micrographic surgery is used in the management of basal cell carcinoma.
- It commonly occurs on the face above the line joining the angle of mouth and the ear lobule.
SCC is classically a scaly, erythematous lesion that may ulcerate. Cutaneous SCCs metastasize, typically to adjacent lymph nodes.
Risk factors for metastatic lesions include location in scar tissue, immunodeficiency, exposure to x-rays and ultraviolet radiation, and location on the head or neck.
Prognosis is excellent if completely excised (95% cure rate), but survival is only 50% at 5 years if metastatic.
Keratin pearls are seen in histo-pathology.
Seborrheic keratosis (SK), which can mimic malignant melanoma, SCC, or BCC, but is a benign lesion. Horny cysts embedded in the surface of the lesion, when present, support this diagnosis. Abrupt eruption of multiple pruritic SKs may occur as a paraneoplastic syndrome (the sign of Leser-Trelat, most commonly seen with gastrointestinal adenocarcinomas), but this association is controversial.
(Bailey 25th edition)
5. The answer is b. (Sabiston 19th edition) Aortic dissection, especially in the ascending portion, is most commonly associated with hypertension.
Acute management of this potentially life-threatening condition involves blood pressure control and prompt evaluation for surgical repair.
Debakey Type I | Debakey Type II | Debakey Type III |
|---|---|---|
Ascending and descending Aorta | Ascending Aorta only | Descending Aorta only |
Stanford A – Proximal | Stanford B – Distal |
Aortic aneurysms, especially in the abdomen, are most commonly associated with atherosclerosis. Until they rupture, these generally present no distress to the patient and may be discovered incidentally. Aortic aneurysms larger than 5 cm are generally treated surgically.
Trauma is a possible etiology of aortic dissection, and this must be ruled out in incidents of trauma, but hypertension is still most common etiology of aortic dissection.
6. The answer is d. (Bailey 25th edition) The most common causes of small bowel obstruction include peritoneal adhesions (from previous abdominal surgery). The abdominal pain typically presents with nausea and/or vomiting, and patients may have a distended abdomen along with high-pitched bowel sounds. Supine and upright x-ray of the abdomen are useful in making the diagnosis because dilated loops of small bowel can be seen, along with air-fluid levels and lack of gas in the colon.
Some patients with partial small bowel obstruction can initially be treated conservatively with close observation, intravenous fluids, and a nasogastric tube for proximal decompression. However, patients with peritoneal signs should be taken to the operating room for surgical decompression and repair.
The acute onset of diffuse abdominal pain and emesis in a patient with a history of previous abdominal surgeries supports a diagnosis of small bowel obstruction more than colon cancer. Although tumors and cancers of the small bowel can cause obstruction, it is unlikely that colon cancer would produce the history, physical examination findings, and radiographic findings noted in this case.
Mesenteric ischemia may present with abdominal pain, nausea, and vomiting; however, the radiographic findings are not typically seen in a patient with mesenteric ischemia. In addition, the majority of cases 52of mesenteric ischemia occur in older patients who have cardiac abnormalities or atherosclerosis.
Patients with a diagnosis of pancreatitis may present with diffuse abdominal pain, nausea, and vomiting; however, the radiographic findings are not typically seen in a patient with pancreatitis.
7. The answer is d. (Maingot's Abdominal Operations) Diffuse rebound rebound tenderness most likely indicates generalized peritonitis, which, combined with signs and symptoms of small bowel obstruction (SBO), most likely indicates rupture of inflamed, obstructed small bowel. This is a surgical emergency requiring an immediate operation. The other symptoms that are worrisome in a patient believed to have an SBO are tachycardia, hypotension, and metabolic acidosis. Bowel sounds can be variable in small bowel obstruction, although the classic presentation is high-pitched tinkles and peristaltic rushes. Although the absence of bowel sounds indicates a progression, it does not necessarily warrant a surgical emergency. Absent bowel sounds can also be seen in non-mechanical bowel obstruction.
The absence of flatus indicates a complete obstruction (obstipation). This is worrisome for a complete obstruction but does not warrant a surgical emergency.
Bilious vomiting is commonly seen in SBO, and the more proximal the obstruction, the more common is the bilious vomiting (although it will not be seen if the obstruction is proximal to the second portion of the duodenum where the common bile duct empties into the duodenum). Although SBO is an indication for surgery within 24 hours, additional diagnostics would need to be performed to confirm this diagnosis.
8. The answer is b. (Bailey 25th edition) The patient has a pheochromo-cytoma, which is associated with multiple endocrine neoplasia (MEN) types 2A and 2B. MEN 2A includes medullary thyroid carcinoma, pheochromocytoma, and parathyroid hyperplasia. MEN 2B includes medullary thyroid carcinoma, pheochromocytoma, and mucosal/gastrointestinal neuromas. Other neoplastic diseases associated with pheochromocytoma include von Hippel-Lindau syndrome and neurofibromatosis.
The gene implicated in MEN 2 syndrome is the RET proto-oncogene.
Medullary carcinoma thyroid in MEN 2B syndrome has the worst prognosis.
- [remember: 2 = Second = Sipple]
- [remember 1 = Won = Wermer's]
MEN 1 = 3 P's – Pituitary adenoma, parathyroid adenoma/ hyperplasia and pancreatic tumors.
9. The answer is c. (Devita 9th edition) Stewart-Treves syndrome is a cutaneous angiosarcoma that develops in long-standing chronic lymphedema. Most commonly, this tumor is a result of lymphedema induced by radical mastectomy to treat breast cancer. Lymphangiosarcoma typically develops in patients many years after mastectomy, more commonly 5-15 years after surgery. The lesions of Stewart-Treves syndrome typically appear as multiple reddish blue macules or nodules that may become polypoid. Around these nodules, small satellite areas can develop and become confluent, forming an enlarging lesion.
Although Stewart-Treves syndrome develops after radical mastectomy in most patients, lymphangiosarcoma also develops in other forms of acquired lymphedema and in congenital lymphedema. The most common approach in patients with lymphangiosarcoma is amputation of the limb or forequarter rather than wide local surgical excision. Even in cases with early surgical treatment, the prognosis is disappointing, with a high rate of local recurrence and metastasis.
10. The answer is a. (Bailey 25th edition, Maingot's Abdominal Operations) Patient has the classical triad of choledocholithiasis [Charcot's triad] – intermittent pain, fever, jaundice.
Reynold's pentad – Charcot's triad plus altered mental status and septicemic shock.
The elevated total bilirubin implies obstruction at this site, with consequent backup of bile into the liver, causing some hepatocelluar damage (i.e., elevated aspartate aminotransferse and alanine aminotransferase). Additionally, the elevated alkaline phosphatase indicates biliary obstruction. The lack of an increase in amylase and lipase makes obstruction at the ampulla less likely (such an obstruction would cause pancreatic inflammation).
A patient with choledocholithiasis should undergo extraction of stones from the common bile duct. This may be achieved endoscopically, via endoscopic retrograde cholangiopancreatography and sphincterotomy, or operatively.
11. The answer is c. In a patient with trauma, remember the principles of ATLS – ABCDE.
- A –Airway maintenance with cervical spine protection
- B –Breathing
- C –Circulation
- D –Disability
- E –Exposure
In this patient airway is a priority because the patient is unconscious and also has multiple facial fractures.
Cricothyroidotomy is indicated in patients who cannot be intubated or who have sustained significant maxillofacial trauma, such as this patient who has multiple maxillary and mandibular fractures. Currently, cricothyroidotomy and percutaneous transtracheal ventilation are preferred over tracheostomy in most traumas because they are relatively safe and simple. However, a disadvantage of a cricothyriodotomy is the inability to use a tube larger than 6 mm because of the limited aperture of the cricothyroid space. Once the initial crisis has been tided over, a formal tracheostomy should be carried out.
The patient is exhibiting classic signs of shock (hypotension, tachycardic, mental status changes, tachypnea, diaphoresis, and pallor) and circulation is one of the first things to evaluate in a trauma. However, an airway is always the primary concern, and in this young patient it is likely that he will maintain circulation until an airway is secured.
Face mask ventilation is not adequate in this patient given the oxygen saturation level and airway patency, and adequacy of ventilation should take precedence over other treatment.
Nasopharyngeal intubation and oropharyngeal intubation are con traindicated in patients who have sustained significant maxillofacial trauma or who have unstable facial fractures.
[ATLS guidelines – American College of Surgeons]
12. The answer is a. (Bailey 25th edition, Sabiston 19th edition) This patient has a typical presentation for Ogilvie's syndrome. Patients typically present with nausea, vomiting, constipation, abdominal distention, a tympanic abdomen, and positive bowel sounds, and with hypokalemia, hypoclacemia, and hypomagnesemia. Water soluble enemas fail to reveal mechanical bowel obstruction. Toxic megacolon 55presents with colonic dilation and fever, tachycardia, leukocytosis, and anemia. The actual etiology of Ogilvie's syndrome is unknown. Treatment includes nasogastric and rectal tube placement and neostigmine to promote decompression of the colon. Neostigmine (Catchpole regime) should only be used after ruling out mechanical obstruction. Serial abdominal x-rays help to monitor cecal size and determine the aggressiveness of therapy.
13. The answer is d. (Sabiston 19th edition, Devita 9th edition) This patient has Turcot syndrome, an autosomal dominant disease characterized by colorectal polyposis and central nervous system tumors, particularly gliomas. All familial polyposis syndromes, with exception of Peutz-Jeghers Syndrome, predispose to colorectal cancer.
Turcot syndrome has also been reported in association with both familial adenomatous polyposis (FAP) and hereditary nonpolyposis colorectal carcinoma, but FAP is the more classic association.
Gardner's syndrome is characterized by colorectal polyposis and osteomas or other bone and soft tissue tumors.
Hereditary nonpolyposis colorectal carcinoma is associated with dozens of colorectal polyps, and a majority of affected patients will develop colorectal cancer.
Tuberous sclerosis is an autosomal dominant condition characterized by mental retardation, seizures, tuberous central nervous system tumors, angiomyolipomas of the kidneys, leptomeningeal tumors, and skin lesions such as ash-leaf spots and shagreen patches.
14. The answer is b. (Bailey 25th edition) Right upper quadrant pain in an obese, middle-aged, multiparous woman with ultrasonographic findings consistent with gallstones is a classic sign and symptom of acute calculous cholecystitis. Acute calculous cholecystitis is an acute mechanical inflammation of the gallbladder commonly resulting from a gallbladder stone obstructing the gallbladder neck or cystic duct, chemical inflammation, and/or bacterial inflammation. Definitive treatment is cholecystectomy.
15. The answer is d. (Bailey 25th edition) Rupture of the urethra below the urogenital diaphragm (at the junction between the membranous and the bulbar) from a so-called “straddle injury” causes urine to flow into the scrotum and the perineal region.
Penile urethra rupture occurs following a crush injury. Urine will flow into the deep fascia of Buck within the penis.
Superior bladder wall rupture, also called dome rupture, is caused by forceful compression of a full bladder. This form of bladder rupture causes urine to flow into the peritoneal cavity.
Urethral rupture above the urogenital diaphragm (at the junction of the prostatic and membranous urethra) due to a fractured pelvis or improper catheter insertion causes urine to flow into the retropubic space. On examination, there is blood at the tip of the meatus and DRE reveals a “high-riding” prostate.
16. The answer is a. This patient presents with chronic diarrhea, intermittent facial flushing, and a murmur consistent with tricuspid stenosis, a triad of findings classic for carcinoid tumor. Carcinoid tumor in the GIT most commonly occurs in the distal part of ileum followed by the appendix. Carcinoid tumor secretes setetonin which causes vasoactive responses such as those mentioned. Electron microscopy reveals “salt and pepper” granlutation of cells, consistent with their neuroendoctrine origin. Elevated urinary 5-HIAA is diagnostic.
Carcinooid tumors can also be found in the rectum but not as frequently as the distal ileum and appendix. Rectal carcinoids have a propensity to metastatize early.
[Maingot's Abdominal Operations]
17. The answer is a. (Bailey 25th edition, Smith's Urology) The patient should undergo an intravenous pyelogram after kidney function tests for a suspected ureteral injury. Iatrogenic ureteral injuries are common after gynaecological and colo-rectal procedures. Intraoperatively, intravenous administration of methylene blue or indigocyanine green may facilitate identification of an injury. However, delay in diagnosis is common, and patients may present with flank pain, fevers, and signs of sepsis, ileus, or decreased urine output.
CT scan may demonstrate hydronephrosis or a fluid collection (urinoma). Initial diagnosis and management should include urinalysis, although hematuria may not always be present. Surgical management should be delayed if diagnosis is late (10 to 14 days), and operative strategy is dependent on the location of the injury. Diagnostic imaging such as a pyelogram or nuclear medicine scan may be helpful to identify the site of the injury.
18. The answer is c. (Bailey 25th edition) Bile and the fluids found in the duodenum, jejunum, and ileum all have an electrolyte content simi-lar to that of Ringer's lactate. Saliva, gastric juice, and right colon fluids have high K+ and low Na+ content. Pancreatic secretions are high in bicarbonate. It is important to consider these variations in electrolyte patterns when cal-culating replacement requirements following gastrointestinal losses.
19. The answer is c. [ATLS guidelines – American College of Surgeons] Most skull fractures do not require surgical treatment unless they are depressed or compound. A general rule is that all depressed skull fractures—defined as fractures in which the cranial vault is displaced inward—should be surgically elevated, especially if they are depressed more than 1 cm or if a fragment is causing neurological symptoms. Compound fractures, defined as fractures in which the bone and the overlying skin are broken, must be cleansed and debrided and the wound must be closed. The presence of rhinorrhea or otorrhea requires observation; although meningitis is a serious sequela, the role of prophylactic antibiotics is controversial. Otorrhea usually heals within a few days. Persistent cerebrospinal fluid from the nose or ear for more than 14 days requires surgical repair of the torn dura.
20. The answer is c (Bailey 25th edition, ATLS guidelines 8th edition) Burns involving the airways in a burns patient are a major cause of morbidity and mortality. The danger points which suggest inhalational injury in a burns patient are:
- Singed nasal air
- Burns involving the face
- Carbonaceous deposits in the sputum
- Burns in a closed room.
21. The answer is b. (Bailey 25th edition) The femoral canal contains the deep inguinal lymph nodes and is enclosed inside the femoral sheath with the femoral artery and vein. In a femoral hernia, this is the potential space into which abdominal contents herniate. A mnemonic for the contents of the femoral triangle is N(AVEL) (laterally to medially) for Nerve, Artery, Vein, Empty space, Lymphatics.
22. The answer is d. (ATLS guidelines 8th edition) This patient's clini-cal presentation suggests rhabdomyolysis. A history of trauma followed by an extended pe-riod of inactivity is a classic cause of rhabdomyolysis. Urine positive for blood by dip-stick but negative for RBCs by microscopic examination suggests the presence of myoglo-bin secondary to rhabdomyolysis. The wide-spread muscle cell damage that occurs in rhab-domyolysis leads to the release of intracellular components into the systemic circulation. Among these, elevations of potassium and structural proteins such as myoglobin can lead to serious problems such as acute renal failure (ARF). Myoglobin accumulation in the kidney can lead to myo-globinuria and ARF, as evidenced by a sharp rise in creatinine levels (out of proportion to increases in blood urea nitrogen).
23. The answer is c. (Bailey 25th edition) This woman is exhibiting signs of subacute thyroiditis, consistent with a low thyroid-stimulating hormone and high thyroxine. This commonly follows a viral upper respiratory infection, and pain from the thyroid can be referred to the throat. It is associated with a diffuse thyroid swelling and an initial phase of hyperthyroidism (as present in this case). This is due to the destruction of follicles. This phase of hyperthyroidism is followed by a prolonged phase of hypothyroidism, which gradually recovers spontaneously.
Riedel's thyroiditis (fibrosing thyroiditis) is a condition in which the thyroid is replaced by fibrous tissue. Patient presents with a diffuse enlargement of the thyroid, which is hard in consistency (and mimics anaplastic thyroid cancer). In addition the patient has features of hypothyroidism.
24. The answer is e. (Maingot's) Patients with pan-creatic cancer can present with weight loss, jaundice, abdominal pain, dark urine, acholic stools, and pruritus. On physical examination the gallbladder can be palpable (Couversier's law). Diagnosis is usually made with ultrasound with findings of dilated bile ducts or visible mass, or CT scan which demonstrates the pancreatic mass. The associated risk factors for pancreatic cancer include (smoking), chronic pancreatitis, a first-degree relative with pancreatic cancer and high-fat diet.
Chronic pancreatitis, not chronic gastritis, is a risk factor for pancreatic cancer.
25. The answer is e. (Washington Manual of Surgery) Diverticulosis accounts for 42-55% of lower gastrointestinal bleeding, followed by cancer/polyps accounting for 8-26%, and bleeding from angiodysplasia accounts for 3-12%.
26. The answer is d. (Devita 9th edition) Superior vena cava obstruction (SVC syndrome) is mostly due to malignancy (90% of cases) and in three out of four cases, results from invasion of the vena cava by bronchogenic carcinoma. Lymphomas are the second most common cause of the superior vena cava syndrome.
Fibrosing mediastinitis as a complication of histoplasmosis or ingestion of methysergide and may rarely lead to SVC syndrome. Rarely, a substemal thyroid or thoracic aortic aneurysm may be responsible for the obstruction. Although constrictive pericarditis may decrease venous return to the heart, it does not produce obstruction of the superior vena cava.
Whatever the cause of the superior vena cava syndrome, the resultant increased venous pressure produces edema of the upper body, cyanosis, dilated subcutaneous collateral vessels in the chest, and headache. Cervical lymphadenopathy may also be present as a result of either stasis or metastatic involvement.
Initial management of superior vena cava syndrome consists of diuresis, and for malignancies, the treat-ment consists of radiation and chemotherapy, if applicable. Occasionally, surgical intervention or thrombolysis may be indicated for severe life threatening complications.
27. The answer is a. (Bailey 25th edition; Sabiston 19th edition) The finding of prolonged high-amplitude contractions in the body of the esophagus in a highly symptomatic patient is diagnostic of diffuse esophageal spasm (DES). Patient presents with complaints of chest pain, which mimics angina or MI. The cause of the hypermotility disorder known as DES is unknown, but its symptoms can be disabling. The recommended treatment for this relatively rare disorder is a long myotomy guided by the manometric evidence.
28. The answer is a.
Classification | Criteria | Risk (%) |
|---|---|---|
Clean | Elective, not emergency, nontraumatic, primarily closed; no acute inflammation; no breka in technique; respiratory, gastrointestinal, biliary and genitourinary tracts not entered | < 2 |
Clean-contaminated | Urgent or emergency case that is otherwise clean; elective opening of respiratory, gastrointestinal, biliary or genitourinary tract with minimal spillage (e.g., appendectomy) not encountering infected urine or bile; minor technique break | < 10 |
Contaminated | Nonpurulent inflammation; gross spillage from gastrointestinal tract; entry into biliary or genitourinary tract in the presence of infected bile or urine; major break in technique; penetrating trauma < 4 hours old; chronic open wounds to be grafted or covered | Approx. 20 |
Dirty | Purulent inflammation(e.g., abscess); preoperative perforation of respiratory, gastrointestinal, biliary or genitourinary tract; penetratinbg trauma > 4 hours old | Approx. 40 |
Out of these classes, prophylactic antibiotics are not indicated in clean cases but are indicated in all other classes. Prophylactic antibiotics should be injected at the time of induction of anaesthesia.
29. The answer is e. (Moh's Micrographic Surgery – Springer) There is no difference in cure rate between Mohs surgery and wide local excision of a basal cell carcinoma. Mohs surgery describes a technique for resecting either basal or squamous cell carcinomas on the face or near the nose or eye in order to achieve the optimal cosmetic result. Resection of the tumor is performed in small increments with immediate frozen section analysis in order to ensure negative margins. The disadvantage of the Mohs technique is the longer time required.
30. The answer is d. (Bailey 25th edition) Staged excision of deep partial-thickness or full-thickness burns is done between three and seven days after the injury. There are several proven advantages to 61early excision, including decreased hospital stay and lower cost. This is especially true of burns encompassing within 20% of the total body surface area. In conjunction with early excision, topical antimicrobials such as silver sulfadiazine are extremely important in delaying colonization of the newly excised or fresh burn wounds. The body surface area burnt in this patient is 45%.
Meticulous attention to deep circumferential burns is racial in the management of burn patients. Progressive tissue edema may lead to progressive vascular and neurologic compromise. Because the blood supply is the initial system affected, frequent assessment of flow is vital, with longitudinal escharotomy performed at the first sign of vascular compromise. A low threshold should be maintained in performing an escharotomy in the setting of severely burned limbs.
31. The answer is b. (Bailey 25th edition) Patients who undergo uncomplicated abdominal surgeries can be given enteral feeds once bowel sounds appear. There is no need to wait for the patient to pass feces. Parenteral nutrition should only be considered if a patient cannot be given enteral feeds for more than 5 days.
The advantages of enteral feeding over parenteral feeding are:
- It is physiological
- Cheap
- No special preparation required; no sterilisation required
- It prevents villous atrophy, which can lead to translocation of bacteria from the gut
- Maintains the entero-hepatic circulation and prevents biliary stasis, which occurs with parenteral nutrition.
32. Answer is c. (Maingot's Abdominal Operations) Osteitis cystica fibrosa is is a finding in patients with primary hyperparathyroidism and represents sub-periosteal resorption, characteristically on the radial aspect of the middle phalanx. This is not a reported complication after partial gastrectomy. Patients who have undergone partial gastrectomy may, however, have osteoporosis secondary to impaired calcium absorption due to the Billroth II reconstruction (since calcium is normally absorbed in the proximal intestine—duodenum and jejunum). Fatty acids may also be malabsorbed due in inadequate mixing of bile salts and lipase with ingested fat, and therefore steatorrhea may result. Either megaloblastic anemia due to vitamin B12 deficiency (due to lack of intrinsic factor, which is necessary for B12 absorption and is normally 62produced by the parietal cells of the stomach) or microcytic anemia due to iron deficiency (due to decreased iron intake and impaired absorption in the duodenum) can result after partial gastrectomy.
33. The answer is a. (Bailey 25th edition) The thyroid scan shows a single focus of increased uptake, often referred to as a hot nodule; the remaining thyroid galnd has not taken up radioactive iodine. Hyperfunctioning adenomas become independent of thyroid stimulating hormone (TSH) control and secrete thyroid hormone autonomously, which results in clinical hyperthyroidism. The elevated thyroid hormone levels ultimately diminish TSH levels severely and thus depress function of the remaining normal thyroid gland. Carcinomas usually display diminished uptake (cold nodules). Grave's disease would probably manifest as a diffusely hyperactive gland without nodularity. Multinodular goiter would display many nodules with varying activity.
34. The answer is c (Malignant Melanoma) (NCCN guidelines, Devita 9th edition) – TNM staging for malignant melanoma
Primary tumor (T) | |
TX | Primary tumor cannot be assessed (ie, curettaged or severely regressed melanoma) |
T0 | No evidence of primary tumor |
Tis | Melanoma in situ |
T1 | Melanoma > 1.0 mm in thickness·
|
T2 | Melanomas 1.01-2.0 mm in thickness·
|
T3 | Melanomas 2.01-4.0 mm in thickness·
|
T4 | Melanomas > 4.0 mm in thickness·
|
Regional lymph nodes (N) | |
NX | Patients in whom the regional nodes cannot be assessed (ie, previously removed for another reason) |
N0 | No regional metastases detected |
N1-3 | Regional metastases based upon number of metastatic nodes and presence or absence of intralymphatic metastases (in transit or satellite metastases) |
N1 | 1 lymph node·
|
N2 | 2 or 3 lymph nodes·
|
N3 | > 4 metastatic lymph nodes, or matted lymph nodes, or in-transit met(s)/satellite(s) with metastatic lymph node(s) |
Distant metastasis (M) | |
M0 | No detectable evidence of distant metastases |
M1a | Metastases to skin, subcutaneous, or distant lymph nodes, normal serum lactate dehydrogenase (LDH) level |
M1b | Lung metastases, normal LDH level |
M1c | Metastases to all other visceral sites or distant metastases to any site combined with an elevated serum LDH level |
Other staging systems used for Malignant Melanoma
- Clarke's
- Breslow's
35. The answer is d. (Bailey 25th edition) Epidural catheters are one of the most effective methods for ensuring pain control in hospitalized patients with multiple rib fractures. Patients with multiple rib fractures should be admitted in the hospital and hemopneumothorax should be ruled out. Those who are elderly and have underlying respiratory problems are at a higher risk of developing pulmonary complications.
Strapping and surgical fixation of fractured ribs is no longer indicated. Strapping can further compound the problem of inadequate ventilation.
Oral analgesics are sufficient for patients with a single rib fracture and no underlying pulmonary complications.
Tube thoracostomy is indicated in the presence of hemo or pneumothorax.
36. The answer is c. (Bailey 25th edition). Tension pneumothorax is a life threatening problem requiring immediate treatment. A lung wound that behaves as a ball or flap vale allows escaped air to build up pressure in the intrapleural space. This causes collapse of the ipsilateral lung and shifting of the mediastinum and trachea to the contralateral side, in addition to compression of the vena cava and contralateral lung. Rapid decompression should be achieved to prevent cardio-respiratory compromise. This is achieved by placing a wide bore needle in the 2nd intercostals space in the mid clavicular line followed by a formal chest tube insertion. Tension pneumothorax produces characteristic x ray findings of ipsilateral lung collapse, mediastinal and tracheal shift, and compression of the contralateral lung.
37. The answer is d. (Bailey 25th edition) Indications for surgery in patients with BPH include
- urinary retention
- BPH refractory to medical therapy
- Hydronephrosis or renal insufficiency secondary to outflow obstruction,
- Bladder stones or diveticulae.
- Recurrent urinary tract infections are also an indication for surgical intervention.
Treatment should be directed at alleviating symptoms; initial management consists of alpha blockade. Outflow obstruction is characterized by high bladder pressures and low flow rates. Low bladder pressures and low flow rates are present when the bladder muscles are poorly contractile due to overdistention and persistent obstruction. Although persistent outflow obstruction can ultimately lead to renal failure, BPH does not always progress to this stage. Surgical treatment for BPH consists of transurethral resection of the prostate (TURP). Because of the use of large volumes of hypotonic fluid during TURP, patients should be monitored postoperatively for hyponatremia due to hemodilution secondary to absorption of the irrigation solution.
38. The answer is a. [Smith's Urology] If time and the patient's condition permit, primary ureteral reconstruction should be carried out. In the middle third of the ureter, this will usually consist of ureteroureterostomy (primary anastamosis) using absorbable sutures 65over a stent. If the injury involves the upper third, ureteropyeloplasty may be necessary. In the lower third, ureteral implantation into the bladder using a tunneling technique is preferred. If time does not permit definitive repair, suction drainage adjacent to the injured segment alone is inadequate; placement of a catheter into the proximal ureter is an acceptable alternative that would allow reconstruction to be performed later. The creation of a watertight seal is difficult and nephrectomy may be required if the injury occurs during a procedure in which a vascular prosthesis is being implanted (e.g., an aortic reconstructive procedure) and contamination of the foreign body by urine must be avoided.
39. The answer is b. (ATLS guidelines 8th edition) The patient should undergo medial and lateral escharotomies of his left lower extremity. Based on his clinical history of a circumferential, full-thickness burn and on his symptoms of numbness and pain, the patient has compartment syndrome. The presence of pedal pulses does not preclude the diagnosis of compartment syndrome. If the diagnosis is in question, compartment pressures can be measured, and a pressure of greater than 30 to 40 mmHg is diagnostic, compartment syndromes secondary to burns are a result of increased pressure secondary to tissue edema and lack of elasticity of the burnt skin eschar, causing compression of the blood vessels.
40. The answer is d. (Bailey 25th edition) The patient has a metabolic alkalosis secondary to gastric losses of HCl, with compensatory hypovention as reflected by the elevated arterial pH and Pco2 and supported by the absence of clinical lung disease. The PCO2 would be normal if the metabolic alkalosis was uncompensated. A respiratory acidosis with metabolic
compensation would characterized by decreased pH, increased Pco2 levels, and increased bicarbonate levels. Mixed acid-base abnormalities should be suspected when the pH is normal but the Pco2 and bicarbonate levels are abnormal or if the compensatory responses appear to be excessive or inadequate. The combination of respiratory acidosis and respiratory alkalosis is impossible.
41. The answer is b. (Sabiston 19th edition) Pancoast tumors are peripheral bronchogenic carcinomas that produce symptoms by involvement of extrapulmonary structures adjacent to the cupula. These structures include the nerve roots of C8 and T1, as well as the 66sympathetic trunk. Interruption of the cervical sympathetic trunk leads to miosis, ptosis, and anhidro-sis, the triad of signs that constitutes Horner's syndrome, involvement of the nerve roots causes pain along the corresponding dermatomes. The peripheral location of the neoplasm makes pulmonary signs, such as atelectasis, cough, and hemoptysis, unlikely.
42. The answer is c. (Sabiston 19th edition) Bronchial carcinoid tumors commonly produce the carcinoid syndrome. They are slow-growing, infrequently metastatic tumors that histologically resemble carcinoid lumors of the small intestine. Over 80% arise in the major proximal bronchi, and their intraluminal growth is responsible for the frequent presentation of bronchial obstruction. The only therapy for this lesion is oper-ative resection, because neither the primary tumor nor the infrequent lymph node metastasis is radiosensitive. The low malignant potential for this lesion is reflected by a long-term survival rate that approaches 90%.
43. The answer is a. (Sabiston 19th edition) The two most important points in this question are that the patient is a nonsmoker and that the lesion is located peripherally (subpleural mass). Lung cancers are typically divided into two types: small-cell lung cancers and non-small-cell lung cancer consisting of adenocarcinoma, squamous cell carcinomas, and other histologic types. These two types are treated with different chemotherapy regimens. The most common lung cancer subtype in nonsmokers and women in general is adenocarcinoma. Adenocarcinomas are peripherally located and are more amenable to (possibly curative) surgical removal than other more centrally located primary lung tumors.
44. The answer is a. Colonoscopy is the method of choice in this individual because the lesion is most likely right sided, as sug-gested by a negative sigmoidoscopy 6 months ago. With colonoscopy, the entire large bowel can be visualized, and it also allows the biopsy of lesions or removal of polyps found on examination.
A CT scan of the abdomenis not the diagnostic method of choice in diagnosing right-sided colon cancers, although CT colonoscopy (high-resolution CT also known as virtual colonoscopy) is currently being explored. This is because current resolution may miss some polyps and other lesions. Also, colonoscopy allows for biopsy of potential lesions.
Double-contrast barium enema can be used to make a radiographic diagnosis of colonic cancer if it is not possible to perform a colonoscopy (e.g. tortuosity of the colon). Colonoscopy is the preferred method.
Sigmoidoscopy would not be helpful here because the patient had a negative sigmoidoscopy 6 months ago, suggesting that the lesion is not on the left side of the colon. To visualize the right side of the colon, a colonoscopy should be performed.
45. The answer is a. NG tube. ACS guidelines (Souba et al)
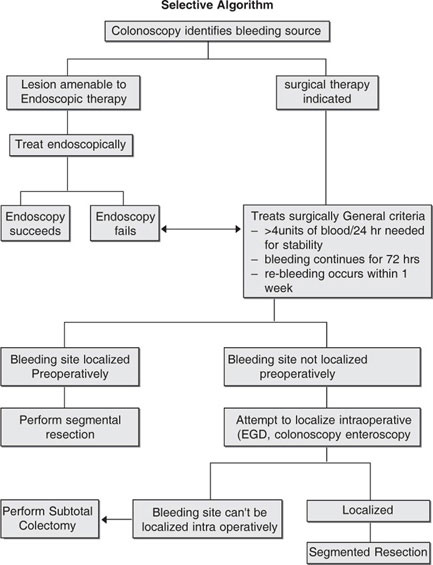
Approach to lower gastrointestinal Bleeding
Patient present with acute lower bleeding
- Resuscitate as necessary
- Simultaneously, take history nature and duration of bleeding, associated symptoms, past medical history, co-morbid condition and perform physical exam (postural vital signs complete abdominal examination)
- Order CBC, electrolytes and coagulation profile.
- Place NG table for gastric lavage
46. The answer is b. (Sabiston 19th edition) In a patient with variceal bleeding due to PHT the first step is to resuscitate the patient with fluid resuscitation and blood replacement. Resuscitation in such scenario is balanced resuscitation to keep the blood pressure at lower side of normal to maintain adequate organ perfusion. Also massive replacement of blood is avoided it should be judicial and one should start prophylactic antibiotic as infection leads to further bleeding. The algorithm in variceal bleeding is as follows
47. The answer is d. (Bailey 25th edition) Gastroesophageal reflux is a common disease that accounts for approximately 75% of esophageal pathology. The most simplistic approach is to define the disease by its symptoms. The history is highly suggestive of gastro-esophageal reflux disease (GERD), which presents with substernal chest pain worse after meals or when recumbent. Patients commonly also complain of an acid taste in the mouth from the reflux. Mild to moderate GERD is treated initially with lifestyle modifications including weight loss, and antacids. Pharmacologic treatment follows in patients with severe or refractory disease, with histamine-receptor antagonists (ranitidine or cimetidine) or proton pump inhibitors (omeprazole or lansoprazole).
48. The answer is a. (Bailey 25th edition) This patient present with acute cholecystitis. This diagnosis is supported by right upper quadrant abdominal pain that is accompanied by nausea, vomiting, fever, guarding, and a positive Murphy's sign. Although obesity increases one's risk of developing galladder disease, this risk is even greater following rapid weight loss (such as after gastric bypass surgery). A presentation suspicious for acute cholecystitis should be worked up initially with an ultrasound as this is an inexpensive test that can be done at the bedside rapidly. Although CT scan of the abdomen may show an edematous gallbladder wall with fluid surrounding the gallbladder, this test is much more expensive than an ultrasound and cannot be performed at the bedside, and therefore it is not the first test that you would order when working-up a patient with a presentation suspicious for acute cholecystitis.
49. The answer is e. (Bailey 25th edition) Impetigo is a bacterial skin infection commonly caused by either Staphylococcus aureus or group A Streptococcus. It characteristically results in crusting skin lesions that are often non painful and non pruritic. The progression of the irritation is generally initiated with a tiny vesicle or pustule that rapidly develops into a honey-colored crusted plaque. For patients with a limited number of lesions, treatment with topical antibiotic (mupirocin) is preferred; for more widespread, severe cases, oral antibiotics may be used(erythromycin, cephalexin, or dicloxacillin).
Acyclovir is not indicated for the treatment of bacterial skin infections. Acyclovir is commonly employed in the treatment of herpes simplex lesions, varicella zoster virus (chickenpox), or herpes zoster. Topical 71steroids, such as hydrocortisone, are not routinely indicated for the treatment of bacterial skin infections. Topical steroids are more commonly employed for conditions such as contact dermatitis, seborrhea dermatitis, or atopic dermatitis (eczema).
Intravenous vancomycin is not indicated for the treatment of impetigo. For severe, widespread impetigo, a course of oral antibiotics is generally sufficient.. Tretinoin cream is not indicated for the treatment of bacterial skin infections. Tretinoin cream is typically used in the treatment of acne vulgaris.
50. The answer is d. (Sabiston 19th edition) A penetrating wound to the chest will produce either a pneumothorax, a hemothorax, or both- The absence of breach sounds confirms that one of those has occurred, and the hyperresonance percussion indicates that air is present. The patient's good vital signs indicate that there is time to do the proper diagnostic study (chest X-ray). The appropriate treatment for a pneumothorax is placement of a chest tube.
Infusion of 2 L Ringer's lactate would have been appropriate if the findings had suggested hemothorax (as evidenced by dullness to percussion), and he had been bleeding (as evidenced by low blood pressure and a fast pulse). A patient who is awake and alert, and who is speaking in a normal tone of voice, has an airway and can maintain it.
Immediate insertion of a needle into the right pleural space would be appropriate management for a tension pneumothorax. If the patient had a tension pneumothorax he would have been in shock and severe respiratory distress, and the mediastinum would have been shifted (evidenced by tracheal deviation).
51. The answer is d. (Bailey 25th edition) Chronic nonbacterial prostatitis is characterized by persistent irritative voiding symptoms, such as dysuria and perineal discomfort, and leukocytes (especially foamy macrophages) in expressed prostatic secretion. No bacteria, however, are isolated from cultures of urine or prostatic secretions. This condition is believed to be of a noninfectious nature and possibly autoimmune-mediated. Treatment is based on symptomatic relief with Sitz bath and anti-inflarnmatory agents. However, some authors recommend a trial with erythromycin.
52. The answer is c. (Bailey 25th edition) Ultrasonography is the most and least expensive method to discriminate between testicular and extra testicular masses. However, a physician should remember 72first use a simple transillumination test for such a differential diagnosis. Fluid collections within the vaginal sac transilluminate, whereas testicular masses do not. CT scanning is used to determine the spread of testicular tumors within the abdominal and thoracic cavity, but is of no use in the initial diagnosis of scrotal masses. Serum levels of hCG, alpha-fetoprotein, and LDH - are important adjunct parameters in the diagnosis and subsequent management of testicular neoplasms. LDH may be elevated in seminomas and non seminomas, alpha-fetoprotein is elevated in non seminomas (especially yolk sac tumors), and hCG is elevated in nonseminomas (especially choriocarcinomas). Inguinal orchiectomy is, performed when ultrasonography has established that scrotal enlargement is caused by an in testicular tumor. This allows most accurate pathologic diagnosis and appropriate management.
53. The answer is d. (Bailey 25th edition) The rule for abdominal gunshot wounds is simple: an exploratory laparotomy should be done in every case, before there are obvious signs of either bleeding or peritonitis hence a most important step.. Clinical observation alone is not wise, since the risk of complications will increase the longer one waits. Emergency ultrasound followed by CT scan is the right approach to plan accordingly before exploratory laparotomy.
54. The answer is c. (Bailey 25th edition) In the setting of massive blood loss and multiple transfusions, the development of coagulopathy is almost predictable. Packed red cells contain virtually no viable platelets and only a very small concentration of clotting factors. Prophylactic administration of clotting factors has not proven to be advantageous, but once the coagulopathy occurs, a shotgun approach to provide fresh frozen plasma and platelet packs is indicated. Ignoring the coagulopaihy and continuing to operate and transfuse would be doomed to failure. Surgeons can ligate or cauterize big vessels but cannot do the same for capillaries. Proper clothing is indispensable in all surgical operations. Although it would be more elegant to determine exactly what is missing, under these circumstances there is no time to do the detailed studies If hypothermia and acidosis had also developed, a more drastic approach would have been necessary: stop the operation and close the abdomen temporarily.
55. The answer is c. (Bailey 25th edition) Severe blunt trauma to the chest can produce obvious injuries, such as broken ribs, but it can 73also lead to pathology that may not show up until later, such as pulmonary contusion or myocardial contusion. The former produces the classic “white-out” of the lung (contused lung is exquisitely sensitive' to fluid overload, and the fluid leaks easily) along with respiratory distress. Myocardial contusion shows up like an infraction, both clinically (arrhythmias) and on ECG. You would expect it in association with sternal fractures rather than with rib fractures.
Tension pneumothorax produces shock and high central venous pressure (CVP), along with respiratory distress, and air is seen in the x-ray. The ultimate hidden injury in blunt, chest trauma is traumatic rupture of the aorta. X-ray films would show widening of the mediastinum, and the eventual clinical manifestation would be exsanguinating hemorrhage.
56. The answer is d. (Bailey 25th edition) Prostatic hyperplasia results in partial obstruction of the proximal urethra, causing hesitancy and decreased force of stream. With increasing degrees of prostatic enlargement, the volume of urine remaining in the bladder after voiding increase progressively until complete urinary retention manifests with occasional overflow incontinence. Urinary retention leads to dilatation of the ureters and renal pelvis.
Age-associated detrusor overactivity is the most common cause of urinary incontinence in the elderly. It manifests with an uncontrollable urge to urinate not triggered by Stress maneuvers. It seems to be related to a deficiency in the descending pathways that inhibit the voiding reflex triggered by bladder distension. This condition does not lead to urinary retention. Urinary incontinence associated with Alzheimer disease and normal pressure hydrocephalus is similar to detrusor over actvity and results from failure to inhibit the contractions of the vesical detrusor muscle.
57. The answer is a. (Bailey 25th edition) The During vascular procedures, the use of cross clamping and tourniquets produces localized or regional ischemia. The consequences of ischemia include the accumulation of metabolic waste products and acid load, which are freely available the systemic circulation once they gain access to it. The primary consequence of this is profound and dramatic systemic hypotension that can be prolonged for hours after a procedure. Such a phenomenon has obvious con sequences for management of patients such as this man with coexisting cardiac disease.
A drop in systemic blood pressure from severe vasodilation will lead to decreased preload and thus a decrease in stroke volume and cardiac output restoration of circulation to the previously clamped limb opens an entirely new venous reservoir, thus dramatically reducing venous return in addition, the massive systemic vasodilatation would further decrease venous return. The result of these two events is a dramatic and often profound drop in systemc blood pressure.
58. The answer is b. (Bailey 25th edition) This patient has an intracranial bleed, signs of increased intracranial pressure (ICP), and evidence on a CT scan of impending herniation. This patient requires rapid lowering of his ICP. The most rapid method available is hyperventilation to lower Pa C02 which leads to decreased cerebral blood low and ICP. Administration of IV mannitol is also an appropriate therapy in this case. However, manitol has an onset of action approximately 90 minutes after dosing, which makes hyperventilation the mainstay of acute therapy. Induction of a barbiturate coma is used as a last resort to dramatically lower ICP. In cases of severe emergency, patients are mechanically ventilated awl placed in a barbiturate coma So that maximal ICP can g of ICP can be attained.
Initiating immediate surgical decompression (maybe appropriate, but not until hyperventilation has begun. Like mannitol, surgical decompression (even as emergent surgery) is not immediate; therefore, therapy needs to be instituted during that interval.
59. The answer is a. (Bailey 25th edition) This patient most likely has a pulmonary embolism. Pulmonary embolism occurs following general surgery In 1% to 2% of patients older incidence is higher (5% to 10%) following orthopedic surgery of the hip or knee. Venous stasis due to immobilization is probably a major reason for venous thrombosis with surgery. However, other factors, such as increased blood fibrinolytic activity and vessel damage may be involved as well. an increased alvcolar arterial oxygen difference (A-a gradient) seen on arterial blood gas on room air supports the diagnosis, along with sinus tachycardia cn ECG and a normal chest X-ray.
Ventilation perfusion scan are important in confirming the diagnosis of pulmonary embolism, but an arterial blood gas should be performed first. Supplemental oxygen should be given after an arterial blood gas is obtained. IV heparin is the treatment of choice for a pulmonary embolus but should not be administered until there are some objective data that support the diagnosis.
60. The answer is a. (Bailey 25th edition) All penetrating injuries require tetanus prophyxis, an often overlooked detail when dealing with other more impressive problems in this case, the key to the correct answer lies in the fact that the other options are not indicated. In gunshot wounds of the extremities, the main concern is the possibility of major vascular injuries. Such injurires can be evaluated with Doppler studies, arteriograms or surgical exploration but none of those are needed here. A rudimentary knowledge of anatomy allows the physician to skip all those expensive procedures: the femoral artery (With the femoral vein adjacent to it) is located anteromedial in the upper thigh and eventually becomes centered on the axis of the extremity when it becomes the popliteal. It is never located on the lateral side of the thigh. where the bullet tract is located in this vignette.
61. The answer is d. (Bailey 25th edition) Circumferential burns of the extremities pose a distinct hazard to peripheral circulation because the edema fluid resulting from the burn cannot expand under the unyielding envelope of the burn eschar. compulsive monitoring of pulses and capillary filling is required; escharotomy also may be required.
Although flame burns can cause smoke inhalation and the so called respiratory burn, they do so only when the victim is trapped in an enclosed space: a burning car, a plane, a building in those situations you would monitor blood gases and carboxyhemoglobin levels.
Body weight does not change much with the massive internal fluid internal fluid shifts of a major burn. We guide our fluid therapy by urinary output and central venous pressure, not by monitoring body weight.
62. The answer is d. (Campbell) Retrograde ejaculation occurs in up to 90% of patients undergoing transurethral resection of the prostate (TURP)). The fragmented appearance of the specimen is due to the type of surgical technique used to remove the prostate. The periurethral prostatic tissue is excised through the. urethra in small-chips. Retrograde ejaculation leads to small volumes of ejaculate (<1.5 ml).
Bladder neck contracture incontinence and urethral strictures occur in less than 3% of patients undergoing TURP.
63. The answer is d. (Bailey 25th edition) Subphrenic abscess is a common complication of splenectomy and is implied by the patient's 76elevated temperature and elevated WBC, pleuritic pain (which is the probable cause of his rapid and shallow respirations), and left upper quadrant tenderness. A subphrenic abscess would irrigate the phrenic-nerve (nerve root C3-C5), causing referred pain toward dermatome of the nerve root, which includes' the left shoulder.
Left clavicular fractures appear eryhematous at the site of fracture and exhibit crepitus on palpation. The arm is usually held close to the body, and the ipsilat eral shoulder appears lower than the opposite side. One would expect rales or rhonchi instead of clear lungs and equal breath sounds in a patient with left lower lobe pneumonia.
Post splenectomy sepsis would not produce such localized symptoms.
64. The answer is d. (Bailey 25th edition) The woman was stabbed in the heart, leading to cardiac tapenade (Blood collecting in the pericardial sac). This causes impairment in heart function, leading to hypotension, distension of neck veins. due to pump failure, and muffled heart sounds due to the collection of blood. The immediate concern is removing the blood from the pericardial sac by performing pericardiocentesis All the other tests would lead to unnecessary delays in diagnosis and would result in death.
Echocardiogram could aid in the diagnosis of pericardial effusion but would take too long to administer in such an emergent situation.
A chest x-ray film would show pericardia effusion, but there already are enough data to support the diagnosis, so x-ray would cause unnecessary delay in therapy. Chest tube placement is used for pneumothorax and pleural effusions but would not be effective in the present scenario.
65. The answer is c. (Sabiston 19th edition) In gunshot wounds to the neck, the main concern is the possibility of significant vascular injuries. The area is too high to involve the aerodigestive tract, and it is also rather difficult to explore surgically. Arteriogram offers the best way to assess the extent of the injuries, and also provides a way for remobilization of major arteries that might be bleeding significantly.
Clinical observation is the second best answer, but it would delay recognition of significant vascular injuries that the arteriogram might demonstrate. Clinical observation is often all we do in asymptomatic stab wounds, where serious damage is less likely to occur.
Barium studies are essential when one suspects esophageal injury that is not demonstrated by gasirografin swallow. As pointed out above, however, that area of injury here is well above where the esophagus begins. Surgical exploratory might be unavoidable in hemodynamically unstable patients whose vascular injuries cannot be controlled by arteriographic embolizalition Surgery can be performed in this area if needed, but for technical reasons it is not our first choice of management.
66. The answer is c. (Bailey 25th edition) There are a host of important factors in the assessment of preoperative risk for patients undergoing non cardiac surgical procedures criteria have been published that aid in this stratification. One needs a very basic understanding or important preoperative risk factors that portray a very poor surgical outcome. any evidence of recent exacerbation of a patients underlying coronary disease (angina, worsened or poor baseline exercise tolerance recent infarction are major red flags that should make the physician call into question the need for a non-emergent procedure. Of these the one with the highest incidence of perioperative death or cardiac event is a recent myocardial infarction.
Poor exercise tolerance certainly suggests underlying coronary disease in this patient; but that diagnosis is already known. The critical issue is assessing his risk of an event given his underlying condition.
Premature ventricular contractions (PVCs) on ECG are common findings in patients with coronary disease. ECG indications of poor risk mostly reflect an exacerbation of underlying heart disease heart disease (ST segment depressions, new bundle branch blocks. PVCs.
However, are common even in healthy patients, and numerous clinical trials have demonstrated that they are quite benign. Suppressing them with medications is associated with increased mortality. Unless tachtcardia sustained runs (ventricular tachycardia), they are not a predictor of adverse events.
67. The answer is c. (Bailey 25th edition) Fever on first postoperative day is almost invariably from atelectasis, the treatment of which requires active participation and cooperation from the patient. If atelectasis does not resolve, it leads lo he development of pneumonia, which can be identified in chest x-ray films and confirmed with sputum cultures. AT that time the process is no longer purely mechanical but is also infectious, thus requiring antibiotics. Deep venous thrombosis) occurs 78about 5-7 days after surgery and is a ‘hidden source of fever, i.e. nothing else seems be wrong. This patient is clearly a candidate for thrombosis (he lies in bed doing nothing all day) but right now his problem is probably in the lung. The urine is a good possibility “when the fever starts on day 3, but the persistence of fever since day 1 points to the lung. Three days is too soon for a wound infection to be the cause of the fever. Five to seven days is a more likely time frame.
68. The answer is d. (ATLS guidelines 8th edition) This patient experienced a severe de-acceleration injury. He is hypotensive, tachycardic, and minimally responsive. He is in hemorrhagic shock. The chest X-ray reveals a widening mediastinum suggesting rupture of the thoracic aorta, which is a common catastrophic injury in deceleration accidents. This patient is in grave danger. The treatment is immediate surgical repair of the injury with fluid and blood resuscitation.
Cardiac tamponade is associated with hypotension and tachycardia. However, pulsus para-doxus (systolic blood pressure drops 10 mm Hg on respiration) and distant heart sounds might be discovered on physical examination, and his central venous pressure would be high. Chest x-ray films would show an enlarged cardiac silhouette. The ECG would exhibit low lead voltage and variable amplitude. However, pericardtocentesis is both the diagnostic and therapeutic procedure of choice.
69. The answer is c. (Bailey 25th edition) This man With a central lesion, would require a pneumonectomy rather than a lobectomy. After resectional pulmonary surgery is done, however, a patient must be left with a least 800 ml in the FEV to live a decent life. Anything less than that would make him a pulmonary cripple, or outright kill him. Because of his COPD, this patient is already severely limited, with a total FEV of 1100 ml. Were the bad lung to be removed, he would be left with only 40% of 1100 ml 440 ml The only option left is radiation and chemotherapy.
CT scan of the upper abdomen to rule out liver metastasis and mediastinoscopy to biopsy carinal nodes are necessary steps to establish curability. There is no point in doing a pneumonectomy if there are liver or carinal node metastases.
70. The answer is b. (Bailey 25th edition) Squamous cell carcinoms of the penis, It is virtually unknown in nations that practice early (i.e. in infancy) circumcision. It presents as a fungating or ulcerated mass on the glans penis or in the sulcus between the prepuce and the glans. Carcinogenic agents forming in the smegma are suspected to play a pathogenic role which may be enhanced by lack of circumcision. Other risk factors include lesions (condyloma acuminatum) due to human papillomavirus (HPV) types 16 and 18. Genomic material from these HPV types has been demonstrated in numerous cases. No association has been observed between penile cancer or its precursors and other types 6 or 11. Peyronie disease, which is a form of fibro matosis affecting the penis, results in induration nodularity, and deformities, it causes severe functional deficeits but is not associated with increased risk of cancer. This condition is akin to other forms of fibromatosis such as Deputytren cancer. The primary stage of syphilis manifests with a painless, sharply demarcated ulcer (chancre) often located in the glans. there is no association between syphilis and penile cancer.
71. The answer is b. (Bailey 25th edition) A plain abdominal X-ray film is most likely to detect a stone in this patient, who manifests the typical symptomatology of renal colic, most commonly due to a urinary stone impacted in the ureter. Usually, gross or microscopic hematuria is present Absence of fever is an important negative sign excluding-coexistence of-urinary tract infection. Most urinary stones consist of calcium phosphate or oxalate and thus contain enough calcium to be visible on plain x-ray films. However, some urinary calculi are radiolucent (especially uric and cystine stones), whereas others are so small as to be undetectable on plain x-ray films. Intravenous pyelography IVP) is rarely necessary in patients with the typical presentation of renal colic. However, IVP becomes necessary when the diagnosis is uncertain. Frequently, this investigation will demonstrate dilatation of the ureter proximal to the site of stone blockage.
Renal ultrasound examination is useful when the stone is suspected to be located at the ureterovesical junction. The bladder should be full to allow ultrasonography.
Serum calcium, phosphorus electrolytes, and uric acid should be evaluated in patients experiencing a first urinary tract stone, but serum chemistry studies are not necessary as initial diagnostic investigations.
72. The answer is a. (Bailey 25th edition) In uncomplicated renal colic due to a small stone impacted in the ureter, conservative management is usually the only treatment needed, as most stones will pass spontaneously. Naturally, pain medication should be provided. Conservative management is recommended for 6 weeks after presentation, but intractable pain, fever, or persistent vomiting may warrant more aggressive treatments.
Aggressive diuretic treatment or forced diuresis by IV fluids will not hasten passage of stones but will probably increase colicky pain. Extracorporeal shock wave lithotripsy (ESWL is performed by directing an external source of sound waves toward the stone. The energy beam will gradually disintegrate the calculus while producing no tissue damage. This procedure is particularly effective on stones impacted in the distal ureter that have failed to pass spontaneously with conservative management. Ureteroscopic stone extraction should be used if spontaneous stone passage has failed during the first weeks following presentation and ESWL is not feasible. This treatment is most appropriate for distal ureteral stones. An endoscope is inserted through the urethra and into the ureter. Under direct vision, the stone can be fragmented and then extracted or, if small enough, extracted with a basket. Percutaneous lithotomy is used for large renal stones located within the pelvicaliceal system.
73. The answer is c. (Bailey 25th edition) Patients with a recent history of kidney transplant are at an increased risk of bacterial infections. Septicemia and peritonitis in these patients is often caused by Pseudomonas aeruginosa, which is mostly hospital acquired. Patients with cystic fibrosis and patients with HIV are also at an increased risk of infection with this organism. Patients who have received liver transplants, not kidney transplants, are at an increased risk for infection with Enterococci.
Patients with HIV and low CD4+ counts, as well as infants 2-8 months old, have the most increased risk for infection with Pneumocystis carinii. Rather than peritonitis and septicemia, P. carnii usually causes pneumonia with characteristically low oxygen saturation.. Staphylococcus aureus is a common, pathogen, but not one that would carry an increased risk for this patient as opposed to other immunosuppressed patients.
74. The answer is b. (Bailey 25th edition) Cystic fibrosis often presents primarily with gastrointestinal symptoms in infancy, most commonly a failure to thrive and malabsorption.
These effects are due to thick pancreatic secretions secondary to ineffective chloride transport, which leads to plugging of the pancreatic acini. This means that the pancreatic enzymes cannot enter the gastrointestinal tract, and the lack of pancreatic enzyme leads to malabsorption of fats. Parents will report typically foul-smelling oily stools and difficulty feeding. Seven to ten percent of patients will have a history of meconium ileus at birth. Diagnosis can be confirmed by a sweat chloride test result> 60 mEq/L. A biopsy may be useful in diagnosing malabsorptive disorders due to mucosal abnormalities such as celiac disease.
75. The answer is a. (Smith Urology) The patient has high-grade reflux that has persisted past puberty. Although there is much debate over the management of VUR in younger patients, the situation in this case is much clearer. High-grade reflux in females that persists into adulthood with no clear secondary cause should be managed surgically. Surgical correction in this population is change to favoured because of the increasd likelihood of the complications of UTIs during pregnancy. During pregnancy, physiologic relaxation of the ureter allows for more urinary stasis and makes women with bacteriuria much more susceptible to developing pyelonephritis. Untreated upper tract infections are associated with morbidity for both the mother and the fetus, including premature labor, low birth weight, preeclampsia, and maternal anemia. This patient is also a candidate because she is already exhibiting the feared complication of untreated VUR, which is renal failure (creatinine 1.5mg/dL). Given this patient's elevated creatinine, infection despite prophylaxis, and risks associated with antibiotics, antibiotics should only be used as a temporizing therapy (i.e.,until elective surgery can be performed).
Dimercaptosuccinic acid scans used the extent of renal scarring that can result in situations where reflux surgery is more questionable or where evidence of organ damage is required before proceeding to surgical management.
76. The answer is d. (Sabiston 19th edition) The patient most likely has a pancreatic pseudocyst, which is a complication of pancreatitis. Pancreatic pseudocyst is not a true cyst; it is lined by granulation tissue 82and collagen. It contains pancreatic juices and lysed blood, so rupture would spill the active digestive enzymes onto the adjacent viscera, particularly the stomach, small intestine, and transverse colon. Digestive action of enzyme elastase produces potentially severe gastrointestinal hemorrhage (pseudoaneurysms). Anaphylactic shock results from massive activation of the IgE-mediated branch of the immune system. Pancreatic secretions do not elicit an IgE response. The classic abdominal cyst that ruptures, producing anaphylactic shock, is a hydatid cyst. Carcinomatosis is widespread serosal spread of a carcinoma, typically due to tumor spillage into a body cavity. Although this may occur with pancreatic mucinous cystadenocarcinoma, this disease is far less likely to occur than is pancreatic pseudocyst in a patient with chronic pancreatitis. Pancreatic pseudocyst is not an infective disease. Although septic abscesses do occur in the abdomen, and may even complicate a pancreatic pseudocyst, the danger of rupture is more associated with tissue destruction by pancreatic enzymes than with infection.
77. The answer is b. (Bailey 25th edition) This patient presents with signs and symptoms suggestive of Zollinger-Ellison syndrome. The most common cause of this condition is a gastrin-producing pancreatic tumor. As a result of uncontrolled gastrin secretion, parietal cell hyperplasia develops and stomach acid production is significantly increased. Multiple duodenal ulcers are typical, and a jejunal ulcer is almost pathognomic for this condition. Steatorrhea may develop, because increased production of stomach acid inactivates pancreatic enzymes. Pancreatic enzyme deficiency is characteristic for chronic pancreatitis and is typically alcohol-related. Reduced bile salt absorption (may develop after ileal resection. Defective intestinal absorption causes malabsorption in various intestinal diseases including non-tropical sprue.
78. The answer is a. (Sabiston 19th edition) Abdominal aortic aneurysms (AAAs) are typically asymptomatic until rupture but can occasionally cause a dull lower back or flank pain. The aneurysms are predominantly caused by atherosclerosis, and more then 90% occur below the renal arteries. Real-time ultrasonography is the gold standard for screening for AAA because sensitivity with this imaging method approaches 100%. Routine sonographic evaluation involves measuring the longitudinal, anterposterior, and transverse dimensions of the aorta. 83The normal diameter of the aorta is approximately 2 cm, and surgery is generally indicated above 5.5 cm The finding of a pulsatile epigastric mass is highly suggestive of AAA. Colonic obstruction does not fit with gradual nature of the complaint. Colonic obstruction would present with abdominal distention and pain in a more acute fashion. An intestinal arteriovenous malformation would rarely be large enough to cause somatic symptoms without also causing hemodynamic complications.
Although the presenting complaint could be interpreted as an episode of chronic pancreatitis, which can also present with a pseudocyst, the mass would not be pulsatile. Furthermore, one would expect pancreatitis to occur in alcoholics or patients with gallstones, neither of which is indicated in this patient
79. The answer is c. (Devita 8th Edition)
Women's Risk level | Mammography | MRI |
|---|---|---|
LCIS ADH ALH | Annual after diagnosis | |
Personal History of Breast Cancer | Annual after diagnosis | |
BRCA (+) Multiple | ||
| Annual screening starting 10 years before diagnosis of youngest relative | Annual |
Hodgkins lymphoma treated With mantle radiation | Annual mammography starting 8 years after treatment | Annual |
80. The answer is a (Devita 9th edition) Breast cancer screening is based on the concept that early detecting of this disease often makes it possible to abort nature progression to death, while a late diagnosis has more ominous outwent.
Breast self examination (BSE) historically has been promoted because of absence of cost, privacy lock of retaliation and self awareness about breast cancer that it promotes. However data meta analysis has reached somewhat different conclusion about its usefulness. Although BSE can be taught to those women who wish to use it, evidence absent support it as an effective breast cancer screening tool.
Clinical breast examination (CBE) is recommended by many organization as post of routine physical examination for a women starting in their 20s. The American cancer society recommences CBE as post of screening tool.
All studies have demonstrated a sensitivity for MRI screening in women at high risk for familial breast cancer.
81. The answer is c. CT scan. (ATLS guidelines 8th edition) In a hemodynamically stable patient with abdominal trauma, the investigation of choice is CECT (contrast enhanced CT scan)
In a hemodynamically UNSTABLE patient with suspected abdominal trauma, the investigation of choice is FAST (focussed abdominal sonogram in trauma).
82. The answer is c. (Bailey 25th edition)
OPSI [Opportunistic post-splenectomy infection]
- Usually caused by encapsulated bacteria (Streptococcus pneumonia, Neisseria meningitides, Haemophilus influenza)
- Risk is greater in younger patients and in patients who have undergone splenectomy for hematological conditions
- Published guidelines emphasise that most infections after splenectomy can be avoided through timely immunization, antibiotic prophylaxis, education and prompt treatment of infection.
- The risk of infection is greatest within 2-3 years after splenectomy
- Patients who have undergone splenectomy before the age of 5 should be given antibiotic prophylaxis (oral penicillin) till that age of 10
- In cases of elective splenectomy, vaccination should ideally be given 2 week before surgery.
- In patients who have undergone an emergency splenectomy, the vaccines should be given in the post-operative period but the antibody titer achieved in these individuals in less than those achieved if the vaccine is given before splenectomy.
- Pneumococcus and meningiococcus vaccine should be repeated after 5 years whereas H.influenzae vaccine should be repeated every 10 years.
83. The answer is b. (Bailey 25th edition)
- USG is the most sensitive investigation for cholelithiasis. [For acute cholecystitis the most sensitive is HIDA scan]
- Gall stones appear as post-acoustic shadows on USG
- It is not a sensitive investigation for the lower end of CBD, as the bowel gas interferes in the study
- CT is the investigation of choice for pancreatitis.
84. The answer is b. (Bailey 25th edition) In this image the tumor is infiltrating into the muscularis propria but not into the serosa, therefore the lesion is B1.
Astler-Coller Modification of Duke's Staging for Colo-rectal cancers
Stage | Features | 5-years survival |
|---|---|---|
A | Tumor confined to the mucosa | 90-95% |
B1 | Tumor growth into muscularis propria | 75-80% |
B2 | Tumor growth through muscularis propria and serosa (full thickness) | 60% |
C1 | Tumor spread to 1-4 regional lymph nodes | 25-30% |
C2 | Tumor spread to more than 4 regional lymph nodes | |
D | Distant metastases (liver, lung, bones) | <1% |
85. The answer is a. (Maingot's Abdominal Operations) From the history and the CT one can make out that the patient is suffering from a pseudopancreatic cyst. All pseudo-pancreatic cysts do NOT require surgery and most of them resolve spontaneously. The indications for intervention in a pseudo-pancreatic cyst are:
- Size more than 6 cms
- More than 6 weeks old
- Wall thickness more than 6 mm (RULE of 6)
Pseudo-pancreatic cysts can be managed by
- Open/ laparoscopic surgery
- Endoscopic surgery
- External drainage
External drainage is indicated in infected cysts but it is important to rule out communication with the pancreatic duct before carrying out external drainage, otherwise it can lead to the formation of a pancreatic fistula.
A pseudo-pancreatic cyst can mimic a cystic neoplasm of the pancreas and this should be suspected if the cyst fluid has high CEA levels (more than 400 ng/ml).
86. The answer is c. (Bailey 25th Edition) The patient has classical history and presentation suggestive of posterior urethral rupture. This is usually associated with pelvic fracture. Retrograde urethrogram (ascending urethrogram) with water based contrast media is the first step in the management of such patients to assess the magnitude of injury. The patient should then undergo a suprapubic catheter insertion. Attempting a Foley's or giving diuretics in such a patient can aggravate the existing injury.
87. The answer is a. (Washington Manual of Surgery 5th Edition 375-376)
Neck is divided into three trauma neck zones.
- Zone I: Clavicles to cricoid cartilage
- Zone II: Cricoid cartilage to angle of mandible
- Zone III: Angle of mandible to base of skull
Zone I injuries: There are chances of vascular injury in this region, which is close to the thorax. Exploration in this region is also difficult because of the presence of vital structures. Evaluation of a patient in this region should include arteriography along with esophagography and bronchoscopy before surgery.
Zone II: This is the most frequently involved region in a neck trauma and often major injuries are missed in this zone. It is therefore advisable, to explore all gunshot wounds, to the middle zone of the neck.
Zone III: Extends from the angle of mandible to the base of skull and exploration in this region is limited. Injuries in this region should be managed by arteriography and embolization.
Zones of the Neck |
|---|
|
88. The answer is c. (Bailey 25th Edition) The question stem describes a patient with fibrocystic disease of the breast. In these patients if a cystic lump is present, it should be aspirated. If it completely disappears on aspiration and the aspirated fluid is not hemorrhagic, the patient should just be kept under observation and no further treatment is required.
If the fluid is hemorrhagic or the cystic cavity does not resolve completely, then local excision should be carried out to rule out malignancy.
- Patient had already undergone an USG of the breast which is more sensitive in younger women in which the breast tissue is more dense
- Oral contraceptives have no role in the management of a cystic lesion in the breast. They are used sometimes to control mastalgia.
- Oral antibiotics should be given to patients with breast abscess after incision and drainage.
89. The answer is d. (Hamilton Bailey Emergency Surgery 13th Edition) In a patient with a bony and neurovascular injury, the bone should be repaired first because sometimes the neurovascular deficit improves after reduction of the fracture segments. Also neurovascular repair is a delicate repair, which can get disrupted if the bony segments are reduced afterwards. Vascular injury takes precedence over nerve injury and should be repaired first.
90. The answer is b. (Hamilton Bailey Emergency Surgery 13th Edition) The question stem suggests that the patient is suffering from cardiac tamponade following a stab injury. Beck's triad is seen in cardiac tamponade – it can be remembered by a mnemonic of 3 D's. – distended neck veins (raised JVP), distant heart sounds (muffled heart sounds) and decreased stroke volume (decreased arterial pressure).
It is a clinical diagnosis and in an unstable patient emergency needle pericardiocentesis should be done. ECG may show low voltage complexes.
Emergency room thoracotomy should not be done immediately in such patients.
91. The answer is a. (Sabiston 18th edition) (Mostly arise from 2nd branchial arch)
- The mature structures of the head and neck are embryologically derived from six pairs of branchial arches, their intervening clefts externally, and pouches internally. Congenital cysts, sinuses or fistulas result from failure of these structures to regress, persisting in an aberrant location.
- By definitions, all branchial remnants are present at the time of birth, although they may not become clinically evident until later in life.
- In children, fistulas are more common than external sinuses, which are more common than cysts.
- In adults, cysts predominate.
- First branchial remnants are typically located in the front of back of the ear, or in the upper neck in the region of the mandible. Fistulas typically course through the parotid gland, deep, or through branches of the faicla nerve, and end in the external auditory canal.
- Remnants from the second branchial cleft are the most common. The external ostium of these remnants is located along the anterior border of the SCM, usually in the upper half to lower third of the muscle. The fistula ascends along the carotid sheath till the hyoid bone and then traverses medially to extend between the carotid artery bifurcation. It then courses behin the posterior belly of digastrics and ends in the tonsillar fossa.
- Third branchial cleft remnants usually do not have associated sinuses or fistulas and are located in the suprasternal notch or clavicular region.
- All branchial anomalies should be excised early in life since repeated infections are common and make the resection difficult at a later stage.
92. The answer is c. (ATLS guidelines 8th edition)
There are three components of GCS:
- Eye openinig
- Motor response
- Verbal response
Response | Score |
|---|---|
Eye opening | |
| 4 |
| 3 |
| 2 |
| 1 |
Motor response | |
| 6 |
| 5 |
| 4 |
| 3 |
| 2 |
| 1 |
Verbal response | |
| 5 |
| 4 |
| 3 |
| 2 |
| 1 |
In verbal response, if the patient is intubated or tracheostomised, then it is denoted as VT and is given a score of 1.
In this patient E3 VT (=1) M5 = 9T
93. The answer is c. (Smith's Urology)
Bladder cancer represents 2% of all cancers, and 90% of bladder cancers are of transitional cell origin. It is most prevalent among men with a history of heavy smoking and exposure to aniline dyes. It is usually multifocal and superficial, even when recurrent. When the disease is still superficial, transurethral resection of visible lesions and intravesicular chemotherapy are most often recommended. More radical surgical resection is reserved for advanced stages of the disease.
BCG is the best intra-vesical agent present. The other agents which can be used for intra-vesical chemotherapy are:
– | Thiopeta | – | Mitomycin C |
– | Doxorubicin | – | Gemcitabine |
94. The answer is d. (Devita 9th edition) Involvement of the pectoralis major muscle is not taken as involvement of chest wall in breast cancer patients and fixed axillary lymph nodes are classified under N2.
95. The answer is b. (Bailey 25th edition) Medullary carcinoma thyroid and RET protooncogene.
MEN 1 – (Wermer's syndrome) – 3 P's
- Pituitary adenoma
- Parathyroid adenoma/ hyperplasia
- Pancreatic tumor
Gene involved in MEN 1 syndrome is menin gene
MEN II (A) – (Sipple syndrome)
- Medullary carcinoma thyroid
- Parathyroid adenoma/ hyperplasia
- Pheochromocytoma
MEN II (B)
- Medullary carcinoma thyroid
- Parathyroid adenoma/ hyperplasia
- Marfanoid habitus
- Mucosal ganglioneuromas
96. The answer is c. (Bailey 25th edition) Cystic hygromas (Lymphangiomas)
Lymphangiomas are thought to arise from a combination of the following: a failure of lymphatics to connect to the venous system, abnormal budding of lymphatic tissue, and sequestered lymphatic rests that retain their embryonic growth potential.
CH usually affects the head and neck (approximately 75%), with a left-sided predilection. Within the neck, the posterior triangle tends to be most frequently affected. Approximately 20% of CHs occur in the axilla; more infrequent subsites include the mediastinum, groin, and retroperitoneum.
They can either present as a swelling in the neck which is brilliantly transilluminant or can present with airway compromise (stridor). They can even lead to obstructed labor during birth.
Management: sclerotherapy or surgical management
Sclerotherapy using OK-432 (Pacibinil) is suitable for unilocular cysts
Surgery is the treatment of choice for multi-septate, large cysts.
97. The answer is c. (Campbell) Lesions that are solid and enhancing on CT scan should raise the suspicion for a renal cell carcinoma. Because of a high false-negative rate, suspicious lesions should not routinely be biopsied. For renal cell cancers less than 4 cm, a partial nephrectomy can be performed, but for larger lesions, a radical nephrectomy (which includes the kidney ipsilateral adrenal gland, and perirenal fat) is indicated. Benign kidney lesions include simple cysts, angiomyolipomas, and oncocytomas. Simple cysts do not require further follow-up, but multiple septations or calcifications should increase suspicion for malignancy. Angiomyolipomas can be diagnosed based on appearance on CT scan and do not require removal; larger lesions are at increased risk for hemorrhagic complications. Oncocytomas can be diagnosed only on pathology.
98. The answer is c. (Transfusion medicine technical manual, 2nd edition by Dr R K Saran (WHO)) TRALI is defined as a new episode of Acute Lung Injury that occurs during or within 6 hours of a completed blood transfusion, which is not temporally related to a competing etiology for acute lung injury.
- It is one of the most important causes of transfusion related morbidity and mortality.
- It is more prevalent with plasma containing blood products.
- It is also called as non cardiogenic pulmonary edema.
- It is caused due to the production of cytokines.
- Clinically – patient presents with fever, respiratory distress, cyanosis, cough, dyspnea.
- On X ray chest – there are bilateral pulmonary infiltrates – “ white out appearance”.
99. The answer is a.
Clinical Presentation | Hormone | Most Common Responsible Tumors |
|---|---|---|
Cushing's syndrome | Corticotropin or corticotropin-releasing hormone | Small-cell carcinoma of the lung, carcinoid tumors, medullary thyroid carcinoma, pheo-chromocytoma |
Hypercalcemia | Parathyroid hormone-related peptide 1,25-Dihydroxycho-lecalciferol | Squamous-cell carcinoma of the lung, skin, head and neck; renal carcinoma; carcinoid tumors Lymphomas |
Acromegaly | Growth hormone Growth hormone–releasing hormone | Carcinoma of the lung. lymphoma Small-cell carcinomas, carcinoid, pancreatic endocrine tumors |
Gynecomastia | Human chorionic gonadotropin | Carcinomas of the lung, bladder, or kidney |
Hyponatremia | Arginine vasopressin | Small-cell carcinoma of the lung, carcinomas of the head and neck |
Hypoglycemia | Insulin-like growth factors | Epithelial and mesenchymal tumors, hepato-cellular carcinoma |
Hypertension | Renin | Wilms' tumor; sarcomas; carcinomas of the lung, ovary, liver, pancreas |
Zollinger-Ellison syndromeo | Gastrin | Pancreatic endocrine tumors, ovarian cancers |
Polycythemia | Erythropoietin | leiomyoma, renal-cell carcinoma, hepatocellular carcinoma |
100. The answer is c. (Transfusion medicine technical manual, 2nd edition by Dr R K Saran (WHO)) This patient in the question stem has suffered from acute massive blood loss. So, he has been given massive blood transfusion.
Massive blood transfusion has been defined as replacement of patient's blood loss with transfusion of stored blood equivalent to the total blood volume within 24 hours.
Complications of massive blood transfusion are:
- C – Coagulopathy
- A – Acidosis
- T – Low temperature (hypothermia)
- C – Citrate toxicity
- H – Hyperkalemia
101. The answer is c. (Transfusion medicine technical manual, 2nd edition by Dr R K Saran (WHO))
Platlets are stored at 20 – 24 degree Celsius with agitation. They can only be stored for 5 days.
Whole blood and packed red cells are stored at 2 – 6 degree Celsius for 35 days. The anticoagulants which are used for their storage are either CPD (Citrate, Phosphate, Dextrose) or CPDA (Citrate, Phosphate, Dextrose, Adenne)
Fresh frozen plasma is stored at – 18 degree Celsius for 1 year.
102. The answer is d. (Tumor lysis syndrome) (Devita 9th Edition)
Spontaneous or treatment-induced cell death leads to a constellation of metabolic abnormalities that together comprise the tumor lysis syndrome (TLS). Although it can occur as a result of ongoing cell death in a rapidly growing tumor, it occurs most frequently following the administration of cytotoxic chemotherapy to patients with hematologic malignancies, where a large percentage of cells are proliferating and drug sensitive. In these patients, TLS occurs a few hours to a few days after the initiation of therapy. Cell death leads to the release of potassium, phosphate, uric acid, and other purine metabolites, overwhelming the kidney's capacity for clearance with resultant hyperkalemia, hyperphosphatemia and secondary hypocalcemia, and hyperuricemia (discussed further below). Significant increases in serum lactate dehydrogenase (LDH) occur frequently. Unchecked, TLS can progress to lactic acidosis and acute renal failure. Although established tumor lysis syndrome is associated with a high morbidity and mortality, judicious prophylaxis can lead to successful treatment or even prevention.
103. The answer is c. (Devita 9th edition)Recognition of the syndrome of inappropriate antidiuretic hormone production (SIADH) as a paraneoplastic syndrome was first reported in 1957, with 95confirmation of this hypothesis in 1968. The principal malignancy associated with SIADH is SCLC (75% of cases), although others have been described (non-small-cell lung cancer, head and neck cancer, and other cancers are also associated with SIADH). Although the majority of SCLC specimens test positive for arginine vasopressin by radioimmune assay, only 3% to 15% of patients with SCLC have the syndrome.
The hyponatremia is initially mediated by antidiuretic hormone (ADH) induced water retention. The ensuing volume expansion activates secondary natriuretic mechanisms, resulting in sodium and water loss and the restoration of near euvolemia. The combination of water retention due to inappropriate ADH secretion and secondary solute loss (sodium and potassium) accounts for the fall of the plasma sodium concentration. Thus, patients with SIADH have normal volume status, hyponatremia with hypo-osmolality, elevated renal excretion of sodium (greater than 20 mEq/L), and urine osmolality greater than plasma osmolality.
104. The answer is b. (Devita 9th edition) Seminoma accounts for approximately 50% of GCTs, and most frequently appears in the fourth decade of life. The typical or classic form consists of large-cell sheets with abundant cytoplasm, and round, hyperchromatic nuclei with prominent nucleoli. Although seminoma displays neither differentiation in vitro or in vivo nor expresses markers of somatic differentiation, essentially all seminomas express PLAP, OCT3/4, and CD117 (the kit receptor). Loss of c-kit expression in seminoma may be associated with a clinically more aggressive phenotype. Embryonal carcinoma and yolk sac tumor display somatic differentiation and surface expression of low-molecular-weight keratins (e.g., AE-1, CAM 5.2). Most embryonal carcinomas, but not seminoma, also express the CD30 antigen Vimentin expression is limited to mesenchymal components of mature teratoma and interstitial and other support cells.
105. The answer is c. (Bailey 25th edition)
A Marjolin's ulcer refers to a squamous cell carcinoma that develops in a chronic wound such as a previous burn scar, chronic venous ulcer or a sinus tract secondary to osteomyelitis. Although basal cell carcinoma, melanoma, and other malignancies can develop in a chronic wound, squamous cell carcinoma is the most common. The mainstay of is treatment is surgical excision or amputation. Kaposi's 96sarcoma usually presents as multifocal lesions on the extremities that may be associated with immunocompromised individuals. Keloids can occur in areas of previous burn and represent an exuberance of wound healing. Surgical excision alone is associated with a high recurrence rate, and other adjunctive modalities that have been utilized include injection of steroids, radiation, external compression, and topical retinoids.
106. The answer is c. (Bailey 25th edition)
Ranulas are mucoceles that occur in the floor of the mouth and usually involve the major salivary glands. Specifically, the ranula originates in the body of the sublingual gland, in the ducts of Rivini of the sublingual gland, in the Wharton duct of the submandibular gland.
These lesions are divided into 2 types: oral ranulas and cervical or plunging ranulas. Oral ranulas are secondary to mucus extravasation that pools superior to the mylohyoid muscle, whereas cervical ranulas are associated with mucus extravasation along the fascial planes of the neck.
- Oral ranula: With most oral ranulas, surgical management is preferred, which includes the removal of the affected gland.
- Cervical ranula: The elimination of cervical ranulas depends on the complete surgical excision of the oral portion of the ranula with the associated sublingual salivary gland or, rarely, the submandibular gland.
- When this procedure is performed, the cervical ranula resolves and has a low risk of recurrence. With drainage of the cervical ranula alone, the recurrence rate is greater than 85%.
The most important factor in surgical management for cervical ranulas is removal of the responsible major salivary gland
Ranulas are brilliantly transilluminant.
107. The answer is c. (DeVita 9th edition)
Breast conservative surgery
Guidelines for patient selection
The four critical elements in patient selection for BCT are
- History and Physical examination
- Mammographic evaluation
- Histological assessment of resected specimen
- Assessment of patient needs and expectations.
Recent (i.e. within 3 month) Preoperative mammographic evaluation is necessary to determine patients eligibility for BCT. MR mammography is the most sensitive investigation to demonstrate multi-sentricity before BCT.
108. The answer is a. (Devita 9th edition) Absolute C/I to Breast conservative therapy:
- Pregnancy: However in many cases it may be possible to perform BCS in third trimester and treat patient with irradiation after delivery.
- Women with two or more primary tumors in separate quadrant of breast or with diffuse malignant appearing micro calcification.
- History of prior therapeutic irradiation to breast
- Persistent positive margins after two surgical attempts.
Relative contraindications:
- H/o collagen vascular disease because reports indicates that such patients tolerate radiation poorly. Scleroderma or active SLE are considered absolute contraindications. In contrast rheumatoid arthritis is not a relative or an absolute contraindications.
- Tumor size-A relative contraindications is the presence of a large tumor is a small breast in which an adequate resection would result is significant cosmetic alteration.
- Breast size-Large or pendulous breast is a realistic contradiction.
109. The answer is d. (Devita 9th edition) Ductal carcinoma in situ
It is defined as proliferation of malignant appearing mammary ductal epithelial cells without evidence of invasion beyond the basement membrane.
Tradition morphological classification
- Comedo
- Papillary
- Micropapillary
- Solid
- Cribiriform
As many as 30 – 60 % of DCIS lesions display more than one histologic pattern.
Treatment of DCIS
Mastectomy, Excision and radiotherapy and excision alone have all been proposed as management strategies for DCIS. The appropriate therapy for women with DCIS depends on the extent of the lesion, risk of local recurrence with each form of treatment and patient's attitude towards the risk and benefits of a particular therapy.
Indications of Breast conserving surgery in DCIS
- Localized DCIS excised to clear margins
- Lesion <2.5 and those with low or intermediate grade.
- Lesion <1 cm with high grade.
Role of Axillary dissection in DCIS
Insitu carcinoma by definition does not metastasize so theoretically axillary staging should be unnecessary inpatients with DCIS.
However most investigations agree that selective used sentinel lymph node biopsy in patients with DCIS who are at significant risk of having co-existent invasive concern is appropriate. Hence it is recommended that in patients requiring mastectomy for DCIS should be subjected to sentinel lymph node biopsy.
Role of Endocrine Therapy in DCIS
Endocrine therapy has two potential benefits in women with DCIS:
- Reduction in Local recurrence after breast conserving therapy.
- Prevention of development of new primary breast cancer in the contra lateral breast.
110. The answer is b. (Campbell 9th edition)
RENAL TRAUMA
Of all the injuries to the genitourinary systems injuries to the kidney from external trauma are the most common.
Hematoma is the best indicator of traumatic running system injury. However, the degree of hematoma and severity of the renal injury do not correlate consistently.
Classification of renal injury (developed by American association for the surgery of trauma's organ injury scaling committee.
Grade | Type | Description |
|---|---|---|
I | Contusion | Microscopic or gross hematoma urologic studies normal |
Hematoma | Subcapsular, Non-expanding without parenchymal laceration. | |
II | Hematoma | Non-expanding perirenal hematoma confined to renal retropontoneum. |
Laceration | <1cm parenchymal depth of renal cortex without urinary extravasation. | |
III | Laceration | >1cm parenchymal depth of renal cortex without collecting system rupture or urinary extravasation. |
IV | Laceration | Parenchymal laceration extending through renal cortex, medulla and collecting system. |
Vascular | Main renal artery or vein injury with contained hemorrhage. | |
V. | Laceration | Completely shattered Kidney |
Vascular | Avulsion of renal hilum Devascularizing the kidney. |
A hemodynamically stable patient with an injury well staged by CT can usually be managed without renal exploration.
The preferred imaging study for renal trauma is contrast enhanced CT. Excretory urography has largely be replaced by CT. The exception is single shot intraoperative IVU. The indications are uncommon, but when surgeon encounters an unexpected retroperitoneal hematoma surrounding kidney during abdominal exploration the study can provide essential information. Only a single film is taken 10 minutes after intravenous injection of 2ml /Kg of contrast material. If findings are not normal or near normal, the kidney should be explored to complete the staging of the injury and reconstruct any abnormality found.
Arteriography is largely used to define arterial injuries suspect or on CT or to localize arterial bleeding that can be controlled by embolization.
The is looted renal injury, without significant associated injuries ours more commonly from blunt trauma in most circumstances can be managed non operatively. The exception is major grade V vascular pedicle avulse injury.
Patients with grade IV parenchymal laceration who have well contained hematomas can be observed expectantly. They should be closely monitored for bleeding with vital signs, serial hematocrit readings and pulse rates. If urinary extravasation is present beyond usher, placement of urinary internal stent for drainage often prevents prolongation of extravasation and decreases the change of per renal urinoma formation.
111. The answer is c. (Campbell 9th edition) Absolute Indications of Exploration
- Evidence of Persistent renal bleeding
- Expanding perirenal hematoma
- Pulsatile perirenal hematoma
Relative Indications
- Urinary extravasation
- Non-Viable tissue >20%
- Delayed diagnosis of arterial injury
- Segmental arterial injury
- Incomplete staging
112. The answer is a. (Campbell 9th edition)
Cryptorchism
Normal testicular descent is defined as testis that remains stationery within the dependent portion of scrotum. Therefore cryptorchism is a developmental defect in which the testis fails to descent completely in to scrotum.
Prerequisite for testicular descent
- Normal hypothalamic pituitary gonadal axis: Defect many occur in production androgen biosynthesis or androgen action.
- Impaired androgen biosynthesis or action may impede the second phase of testicular descent.
- Prenatal treatment with DES (Diethylstilbestrol) a nosteroidal synthetic estrogeon, is associate with impaired trans-abdominal phase of testicular descent.
- Gubernaculum
- Genito femoral Nerve and Calcitonin Gene related peptide
- Intrabdominal Pressure
Key point
- Testicular decent is normally complete between the 30th and 32nd week of question.
- Normal HPG axis is usually necessary for testicular descent.
- Testosterone and DHT are necessary for the inguinoscrotal phase of descent.
- Upto 90% of cases of crytorchidism have associated epididymis anomalies.
Imp: Hypoplasia of Leydig cells, observed from first month of Life, is the earliest post natal histological abnormality in crypt orchid testis.
Consequences
- Infertility: Paternity significantly compromised in men with previous B/ but not unilateral cryptorchidsm.
- Neoplasia: The most common tumor that develops from crypt orchid testis is seminoma.Hernia: Patent processes vaginitis is found in more that 90% of patients with on undescended testis.
- Testicular torsion
Time of surgery (orchiopexy)
Surgery (orchiopexy) remains the gold standard for management of undescended testis. Definitive treatment of an undescended testis should take place between 6 and 12 month of age. The current treatment recommendations of orchiopexy is at 6 month of age.
113. The answer is a. (Mathes Plastic surgery volume 4 pediatric plastic surgery)
With effective presurgical nasoalveolar molding a definitive cheiloplosty (cleft lip repair) is done at age of 3–5 month.
If there is a wide left (>10mm)P and an associated tissue deficiency an initial nasolabial adhesion cheiloplasty is done at 3 month followed by definitive cheiloplasty at about 9 months.
114. The answer is c. (Mathes Plastic Surgery) Timing of Palatoplasty
The timing for palatoplasty is the development of normal speech. Two crucial aspect of palatoplasty are important in optimal speech outcome:
- Surgical technique
- Timing of palate repair
The best time of repair-9-10 month of age for children with apparently normal development. Very early repair have been proposed but long term result are lacking large cohort of these patents.
115. The answer is d. (Sages mannual (fundamentals of laparoscopy, thoracoscopy and g.i. endoscopy)
Laparoscopic TEP repair
Triangle of doom: Boundaries
Medially | Vas deferens |
Lateral | Gonadal vessel |
Base | Pentoneum |
Content | External illiac vessel |
First Bony landmark
The first landmark/ reference point ie the public bone which appears as white glistering structure in the midline.
Injuries to the inferior epigastric and spermatic vessel are the most common vascular injuries reported during laparoscopic hernia repair.
116. The answer is a. (Blumgart)
Gall stone Ileus
Blockage of the intestinal tract by a gall stone long enough to occlude its lumen partially or completely.
The classical plain abdominal film triad of small bowel obstruction, pneumibila and ectopic gall stone is considered pathognomic of gall stone ileus.
Site of obstruction:- terminal ileum is the site of obstruction is 70 % of cases. In rare instances sigmoid colon is the site of obstruction in case having choleystocolic fistula man.
117. The answer is a. [Blumgart]
The overriding consideration in patients should be relief of the life threatening cause of obstruction i.e. enterolithotomy
There is considerable debate is the surgical literature regarding whether cholecystectomy or CBD exploration with dismantling closure of the cholecystoenteric fistula should accompany enterotomy and relief of obstruction or await a second operation. Data is more in favour of two staged procedure.
118. The answer is b. (Blumgart)
Management of Bile Duct Injury
Injury recognized at Initial Operation
- If injury is recognized at the time of the initial choleystectomy, the surgeon should consider his or her experience and ability to repair it immediately.
- For complete duct transection preferred and recommended approach in Roux-en-Y hepaticojejunostomy.
- Injury to lateral duct wall may be amendable to direct suture repair, with or without T-Tube. Latest report discourages placement of T-Tube for such repairs.
- Long Lateral injuries which are not circumferential preferred approach is Roux-Eu-Y loop of jejunum as a serosal patch with T tube placed across the defect.
119. The answer is a. (Blumgart)
Injuries Recognized in the immediate post operative period
- The mode of presentation may be bile drainage through the wound, bile peritonitis or progressive jaundice depending on the Injury type.
- Drainage of the Bile collection and control of the ongoing bile leak is the primary objective.
- Requires percutaneous drain in combination with percutaneous or endoscopic biliary drainage.
- Definitive repair is seldom possible initially with the bile ducts collapsed, deeply bile stained and friable and is best delayed until the bilary leak has been controlled completely and the patient resuscitated fully.
120. The answer is a. (Devita 9th edition)
Treatment of Well differentiated Papillary thyroid carcinoma.
There is a long standing controversy among endocrine surgeons regarding the extent of surgery in well differentiated thyroid cancers because of its multi-centric nature
Devita advocates for a more aggressive (i.e. total thyroidectomy) for a vast majority of patients with well differentiated papillary thyroid carcinoma. This recommendation is also shared with the recent 105American thyroid Association guidelines. The author concluded that the significant improvement in local recurrence with a minimal operative morbidity in the hands of experienced surgeon would lead to recommendation of total thyroidectomy for even low risk category of patients.
121. The answer is a. (Devita 8th edition.) Medullary Thyroid Carcinoma
Most patients with sporadic MTC typically presents with an asymptomatic thyroid mass. Patient with bulky disease, local or metastatic with extremely high levels of calcitonin may have severe secretary diarrhea as principal symptom.
122. The answer is a. ([Devita 9th edition])
T/t of MTC
Chemotherapy and EBRT (Ext. Beam RT) are of the most part ineffective against MTC rendering surgical resection the only definitive therapy.
For MTC the appropriate operation in much cases is total thyroidectomy with central node dissection and ipsilateral modified neck dissection (if central in enlarged or tumor size > 2 cm.)
For metastatic MTC, surgical resection may still offer the best chance of survival as well as long term palliation.
123. The answer is d. (Devita 9th edition) Risk factors for cholangio carcinoma
In most patients cholangiocarcinoma are sporadic and no precipitating factor can be identified. In minority of patients, a number of risk factors can be identified. In minority of patients, a number of risk factors can be identified. These predisposing factors all cause inflammation of the bile duct. These include:
Primary Sclerosing cholangitis most important risk factor
- Choledochal cyst
- Lives fluke infestations
- Chronic calculi of the bile duct chole-docholithiasis)
- Chronic portal bacteremia and portal phelebitis.
- Anomalous pancreaticobilary junction.
- Exposure to thorotrast.
- Cigarette smoking.
- HIV
- Alcoholic liver disease.
- Hepatolithiasis.
- Diabetes Mellitus.
- Cholelithiasis has minimal impact as a risk factor for cholongiocarcinoma.
124. The answer is a. (Devita 9th edition)
Most common site of chlogiocarcinoma
Hilum | – | 67% |
Distal | – | 2.7% |
Intrahepatic | – | 6% |
Most common presentation painless jaundice 70-90%), followed by pruritus (66%), abdominal pain, weight loss (30-50%) and fever (20%).
125. The answer is c. (SAGES manual) Classification of surgical procedures
Predominantly malabsorptive procedures
- Biliopancreatic diversion
- Jejunoileal bypass
- Endoluminal sleeve
Predominantly restrictive procedures
- Vertical Band Gastroplasty
- Adjustable gastric band
- Sleeve gastrectomy
- Intragastric balloon
Mixed procedures
- Gastric Bypass Surgery
- Sleeve gastrectomy with duodenal switch
- Implantable Gastric Stimulation
126. The answer is a. (Blumgart)
Bile Duct Anastomosis
The donor and recipient common bile ducts are anastomosed end-to-end using interrupted fine sutures usually 6-0 PDS. The anastomosis 107may be stented with a Ttube brought out through the distal recipient duct. The T-tube is removed 3 months later, after a normal cholangiogram has been obtained. Many surgeons no longer use T-tubes routinely. Less commonly, If there is a major size discrepancy between the donor and recipient ducts, or if the recipient bile duct is diseased (as in PSC) or too small (as in pediatric cases), a choledochoje-junostomy is performed. The duct is anastomosed to a Roux-en-Y limb of jejunum using a stented end-to-side technique.
127. The answer is d. (Trauma care) RTS, ISS, AGE are included in TRISS
TRISS The international golden standard for severity scoring and probability of survival (Ps) calculation is the TRAUMA AND INJURY SEVERITY SCORE/ TRISS. TRISS is a composite calculator based on anatomical and physiological severity indicators. For TRISS operation, the RTS parameters(RR, BP, GCS) are vected, vectors being deducted by logistic regression analysis on large US trauma databases
RTS(vected) = 0.9386(GCS CODE) + 0.7326(BP code)+ 0.2908(RR code).RTS can thus take on values from 0 to 7.848
TRISS is based on a probability distribution: Ps=1/(1+e)^ (-b)
The value b is set by the regression equation b= b0 +b1(RTS)+b2(ISS) + b3(AGE). AGE is defined as a dichotomy vaiable: (AGE <55yrs)= 0: (AGE > 55yrears)= 1. THE value b is set separately for blunt and penetrating injury.
128. The answer is a. (Smith's Urology) Compliation of PCNL
The most common complication of PCNL is bleeding. Others are extavasation, inadvertent perforation of collecting system, incomplete stone removal and sepsis. But in few cases to approach upper calyceal stones 11th rib approach is employed in thoses cases pleural injury in the form hydrothorax or pneumothorax is more common.
- Bleeding – venous bleeding is most common, it can be managed by clamping the nephrostomy tube for 30 to45 min. arterial bleeding is more serious prolem, can occur either preoperative or in postoperative period.
- Extravasation-normal saline should be used as the irrigation fluid to minimize adverse effect if extravasation occurs..
- Retained fragments-on a post procedure film can be an unwanted finding. Reinsertion of the nephroscope will permit removal. Sometimes stones are extruded through the collecting system or noted in the perinephric tissues outside the kidney. It is not important to remove them.
- PUJ
- Sepsis
However in case when PCNL is done through 11 th rib approach most common complication is pleural injury in the form of hydrothorax, hemopneumothorax.
129. The answer is a. (Sabiston 19th edition) The onset of irregular respirations, bradycardia, and, finally, increased blood pressure with increasing intracranial pressure (ICP) is termed the Cushing response. These physiologic alterations are caused by brainstem compression. Slow rises in ICP are, by contrast, autoregulated by the brain's compensatory mechanisms and lead to a late onset of neurologic sequelae. A mass lesion is more apt to compromise local cerebral blood flow and to increase cerebral edema and ICP. The vector of the mass effect may lead to herniation of brain parenchyma through the tentorial incisura or foramen magnum, with resultant brainstem compression. Herniation usually causes compression of the third cranial nerve and thus leads to a fixed and dilated pupil on that side. Papilledema is a finding with chronic increases in ICP.
130. The answer is d. (Sabiston 19th edition) Atherosclerotic occlusion of the subclavian artery proximal to the vertebral artery is the anatomic situation that results in the subclavian steal syndrome. On being subjected to exercise, the involved extremity (usually the left) develops relative ischemia, which gives rise to reversal of flow through the vertebral artery with consequent diminished flow to the brain. The upper extremity symptom is intermittent claudication. Venous occlusive disease is not a feature of the syndrome. The operative procedure for treating the subclavian steal syndrome consists of delivering blood to the extremity by creating either a carotid-subclavian bypass or a subclavian-carotid transposition. Dilatation and stenting of the artery by endovascular techniques is effective as well.
131. The answer is d. (Devita 9th edition) There is no difference in cure rate between Mohs surgery and wide local excision of a basal cell 109carcinoma. Mohs surgery describes a technique for resecting either basal or squamous cell carcinomas on the face or near the nose or eye in order to achieve the optimal cosmetic result. Resection of the tumor is performed in small increments with immediate frozen section analysis in order to ensure negative margins. The disadvantage of the Mohs technique is the longer time required.
132. The answer is d. (ATLS guidelines 8th edition) The patient is in neurogenic shock as a result of a spinal cord injury. Neurogenic shock is characterized by loss of sympathetic tone peripherally as well as bradycardia due to loss of the reflexive increase in heart rate in response to hypotension. Initial treatment is with fluid resuscitation followed by initiation of vasoconstrictors such as dopamine or phenylephrine. Hypovolemia due to hemorrhage should also be ruled out in trauma patients. Steroids might seem an attractive option but they are not used in the initial management of these patients.
133. The answer is d. (ATLS guidelines) At one time all full thickness burns were allowed to heal by granulation over a period of 2-3 weeks, before skin grafting was done. The area was kept free of bacteria by the use of topical agents. the current preference is to do early excision and grafting of burned areas that appear to be full thickness, if they are not extensive. Best time of this is within 3-5 days and it should not be delayed beyond 10 days. Debridement is often indicated in the long term preparation of the area to be grafted but wet to dry dressing would be less effective than antibacterial agents. Mafenide is used in areas where deep penetration is needed, otherwise its not a first choice as its application is painful and can produce acidosis.
134. The answer is c. (Devita) The most common procedure today for treatment of localized renal carcinoma greater than 4 cm is radical nephrectomy. Radical nephrectomy includes complete removal of Gerota's fascia and its contents, including the kidney and the adrenal gland, and provides a better surgical margin than simple removal of the kidney. Many clinicians believe that in view of the rarity of ipsilateral adrenal metastasis and the potential morbidity associated with adrenalectomy, a macroscopically normal ipsilateral adrenal gland should not be removed with the kidney when the tumor is in the lower pole of the kidney The treatment of patients with either bilateral renal 110carcinoma or renal carcinoma in a solitary kidney is evolving toward a more minimally invasive approach. Patients with tumor in a solitary kidney may be treated by either partial nephrectomy or nephrectomy followed by dialysis and/or transplantation if the tumor is too large for a partial nephrectomy. In selected patients, nephron-sparing surgery may be recommended for patients with sporadic renal cell cancer, particularly those with a small tumor (4 cm or less) or a tumor in a solitary kidney. Nephron-sparing surgery for localized renal tumors has been found to be a safe procedure, providing long-term tumor control and preservation of renal function.
135. The anwer is c. Graigner and Allison Diagnostic Radiology
Radial scars, also called complex sclerosing lesions, can produce a spiculated lesion indistinguishable from malignancy on both mammography and ultrasound. Many of these lesions are asymptomatic and are encountered on screening mammography. It Is also called great mimic of carcinoma breast
136. The answer is a. (Blumgart) Bismuth Strasberg Classification Of Biliarry Injury And Stricture
CLASS A | Injury to small ducts in continuity with the biliary system, cystic duct leak |
CLASS B | Injury to sectoral ducts with consequent obstruction |
CLASS C | Injury to sectoral duct with consequent bile leak |
CLASS D | Lateral injury to extrahepatic ducts |
CLASS E1 | Stricture > 2 cm distal to bifurcation |
CLASS E2 | Stricture < 2 cm distal to bifurcation |
CLASS E3 | Stricture at bifurcation |
CLASS E4 | Stricture involving right and left ducts, ducts are not in continuity |
CLASS E5 | Complete obstruction of bile buct |
MRCP has been demonstrated to be an effective non invasive method for demonstrating billiary leakage or obstruction as well as precisely defining anatomy and the nature of the injury.
137. The answer is a. (Bailey 25th edition) A robot is a mechanical device that performs automated physical tasks according to direct human supervision, a predefined program or a set of general guidelines 111using artificial intelligence techniques. In terms of surgery, robots have been used to assist surgeons during procedures. This has been primarily in the form of automated camera systems and telemanipulator systems, thus resulting in the creation of a human–machine interface. There are different robotic systems available. Robotic camera systems include AESOP (Computer Motion, Goleta, California, USA) and EndoAssist (Armstrong Healthcare Ltd, High Wycombe, UK). Telerobotic manipulators include the da Vinci (Intuitive Surgical, Inc., Menlo Park, California, USA) and ZEUS (Computer Motion, Goleta, California, USA) manipulators. Finally, telerobotics and telementoring has been combined in systems such as SOCRATES (Computer Motion, Goleta, California, USA). All of these systems offer different advantages to the operating surgeon, ranging from reducing the need for assistants and providing better ergonomic operating positions to providing experienced guidance.
138. The answer is b. (Schwartz) Cerebral contusions are bruises of neural parenchyma that most commonly involve the convex surface of a gyrus. The most frequent sites of cerebral contusion are the orbital surfaces of the frontal lobes and the anterior portion of the temporal lobes. The etiology of the contusion is always traumatic. Injuries may be seen both at the site of impact (coup) and in parenchyma opposite the site (contre-coup). Patients deemed to have a substantial contusion should receive anti-convulsants to prevent seizures in the early posttraumatic period.
139. The answer is d. (Schwartz)
Both low-dose heparin and pneumatic compression stockings are acceptable prophylactic mea-sures in patients at moderate risk for deep vein thrombosis; however, they are not effective against established thrombosis, the initial treatment for which is therapeutic heparinization (either with intravenous heparin or low-molecular-weight heparin administered subcutaneously). Even following prompt, aggressive treatment of deep vein thrombosis of the calf, as many as half of affected patients will develop symptoms of chronic venous hypertension, and a larger number will have abnormal venous hemodynamic findings. Untreated vein thrombosis of the calf may propagate into the larger popliteal veins and cause life-threatening pulmonary embolism.
140. The answer is d. (Schwartz)
Any patient who has lost much of the ileum (whether from injury, disease, or elective surgery) is at high risk of developing hyperoxaluria if the colon remains intact. Calcium oxalate stones can subsequently develop due to excessive absorption of oxalate from the colon.
141. The answer is a. [Schwartz]
The slow progression of aortoiliac atherosclerotic occlusive disease is usually associated with the development of collateral flow through the lumbar branches of the aorta anastomosing via retroperitoneal branches of the gluteal arteries with the profunda femoris arteries in the legs. This network of collateral vessels provides sufficient blood flow to nourish the extremities at rest but cannot prevent claudication of the upper and lower muscle groups of the leg during exercise. Sexual impotence, also part of Leriche's syndrome, is believed be a result of bilateral stenosis or occlusion of the hypogastric arteries. Retrograde ejaculation can occur after disruption of the sympathetic chain overlying the distal aorta and left iliac and can occur after dissection around these vessels during vascular reconstructions. Gangrene of the feet or toes is rarely seen unless distal embolization of atherosclerotic material from the aorta occludes the pedal or digital arteries.
142. The answer is b. (Schwartz)
The initial and often defin-itive management of hyponatremia is free-water restriction. Symptomatic hyponatremia which occurs at serum sodium levels less than or equal to 120 meq/L, can result in headache, seizures, coma, and may require infusion of hypertonic saline. Rapid correction should be avoided so as not to cause central pontine myelinolysis, manifested by neurologic symptoms ranging from seizures to brain damage and death. Additionally a search for the underlying etiology of the hyponatremia should be undertaken.
143. The answer is a. (Schwartz)
The appropriate dosing and timing of antibiotic prophylaxis to prevent surgical site infections in an elective procedure is a single dose no greater than 1 h prior to the incision. Additionally, most textbooks recommend use of an oral, non-absorbable antibiotic regimen effective against aerobes and anaerobes in combination with a mechanical bowel preparation before elective colon resections. There is no evidence to support the continuation of antibiotics for more than 12 113hrs after an elective operation has been completed and this practice should be avoided to prevent increasing microbial drug resistance. Broad-spectrum antibiotic coverage, including against anaerobic organisms, is required only in cases where such flora are anticipated, such as during colon resections; otherwise cefazolin is the antibiotic of choice for cases requiring antibiotic prophylaxis.
144. The answer is c. (Schwartz)
Heparin induced thrombocytopenia (HIT), which is a complication of heparin therapy, at both prophylactic and therapeutic doses of heparin, is mediated by antibodies to the complexes formed by binding of heparin to platelet factor 4 in a pre-viously unexposed patient. HIT typically manifests after five days as a decrease in platelet counts by 50% of the highest preceding value or to a level less than 100.000/mm3. Complications of HIT are related to venous and/or arterial thromboembolic phenomena. Treatment of HIT consists of cessation of heparin (including low-molecular weight heparins) and institution of a non-heparin anticoagulant such Lepirudin and conversion to oral warfarin when appropriate. Cessation of heparin alone is inadequate to prevent thromboembolic complications, and warfarin should not be started until the platelet count is above 100,000/cumm. Platelet transfusion is not indicated, as HIT results in thrombotic rather than hemorrhagic complication.
145. The answer is a. (Sabiston 19th edition, Robbins)
Glioblastoma multiforme is the most common form of primary intracranial neuro-epithelial tumor. It is a heterogeneous glial cell tumor derived from the malignant degeneration of an astrocytoma or anaplastic astrocytoma. These tumors are most com-monly found in the cerebral hemispheres during the fifth decade of life. CT and MRI scans typically reveal an irregular lesion with hypodense central necrosis, peripheral ring enhancement of the highly cellular tumor tissue, and surrounding edema and mass effect. Curative resections are rare. Therapy consists of surgical resection followed by external beam radiation. The course of the disease progresses rapidly after presentation, with median survival being one year.
146. The answer is d. (Sabiston 19th edition)
Penetrating injury to the intra-peritoneal or extra-peritoneal rectum should be diagnosed by immediate sigmoidoscopy. Contrast studies 114of the rectum when sigmoidoscopy is inconclusive should use a water soluble radiopaque medium such as gastrografin. The use of barium is contraindicated because its spillage into the peritoneal cavity mixed with faces would increase the likelihood of subsequent intra-abdominal abscesses. Instrumentation of the bullet track is also contraindicated because of the risk of injury to adjacent structures. Angiography is not a sensitive method for demonstrating injury of the intestinal wall.
147. The answer is d. (Bailey 25th edition) The various agents used for dressing of burns are:
Silver sulphadiazine cream (1%)
- Provides broad spectrum prophylaxis particularly against Pseudomonas (commonest cause of secondary infection in burns patients); also effective against MRSASilver nitrate solution (0.5%)
- Highly effective against Pseudomonas
- Needs to be changed every 2-4 hours
- Produces black staining of all furniture
- Complications – methemoglobinemia, hyponatremia
Mafenide acetate cream- Painful
- 5% solution; can lead to metabolic acidosis
Silver sulphadiazine and cerum nitrate- Induces hardening of burnt skin
- Reduces immunosuppression caused by burns
148. The answer is b. (Sabiston 19th edition)
Increasing intracranial pressure tends to displace brain tissue away from the source of the pressure and if the pressure is sufficient, herniation of the uncal process through the tentorium cerebri occurs. Pupillary dilation is caused by compression of the ipsilateral oculomotor nerve and its parasympathetic fibers. If the pressure is not relieved, the brainstem will herniate through the foramen magnum and cause death.
149. The answer is c. (Bailey 25th edition)
In patients with suspected necrotizing fascitis, an infection of the superficial and deep fascia that is associated with high rates of morbidity 115and mortality, prompt surgical exploration is mandatory. These infections are more common in immunocompromised patients. Treatment consists of prompt surgical debridement and intravenous antibiotics. Most of these infections are polymicrobial, although mono-microbial necrotizing soft tissue infections can be caused by group A beta hemolytic streptococcus or clostridium. If the latter is suspected, high dose penicillin G should be administered. Hyperbaric oxygen may be used as an adjunct in the management of such patients.
150. The answer is c. (ATLS guidelines)
The spectrum of blunt cardiac injuries includes myocardial contusion, rupture and internal (chamber and septal) disruptions such as traumatic septal defects, papillary muscle tears, and valvular tears. Myocardial contusions are by far the most common of these injuries. They usually occur in persons who sustain a direct blow to the sternum as seen in a driver whose sternum is forcibly compressed by the steering column in a deceleration injury. They may have external signs of thoracic trauma, including sternal tenderness, abrasions, ecchymosis, palpable crepitus, rib fractures or flail segments. Only 10% patients show abnormalities on the initial ECG. Elevated cardiac isoenzyme levels are specific for myocardial injury, but they lack clinical significance in patients without ECG abnormalities or hemodynamic instability. Echocardiography provides a sensitive assessment of ventricular wall motion and ejection fraction after blunt chest trauma but is a poor predictor of the significant cardiac complications of pump failure and arrhythmia. Patients without evidence of ECG abnormalities on presentation and who are hemodynamically stable do not require extended ICU monitoring.
151. The answer is d. (Sabiston 19th edition)
Penetrating injury to the intra-peritoneal or extra-peritoneal rectum should be diagnosed by immediate sigmoidoscopy. Contrast studies of the rectum when sigmoidoscopy is inconclusive should use a water soluble radiopaque medium such as gastrografin. The use of barium is contraindicated because its spillage into the peritoneal cavity mixed with faces would increase the likelihood of subsequent intra-abdominal abscesses. Instrumentation of the bullet track is also contraindicated because of the risk of injury to adjacent structures. Angiography is not a sensitive method for demonstrating injury of the intestinal wall.