Headquarter
Jaypee Brothers Medical Publishers (P) Ltd
4838/24, Ansari Road, Daryaganj
New Delhi 110 002, India
Phone: +91-11-43574357
Fax: +91-11-43574314
Email: jaypee@jaypeebrothers.com
Overseas Offices
J.P. Medical Ltd
83 Victoria Street, London
SW1H 0HW (UK)
Phone: +44-2031708910
Fax: +02-03-0086180
Email: info@jpmedpub.com
Jaypee-Highlights Medical Publishers Inc
City of Knowledge, Bld. 237, Clayton
Panama City, Panama
Phone: + 507-301-0496
Fax: + 507-301-0499
Email: cservice@jphmedical.com
Jaypee Brothers Medical Publishers (P) Ltd
17/1-B Babar Road, Block-B, Shaymali
Mohammadpur, Dhaka-1207
Bangladesh
Mobile: +08801912003485
Email: jaypeedhaka@gmail.com
Jaypee Brothers Medical Publishers (P) Ltd
Shorakhute, Kathmandu
Nepal
Phone: +00977-9841528578
Email: jaypee.nepal@gmail.com
Jaypee Brothers Medical Publishers Ltd
The Bourse
111 South Independence Mall East
Suite 835, Philadelphia, PA 19106, USA
Phone: + 267-519-9789
Email: joe.rusko@jaypeebrothers.com
Website: www.jaypeebrothers.com
Website: www.jaypeedigital.com
© 2013, Jaypee Brothers Medical Publishers
All rights reserved. No part of this book may be reproduced in any form or by any means without the prior permission of the publisher.
Inquiries for bulk sales may be solicited at: jaypee@jaypeebrothers.com
This book has been published in good faith that the contents provided by the author contained herein are original, and is intended for educational purposes only. While every effort is made to ensure accuracy of information, the publisher and the author specifically disclaim any damage, liability, or loss incurred, directly or indirectly, from the use or application of any of the contents of this work. If not specifically stated, all figures and tables are courtesy of the author. Where appropriate, the readers should consult with a specialist or contact the manufacturer of the drug or device.
Obstetric Vasculopathies
First Edition: 2013
9789350903445
Printed at
ARTHRITIS (FLOW CHART 6 OF ANNEXURE)
Osteoarthritis is idiopathic slowly progressive disease of synovial joints occurring late in life and characterized pathologically by focal cartilage degeneration, subchondral bony thickening, marginal osteochondral outgrowths and joint deformity.
- Primary osteoarthritis—unknown etiology.
- Secondary osteoarthritis—trauma, stress, loads, infection, rheumatoid arthritis, gout, chondromalacia patellae.
- It begins at second decade.
- Women are more frequently affected.
- Prevalent in obese.
- Patients present with pain, stiffness, crepitus, osteophytes, decreased range of motion, locking.
- X-ray—decreased joint space, sclerosis, subchondral cyst, osteophytes, bony collapse, loose bodies, deformity and malalignment.
- Conservative treatment modalities—rest, exercise, support, traction, physiotherapy, corticosteroids.
Rheumatoid Arthritis
It is chronic inflammatory joint disease affecting young or middle aged adult characterized by deforming polyarthritis affecting small and large peripheral with associated systemic disturbance and circulating antiglobulin antibodies rheumatoid factor affects synovial membrane, perineural sheath which causes joint destruction ankylosis, and deformity.
- Male:female = 1:3 more common in females
- Genetic influence—increase lymphocyte activation with defined HLA class 2 haplotype
- Immune overactivity may be the cause
- Infectious agents—Streptococcus, Bacillus, Mycoplasma
- Endocrine—adrenocorticosteroids
- Allergy—eosinophilia.
Diagnosis features:
- Morning stiffness
- Arthritis of 3 or more joints (pain on motion/joint tenderness)
- Arthritis of peripheral joints of hand swelling (soft tissue thickening) in at least 1 joint > 6 weeks
- Symmetrical arthritis
- Rheumatoid nodules
- Rheumatoid factor
- Radiological changes
- Poor mucin clot
- Histological changes in synovium.
X-Ray features of rheumatoid arthritis:
- Soft tissue prominence around the joint, joint space narrowing, osteopenia delayed erosions, cystic spaces, subluxations and deformities, ankylosis.
- Absorption of locally applied NSAIDs is usually not proper but have a strong psychological value.
- Treatment is rest, splint, intra-articular steroids, NSAIDs, DMARDs, surgery.
Role of Corticosteroids
Intra-articular (IA) steroids produce marked improvement in symptoms, lasting for weeks to months. But repetitive large dose injections are associated with delayed repair and may lead to more cartilage damage. It is recommended that their use should not be more than 3–4 times a year. Inflammatory reaction to crystalline depot preparation may occur but it does not affect efficacy of the injected steroid.
Incidence of joint infection following steroid is low.
Steroids are useful for rapid disease control until DMARDs start acting. They have been shown to reduce progression, but should be administered not on routine basis because of their side effects. Intra-articular steroids should be used to treat disease limited to few joints, or to treat acute flare in a joint. Over enthusiastic and frequent use of Intra-articular steroids should be avoided, (not more than 3 joints it a time, not the same joint more than 3 times a year, and a minimum interval of 3 months between successive injections in the same joint).3
Crystal Induced Arthropathy
Diagnosis: Intra and/or periarticular calcification with or without erosions destruction or hypertrophic changes may be seen on X-ray. Definitive diagnosis depends on identification of crystals from synovial fluid or tissue. Hydroxyapatite crystals are very small, nonbirefringent and can only be seen by electron microscopy. Appetite aggregates may appear as 1–20 shining intra- or extracellular globules that stain bright red with alizarin red S (nonspecific calcium staining).
It is necessary to differentiate it from sepsis, late avascular necrosis and neuropathic joint.
Treatment: No specific treatment is available. Acute attacks usually resolves spontaneously over 1 to 3 weeks. NSAIDs, oral colchicine, aspiration of effusion and intra-injection of steroid shorten the duration and intensity symptoms. Destructive arthropathy usually requires joint replacement surgery.
Ankylosing Spondylitis
Chronic inflammatory disorder in late adulthood and young age characterized by progressive inflammation of spine, sacroiliac joints and large joints of extremity leading to fibrous or bony ankylosis and deformities associated with HLA B 27.
Primary site of affection is attachment of ligaments and capsules to bone with enthesopathy, fibrosis, calcification, ossification to para-articular structures-degenerated calcified and ossified, commonly anterior longitudinal ligament of spine but are friable and rupture and easily increase bone production adjacent to joint.
Rome criteria for ankylosing spondylitis—low back pain and stiffness > 3 months not decreased by rest, stiffness in thoracic and decreased motion of lumbar spine, decreased chest expansion, iritis and its sequelae, bilateral sacroilitis, with X-ray and one or more clinical criteria /4 of 5 clinical criteria are useful in diagnosis.
Tendons are made of specialized cells including tenocytes, water and fibrous collagen proteins. These collagen proteins weave together to form a strand of flexible tissue to make up tendon. They anchor to the bone and form a mineralized connection.
Tendons transfer force, and as a result are susceptible to injury when they are overused. With repetitive overuse, collagen fibers in the tendon may form micro- tears, leading to tendonitis; or more appropriately tendinosis or tendinopathy.
The injured tendons heal by scarring which adversely affects function and increases risk of reinjury adding to the problem tendons heal at a slow rate due to poor vascularization (Flow chart 3 to 5 of Annexure).
Chronic cases indicate that there is no inflammatory response, but rather a release of one's own natural growth factors for normal tendon repair with a fibroblastic and a vascular response called, angiofibroblastic degeneration. Due to this mode of healing, treatment options including dry needling, prolotherapy, and extracorporeal shockwave therapy are aimed at increasing inflammation rather than suppressing it.
Peritendinitis is inflammation of paratendon which causes, pain, tenderness and restricted movements of muscles.4
Tendinosis—degenerative changes in tendon. Macroscopically-degenerative changes in tendon with disorganized tissue, microscopically-degenerative changes to collagen with fibrosis. Inflammatory mediators are not usually present as more degenerative changes occur.
Muscle imbalance is a cause of tendinitis.
Tendinitis or Tendonitis is inflammation of tendon and the paratendon. Chronic overload cause microscopic tears in tendon which trigger's inflammatory response. Over use/overload cause sudden accentuation of tendinitis.
Bursae are sacs lined with a membrane usually located about joints or where skin, tendon or muscle moves over a bony prominence and may or may not communicate with a joint. They reduce friction. These are two types.
- Those normally present, e.g. patella and olecranon
- Adventitious bursae—Bunion, osteochondroma
Adventitious bursae are produced by trauma friction or pressure.
Mechanical theory—Repeated loading causes microscopic degeneration. fibroplasias occurs within tendon which in turn cause scar tissue.
Vascular theory—Areas of local vascular disruption.
Neural modulation—Neurally mediated mast cell degranulation and release of substance p. Treatment of bursitis is treatment of primary cause of bursitis.
Conservative treatment in form of rest, hot wet pack, elevation, where applicable immobilization should be done, is very effective most of the times.
Surgical procedures useful are:
- Aspiration and injection of appropriate drug
- Incision and drainage of acute suppurative bursitis which fails to response to non-surgical treatment—rarely indicated
- Excision of chronically infected and thickened Burse
- Removal of underlying bone prominence.
Traumatic Bursitis Respond Favorably to Aspiration
Adventitious bursa develops as a result of repeated trauma and is more susceptible to inflammatory changes.
Syringes and Needles Used
Syringes used for injection: 2 ml, 5 ml, 10 ml depending on the quantity of drug to be injected or aspiration to be done and site of injection.
Needles used are 18 gauge usually for aspiration and 22, 24 gauge used for injection (Figs 1.2, 1.4, 1.8 and 1.10).
INJECTABLE CORTICOSTEROIDS
Mechanism of Action
Decreasing inflammation in synovial tissue is primary effect in synovial tissue of depot corticosteroid. The effects particularly profound on edema as well as the 5number of lymphocytes macrophages and mast cells. It has also been found that there is production in inflammatory cell in joints after corticosteroid injection. Although this may be preceded by mild initial inflammatory response immediately following injection.
It also has systemic effects on non-involved inflamed joints.
Marked improvement in inflammatory markers such as ESR, CRP, can occur in patients with rheumatoid arthritis who receive corticosteroid.
Depot formulations are useful due to local effects for long-term. Less soluble agents are preferred.
Most commonly used corticosteroid is methyl prednisolone acetate (35%).
Ability of methyl prednisolone for use in both joints and soft tissues are likely to contribute to its widespread use compounds with lower solubility have more synovial levels for a longer time and produce low systemic levels then would compounds with greater solubility.
A lower systemic level of corticosteroid is generally viewed as favorable feature because of potential reduction in systemic toxicity.
Compounds with low solubility are well suited for intra-articular injections. They may not be appropriate for soft tissue injections because of associated side effects.
Injectable corticosteroid often combine with local anesthetics because injecting both agents not only can verify that site injected was the source of pain.
Uses: Used in osteoarthritis and rheumatoid arthritis other joint conditions such as juvenile. Rheumatoid arthritis, crystal deposition diseases, connective tissue disease psoriatic arthritis. Ankylosing spondylitis and arthritis associated with inflammatory gastrointestinal disorders.
Goal is to relieve pain and control synovitis associated benefit of reducing synovitis may be ability to exercise and muscle strength.
They have also been used after arthroscopic surgery and rehabilitation period.
Corticosteroids are also useful in nonarticular disorder like overuse syndrome (tendinitis, bursitis, ligament sprain, tenosynovitis) acute athletic injuries and nerve compression syndromes, rather than entering joint extra-articular sites are targeted.
Outcomes in patients who received accurately placed injections are good.
Safety
Glucocorticoid injection of joints and periarticular structures are safe and effective when administered by experienced physician, most commonly there is transient injection pain.
Rare long-term effect is subcutaneous injection causing lipodystrophy.
Absolute contraindication to corticosteroid is joint infection, presence of prosthetic joint or fracture in joint.
Caution should be used in patients with joint instability, coagulopathy or overlying cellulitis or infection.6
Side Effects
Most common side effects are postinjection flare, facial flushing and skin or fat atrophy.
Frequency of these events depends on frequency and dose of administration and how closely patients are followed up.
There was usually a lag time of 1 day between injection and postinjection flare present in 10% patients more commonly from chemical synovitis in response to injected crystals.
Treated with Analgesics and Ice Packs
Facial flushing is seen in 15% of patients, more in women subsides within maximum of 3–4 days. Skin and fat atrophy is reported to be approximately in 0.6% of patients. Effects lasted for approximately 6 months.
Joint sepsis of greatest concern, occurs very rarely due to strict asepsis maintained during procedure.
Other major concern is ruptured tendons after intratendinous injection which may accelerated degeneration of already damaged tissue.
Animals studies show deleterious effects of cartilage but not in humans.
Systemic Side Effects
Depends on agent used, dose, frequency and number of joints injected milder than other preparations.
Steroid can cause osteoporosis but intra-articular steroid has no effect on bone resorption and only a transient effect on bone formation.
Corticosteroid induced myopathy is also possible consequence but not reported after intra-articular injection. More common triamcinolone and dexamethasone suppression and hypothalamus pituitary adrenal axis is well documented but is mild and transient.
Prolonged hypothalamus pituitary axis suppression for 5–7 weeks after last injected has been reported, in one can accompanied by Cushing syndrome.
It can increase hepatic glucose synthesis and antagonize insulin effects resulting in worsening of glucose tolerance and increase in blood glucose transiently.
Structure Lesion Relationship
Tendon and tendon sheaths | Tendinitis, peritendinitis degeneration, rupture, tenosynovitis |
Tenoperiosteal junction | Enthesopathies, apophysitis |
Bursae | Acute and chronic bursitis |
Fasciae | Fasciitis, Dupuytren's contracture |
Ligament | Sprain and tear |
TRIAMCINOLONE ACETONIDE INJECTION
It has highly selective glucocorticoid activity and anti-inflammatory actions acetonide ester of triamcinolone is long acting for several days or weeks. Patients have prolonged remission of symptoms.
Most important mechanism is limitation of recruitment of proinflammatory leukocytes at affected site.
Triamcinolone is short acting plasma elimination half-life is 200 minutes and biologic elimination half-life is 18–36 hours.
It crosses placenta and secreted in breast milk. Its mean residence time after intra-articular injection is 4 days. with IM injections suppression of adrenal glands tends to occur within 24–48 hours gradually reversing over next 1 month.
By intra-articular, intrabursal route or in intratendon sheath is indicated as an adjuvant for short-term administration of acute exacerbation of: synovitis in osteoarthritis, acute and subacute bursitis, acute gouty arthritis, epicondylitis, acute nonspecific tenosynovitis and post-traumatic osteoarthritis.
Contraindications: Systemic fungal or viral infection, tuberculosis idiopathic thrombocytopenic purpura.
Not recommended for children less than 6 years not given intravenously, should not be given to nursing mothers, overuse of joint should be avoided, unstable joints should not be injected, it is associated with skeletal muscle atrophy so prolonged dose regimen should be avoided. There is a possibility of adrenal insufficiency.
In general, it is contraindicated in those with peptic ulcer, diabetes mellitus, other cardiovascular disorders, glaucoma, osteoporosis and infection also not recommended in those with myasthenia gravis, diverticulitis, thrombophlebitis, psychotic tendencies chronic nephritis, and metastatic carcinoma.
Dosage for smaller joints—20 to 40 mg dose is sufficient when given in large joint or multiple joints or peritendinous 80 mg should be the dosage, but not exceeding that.
Side effects—muscle weakness and fatigue, pain at injection site, transient pain, post injection flare, post injection discomfort, subcutaneous atrophy, hypo- or hyperpigmentation and Charcot like arthropathy.
Note: Intramuscular route can be useful for some disorders.
HYALURONIDASE
Each ampoule contains 1,500 international units of hyaluronidase comes as white powder for solution for injection/infusion. Hyaluronidase is used to enhance permeation of subcutaneous or intramuscular injections, local anesthetics and subcutaneous infusions and to promote resorption of excess fluids and blood in the tissues.
Adult Dosage
Adults, children and elderly: With subcutaneous infusion (hypodermoclysis), intramuscular injections, with local anesthetics: 1500 IU.8
Extravasation, hematoma: Where dispersal rather than localization is indicated.
Immediately before use dissolve the freeze-dried powder in approximately 1ml of water for injections or directly in the solution with which Hyalase® is to be combined.
Care should be taken to control the speed and total volume of fluid administered and to avoid over-hydration, especially in renal impairment.
Contraindications: Hypersensitivity to hyaluronidase, not to be used to reduce the swelling of bites or stings or at sites where infection or malignancy is present. Not to be used for anesthetic procedures in cases of unexplained premature labor.
Special precautions: Do not apply directly to the cornea, or intravenously.
Solutions for subcutaneous administration should be isotonic (0.9% sodium chloride, with 4% glucose) with extracellular fluid. Use in hypodermoclysis has been reported.
Adverse Reactions
Rare reports of periorbital edema occurring with the use of hyaluronidase in conjunction with local anesthetics in ophthalmology. Severe allergic reactions including anaphylaxis have been reported rarely. Local irritation, infection, bleeding and bruising occur rarely. Edema has been reported in association with hypodermoclysis.
It is defined as a volume of the plasma fraction of blood having a platelet concentration above baseline.
Autologous platelet rich plasma (PRP) was first used in 1987 by Ferrari et al
- Platelets release many growth factor responsible for attracting macrophages, mesenchymal stem cells, and osteoblasts.
- It promotes removal of necrotic tissue, and enhances tissue regeneration and healing. Growth factors stimulate recovery in non-healing injuries.
- Varying results are attributed to the need for additional standardized PRP protocols, preparations, and techniques. Although some authors have reported improved bone formation and tissue healing with PRP, others have had less success.
- Sample sizes are frequently small, there are few controlled trials. PRP has been found to be useful in chronic non-healing tendon injuries including lateral epicondylitis and plantar fasciitis and cartilage degeneration. It is an alternative to surgery by providing natural healing.
- Other uses include diabetic wound management, treatment of non-unions, and use in acute tendon injuries.
- Typically a blood specimen contains 93% RBC, 6% Platelets, and 1% WBC. The rationale for PRP is decreasing RBC to 5%, and increasing platelets to 94%.
- Platelets are made in bone marrow with a lifespan of 7–10 days. Inside the platelets are many intracellular structures containing glycogen, lysosomes, 9and two types of granules. The alpha granules contain the clotting and growth factors that are eventually released in the healing process. Normally they are at resting state. Upon activation by thrombin, platelets changes shape and develop branches, called pseudopods that spread over injured tissue (aggregation). Eventually the granules contained within platelets release growth factors. Alpha granules are storage units within platelets, which contain pre-packaged growth factors in an inactive form.
- Growth factors contained in these granules are platelet-derived growth factor (PDGF), stimulates cell replication, promotes angiogenesis, epithelialization, granulation tissue formation.
Transforming growth factor (TGF) promotes formation of extracellular matrix, regulates bone cell metabolism.
Vascular endothelial growth factor (VEGF) promotes angiogenesis.
Epidermal growth factor (EGF) promotes cell differentiation and stimulates, re-epithelialization, angiogenesis and collagenase activity.
Fibroblast growth factor (FGF) promotes proliferation of endothelial cells and fibroblasts stimulates angiogenesis.
Vitronectin is a cell adhesion molecule which helps with osseointegration and osteoconduction.
- It is prepared by centrifuging blood for 15 minutes at 3,200 rpm, it is spread in a clock-like manner to achieve a more extensive zone of delivery.
- Patients may experience minimal to moderate discomfort following the injection which may last for up to 1 week. This is likely due to the stimulation of the body's natural response to inflammatory mediators.
- No studies have documented that PRP promotes hyperplasia, carcinogenesis or tumor growth. Growth factors act on cell membranes rather than on the cell nucleus and activate normal gene expression. Growth factors are not mutagenic and naturally act through gene regulation and normal wound healing feedback control mechanisms.
- Relative contraindications include the presence of a tumor, metastatic disease, active infections, or platelet count/10.5/ul/Hgb/10 g/dl, pregnancy or active breastfeeding.
- Although adverse effects are uncommon, they are infection, no relief of symptoms, and neurovascular injury. Scar tissue formation and calcification at the injection site are also rare risks.
- Taylor et al demonstrated safety and efficacy while injecting autologous blood in white rabbits at the patellar tendon.
- Berghoff et al retrospectively reviewed patients to access autologous blood product effects in patients undergoing total knee arthroplasty (TKA). The study included 66 control and 71 treated with autologous blood products at the wound site.
- Everts et al reviewed 160 patients, who undergoing total knee replacements (TKR), in which 85 received PRP with sealants; which resulted in decreased blood transfusion requirements, lower postsurgical wound disturbances, shorter hospital stay, and fewer infections.
- Crovetti et al reviewed 24 patients with chronic cutaneous ulcers, who were treated with a series of PRP Gel treatments, 9 patients demonstrated complete wound healing 2 patients had wound infection, both with positive Staphylococcus aureus which were positively treated with oral antibiotics.
In a recent study by Ranly et al, PRP was shown to decrease osteoinductivity of demineralized bone matrix in immunocompromised mice. The timing of the assays looking at osteoinduction may have been too late to accurately access early bone formation.
McAleer et al involved 24 patients with 33 chronic non-healing lower extremity wounds. Patients failed conservative treatment judged by lack of reduction of surface area. Surgical wound debridement was initially performed to convert chronic ulcers to acute wounds, in an effort to promote wound metabolism and chemotaxis wound closure and epithelialization was obtained in 20 wounds. The mean time for closure was 11 to 15 weeks. There was No improvement in 5 wounds.
Diabetes impairs fracture healing with reduced early proliferation of cells, delayed osteogenesis, and diminished biomechanical properties of the fracture callus. Platelet rich plasma (PRP) shows favorable results in these.
Barett et al evaluated nine patients given PRP injections for plantar fasciitis in which 6 of 9 patients achieved complete symptomatic relief after 2 months. At 1 year 77.9% patients had complete resolution of symptoms. Again, this was a non-controlled study with a small sample size.
Kajikawa et al showed that there was increased quantity of circulation-derived cells in the early phase of tendon repair after injury versus controls study in the American Journal of Sports Medicine. Mishra et al evaluated 140 patients with chronic epicondylar elbow pain, treatment group noted 60% improvement at 8 weeks, 81% at 6 months, and 93% at final follow-up at 12–38 months. Additionally, there was a 94% return to sporting activities and a 99% return to daily activities.
In 2003 Edwards and Calandruccio, demonstrated that 22 of 28 patients (79%) with refractory chronic epicondylitis were completely pain free, following autologous blood injection therapy. This study is limited by its small sample size and lack of control group.
A study from Chen et al demonstrated that PRP might potentially play a role in prevention of disc degeneration maintaining arthrodesis in a posterolateral lumbar fusion can be challenging and may necessitate revision. Screw instrumentation, interbody fusion, bone morphogenic protein was employed in an attempt to promote arthrodesis also limiting risk factors such as smoking, NSAID and corticosteroid use are recommended. Platelet rich plasma (PRP) is not of much help in this was shown by few authors. Lowery et al retrospectively reviewed 19 spinal fusion patients with PRP after 13 months. There was no pseudoarthrosis seen on exploration or plain radiographs in 100% of cases.
Hee et al evaluated 23 patients treated by instrumented transforaminal lumbar interbody fusions with PRP versus control with a 2-year follow-up. They found accelerated bony healing in the PRP group.
Jenis et al explored anterior interbody lumbar fusions in 22 patients with autograph using iliac crest bone graft versus 15 patients with allograft combined 11with PRP at 12 and 24 months demonstrated an 85% fusion rate for autograft versus 89% with PRP and allograft.
Classification of soft tissue rheumatism | |
Localized | Generalized |
Epicondylitis | Myofascial pain syndrome |
Enthesitis | Chronic fatigue syndrome |
Tendinitis | Psychogenic rheumatism |
Tenosynovitis | |
Bursitis | |
Capsulitis | |
Ganglion | |
Periarthritis | |
Rotator cuff syndrome | |
Fasciitis | |
Dupuytren's contracture | |
Regional myofascial pain | |
Common sites of lesions | |
Shoulder | Rotator cuff disorders, capsulitis of joint |
Elbow | Lateral and medial epicondylitis, olecranon bursitis |
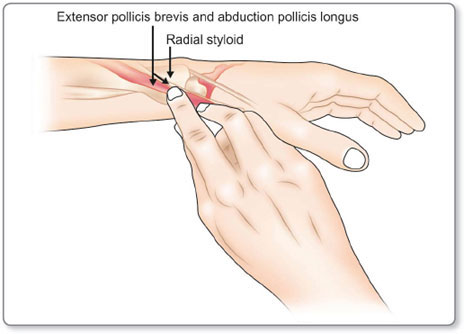
Wrist and hand | Carpal tunnel syndrome, Dupuytren's contracture, de Quervain's tenosynovitis |
Trunk | Costochondritis, trapezitis, nonspecific neck and low back pain |
Hip | Ischial and trochanteric bursitis, meralgia paresthetica |
Knee | Bursitis and ligament sprain |
Ankle and foot | Achilles tendinitis, peritendinitis, plantar fasciitis, bursitis around calcaneus |
Noninflammatory arthritis | Inflammatory arthritis |
Osteoarthritis | Rheumatoid arthritis |
Trauma | Ankylosing spondylitis |
Internal derangement | Crystal induced arthritis |
Osteochondritis dessicans | Psoriatic arthritis |
Charcot's arthropathy | Reactive arthritis |
Villonodular synovitis | Polymyalgia |
Acromegaly | Behcet's syndrome |
Sickle cell disease | Leukemia |
Lyme disease |
Viscosupplementation with hyaluronan intra-articularly can provide symptomatic relief for several months when given weekly with less side effects (approximately 8%). It has shown to have reduced disease progression as evident by arthroscopy. It is effective in those with high intra-articular aggrecan fragment concentration, i.e chondrocyte residual activity remains.12
Hyaluronic acid is an important glycosaminoglycans component. It is an important ground substance of synovial fluid and vitreous of eye. Its concentration is high in embryonic tissue and is thought to play a role in permitting cell migration during morphogenesis and wound repair. It has ability to attract water in extracellular matrix thereby loosening it up. Along with chondroitin sulfate is important part of cartilage.
INTRA-ARTICULAR ASPIRATIONS
Indications
- Rheumatoid arthritis
- Osteoarthritis
- Ankylosing spondylitis
- Psoriatic arthritis
- Lupus erythematosis
- Traumatic arthritis.
Contraindications
Charcot's arthropathy, local sepsis, hemophilia, avascular necrosis of cartilage.
Complications
Septic arthritis, Charcot's arthropathy, traumatic arthritis, avascular necrosis.
SYNOVIAL FLUID (FIG. 1.5 AND FLOW CHARTS 1 AND 7 OF ANNEXURE)
- It is ultrafiltrate of plasma to which proteoglycan is added by local synthesis by joint tissue contents are 96% water and 4% solutes
- Gross appearance: clear pale yellow viscous does not clot-absent fibrinogen
- Intra-articular pressure: 8 to 12 cm of water
- Bacteriologically sterile
- Specific gravity:1.008 to 1.015, with PH 7.3 to 7.6 (decreased in OA and trauma). Viscosity depend on concentration of hyaluronic acid (decreased in aging, OA and trauma)
- Cytology: average 65 cu/mm, mostly lymphocytes and monocytes
- Protein: about 2 gm/dl with 2/3 albumin mucin and globulin, the A/G ratio is 20:1
- Mucin is responsible for viscosity with average 235 at 38°C ranges from 5.7 to 1160
- For cytology methylene blue is added to the saline and nucleated cells are stained. Differential count is done on dried smears stained with Wright's stain mucus, amorphous deposits stains deeply basophilic
- Protein measured by electrophoresis method
- Mucin and viscosity: known as Rope's test
- Synovial fluid hyaluronate concentration: this test lacks specificity but bears correlation with presence or absence of inflammation, finding is nonspecific and alone is not diagnostic of single pathology.
Equal amount of fluid and 5% acetic acid added on glass slide—normal fluid produce long strings, inflammatory fluid produce short strings.
Reference range—mucin clot positive (firm clot).
Ultrasonographic Appearance of Tendons (Figs 1.6 and 1.11 and Flow chart 2 of Annexure)
Ultrasound usage: Use highest frequency available, use linear array transducer, avoid improper angling of probe to avoid false hypoechogenicity, combine longitudinal and transverse at same site, check contralateral tendon for reference, perform dynamic examination, use color from for Doppler imaging.
Machine of USG is compact and cost effective. Its use was most significant in
specialities outside radiology profession.
- There is interobserver variability depend on number of years, number of cases per year and quality of training.
- Limitation: Inability to penetrate beyond bony cortex, also true for intra-articular structures as cruciate.
- Real time examination and visualization of needle helps in giving USG guided injections.
- Tendons consist of linear fibrils of collagen with a supporting matrix fibrils are oriented in direction specific to forces applied to tendon, its vascularity is also important. Tendon show increase echogenicity and oval in cross section. It is used for conditions like tennis elbow and golfer elbow for identifying common extensor and flexor origin over humerus.
- Long tendons running in osseofibrous canals are surrounded by fluid filled synovial sheath which facilitates free tendon movements. Long tendons which are not surrounded by synovia lie within a vascularized loose areolar and adipose tissue.
- Fluid in synovial sheath is visible as thin hypoechoic rim surrounding the hyperechoic tendon.
- Tendons may be surrounded by synovial sheath or dense connective tissue which appears echogenic and can be differentiated from tendon by thin hypoechoic boundary.
- All normal tendons are highly echogenic they show fine parallel longitudinal echoes resembling fibrils. These echoes correspond to endotendinium septa running within the tendon. As frequency increase these fibrils becomes distinguish.
- The attachment of tendons to their muscles appear as a crowding of muscular fibers with rapid reduction of volume of muscle.
- Nerve is less echogenic than tendon. This phenomenon can be used in identifying carpal tunnel and median nerve in it. Normal ligaments appear 14hyperechoic with compact echotexture at USG. Individual nerve fascicle show honeycomb appearance, nerve fascicle appear hypoechoic and surrounding hyperechoic connective tissue element.
- Examiner should hold the transducer near its footprint and spread the other fingers out to stabilize the transducer on skin.
- Excessive transducer pressure and tendon tension can compress and artificially eliminate neovascularity.
Ultrasonography is reliable for tendon sheath or peritendinous injections while avoiding on intratendinous injections which are associated with tendon weakening and possible rupture.
Anisotropy is hypoechoic appearance of tendon due to angulation of transducer. Anisotropy is beneficial in confirming tendon position because artifact can be produced in normal linear tendon surrounded by nonlinear echogenic fat. Slight obliquity of the angle of incidence results in hypoechoic appearance which mimics tendon disease.
Active and passive movements can be used for dynamic evaluation of all tendons for tear severity and look for abnormal movement due to subluxation and adhesive tenosynovitis.
A linear multifrequency 9–15 MHz transducer is used for superficial structures; and 5 MHz transducer for deep structures. Structures should always be evaluated in their orthogonal planes for a focal soft tissue abnormality. Advantages: patient interaction, enabling a detailed history and direct correlation with findings from physical examination and perform a dynamic evaluation. Color and Doppler ultrasound helps to diagnose vascular abnormalities.
For a full dynamic assessment, muscles and tendons are evaluated while in a contracted and relaxed state. Knowledge of origin and insertion allows correct identification of tendons. Placing limb in different positions to stretch structure under evaluation is important. Tendons surrounded by fat, that appear hyperechoic. By gently angulating the probe, tendon ligaments will show anisotropy and become hypoechoic, thus allowing visual differentiation from surrounding fat. While holding transducer, the edge of the hand or fifth finger is in contact with patient for stabilization of the transducer and to allow fine controlled adjustments in transducer position.
- Muscle fiber group makes fascicles which are separated by perimysium. On whole, muscle is covered by epimysium.
- In transverse orientation of transducer to muscle, perimysium is seen as dot/ short line in hypoechoic background of muscle fibers. Inter and intramuscular septa produce reticular pattern and increased echogenicity.
- In longitudinal scan perimysium shows obliquely parallel echogenic striae against hypoechoic background. Intramuscular extension of tendon—which is thick fribrillar and echogenic. Intermuscular fascia are bright and echogenic.
- Contraction produce hypoechogenicity with increase angulation of echogenic septa.
- Acute lesions are strains, tears, contusion, hematoma. Chronic lesions—fibrous scars, hernia, calcification.Ultrasonography signs of tendon tear are
- Tendinitis—altered echogenicity, blurred margins, calcification in chronic tendinitis, tendon thickening, vascularity (color Doppler).
- Tendon without synovial sheath like Achilles tendon are surrounded by homogenous hyperechoic tissue within which it can move more freely.
- Synovial bursae are hypoechoic elongated areas, which are rarely thicker than 2–3 mm.
- In chronic bursitis there is illdefined margins, complex appearance with internal echogenic debris due to fibrin and microcalcifications. Color Doppler shows increased vascularity and thickened wall.
- Ultrasound detect minor changes of tendon echotexture which predispose tendon to rupture, these can be recognized as focal enlargements of involved tendon.
- Avulsion of tendon due to force applied to insertion of tendon usually involves tibial tuberosity, ischial tuberosity and iliac crest. When avulsion is incomplete, ultrasonography shows V shaped image at site of lesion with slight irregular adjacent bony surfaces.
- Tendons may be enclosed in synovial sheath (wrist and ankle) or paratenon (patellar/Achilles tendon) many have adjacent bursae (rotator cuff/illiopsoas) overuse cause fluid in these structures before tendon abnormalities are seen. Ultrasonography diagnosis of tenosynovitis should be made if inflammatory changes are located to sheath and joint effusion is excluded.
- In peritendinitis the peritenon becomes hypoechoic and thickened, tendon remains grossely unaffected. Peritendinous inflammation occurs in setting of adjacent tenosynovitis or bursitis. It is also use to assess the response to treatment overtime.
- Tendinosis manifest as alteration of echogenicity.
- In tenosynovitis inflammation of tendon sheath fluid in the sheath may be seen with minimal quantity. In chronic tenosynovitis there may be impairment of movement of tendon. Doppler shows increased vascularity of tissue.
- In inflammatory conditions there is thickening of involved tendon whose structure will become heterogenous with alternating areas of hypo or hyperechoic representing degenerative and fibrotic changes.
- Tendinosis can also manifest as angiofibroblastic response presence of hyperemia may help to localize the areas of tendon that may respond to intratendinous and peritendinous steroid/anesthetic agents.
- There may be cortical erosion seen and microcalcification at insertion seen.
- In transverse images of tendon if inflamed, hypoechoic fluid surrounding hyperechoic tendon sheath can be seen. Thickening of peritendon and adhesions, nodules heterogeneity and irregularity can be seen.
- In degenerative conditions tendons show enlargements, irregularity in texture, small hypoechoic areas within tendon body and associated diffuse or focal microcalcification, scar, granulation tissue may be seen, predisposition of tendons for rupture can be found as altered echotexture. Tendon sheath may be hypoechoic in rheumatoid arthritis, initially there is marked thickening of tendon and then there is marked thinning.
Fibrous scar can lead to further tear extension in superimposed on injuries. Scar is hyperechoic/heterogenous, linear/stellate adherent to epimysium. Lesion does 16not change with muscle belly. Myositis ossification shows coarse calcification in hypoechoic mass similar to adjacent diaphysis.
If tendon is seen with jagged margins, degenerative changes in tendon is termed tendinosis.
- Dystrophic calcification can be identified, focal calcified masses are seen.
- Additional changes can be seen as focal or diffuse thinning of tendon.
Complete tears often diagnosed due to presence of gap of varying length. When torn, fragments are separated by large distance, tendon may not be visible at all. Example rotator cuff tear or tear of flexor tendon of finger.
In complete tears of tendon, the ends of retracted tendons can present as focal mass. USG shows swollen hypoechoic irregular ends of tendon with surrounding effusion. Color Doppler shows local hypoechoicity in acute tears.
Ruptures are associated with minimal focal hemorrhages.
Recent partial ruptures appear hyperechoic defects in tendon or its attachment. Increased vascularity can be seen in inflammatory conditions of tendon sheath in color Doppler, there is thickening of tendon sheath and reduced echogenicity in partial/complete tears.
Tears are most commonly associated with background tendinopathy, which weakens the tendon. Chronic tear/relatively minor injury precipitate complete tear.
- Tendon margins can be separated by fluid, hematoma, herniated adjacent tissue. There is separation of torn margins with dynamic movement. USG is also helpful in diagnosing other similar conditions and associated injury to other structures.
- Note: Fluid could be found in asymptomatic tendon thickening.
- Associated microcyst and increased volume of tendon results in calcification, focal involvement may be seen.
- In acute muscle injury muscles fibers show increase flow on Doppler. musculotendinous junction is most common site of overstretch grade 1 muscle strain—rapid recovery with no loss of power and function.
- Ultrasonography: normal/focal increased echogenicity up to 50% show generalized hyperechogenicity, this should be differentiated by delayed onset muscle edema—geographic hyperechogenicity, symptom increase after first 24–48 hours and peak at day 3 and reduce at day 7.
- Grade 2 intrasubstance tear—presents as pain and loss of function, USG shows discontinuity, perimyseal striae, intramuscular fluid surrounding hyperechoic halo. Dynamic scanning shows increased size and contrast of lesions. In this grade there might be partial detachment of muscle from aponeurosis. Grade 3—complete myotendinous/tendo-osseous avulsion. USG shows complete discontinuity of fibers and hematoma.
- Gouty tophi are echogenic with posterior acoustic shadowing in patients with rheumatoid arthritis joint changes are marked. For examination of joints, USG should be done in static and dynamic phases and simultaneously comparing it with opposite side.
- Fibrocartilage is hyperechoic (Fig. 1.7).
- Subcutaneous fat has variable and heterogenous (internal reflective echoes) appearance.
- During Doppler examination tendon should be in position relaxed contrary to tensed position in which tendons are evaluated for tears and tendinopathy.
- Tendinopathy can also be caused by external impingement. Normal tendons do not exhibit neovascularity, these findings are associated with severe symptoms.
- Tenosynovitis can present as mass in significant synovial hypertrophy and thickening of retinacula, excessive local pressure with transducer can displace fluid and lead to false diagnosis.
- Harmonic imaging results in improved axial resolution and diminished near field artifact. Spatial compounding results in speckle reduction of inherent haziness seen in ultrasound images.
- Traumatic stump neuroma is disorganized proliferation of nerve fascicle after amputation/regeneration (Fig. 1.1).
- Stump neuroma is painless/cause pain nonresponsive to conservative management, steroid can be helpful in reducing inflammation and loosening the connective tissue that surrounds and compromises the nerve.
- Intramuscular phenol or botulinum toxin type A peri and intraneural decrease pain, phenol decreases focal swelling after intra/extrafasicular/intraneural injection and cause severe demyelination, axonal degeneration, edema and hemorrhage leading to architectural nerve disruption.
- Glycerol is useful but highly viscous.
- Alcohol is slowly acting more irritating and cause painful neuritis.
- Neuromas had average maximal diameter 7.15 mm.
- Twenty-one gauge needle is advanced towards nerve and slightly proximal to stump neuroma, if there is complete cessation of pain after injection identification of pain causing neuroma was successful.
- Local anesthesia is given proximal to nerve. Same needle is advanced into nerve proximal to neuroma under vision and used to inject phenolic solution. When injection of nerve is successful, swelling is observed in USG.
Phenol can cause slight burning pain (so needle is flushed with saline to avoid spreading). Shape of neuroma does not change but pain decreases.
Intraneural axonotmesis chemically impair and destroy peripheral neural tissues and does not damage surrounding tissues.
Note: In various chapters emphasis is given on identifying the concerned structure on ultrasound. Reader must see the needle (which appears hyperechoic) extending from skin to concern structure and inject under USG guidance.18
FURTHER READING
- Adler RS, Sofka CM. Percutaneous ultrasound-guided injections in the musculoskeletal system. Ultrasound Quarterly. 2003;19:3–12.
- Adler R, Swanson S, Doi K, et al. The effect of magnetization transfer in meniscal fibrocartilage. Magn Reson Med. 1996;35:591–5.
- Adler RS. Future and new developments in musculoskeletal ultrasound. Radiol Clin North Am. 1999;27:623–31.
- Barberie JE, Wong AD, Cooperberb PL, et al. Extended field-of-view sonography in musculoskeletal disorders. AJR Am J Roentgenol. 1998;171:751–7.
- Beltran J, Noto AM, Herman LJ, et al. Tendons: high field strength surface coil imaging. Radiology. 1987;162:735–40.
- Bouffard JA, Eyler WR, Introcaso JH, et al. Sonography of tendons. Ultrasound Quarterly. 1993;11:259–86.
- Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis. 1984;43:353–60.
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics. Vol 1. Mosby Inc. eleventh edition. 2008:885-905.
- Cardone DA, Tallia AF. Joint and soft tissue injection. Am Fam Physician. 200266283–101. 8,290.
- Dacre JE, Beeney N, Scott DL. Injections and physiotherapy for the painful stiff shoulder. Ann Rheum Dis. 1989;48:322–5.
- Elliott DH. Structure and function of mammalian tendons. Biol Rev. 1965;40:392–421.
- Fredberg, U. Local corticosteroid injection in sport: review of literature and guidelines for treatment. Scand J Med Sci Sports. 1997;7(3):131–9.
- Gottlieb NL, Riskin WG. Complications of local corticosteroid injections. JAMA. 1980;243:1547–8.
- Hamilton JH, Bootes A, Phillips PE, Slywka J. Human synovial fibroblast plasminogen activator. Modulation of enzyme activity by anti-inflammatory steroids. Arthritis Rheum. 1981;24(10):1296–403.
- John O' Neill. Musculoskeletal Ultrasound: Anatomy and Technique. Springer Inc. 2008:20-330.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. Edition 1. 2007:25-112.
- Klippel JH, Weyand CM, Wortmann R. Primer on the Rheumatic Diseases. 11th ed. Atlanta: Arthritis Foundation. 1997:420.
- Koblik PD, Freeman DM. Short echo time magnetic resonance imaging of tendon. Invest Radiol. 1993;28:1095–100.
- Lauzon C, Carette S, et al. Multiple tendon rupture at unusual sites in rheumatoid arthritis. J Rheumatol. 1987;14(2):369–71.
- Lin DC, Nazarian LN, O'Kane PL, et al. Advantages of real-time spatial compound sonography of the musculoskeletal system versus conventional sonography. AJR Am J Roentgenol. 2002;179:1629–31.
- Nelson KH, Briner W Jr, et al. Corticosteroid injection therapy for overuse injuries. Am Fam Physician. 1995;52(6):1811–6.
- Nichols AW. Complications associated with the use of corticosteroids in the treatment of athletic injuries. Clin J Sport Med. Sep 2005;15(5):370–5.
- Rifat SF, Moeller JL. Site-specific techniques of joint injection. Useful additions to your treatment repertoire. Postgrad Med. Mar 2001;109(3):123-6, 129-30, 135-6.
- Rumack C, Wilson S, William J. Diagnostic Ultrasound. 2nd edition, Mosby Inc. 1998:843-83.
- Solbiati L, Rizzatto G. Ultrasound of Superficial Structures. 1st edition. Churchill Livingstone. 1995:279-375.
- Tillander B, Franzen LE, Karlsson MH, Norlin R. Effect of steroid injection of the rotator cuff: An experimental study in rats. J Shoulder Elbow Surg. 1999;8:271–4.
- W Watson Buchaman, Géza Bálint, Karel de Ceulaer. Clinical Examination of the Musculoskeletal System. Williams and Wilkins. 1st Edition. 1997. pp. 25-82.
- Wen-Chung tsai, Fuk-Tan Tang, May-Kuen Wong, Jong-Hwei S Pang. Inhibition of tendon cell migration by dexamethasone is correlated with reduced alpha-smooth muscle actin gene expression: a potential mechanism of delayed tendon healing. J Orth Res. 2003;21:265–71.
- Winters JC, Jorritsma W, Groenier KH, Sobel JS, Meyboomde Jong B, Arendzen HJ. Treatment of shoulder complaints in general practice: long-term results of a randomised, single blind study comparing physiotherapy, manipulation, and corticosteroid injection. BMJ. 19993181395–6. Syst Rev. 2006 Jan 25;(1):CD002824
- Yasher AA, Adler RS, Grady-Benson JC, et al. Ultrasound method to evaluate polyethylene component. wear in total knee replacement arthroplasty. Am J Oilhop. 1996;25:702–4.
Structures defining subacromial space are
- Acromion
- Subdeltoid bursa
- Coracoacromial ligament
- Supraspinatus tendon
Shape of acromion affects the subacromion space and is a contributor to impingement.
Spine of scapula and scapula blade are very important landmarks for identification of various other bones. Clavicle on anterior aspect is also very prominent. Both clavicle and spine of scapula can be palpated as continuous bony structure as a common having at its anterior aspect acromioclavicular articulation and acromion has posterolateral corner. Acromioclavicular articulation is easy to palpate due to slight protrusion of clavicle over acromion and this joint moves with shoulder.
Serially greater tuberosity of humerus is palpated which lies lateral to lateral border of acromion.
The bicipital groove is located anterior and medial to the greater tuberosity and is bordered laterally by greater tuberosity and medially by lesser tuberosity. The tip of the coracoid process projects from scapula forward, laterally, and inferiorly toward the glenoid cavity.
Lesser tuberosity and coracoid process lie at same level. 1 inch distally from the anterior edge of clavicle lies the coracoid process which is palpated by pressing 25laterally and posteriorly in an oblique line.
This process faces anterolaterally. Its medial surface and tip are palpable which may be felt, if pressed firmly into the deltopectoral triangle.
The deltopectoral groove is easier to see than to feel.
Biceps brachii originates with two heads in which short head from tip of coracoid process and long head from supraglenoid tubercle of scapula and inserted to bicipital tuberosity of radius. Its action is flexon of elbow and supination of forearm, it is weak flexor of shoulder. It is supplied by, musculocutaneous nerve.
The shoulder joint capsule bridges the gap across the bicipital groove, forming a structure known as the transverse ligament.
Subscapularis originates from medial four fifths of anterior surface of scapula and inserted to lesser tuberosity of humerus. Its action is internal rotation of humerus supplied by upper and lower subscapularis nerves.
Supraspinatus originates from medial three fourths of supraspinous fossa of scapula and inserted into upper facet of greater tuberosity of humerus. Its action is initiation of abduction of shoulder supplied by suprascapular nerve.
Teres minor originates from axillary border of scapula. Inserted to greater tuberosity of humerus. Its action is lateral rotation of humerus which is supplied by axillary nerve.
Infraspinatus originates from medial three fourths of infraspinous fossa of scapula and inserted on central facet on greater tuberosity of humerus. Its action is lateral rotation of humerus which is supplied by suprascapular nerve.
The acromion is lateral continuation of spine of the scapula, bursa lies between the supraspinatus and deltoid muscles, and between supraspinatus and coracoacromial ligaments. Bursa extends anteriorly from beneath the coracoid process.
When arm is abducted, bursa retreats under the cover of this ligament. At this point, patient feels pain if there is inflammation of bursa.
Passive extension of the shoulder also brings the bursa out anteriorly from beneath the acromion and makes it palpable. Normally there is space of 1.5 cm between bony components of glenohumeral joint and acromion, however, on abduction upper end of humerus would tend to impinge on arch at about 90° abduction.
Abduction of the arm may pinch the supraspinatus muscle between head of humerus and the arch created by acromion and coracoacromial ligament.
Note: In general, for palpation of muscle it is important to palpate from its insertion. So, it is essential to know its anatomy.
Since, rotator cuff lies directly below acromion it must be rotated out from underneath. It can be palpated with passive extension of shoulder and rotation which brings subacromial bursa into palpable position, done by holding patient's arm across just proximal to elbow joint and lifting it posteriorly. Subacromial bursa can be palpated if distended.29
Subdeltoid bursa gets inflamed more often than any other bursa. Inflammation is secondary to tendinitis of rotator cuff muscles.
Subacromial injections are used in adhesive capsulitis, subacromial bursitis, impingement syndrome, rotator cuff tendinosis.
It is seen that subacromion burse injections are effective for rotator cuff tendinitis for up to 9 months (its more effective than NSAIDs). Subacromial space injections should be considered after other intervention such as NSAIDs, physical therapy and activity modification have been tried.
Subdeltoid bursitis can sometimes be confused with neoplasms. So, MRI or bursography can be useful at that time.
Chung Ming Yu, Chin Yuwa et al had injected, 238 shoulders in 209 patients (having impingement syndrome) corticosteroid in subdeltoid bursa. Mean duration of symptoms was 5 months and mean age of patients was 51 years.
Fig. 2.11: Subacromial bursa on ultrasonography. The arrow shows left subacromial-subdeltoid (SASD) bursa
Fig. 2.12: Subacromial bursitis ultrasound. The arrow shows left subacromial-subdeltoid (SASD) bursa
Fig. 2.24: Schematic representation: ultrasonographic appearance of rim rent sign and cartilage interface
Injection was given at interval of 1 week, 91% of these patients had satisfactory pain improvement and range of motion also improved. About 8% had recurrence (these had partial/ complete rotator cuff tears).
Kessel and M Watson et al had in their study of 97 patients with painful arc syndrome showed usefulness of subacromion injection.
In rotator cuff tendonitis, pain is usually felt to front or outer side of shoulder and is worse when arm is used overhead and out to the side. Arm may feel heavy and tire easily, shoulder may also become stiff such that placing the hand behind head on back becomes difficult.
Impingement occurs beneath coracoacromial arch. Major site of compression is slightly anterior to acromion.
According to Neer's stages, injection techniques are affective up to stage of tendinitis and fibrositis and not much after bony changes or tear already occurs.
Rotator cuff tears are seen in throwers, swimmers, tennis players, etc.
It is also seen in degenerative conditions and patients with dislocation.
Patients usually present with painful arc sign and tenderness over greater tuberosity.
In grade I, rotator cuff tears characterized by young age of 18–30 years in which impingement with inflamed supraspinatus is present and degenerative changes are not present.
Ultrasound has 98% sensitivity in diagnosing cuff tears.
Mosts people with cuff tears are > 40 years. Patients will have previous history of trauma.
Hyaluronan injection have been proven to be as effective as corticosteroid for treatment of impingement syndrome and rotator cuff disease without complications associated with corticosteroid.
Local steroid and anesthetics failed to gain significant relief from symptoms of patients who had supraspinatus tendon lesion and degeneration of acromioclavicular joint, and those who had lesion in anterior part of subscapularis, with or without posterior part of subscapularis.
Rotator cuff tendinopathy is caused by intrinsic, extrinsic, and environmental factors. Profound changes in subacromial bursa are strongly related to the pathology of rotator cuff. Cuff pain as described by J lewis as pain located about 3 cm below the top of shoulder and felt when reaching overhead behind back. Tendinitis or more properly tendinosis, i.e. acute or chronic stress of rotator cuff tendons with repetitive overhead recurring activity leads usually to impingement syndrome.
Steroid injected in subacromial bursa show improvement over the placebo in painful shoulder has been described by Michelle Petri et al in 1987. It is also useful in diagnosis of impingement syndrome by eliciting Neer impingement sign.35
In subacromial bursitis—tendon and bursa lies in space between acromion and head of humerus can be impinged, all range of motion is affected but internal rotation is affected the most individual tends to hold arm against chest wall.
Indications: Intrabursal injections are shown to be effective for partial tears of rotator cuff especially bursal surface, more when patients are in painful stage and during rehabilitation period and during early periods of shoulder stiffness. Since intratendinous injections (in partial tears or tendonitis) of steroids are harmful we want to inject it at exact site, ultrasound is most useful of this technique. It is also helpful when patient is at very high risk for surgery and shoulder joint is very painful.
Technique
Posterior Approach
Easier and safe.
Position: Sitting.
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 to 60 mg of methylprednisolone. Syringe: 5 ml 1 ½ inch 25 gauge needle.
Entry point is 1 cm inferior and medial to posterior corner of acromion (posterolateral edge of acromion). It is site where soft spot is felt. Needle is directed upwards and medially or towards coracoid palpated with other hand. The solution should flow freely in space without resistance/discomfort, repeat injections at 4–6 weeks interval. If no benefit then consider other treatment.
Caution: Injecting under pressure may damage tendon.
Lateral Approach
Position: Sitting.
Preparation: Same as above.
Drugs and syringe: Same as above.
Palpate most lateral point of shoulder and make marking at 2 inch. Below the tip of acromion. Steroid and local anesthetic mixture is advanced with needle medially below the acromion horizontally and slightly posterior along line of supraspinous fossa.
ULTRASONOGRAPHY GUIDED INJECTION (FLOW CHART 2.1 AND FIGS 2.9 TO 2.20)
Subscapularis muscle is a multipennate large triangular muscle arising from the subscapularis fossa of scapula and insert onto lesser tuberosity. It is separated from the neck of scapula by subscapularis bursa. As the long head of biceps courses within the intertubercular groove, it is surrounded proximally by the bicipital sheath, a synovial recess of the glenohumeral joint.
Within bicipital groove, the long head of the biceps tendon is held in place by transverse humeral ligament proximally and by a fibrous extension of pectoralis 36major distally. Transverse humeral ligament is a continuation of fibers from subscapularis tendon. The supraspinatus tendon and coracohumeral ligament send fibers, deep to superficial band of subscapularis, which form the roof of bicipital groove inferiorly, roof of the groove is maintained by pectoralis major tendon. Infraspinatus muscle is single or multipennate. The teres minor is a smaller, elongated muscle in close contact with the infraspinatus, arising from the infraspinatus fascia and the axillary border of scapula. It has a short tendon, that inserts onto the posterior facet of the greater tuberosity and adjacent humerus. The coracohumeral ligament is composed of two bands extending from base of the coracoid process to the lesser and greater humeral tuberosities. The pectoralis major muscle tendon is broad and bilaminar, rotator cuff tendons measure between 5 and 10 mm in thickness and the biceps less than 5 mm.
The subacromial-subdeltoid (SASD) bursa attached to periosteal undersurface of the acromion. It extends laterally beyond the attachment of the rotator cuff by up to 3 cm, medially to the acromioclavicular joint, anteriorly overlie the bicipital groove, and posteriorly over the rotator cuff. Two opposing hyperechoic layers formed by fibroadipose tissue and capsule with an intervening hypoechoic layer representing the viscous fluid within the bursa. Bursa normally measures less than 2 mm in thickness.
The subcoracoid bursa may communicate with subacromial-subdeltoid (SASD) bursa.
The rotator cuff interval is a triangular space between subscapularis and supraspinatus tendons. Base is formed by the coracoid process and the apex by the transverse humeral ligament. It is a dynamic space whose area decreases significantly in internal rotation, less so in external rotation, and is maximal in neutral position. Long head of the biceps passes through the interval, separated from the supraspinatus and subscapularis by up to 3 mm. Overlying the interval, from superficial to deep, is skin, subcutaneous tissue, deltoid muscle, a fibrofatty layer, coracohumeral ligament, joint capsule, superior glenohumeral ligament, and long head of biceps tendon. This ligament is triangular with the base attached to the lateral coracoid margin and apex attached to anterior margin of the acromion. Deep to coracoacromial ligament lie supraspinatus, superior aspect of subscapularis tendon, and anterior fibers of infraspinatus tendon. An articular fibrocartilage disc is usually present, although it may often be incomplete. This joint is further supported by two additional ligaments, coracoclavicular and coracoacromial ligaments, which do not belong to the acromioclavicular joint. Former is composed of two ligaments, conoid and trapezoid, which extend between lateral aspect of the clavicle and coracoid process of scapula. The trapezoid attaches to oblique line on inferior aspect of the clavicle. Conoid component extends from the base of coracoid to conoid tubercle on clavicular undersurface.
Labrum is composed of fibrous tissue, hyaline cartilage, and fibrocartilage and forms a rim around the glenoid. It serves as a site of attachment for the glenohumeral ligaments. It is supported by the acromioclavicular (AC) ligaments: anterior, posterior, inferior, and superior. Strong superior AC ligament interlaces with fibers from overlying deltoid and trapezius. Weaker inferior ligament and joint are in 37direct contact inferiorly with subacromial-subdeltoid bursa (SASD). Affection of suprascapular nerve at or below spinoglenoid notch affects infraspinatus muscle. Teres minor muscle is supplied by the axillary nerve. Examiner can either sit or stand in front or behind the patient.
The long head of the biceps tendon and sheath are evaluated in a neutral position with arm in supination resting on ipsilateral thigh. Bicipital groove faces anteriorly on longitudinal view, fibrillar pattern of the biceps tendon appears hypoechoic in part, but by gently pressing on inferior aspect of the transducer the fibrillar pattern will, in normal tendons, become homogeneous. A dynamic examination is performed with internal and external rotation of shoulder, maintaining the elbow by side, to assess the integrity of transverse humeral ligament and for biceps tendon subluxation. The superior intra-articular portion of the long head of biceps, within the rotator interval, is evaluated by externally rotating the shoulder, keeping the elbow by the side, and maintaining the transducer in a longitudinal plane to the biceps within bicipital groove (Figs 2.26, 2.28, 2.29 and 2.32).
Bicipital groove, between the greater and lesser tuberosities, is deep and narrow superiorly, becoming wider and shallower inferiorly. Groove has a width of approximately 10 mm and a length of 5 cm. There is normally a minimal amount of fluid in bicipital sheath.
The subcoracoid bursa lies medial to coracoid process on a static study and extend to lateral aspect of coracoid when assessed dynamically. Insertional measurements of rotator cuff: subscapularis 40 × 20 mm, supraspinatus 23 × 16 mm, infraspinatus 29 × 19 mm, teres minor 29 × 21 mm [anterior to posterior (length) × medial to lateral (width)].
There is an extensive interdigitation of fibers between the tendons. On ultrasound, there is a change from hyperechoic fibrillar pattern of supraspinatus tendon to lower echogenicity of infraspinatus. The supraspinatus tendon extends for approximately 2.5 cm in anteroposterior direction. The supraspinatus tendon is normally partially obscured by overlying acromion process. To overcome this, supraspinatus tendon should be viewed in full internal rotation and hyperextension with the forearm behind the back, palm facing posteriorly, overlapping the scapular tip while maintaining elbow by the side, (Crass position). This places the tendon under stress and hence accentuates tears. Examination is repeated in the modified Crass/Middleton position with upper arm extended and shoulder in a neutral position, elbow flexed and pointing directly posteriorly, and palm placed forward against ipsilateral back pocket. This position allows for visualization of supraspinatus tendon adjacent to bicipital interval, an area often obscured by the acromion in Crass position. It is important to keep the elbow adducted (Flow Chart 2.1).
Supraspinatus tendon, on ultrasound they appear as a cone of tendinous bundles anteriorly and a flatter posterior tendon. A hypoechoic band of intervening muscle may be present medially, but fades as one extends laterally toward the greater tuberosity. In modified crass position, longitudinal images are obtained first by visualizing the intra-articular portion of the long head of the biceps tendon in longitudinal plane; this is equivalent to longitudinal plane of supraspinatus. The transducer is then slowly moved posteriorly in plane of supraspinatus, 45° to 50° to coronal oblique plane. Transducer is rotated 90° anticlockwise to assess the tendon 38in the axial plane starting anteriorly. In this position, coracoid process is identified medially, but the subscapularis is poorly visualized as it is now subcoracoid. Biceps tendon is seen as a hyperechoic oval structure. Lying just lateral to the biceps is anterior aspect of supraspinatus. In Crass position, subscapularis and occasionally biceps may not be identified as they are in a subcoracoid position. Transducer is positioned in plane of longitudinal axis of the supraspinatus tendon and over the coracoid process and then in transverse plane.
It is important to use both Crass and modified positions. Where there is limited range of movement, supraspinatus tendon is examined in as much internal rotation and hyperextension as possible. Examiner moves arm back and forth in this position to unroof as much of supraspinatus tendon from under acromion as possible, while assessing the dynamic motion of fibers.
Once the subacromial-subdeltoid (SASD) bursa is identified, it should be followed in anterior, posterior, medial, and lateral direction. This is important as significant distention with fluid may be visualized in only one region, commonly lateral to the greater tuberosity. An alternative position for examination of supraspinatus has been described whereby patient lies supine with shoulder at edge of bed, arm and elbow extended and forearm pronated. This is performed to assess muscle mass and fatty infiltration.
Infraspinatus and teres minor tendons are evaluated with forearm placed across chest and palm of the hand placed against contralateral shoulder. Infraspinatus is larger and lies above teres minor.
Insertion of the deltoid onto lateral aspect of midarm is visible as a distinct elevation. At anterior aspect of arm, biceps brachii is visible as an elongated muscle with lateral and medial depressions at its margins. It forms rounded contour of anterior arm. With flexion or contraction, biceps is identified as a discrete, elongated muscle mass. Proximal tendons of long and short head of the biceps are obscured, distal tendon is visible crossing the elbow joint when elbow is flexed. The humeral head is covered with hyaline cartilage. Greater and lesser tuberosities are separated from head by anatomical neck. The tuberosities represent important bony prominences that are landmarks for insertion sites of rotator cuff tendons. The deltoid tuberosity is an important proximal landmark, which is identified anterolaterally on humerus.
Deltoid muscle is a large multipennate muscle that forms round contour of shoulder. Proximally, muscle has attachments to the distal clavicle, acromion, and spine of scapula. Deltoid muscle has three components:
- Anterior—shoulder flexion
- Intermediate—shoulder abduction
- Posterior—shoulder extension.
Long head has origin at supraglenoid tubercle of scapula and leaves shoulder joint via intertubercular sulcus of proximal humerus. Distal tendon crosses elbow joint to insert onto radial tubercle, with proximal anterior fibers rotating laterally just prior to insertion. Bicipital aponeurosis is seen medially as a broad triangular fascial expansion extending from biceps tendon across brachial artery and cubital fossa into deep fascia of forearm. In 10% of population, a third head of biceps is present, originating from superomedial aspect of brachialis, with fibers attaching 39distally to bicipital aponeurosis and medial aspect of the tendon. Coracobrachialis has a proximal attachment to the coracoid process, in common with short head of biceps. Distally, it attaches to medial side of humeral shaft, near its midpoint, between the attachments of triceps and brachialis. This muscle, which is pierced by musculocutaneous nerve. Functions to weakly flex and adduct the shoulder joint. Brachialis muscle lies in a deep position in arm, with proximal attachment to anterior surface of the distal half of humerus and intermuscular septa. It is anterior to elbow joint, to attach to anterior aspect of the coronoid process of ulna. Brachialis acts as a flexor of elbow joint. Triceps long head originates as a flattened tendon from infraglenoid tubercle of scapula. In arm, it descends medial to lateral head and superficial to medial head. Lateral head arises as a flattened tendon from posterior surface of humerus, above radial groove.
Medial head has an extensive origin from posterior surface of humerus, inferior to radial groove, to within 2.5 cm from trochlea. The three components of triceps muscle have a common insertion onto olecranon process of ulna. Some of the medial head fibers reach olecranon process directly. Triceps is chief extensor of forearm. Other functions include extension of shoulder and adduction of arm.
Quadrilateral Space
It is bordered by the teres minor superiorly, teres major inferiorly, long head triceps medially, and humerus laterally. Subscapularis lies at anterior aspect. Structures traversing within space are axillary nerve and posterior humeral circumflex artery and vein.
Triangular Space
It lies below quadrilateral space. Bordered superiorly by subscapularis at its anterior aspect and by teres major at its posterior aspect. Long head of triceps forms medial border and lateral head of triceps forms the lateral border. Radial nerve and profunda brachii vessels traverse through it. A second triangular intermuscular space lies medial to quadrilateral space, with long head of triceps forming its lateral border and transmitting circumflex scapular artery.
On ultrasound, normal nerves appear as round or oval structures on short axis orientation. Longitudinally, normal nerves appear as cord-like hypoechoic structures of uniform thickness. Parallel hyperechoic linear structures are identified throughout their course, representing normal fascicular pattern of nerve fibers. On transverse imaging, background echotexture is hypoechoic, with multiple, discrete, slightly echogenic foci dispersed evenly throughout that represent nerve fascicles in cross section. As a result of this, ultrasound appearance of nerves is more hypoechoic than tendons.
Ultrasonography has definite role in injection steroid in subacromial space, as blind procedure has more chances of missing subdeltoid bursa and there are more chances of injection solution into rotator cuff which is detrimental to already injured tendon.40
In 1977, Mayer showed rotator cuff abnormality with ultrasound at annual conference in US Institute of Ultrasound in Medicine at Dallas.
Accuracy of injection corticosteroid into subacromial bursa is best at 70% in hands of experienced surgeon, 30% of cases steroid injected into subacromion bursal tissue are injected in rotator cuff tendon and muscle.
Note: Biceps acts as landmark, portion of cuff superior to biceps within 1.5 cm is supraspinatus and portion of cuff > 1.5 cm on the posterior aspect of biceps is infraspinatus.
The USG guided injections are less expensive, dynamic, with low interobserver variability, but it is operator dependent in the way images are taken different observers interpreting same set of images interobserver variability cannot be quantified but it is low and if at all the disagreements are minor it is uncommon for normal cuff to be confused with torn. With lack of surgical evidence for the same.
Position of Transducer (Fig. 2.9)
Parts visualized: Deltoid, with subacromion space beneath it and below it lies supraspinatus tendon with needle at subacromion space. Supraspinatus is seen as parrot beak appearing.
For visualizing biceps tendon position of probe is longitudinal over biceps tendon. It appears hypoechoic, as the angle it makes with transducer diverges from 180°.
Subscapularis is viewed as band of medium echogenicity deep to subdeltoid bursa, when probe is kept along its fibers. When USG probe is kept perpendicular to the direction of tendon of subscapularis, subscapularis and deltoid both are seen along with biceps. It is useful to internally and externally rotate the arm when looking for subscapularis.
When transducer is kept over the lateral aspect of acromion and above the humeral head supraspinatus tendon is seen below subdeltoid bursa as medium level of echogenicity and when probe is shifted anteriorly and arm in extension and internal rotation supraspinatus with parrot beak appearance is seen above which lies subdeltoid bursa.
Similarly infraspinatus is visualized by internally and externally rotating the arm and probe kept along its fibers below deltoid.
Teres minor is similarly visualized as tapered structure below deltoid.
In rotator cuff tear subdeltoid bursa is usually distended, tored tendon is seen as hyperechoic.
In horizontal full thickness tear longitudinal image show retraction of torn tendon. Bursa and prebursal fat rest directly on irregular bone surface of greater tuberosity humerus.
Rotator cuff tears can be diagnosed by nonvisualization of cuff and discontinuity and focal abnormal echogenicity associated and subdeltoid bursal and glenohumeral joint effusion and irregular bone surface and concave subdeltoid fat contours (Figs 2.15 and 2.23).41
Cartilage interface signs seen sometimes due to exposed cartilage of humeral head on transverse view (Fig. 2.24), it can be seen more clearly. Nonvisualization of cuff— contact of acromion with humeral head and deltoid over top of humerus separated by bursa/fat hypoechoic, patchy, tissue layer thin and irregular bursae may be 5 mm in thickness.
Humeral head ascends through defect in cuff due to pull of deltoid. Supraspinatus is under acromion, subacromion space should be smaller than 5 mm.
Focal nonvisualization of cuff at tendon bone junction leave bare area over bone with irregular surface of bone—naked tuberosity sign. Small amount of tissue will be preserved surrounding biceps. Small horizontal tears appear on longitudinal images but not on transverse. Infolding of bursal and peribursal fat in to focal defect—sign of full thickness tear. If tear is larger bursal and peribursal, fat tissue will approximate bone surface. Vertical tears are more traumatic may have history of dislocation. Defects appear increase in size on placing arm in extension and internal rotation.
Manual compression of bursa by transducer can move fluid into joint. Focal bright interface is present around a segment of hyaline cartilage—interface sign.
Focal abnormality, increased echogenicity may suggest new interface within the tendon at site of fiber failure (partial thickness tear).
Codmen defined rim rent sign (Figs 2.23 and 2.24)—partial thickness tears, anechoic spot on articular/bursal side of tendon. Focal lesion that violate defects are considered tears.
In intrasubstance lesions (50% of defects) associated findings are helpful (bursal synovium) edema is common finding in shoulder impingement rarely associated with tear.
Recess with synovial edema may not change its shape on compression, other causes of fluid in bursa—septic bursitis and calcium milk. Joint effusion occurs in recess like infraspinatus, subcoracoid and axillary.
Fluid in biceps tendon sheath is due to joint fluid gravitating down, many are associated with rotator cuff tear.
Large fluid in infraspinatus without fluid in subdeltoid bursa may be due to inflammatory or infectious cause.
Bright linear echoes from subdeltoid bursal fat are convex, upward concavity may be noted in medium and large tears reflecting the absence of cuff tendon. The cause of irregularity of tuberosity on acromion seen during elevation has been seen in rotator cuff tears insidious in onset and unnoticed by creeping tendon ruptures. It occurs in 30% at 60 years age.
Failure of cuff would lead to shoulder instability and internal impingement. Humeral head is no longer stabilized which leads to sclerosis and traction spur along coracoacromial ligament, high frequency transducer is preferred. Bicipital groove act as an anatomical landmark to separate subscapularis from supraspinatus in groove biceps tendon is visualized as oval structure when transducer is aligned along biceps tendon. Gentle pressure is necessary to parallel align transducer to tendon.42
Subscapularis appears as band of medium level echoes deep to subdeltoid fat and bursa.
External rotation is necessary to diagnose subluxation of long head of biceps if present intermittently
Supraspinatus is scanned perpendicular to its axis by moving transducer laterally and posteriorly.
Rest examination is done with arm adducted and hyperextended and shoulder in internal rotation.
During longitudinal scan transducer overlay acromion medially and lateral aspect of greater tuberosity laterally. Transducer perpendicular to humeral head surface approximately 7.5 cm lateral to long biceps tendon is scanned for infraspinatus. Critical zone is that part of tendon that begins approximately 1 cm posterolateral to biceps.
Transducer is kept in plane parallel to scapular spine for infraspinatus and teres minor. Beak shaped is seen at its attachment to greater tuberosity.
Posterior glenoid labrum is seen as hyperechoic triangle structure, with fluid of infraspinatus recess surround labrum.
Hypoechoic articular cartilage of humeral head contrast significantly with hyperechoic fibrocartilage teres minor is trapezoidal broad and more muscle attachment (Figs 2.23 and 2.24).
Rotator cuff tendons are hyperechoic compared to deltoid. Cuff enveloped by thin 1.5 mm bursa appears relatively hypoechoic. Thickness of bursa does not change.
Bursa is hypoechoic stripe thinner than thickness of hypoechoic hyaline cartilage over humeral head.
Bursa is hoof shaped.
Bursal vessels are not normally shown in color Doppler between bursa and deltoid is peribursal fat.
Prevalence of full thickness tears over 50 years age is 31% no significant difference were found in prevalence of rotator cuff (RC) lesion in each gender for either the dominant or nondominant arm/emotional activities but there is linear increase after 50 years of age.
Difference was significant 64% had bilateral tear, 26 full thickness and 15 partial age, range 35–80 years.
Average age in partial thickness—56 years.
For full thickness—63 years.
Rotator cuff tear can be incidental finding rotator cuff tear and fluid in biceps tendon can occur in normal individuals also.
BICIPITAL TENOSYNOVITIS
This condition is seen in repeated elbow flexion against resistance, it is common cause of shoulder pain in elderly with woman > men.
Tenosynovitis is caused by impingement and instability or generalized inflammatory process. It is more in weightlifters, masons and rock climbers.43
Mostly presents with pain and tenderness along long head of biceps causing cuff tendinosis.
Post and Been et al has shown that tendonitis is primarily related to bony abnormalities of bicipital groove or transverse humeral ligaments.
Tenosynovitis is idiopathic, due to trauma or calcium deposits. Injuries are common with repetitive overhead activity and degenerative changes can occur in old people without inflammation. It may be secondary to disorders like rotator cuff disorder, labral tear and intra-articular pathology. Long head of biceps is intimately involved with capsule of shoulder joint, it is frequently involved by inflammatory process affecting joint.
Tendonitis of biceps tendon frequently coexist with bursitis of associated bursa causing additional pain and functional disability.
Reasons for tendonitis are:
- Wide range of repetitive trauma
- Space is restricted by coracoacromial arch.
- Blood supply of musculotendinous unit is poor.
All these factors contribute to tendonitis of biceps.
It is seen that shoulder complaints in patients with reflex sympathetic dystrophy of upper limb is shown to be attributed to bicipital tendinitis.
Biceps tendinitis should be treated by treating the cause of tendinitis.
It usually responds to conservative treatments. If there is extensive fraying of tendon, then only tenodesis is to be done and adequate treatment of associated cuff pathology/joint pathology should be done. Surgery should be considered only after 6 months trial of conservative treatment, according to newer treatment options biceps tenotomy with needle and followed with local injection of platelet rich plasma can be given.
It is usually recommended 3–6 weeks after acute episode of pain.
Range of motion is usually normal, although restricted at times, strength is normal, pain with elbow at 90° and internal and internal rotation of arm causes pain in bicipital groove. There is also pain with shoulder elevation. Rolling of bicipital tendon elicit pain.
Indications: Injections are shown to be effective when associated with rotator cuff lesions. More when patients are in painful stage and during rehabilitation period and during early periods of shoulder stiffness. Since, intratendinous injections of steroids are harmful and if platelet rich plasma is given, we want to deliver it to exact site of infiltration. Ultrasound is most useful of this.
Technique (Figs 2.28 and 2.30 and Flow Chart 2.1)
Position: Patient sitting/lying down with affected arm by side with external rotation by 45°.
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 mg of methylprednisolone. Syringe: 2 ml/1 ½ inch, 25 gauge needle palpate the bicipital groove with arm in external rotation which brings lesser tuberosity into view.44
Biceps tendon is identified in groove, point of maximal tenderness is noted in order to inject into the area of long head of biceps, needle is inserted directly into most tender area over groove needle must be at 30° to skin and directed parallel to groove.
Objective is to infiltrate the area in and around the groove and not into the tendon as if may result in rupture. Increase resistance to injection suggest that needle is in tendon and it should be withdrawn a little.
Benefit takes 2–3 days to appear.
Patients are advised to restrict overhead activity and weight lifting for 1 month.
Risk of tendon rupture is present in old age and those with repeated injections.
Sometimes pain may worsen.
Steroid can precipitate as crystals which can cause extreme pain.
Same as above, biceps is identified as long fibrillar structure surrounding which there is fluid injection is given in to the sheath. Biceps is identified by rotating arm. The entry point and position of needle is same as above.
Probe is kept on longitudinal plane of arm and transverse to it.
Glenohumeral Joint Injection
Main indications are osteoarthritis, adhesive capsulitis, rheumatoid arthritis and rotator cuff lesions (not common).
Patients with osteoarthritis of glenohumeral joint usually present with old age or traumatic injury in young, chronic pain and decrease in range of movements.
Adhesive capsulitis usually occurs in middle aged, secondary to non use of shoulder due to pain and prolonged immobilization. It is seen most commonly in women and with those with diabetes, it is usually associated with tendinosis and bursitis.
Rheumatoid arthritis is systemic inflammatory disease of autoimmune nature that involves inflammation of synovium.
S Arstan and Reyhon Celifer showed that local steroid injection therapy was as effective as physical therapy for treatment of adhesive capsulitis.47
Firm painful endpoint is present in range of motion during physical examination.
Frozen shoulder syndrome is capsular inflammation in outer synovial recess with resulting tenting of adjacent subcapsularis and biceps tendon involved.
Bernstein and Roberts et al showed that there is limited evidence of effectiveness of steroid for shoulder arthritis and nonspecific painful shoulder.
Indications: Since intra-articular injections are of usefulness in post-traumatic arthritis and osteoarthritis and it has effect for medium term, it is useful during acute painful episodes in order to provide more faster rehabilitation. It is done when all other methods of conservative management are exhausted and to bye time before surgical intervention. Image intensifier or ultrasound can be used for this purpose always rule out tuberculosis and neuropathic affection of joint before injection with help of investigations.
Glenohumeral joint can be injected from anterior, posterior or superior approach.
Position: Patient arm is resting comfortably at side and shoulder is internally rotated in posterior approach.
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 to 80 mg of methylprednisolone.
Syringe: 5 ml 1 ½ inch 25 gauge needle.
Posterior Approach
Not technically demanding and safe.
Needle is inserted 2–3 am inferior and medial to posterolateral corner of acromion and directed inferiorly anteriorly and medially in direction of coracoid process, aspiration is done to confirm that blood vessel is not punctured.
Injection is given slowly but with constant pressure.
Anterior Approach
Technically demanding and associated with dangers of injuring brachial plexus.
Position: Patient is sitting or lying on back with the forearm placed on abdomen and shoulder partially internally rotated.
Needle is placed just medial to head of humerus palpated by rotating the arm and 1 cm lateral to coracoid process below the acromion.
Needle is directed posteriorly and slightly superiorly and laterally. If needle hits bone it should be pulled back and redirected at different angle.
After injection, joint is put in passive range of motion and pendulum exercises monitored for 30 minutes.
Patient is instructed to avoid driving activities for 48 hours.
Follow-up examination is arranged within 3 weeks.
Lateral Approach
Position: Sitting or supine.
Midpoint of acromion is palpated. Shoulder joint space is 2.5 cm below the midpoint. Needle is advanced carefully into this space.
If no resistance is felt then it is in the joint.
If resistance is felt-hit the bone, draw needle and redirect it.
Needle has gone superiorly and is in ligament medially needle is advanced slightly further and injected.
Ultrasonography Guided Injection is Helpful
Position of patient and approach is same as above probe is kept on superior aspect of acromial arch and needle is visualized in joint.
Position of transducer is same as that used for subdeltoid injection and approach is same as given above.
CALCIFIC TENDINITIS (FIG. 2.16)
In this condition there are deposits of hydroxyapatite crystals seen in rotator cuff tendon which most commonly involves supraspinatus tendon.
Collection of crystals may rupture and thick while material is seen as vague shadow on they if viewed angled around clavicle.
It presents with acute deltoid pain and tenderness.
Codron proposed vascular cause with degeneration of tendon fibers proceeding calcification. It has following stages: precalcific phase, calcific phase and post calcific phase. Injections are affective in most precalcific phase and calcific phase.
The X-ray reveals calcium deposits within rotator cuff or overlying head of humerus and symptoms include excruciating pain and severe resistance of movement.
Rina Aiva, Etionne et al showed that treatment with ultrasound guided fine needle technique showed improvement in pain and disability index for calcific tendinitis patients.50
ADHESIVE CAPSULITIS
Neviser in 1945 introduced adhesive capsulitis and described it as inflammatory process.
It shows contracted thickened shoulder joint capsule with relative absence of synovial fluid and chronic inflammatory change.
Limberge classified it to primary, i.e. with no inciting event and with no abnormality on examination and secondary with precipitant traumatic injuries.
Initially internal rotation is lost followed by loss of flexion and external rotation and less than 90° abduction. It has typically 3 phases, i.e phase of freezing (pain)followed by frozen (stiffness) and phase of thrawing.
Treatment should be given as early as possible. Useful in painful stages to initiate physiotherapy early.
Injection site is directed by prime cause of adhesive capsulitis.
If it is frozen shoulder syndrome, injection is to be given in glenohumeral joint.
Ajda-Emer Eksongh et al in 2008 showed addictive effect of corticosteroid in providing rapid pain relief mainly in 1st week of exercise treatment period.
Number of patients were 80. They were divided in 2 groups, group-I were given steroid and 12 weeks comprehensive home exercise program as against group-II given serum and 12 weeks exercise program, they were evaluated with shoulder pain and disability index.
Scores were good at end of 2nd week with better scores in group-I but no significant difference between groups at 12 weeks.
Cytokines have been recently implicated in inflammation and fibrosis and initiation and termination of repair process in multiple musculoskeletal disorders with production of tissue fibrosis.
Rizk et al showed that early treatment with intra-articular steroid acts as chemical ablator of synovitis.
There were various studies comparing use of steroids with local anesthetic and use of steroid and local anesthetic alone. Most of them found that injection steroid and local anesthetic had advantage of partial transient pain relief.
Balgen et al also showed that initial response to treatment with steroid was most marked but long-term outcome was same with all modalities.
Same results were shown by Vendor Wait, he used Los Angeles score which incorporates patient satisfaction, shoulder function, range and strength of forward elevation. Those with predominant pain symptom, intra-articular steroid treatment could be advised concomitantly with exercise.
Ryon et al also showed same results, local steroid can be effective up to 6 weeks.
Arthrocentesis followed by injection of local anesthetic and steroid provide joint and soft-tissue of shoulder with focal pain relief without toxicity with long- term use of steroid. Shoulder steroids in conjugation with adequate rest and other modalities help to reduce pain and discomfort. Arthrocentesis is aspiration of synovial fluid from swollen or painful joint. It is important diagnostic and therapeutic tool to establish diagnosis and limit joint damage.51
ACROMIOCLAVICULAR JOINT
It is diarthrodial joint that connects acromion to distal clavicle. Local injection steroid is given after trial of other conservative methods.
Osteolysis of distal clavicle is degenerative process that results in chronic pain particularly with adduction.
Osteolysis secondary to traumatic injury or in person who perform repetitive weight training involving shoulder.
Osteoarthritis may also develop is acromioclavicular joint secondary to previous trauma or injury.
Pain is increased by having patient hold opposite shoulder and pushing the elbow toward ceiling against resistance.
Differential Diagnosis
Impingement syndrome.
X-ray is used for confirming the diagnosis.
Subacromion injection is done prior to rule out impingement syndrome as cause of pain.
Patient with osteolysis/arthritis of acromioclavicular joint will not have temporary relief of symptoms.
Indications: Since intra-articular injections are of usefulness in post-traumatic arthritis and osteoarthritis and it has effect for medium term. It is useful during acute painful episodes in order to provide more faster rehabilitation. Since it is superficial joint. Image intensifier guided injections are less useful but they can be used for this. It may be useful in painful chronic AC joint dissociation, if patient is not willing/not medically fit for surgery.
Position: Supine/seated position with arm at side.
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1 ½ inch 25 gauge needle.
Acromioclavicular joint is identified with a point with as slight depression felt at joint articulation.
Needle is inserted from superior and anterior approach to acromioclavicular joint and directed inferiorly.
If there is resistance while attempting to inject the solution, partially withdraw the needle and if the needle is in proper plane, there is little resistance to injection of local anesthetic and steroid.53
The USG guided injections are helpful.
Probe is kept one end over acromion and other end over clavicle lateral end and joint is visualized. Needle is approached as in open technique. Position of patient remains same C arm guided injections are useful. Similarly hand cross over is useful maneuver for visualizing acromioclavicular joint
SUPRASPINATUS INFILTRATION
Technique
Position: Patient bends his/her elbow to right angle and puts forearm behind back with elbow well into the side.
Patient then leans back in half lying position and fixing his/her arm in adduction and medial rotation.
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1 ½ inch 25 gauge needle.
Supraspinatus tendon is bent through right angle and lies in sagittal plane, passing from base of coracoid process forwards over head of humerus to greater tuberosity emerging under anterior edge of acromion.
If no resistance is felt for first 1 cm when needle reaches the tendon, operator recognizes the tough tissue. It is difficult to appreciate this structure by palpation.
On ultrasonography, supraspinatus is visualized as parrot beak structure. It is to be confirmed by repeated abduction and external and internal rotation also spine of scapula serves as landmark for the tendon keep transducer above the spine and trace the tendon to its insertion.54
Hypoechoicity of tendon or bursal thickening or peritendon fluid are signs of partial tear of supraspinatus. Complete tear of supraspinatus is visualized clearly.
Approach position and entry point of needle remains same as above.
Technique
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1 ½ inch 25 gauge needle.
Position: Patient lies facing downwards propping his/her self up on elbow. This ensures that scapula is at right angles to humerus and acromion is drawn away from greater tuberosity of humerus, this brings tuberosity of humerus backwards.
Arm is then adducted, infraspinatus tendon is felt on lateral extent of spine of scapula. Point of insertion on the tuberosity of humerus is felt.
Needle is thrust vertically downwards until resistance of tendon is felt. Injection is infiltrated by half withdrawing and reinserting the needle and then at different angle and different depth.
On USG, infraspinatus is visualized as fribrillar structure. It is to be confirmed by repeated resisted adduction and external rotation, also spine of scapula serves as landmark for the tendon keep transducer below the spine and trace the tendon to its insertion (Figs 2.41, 2.43 and Flow Chart 2.1).
Hypoechoicity of tendon or bursal thickening or peritendon fluid are signs of partial tear of infraspinatus. Complete tear of infraspinatus is visualized clearly.
Approach position and entry point of needle remains same as above.
SUBSCAPULARIS TENDON INFILTRATION
Technique
Position: Patient in supine on couch, with her hand on thigh, such that bicipital groove faces anteriorly immediately medial to it lies the subscapular tendon. Insertion is 3 cm long approximately.
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 mg of methylprednisolone.
Syringe: 2ml/1 ½ inch 25 gauge needle.
Tendon is infiltrated on medial edge of bicipital groove. Tendon can then be recognized by resistance it offers to the progress of needle.
On USG, subscapularis is visualized as fribrillar structure. It is to be confirmed by repeated resisted adduction and internal rotation also, biceps serves as landmark 56for the tendon. To differentiate tendon from supraspinatus keep transducer medial to biceps the tendon to its insertion.
Hypoechoicity of tendon or bursal thickening or peritendon fluid are signs of partial tear of subscapularis. Complete tear of subscapularis is visualized clearly.
Approach position and entry point of needle remains same as above.
ROTATOR CUFF ARTHROPATHY
It is multifactorial in causation, causes include extrinsic like coracoacromial arch, overuse phenomenon. Intrinsic causes are degeneration vascular supply, collagen fiber orientation and regional variation of tendon.
Important feature is coarse palpable crepitation, night pains (DD tuberculosis) muscle atrophy. X-rays show superior migration of humeral head with degenerative changes in shoulder joint, subchondral sclerosis, and erosions on glenoid acromion and clavicle.
When migration of humeral head occurs local injections are of no use. They are useful in initial stages to avert night pains and improve range of motion with help of physiotherapy. Methodology of injection is same as described for glenohumeral joint injection.
FURTHER READING
- Adler RS, Fealy S. Ultrasound of rotator cuff tear: current status. Techniques in Shoulder and Elbow Surg. 2003;4:121–32.
- Andrieu V, Dromer C, Fourcade D, Zabraniecki L, Ginesty E, Marc V, et al. Adhesive capsulitis of the shoulder: therapeutic contribution of subacromial bursography. Rev Rhum Engl Ed. 1998;65:771–7.
- Arslan S, Celiker R. Comparison of the efficacy of local corticosteroid injection and physical therapy for the treatment of adhesive capsulitis. Rheumatol Int. 2001;21: 20–3.
- Basset RW, Cofield RH. Acute tears of the rotator cuff: the timing of surgical repair. Clin Orthoped Relate Res. 1983;175:1824–7.
- Blair B, Rokito AS, Cuomo F, Jarolem K, Zuckerman JD. Efficacy of injections of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg (Am). 1996;78:1685–9.
- Brandt TD, Cardone BW, Grant TH, Post M, Weiss CA. Rotator cuff sonography: a reassessment. Radiology. 1989;173:323–7.
- Bryant L, Shnier R, Bryant C, et al. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging and arthroscopy in determining the size of rotator cuff tear. J Shoulder Elbow Surg. 2002;1:219–24.
- Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis. 1984;43:353–60.
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics. Vol 3, 11th ed. Mosby Inc. 2008. pp. 2339-77.
- Cardone DA, Tallia AF. Joint and soft tissue injection. Am Fam Physician. 2002;66:283-45. 8,290.
- Chang CY, Wang SF, Ohiou HJ, et al. Comparison of shoulder ultrasound and MR imaging in diagnosing full thickness rotator cuff tears. Clin Imaging. 2002;26:50–4.
- Churgay CA. Diagnosis and treatment of biceps tendinitis and tendinosis. Am Fam Physician. Sep l 2009;80(5):470–6.
- Crass JR, Craig EV, Feinberg SB. Ultrasonography of rotator cuff tear: a review of 500 diagnostic studies. J Clin Ultrasound. 1988;16:313–27.
- Dacre JE, Beeney N, Scott DL. Injections and physiotherapy for the painful stiff shoulder. Ann Rheum Dis. 1989;48:322–5.
- de Jong BA, Dahmen R, Hogeweg JA, Marti RK. Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Re Habil. 1998;12:211–5.
- Dickson J. Shoulder injections in primary care. Practitioner. 2000;244:259–65.
- Eakin CL, Faber KJ, Hawkins RJ, et al. Biceps tendon disorders in athletes. J Am Acad Orthop Surg. Sep-Oct 1999;7(5):300–10.
- Ekeberg OM, Bautz-Holter E, Tveita EK, et al. Subacromial ultrasound guided or systemic steroid injection for rotator cuff disease: randomised double blind study. BMJ. 2009 Jan 2\;338:a3112. doi: 10.1136/bmj.a3112
- Farin PU. Sonography of the biceps tendon of the shoulder: normal and pathologic findings. J Clin Ultrasound. Jul-Aug 1996;24(6):309–16.
- Farin PU, Jaroma H, Soimakallio S. Rotator cuff calcifications: treatment with ultrasound-guided technique. Radiology. 1995;195:841–3.
- Flannigan B, Kursonoglu-Brajme S, Snyder S, et al. MR arthrography of the shoulder: comparison with conventional MR imaging. AJR Am J Roentgenol, 1990;155:829–32.
- Fongemie AE, Buss DD, Rolnick SJ. Impingement syndromes and injection technique. American Family Physician. 15th February 1998.
- Halverson L, Maas R. Shoulder joint capsule distension (hydroplasty): a case series of patients with “frozen shoulders” treated in a primary care office. J Fam Pract. 2002;51:61–3.
- Harryman DT, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA 3rd. Rotator cuff repair: correlation of functional results with cuff integrity. J Bone Joint Surg. 1991;73A:982-9.
- Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151–8.
- Hiemstra LA, MacDonald PB, Froese W. Subacromial infection following corticosteroid injection. J Shoulder Elbow Surg. 2003;12:91–3.
- Hodler J, Fretz C J, Terrier F, Gerber C. Rotator cuff tears: correlation of sonography and surgical findings. Radiology. 1988;167:791–3.
- Holtby R, Razmjou H. Accuracy of the Speed's and Yergason's tests in detecting biceps. Pathology and Arthroscopy. Mar 2004;20(3):231–6.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. 1st ed. 2007. pp. 25-112.
- John O Neill. Musculoskeletal Ultrasound Anatomy and Technique. Springer Inc. 2008. pp. 20-330.
- Kelley MJ, Ramsey ML. Osteoarthritis and traumatic arthritis of the shoulder. J Hand Ther. 2000;13:148–62.
- Klippel JH, Weyand CM, Wortmann R. Primer on the Rheumatic Diseases. 11th ed. Atlanta: Arthritis Foundation, 1997. p. 420.
- Larson HM, O'Connor FG, Nirschl RP. Shoulder pain: the role of diagnostic injections. Am Fam Physician. 1996;53:1637–47.
- Larson HM, O'Connor FG, Nirschl RP. Shoulder pain: the role of diagnostic injections in primary care. Practitioner. 2000;244:259–65.
- Mack LA, Nyberg DA, Matsen FA III. Sonographic evaluation of the rotator cuff. Radiol Clin North Am. 1988;26:161–77.
- Mantone JK, Burkhead WZ Jr, Noonan J Jr. Nonoperative treatment of rotator cuff tears. Orthop Clin North Am. 2000;31:295–311.
- Masten FA, Arntz CT. Subacromial impingement. In: Rockwood CA, Matsen FA (Eds). The Shoulder, Vol II. W B Saunders, Philadelphia 1990.
- Miller CL, Karasick D, Kurtz AB, Fenlin JM. Limited sensitivity of ultrasound for the detection of rotator cuff tear. Skeletal Radiol. 1989;18:179–83.
- Morrison DS, Greenbaum BS, Einhorn A. Shoulder impingement. Orthop Clin North Am. 2000;31:285–93.
- Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. Sep-Oct 2000;9(5):382–5.
- Neer CS II, Craig EV, Fakuda H. Cuff tear arthropathy. J Bone Joint Surg (Am). 1983;65A:1232-44.
- Neer CS 2nd. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg (Am). 1972;54:41–50.
- Nidecker A, Guckel C, von Hochstetter A. Imaging the long head of biceps tendon-a’ pictorial essay emphasizing magnetic. Eur J Radiol. Nov 1997;25(3):177–87.
- Partington PF, Broome GH. Diagnostic injection around the shoulder. Hit and miss? A cadaveric study of injection accuracy. J Shoulder Elbow Surg. 1998;7:147–50.
- Patel DR, Nelson TL. Sports injuries in adolescents. Med Clin North Am. 2000; 84:983–1007.
- Patten RM, Mack LA, Wang KY, Lingel J. Nondisplaced fractures of the greater tuberosity of the humerus: sonographic detection. Rhum Engl Ed. 199865771–7. TL7.
- Raynauld JP, Choquette D, Haraoui B, Zummer M, Pelletier JP. Hylan versus triamcinolone acetonide injection for acute supraspinatus tendinitis: Early report of a randomised controlled trial. Arthritis Rheum. 1994;37:1111.
- Rumack C, Wilson S, William J. Diagnostic Ultrasound. Vol 1. 2nd Edition. Mosby Inc. 1998:843-83.
- Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. Nov-Dec 1999;8(6):644–54.
- Siegel LB, Cohen NJ, Gall EP. Adhesive capsulitis: a sticky issue. Am Fam Physician. 1999;59:1843–52.
- Solbiati L, Rizzatto G. Ultrasound of Superficial Structures. 1st edition. Churchill Livingstone. 1995:279-375.
- Stelnbrocker O, Argyros TG. Frozen shoulder: treatment by local injections depot corticosteroids. Arch Phys Med Rehabil. 1974;55:209–13.
- Teefey SA, Middleton WD, Rubin DA, et al. Detection of partial and full thickness rotator cuff tears in patients with a painful shoulder: a comparison of ultrasound, MRI and arthroscopic surgery. Radiology. 2000;217:430.
- Teefey SA, Rubin DA, Middleton WD, et al. Detection and quantification of rotator cuff tears: a comparison of ultrasound, MRI and arthroscopic findings in seventy one consecutive cases. J Bone Joint Surg (Am). 2004;86:708–16.
- Tsur A, Gillson S. Brachial biceps tendon injuries in young female high-level tennis players. Croat Med J. Jun 2000;41(2):184–5.
- van der Windt DA, Koes BW, Deville W, Boeke AJ, de Jong BA, Bouter LM. Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care: randomised trial. BMJ. 1998;317:1292–6.
- van Holsbeeck M, Kolowich PA, Eyler WR, Craig JG, Shirazi KK, Habra GK, et al. Ultrasound evaluation of the rotator cuff. Radiol. 1985;157:205–9.
- Watson Buchaman W. Clinical Examination of Musculoskeletal System. Williams & Wilkins. 1st Edition. 1997:25-82.
- Winters JC, Jorritsma W, Groenier KH, Sobel JS, Meyboomde Jong B, Arendzen HJ. Treatment of shoulder complaints in general practice: long-term results of a randomised, single blind study comparing physiotherapy, manipulation, and corticosteroid injection. BMJ. 1999;318:1395–6.
- Woodward TW, Best TM. The painful shoulder: part II. Acute and chronic disorders. Am Fam Physician. 2000;61:3291–300.
- Wright T, Yoon C, Schmit BP. Shoulder MRI refinements: differentiation of rotator cuff tear from artifacts and Semin Ultrasound CT MR. Aug 2001;22(4):383–95.
- Yamakado K. The targeting accuracy of subacromial injection to the shoulder: an arthrographic evalustion. J Arthroscopic & Related Surg. 2002;18(8):887–91.
- Zancolli EA, Cozzi EP. The flexor tendon sheaths of the fingers and the thumb. In: Atlas of Surgical Anatomy of the Hand. New York, NY: Churchill Livingstone. 1992:327-45.
Medial epicondyle and lateral epicondyle can be palpated as a prominence on both medial and lateral side of elbow. Lateral epicondyle is smaller than medial.
For palpating olecranon patient is asked to flex elbow, which makes it prominent. Bursa covering olecranon usually does not hinder olecranon palpation. Olecranon bursa is boggy and thick. Posterior ulnar border is palpated distally.
Ulnar border is palpated with patients arm in abduction and straight subcutaneous ulnar border to ulnar styloid of wrist can be palpated. Radial head is palpated in same position with elbow in flexion and just distal to lateral epicondyle.
The radial head is felt as depression 2.5 cm distal to lateral epicondyle. As forearm is pronated and supinated, movement of radial head can be felt beneath the surgeon's fingers.
Wrist flexor pronator group consist of 4 muscles.
(1) Pronator teres, (2) Flexor carpi radialis, (3) Palmaris longus, (4) Flexor carpi ulnaris.
Four muscles arising from common extensor origin: Extensor digitorum communis, extensor digiti minimi, extensor carpi ulnaris, and anconeus.
Medial collateral ligament (MCL) of elbow is fan shaped arising from medial epicondyle and extended to medial margin of ulna trochlea.
Brachioradialis originates from lateral supracondylar ridge of humerus. The brachioradialis is a fleshy muscle that forms lateral border of supinated forearm.
Radial nerve, at the level of the elbow joint lies between brachialis and brachioradialis.
Radial nerve divides into three terminal branches: Posterior interosseous nerve enters supinator muscle, motor branch to extensor carpi radialis brevis enters 63that muscle immediately, and sensory branch passes down forearm behind the brachioradialis.
Radial nerve crosses in front of elbow joint in interval between brachialis and brachioradialis muscles. It divides in the cubital fossa at radiohumeral joint line into superficial radial nerve (which descends on lateral side of forearm under cover of brachioradialis muscle) and posterior interosseous nerve (which enters substance of supinator muscle).
Posterior interosseous nerve is vulnerable to injury as it winds around neck of radius within the substance of supinator muscle.
Bicipital aponeurosis (lacertus fibrosus), is a band of fibrous tissue coming from the biceps tendon and moves medially across the forearm superficial to proximal part of superficial flexor muscles. Radial artery lies immediately deep to the bicipital aponeurosis.
Ulnar nerve lies in sulcus between medial epicondyle and olecranon process and can be palpated as it is rolled gently under index and middle finger. It is felt as tubular structure.
Ulnar nerve enters the anterior compartment of the forearm by passing between the two heads of flexor carpi ulnaris muscle, which it supplies and where it may be entrapped.
Cubital fossa is triangular space bordered laterally by brachioradialis and medially by pronator teres and an imaginary line drawn between the two epicondyles of humerus. Contents from medial to lateral are musculocutaneous nerve, median nerve, brachial artery and biceps tendon.
It is felt as a skin depression in front of elbow and boundaries can be seen and felt. The bicipital aponeurosis can be felt as it leaves the tendon to join the deep fascia on medial side of forearm in flexion against resistance.
WRIST EXTENSOR GROUP
Mobile wad of three consists of brachioradialis, extensor carpi radialis brevis and longus. Initially palpated on lateral epicondyle.
For brachioradialis, which originates from lateral supracondylar ridge of humerus, patient is made to close fist placed in neutral position under edge of table and then lift up against weight of table.
Extensor carpi radialis longus and brevis can be palpated by asking patient to make fist and resist extension of flexed wrist. They can be traced distally to proximal part of 2nd and 3rd metacarpal. Lateral collateral ligament (LCL) similarly extends from lateral epicondyle at side of annular ligament which encircles the radius (injured due to varus stress).
Muscles and tendons: Position for ultrasound examined
Deltoid arm adducted, in neutral and relaxed position
Biceps brachii—long head elbow flexed, forearm supinated
Biceps brachii—short head elbow flexed, forearm supinated
At elbow joint, joint capsule is immediately deep to brachialis muscle.
Median nerve lies in close approximation to brachial artery, at level of antecubital fossa. For this reason, brachial artery serves as a quick and easy 64anatomical landmark for the median nerve. Median nerve can be followed proximally into arm. This is often easiest to perform in the transverse orientation. Nerve can be quickly identified at the level of carpal tunnel, at wrist, and followed proximally into forearm and arm. Nerve is then imaged along its longitudinal course.
In proximal half of the arm, ulnar nerve is located medial, adjacent to brachial artery. At midarm, it pierces intermuscular septum and continues descending along a medial course, anterior to medial head of triceps. At elbow, it is identified lying adjacent to medial epicondyle. As with median nerve, course and location of ulnar nerve in arm are often easiest to assess by first identifying this structure at level of elbow joint and following it proximally.
This is accomplished by bridging the ultrasound probe with one end on olecranon process and other on medial epicondyle. In this position, ulnar nerve is identified as a round to oval structure adjacent to medial epicondyle, which is a key anatomical landmark for this nerve.
When imaging radial nerve, examiner first identify the structure at level of deltoid tuberosity, from which point it can be followed proximally (posterior and superior) and distally (anterior and inferior) with ultrasound probe in transverse position. At level of posterolateral humerus, nerve runs alongside the brachial artery. Proximally, it can be identified between coracobrachialis and inferior margin of teres major muscles approximately 10 cm above the lateral epicondyle of humerus, nerve penetrates the lateral intermuscular septum and passes into anterior compartment of arm. At this point, the radial nerve is identified anteriorly. It lies in a groove between brachialis and brachioradialis muscles. Normal radial- nerve has a round appearance proximally, an oval shape at the level of the mid- humerus, and returns to a round shape at the distal third of the humerus. At the level of spiral groove on humerus, the normal diameter of this nerve is 4.0–4.2 mm in transverse and 2.3–3.5 mm in anteroposterior direction.
Elbow sonographic evaluation also includes articular abnormalities, including joint effusions, assessment of complications from arthritis, presence of intra-articular bodies, and synovitis. Choice of probes and ideal frequency are affected by body habitus. In general, highest frequency that permits adequate pentration of structures of interest is recommended. Color and power Doppler are useful for demonstrating hyperemia and relation of regional structures and pathology to normal arteries and veins. Doppler is useful for assisting in determining cystic versus solid nature of any hypoechoic or anechoic abnormalities identified. For superficial structures, used of more gel is recommended.
Cubital fossa is a triangular space or depression at anterior aspect of elbow. Fossa is bounded by medial and lateral muscle groups that form respective boundaries of space. Medial elevation consists of pronator teres muscle; brachioradialis muscle forms lateral elevation. Conventionally, imaginary line traversing between two humeral epicondyles defines proximal boundary of fossa. Distally, medial and lateral muscle groups converge to create a triangular configuration. Brachialis and supinator muscles form floor of fossa. Deep fascia, strengthened by bicipital aponeurosis, forms the roof of fossa, which is covered by superficial fascia and skin. With elbow joint flexed, tendon of biceps brachii is visible as a cord-like structure crossing front of elbow crease. This structure is palpated. In addition, 65bicipital aponeurosis is palpated proximally, where it passes on an oblique course over median nerve and brachial artery.
TENNIS ELBOW (FIG. 3.27)
Most commonly seen in the age group of 40 to 50 with equal gender incidence. Runge (1873) described it as angiofibroblastic hyperplasia, most commonly involving extensor carpi radialis brevis, which can also involve extensor carpi radialis longus and extensor digitorum communis.
Other causes may be periostitis, inflammation of bursa at common extensor origin, calcified deposits, painful annular ligament.
Tenderness is present over the lateral epicondyle, approximately 5 mm distal and anterior to the midpoint of lateral epicondyle. The pain of radial tunnel syndrome is located 3 to 4 cm distal to the lateral epicondyle and may be reproduced with long finger extension against resistance.
More common in dominant arm and serve players. Also seen in swimmers, carpenters, plumbers, housewives, textile workers.
Resisted wrist dorsiflexion and supination of forearm exacerbate pain. Pain also occurs while grasping objects. Forced palmar flexion elicit pain maneuver of raising chair causes severe pain.
Nonoperative treatment is successful in 95% cases.
Pametta and Jones showed that 40% patients had complete relief of symptoms after steroid injection. High success rate was seen after early local corticosteroid injection as an adjuvant to local anesthetic. An attempt was made to complete lesion by forcibly flexing the wrist after local anesthetic to initiate inflammatory cascade and healing.
Autologous blood is shown to be beneficial in certain patients. Edwards and Calem Druceie showed 79% success in relieving pain.
Smidt, Vanderwindt DA et al (2002) showed that corticosteroid offers immediate and short-term improvement but more sustained improvement is seen after physiotherapy. It needs to be differentiated from radial tunnel syndrome, cervical radiculopathy, radiocapitellar osteochondral lesion and posterolateral elbow instability. On X-rays, calcifications may be seen over lateral epicondyle.
In one such trials of duration 6 weeks, with outcome measured as pain relief on resisted dorsiflexion; 57 patients in injection group (given 1 ml of injection triamcinolone acetonide and 1 ml of lidocaine 2% at the tender spot), 30 patients in physiotherapy group and 1 in wait-and-see group were evaluated. Significant improvement was noted initially in those in wait-and-see group treated with NSAIDs; corticosteroid group initially scored significantly better in all primary and secondary outcomes; and at 26–52 weeks, physiotherapy group scored better than injection treatment group. Mafulli et al reported possible prognostic value of USG as diagnostic modality. Results are good in early stages.
Indications: Injection steroid (given in tendon sheath and peritendinous) or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority (90%) and in order to 66avert painful episodes. These injections are preferred prior to physiotherapy. USG guided injections are useful.
Local injections work in all stages of disease whether rest pain or night pains or pain on activity is present.
Position: Sitting position, arm directed at patients side and elbow extended/flexed with forearm supported on table, elbow held fully supinated and in extension with surgeon's thumb on most tender point.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/ 1 ½ inch 25 gauge needle.
Lesion is pinched between thumb and index finger and needle is inserted obliquely through the belly of brachioradialis muscle until tip of needle lies deep to brachioradialis. Subcutaneous wheal with local anesthetic is made and needle is advanced through the tendon sheath of extensor carpi radialis brevis to inject the solution.
Fig. 3.15: Schematic representation: common extensor origin on ultrasonography, lateral epicondyle (EP), radius (R)
Approach and position same as above transducer is kept longitudinally over lateral epicondyle and distal part of transducer over radius head.
Origin of common extensor is visualized and patient is asked to alternatively flex and extend the wrist to see the movements of common extensors at the region 69of hypoechoicity injection is provided. Head of radius is visualized by alternatively pronating and supinating forearm, swelling of tendon itself can be evaluated—more than 30% increase of thickness than opposite normal side. Calcification, bursa under inferior surface of extensor carpi radialis brevis is normally absent. Its presence indicates tendinitis. Peritendinosis (thickening of peritedon is also identified), enthesopathy or tendinosis is also noted due to thickening of tendon. But whatever is the finding there is no significant difference in effectiveness of therapy, so these abnormalities have no predictive value in treatment. It is correlated with pain in 75% patients only. Miller et al reported sensitivity of 64–82% and specificity of 67–100%. Connell et al found positive value in diagnosis of tennis elbow by USG in 95% patients.
Lateral ligament complex consists of radial collateral ligament, lateral ulnar collateral ligament (LUCL), annular ligament and accessory radial collateral ligament. Lateral ulnar collateral ligament is primary stabilizer of elbow. From posterior inferior aspect of lateral epicondyle extends to supinator crest of proximal ulna, it is deep to common extensor origin. There is posterolateral rotatory instability of elbow, if this is affected. Lateral epicondylitis can accompany LUCL insufficiency. Elbow flexed 90°–120°. Initially LUCL is lateral to radial head with cranial edge of probe placed on lateral epicondyle. Cranial end of probe placed at radial head and rotated 80°–90° and distal end scans ulna lateral aspect of supinator crest in both pronation and supination. Mean thickness of LUCL over radial head is 1.2 mm and at humeral attachment 1.7 mm.
Megnatic resonance imaging is not valuable in detecting injuries at LUCL.
The LUCL can be difficult to differentiate from radial collateral ligament in its proximal course. LUCL portion of ligament by sliding probe posterior on lateral epicondyle and identifying continuity with oblique course towards ulna. LUCL tear most commonly proximally, USG may have greater accuracy, best with elbow's 90°–100° flexion and neutral rotation with pronation and supination and tendon anisotropy are seen.
Dynamic images for posterior rotatory instability by stress testing of posterolateral rotatory complex is required (patients will usually have clinical tests for instability positive with symptoms of instability/give away and pain).
GOLFER ELBOW (SWIMMERS ELBOW OR EPITROCLEITIS) (FIG. 3.27)
Pain is on the medial aspect of elbow, worse on resisted forearm pronation/wrist flexion.
Maximum tenderness is at 5 mm distal and anterior to midpoint of medial epicondyle. Tenderness is seen at origin of flexor carpi radialis and pronator teres (flexor pronator group); other muscles commonly involved are flexor digitorum superficialis and flexor carpi ulnaris. Loss of ROM and flexion contracture may be presentation.
X-ray is normal.
Differential diagnosis: Ulnar nerve neuropathy and MCL instability.
Indications: Injection steroid seen to have short-term effect and medium-term effect, for long-term, exercises and splinting are preferred. But conservative 70treatment is effective in majority and in order to avert painful episodes. These injections are preferred prior to physiotherapy. Ultrasonography guided injections are preferred to avoid complications.
Position: Sitting position, arm directed at patients side and elbow extended/flexed with forearm supported on table, elbow held fully supinated and in extension with surgeon's thumb on most tender point.
Preparation: Elbow is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/ 1 ½ inch 25 gauge needle.
Most tender spot over flexor pronator group is felt.
Steroid anesthetic mixture is injected with needle thrust vertically downwards until tendon resistance is felt and droplets are injected.
Needle is then pushed down till the tip reaches bone and further droplets are injected at tenoperiosteal junction. By serial withdrawal and reinsertion, whole area is infiltrated.
Approach and position same as above transducer is kept longitudinally over medial epicondyle and distal part of transducer over ulna and coronoid process.
Origin of common flexor is visualized and patient is asked to alternatively flex and extend the wrist to see the movements of common flexors at the region of hypoechoicity injection is provided.
OLECRANON BURSISTIS: (MINERS ELBOW OR DRAFTSMAN'S ELBOW) (FIG. 3.27)
Two olecranon bursae are of clinical significance one that lies between tendon of triceps and posterior ligament of elbow and olecranon and other that is inflamed much more often lies between attachment of triceps to olecranon and skin. Mostly associated with crystal-induced disease.
More superficial bursa often is distended with fluid that tends to recur after aspiration often painful to pressure. When not distended and movable synovial/ fibrotic nodules may be palpable.
Most patients respond to conservative treatment for chronic bursits causing significant symptoms. Stewart et al advocated surgical treatment for long lasting benefit.
Olecranon bursa can also be seen on USG but can usually be identified without it because of superficial nature, when probe is kept over it. Olecranon is identified overlying which is subcutaneous tissue and thickened fluid filled bursa.
Olecranon bursa aspiration is considered in cases of suspected abscess. If non-infective condition is suspected, consider giving injections. USG guidance is useful rarely but in very small painful bursa. Usually steroid are preferred.
Position: Sitting position, arm directed at patient's side and elbow fully extended with forearm supported on table, elbow held fully supinated and in flexion with surgeon's thumb on most tender point.
Preparation: Elbow is painted with antiseptic solution and draped.
Drugs: 0.25% preservative free bupivacaine and 40 to 60 mg of methylprednisolone. Syringe: 2 ml/1½ inch 25 gauge needle. 22 gauge needle can also be used.
Bursa is very superficial. It is usually clearly visible, so direct entry is made into bursa as it lies in subcutaneous tissue. First aspirate and if fluid is nonpurulent and patient does not have infectious etiology then consider injecting steroid.72
ELBOW JOINT ASPIRATION (FIG. 3.27)
Indications: Elbow joint aspiration is considered in cases of suspected septic arthritis of elbow. If noninfective condition is suspected, consider giving injections under image intensifier guidance. Usually steroids are preferred.
It is last resort to all conservative means of management.
Position: Sitting/supine, midprone position of elbow, flexed forearm supported on table.
Preparation: Elbow is painted with antiseptic solution and draped.
Note that landmarks are easier to identify when elbow is first extended and then flexed.
Drugs: 2% preservative free lignocaine and 40 to 80 mg of methylprednisolone.
Syringe: 2 ml/ 1 ½ inch 22 gauge needle.
The part of joint nearest to the surface lies posteriorly between capitellum of humerus and head of radius. Head of radius can always be distinguished and needle is entered just proximal to head in direction towards anterior.
Sometimes there is risk of injury to radial nerve and triceps tendon. Ultrasound may aid in directing the needle.
Advance the needle slowly until aspirating the synovial fluid from the joint.
Elbow joint injection or aspiration C arm guided:
Same as above.
Position and approach same as above.
Needle is visualized in C arm.
CUBITAL TUNNEL SYNDROME (FIG. 3.27)
Entrapment neuropathy of ulnar nerve by aponeurotic band that runs from medial epicondyle of humerus to medial border of humerus. It bridges the dual origin of flexor carpi ulnaris, compression is more in elbow flexion.
In cubital tunnel syndrome tenderness is one inch below medial epicondyle. Ulnar nerve may be compressed in cubital tunnel against posterior aspect of medial epicondyle of humerus. It compressed externally while patient is in bed, on table, in armchair. Also seen after cubitus valgus deformity.
Patients presents with pain and paresthesia in medial forearm that radiate to wrist, ring and little finger.
In late stage, there could be flexion contracture of affected fingers (claw hand deformity) and ulnar innervated muscles. There is sensory loss at pulp of small finger.
Tenderness is present over ulnar nerve of elbow. Ulnar nerve is sometimes compressed more by deep fibers of flexor carpi ulnaris distally. Results are good in early stages and when compressive pathology like ganglion is found.
Indication: When patient has tingling of fingers or patients have disturbed sleep at night due to same are indications for giving injection locally. When patient has developed weakness or atrophy of hypothenar muscles or numbness the results of same are not good.
Technique
Position: Supine/sitting with arm fully adducted at patient's side and elbow flexed with dorsum of hard resting on a small pillow or folded towel to relax the affected tendons.
Sitting position, arm directed at patients side, elbow held fully supinated and in flexion with surgeon's thumb on most tender point.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/ 1½ inch 25 gauge needle.
Identify the olecranon and medial epicondyle then identify the sulcus, in between them insert needle proximal to sulcus and advance it in slightly cephalad direction through skin.
After advanacing ½ inch strong paresthesia is elicited in distribution of ulnar nerve, as paresthesia is felt, aspirate for presence of blood.
If aspiration test is negative and no persistent paresthesia, inject solution slowly.
If bone encountered then slightly withdrawn needle and reinjected and if no paresthesia is encountered, then inject the drug in flow.
In inflammatory condition cortical changes if present takes form of spurs and or microerosions. The insertion of muscles show an increase in convexity at insertion. Coarse irregularities of structure with increase of fiber component.76
Adjacent tendons may show tendinotic change and nerve may show compression, also it is necessary as not to damage the superficial branch of median nerve.
There may be intracompartmental ganglion.
Injection is given with needle tip beside the nerve and not in the nerve. In synovitis, post-traumatic or inflammatory, the arthritic compartment may be regular hypoechoic or hyperechoic increase in volume of joint space which may present with fine internal echogenicity. Transducer is kept with one end over medial epicondyle and other at olecranon. Ulnar nerve is visualized and approach and technique same as above is applied.
POSTERIOR INTEROSSEOUS NERVE SYNDROME
The posterior interosseous nerve (PIN) may get entrapped as it courses under arcade of Frohse and enters supinator muscles, there might be lipoma, ganglia, or fibroma, or traumatic cause (fracture of forearm, bones fracture and dislocation of elbow, Volkman's ischemic contracture). Hallmark is abnormal swelling of involved nerve and abrupt caliber change at entrapment site (but this should not be interpreted as entrapment without change in nerve area). Compression sites may be – origin of ECRB, arcade of Frohse, adhesion around radial head and radial recurrent arterial fan.
There is pain in elbow, partial wrist drop, all extensors of forearm are affected except brachioradialis and extensor carpi radialis longus.
Chronic entrapment of radial nerve may cause tennis elbow like picture—known as radial tunnel syndrome (Chronic and refractory tennis elbow).
Radial tunnel is formed by brachioradialis, extensor carpi radialis brevis, extensor carpi radialis longus, medial wall by biceps tendon and brachialis. Floor of tunnel is formed by capsule of radiocapitellar joint, it is 5 cm long lies over anterior aspect of radius. Patients present with pain in region of radial nerve distal to radial head beneath extensor mass. Pain increases on resistive active forearm supination. It may radiate proximally or distally.
Indication: When patient has tingling of fingers or patients have disturbed sleep at night due to same are indications for giving injection locally. When patient has developed weakness or atrophy of hypothenar muscles or numbness, the results of same are not good.
Technique
Position: Supine/sitting with elbow flexed with dorsum of hand resting on a small pillow or folded towel to relax the tendons.
Sitting position, arm directed at patient's side, elbow held fully supinated and in flexion with surgeon's thumb on most tender point.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml 1½ inch 25 gauge needle.
Identify the point 5 cm distal to the lateral epicondyle on pressing of which tenderness can be felt. After advanacing ½ inch, aspirate for presence of blood. If aspiration is negative, inject solution slowly.78
If bone encountered then slightly withdrawn needle and reinjected, drug is injected in flow.
Transducer is kept with one end over point 5 cm distal to lateral epicondyle and along direction of brachioradialis till radial nerve is appreciated. Technique and approach same as above is applied.
CHEIRALGIA PARESTHETICA
It is compression of sensory branch of radial nerve at edge of brachioradialis (7 cm proximal to radial styloid process) caused by tight watch bands, hand cuffs, tight cast patient presents with pain and burning over dorsoradial aspect of proximal forearm and wrist and altered sensibility of dorsal thumb web space. There is no motor involvement and Tinel sign is present. Palmar flexion and ulnar deviation increases symptoms.
Biceps insertion—starting from myotendinous junction distally look for hypoechoicity, enlarged rounded bursa, hematoma.
Indication: When patient has tingling of fingers or patients have disturbed sleep at night due to same are indications for giving injection locally. When patient has developed weakness or atrophy of hypothenar muscles or numbness the results of same are not good.
Technique
Position: Supine/sitting with elbow flexed with dorsum of hand resting on a small pillow or folded towel to relax the tendons.
Sitting position, arm directed at patient's side, elbow held fully supinated and in flexion.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml 1½ inch 25 gauge needle.
Identify the point after advanacing ½ inch, paresthesia in region of sensory distribution of radial nerve is felt, i.e. at dorsal medial half of palm till middle phalanx. Aspirate for presence of blood. If aspiration is negative, inject solution slowly.
Fig. 3.27: Schematic representation of sites of pain or tingling/numbness in various elbow conditions
If bone encountered then slightly withdrawn needle and reinjected, if not drug is injected in flow.
Transducer is kept with one end over point 7 cm proximal to radial styloid and along direction of brachioradialis till superficial radial nerve is appreciated. Technique and approach same as above is applied.
FUTHER READING
- Andrews JR, Whiteside JA. Common elbow problems in the athlete. J Orthop Sports Phys Ther. 1993;17:289.
- Azar FM. Elbow. In: Miller MD, Cooper DE, Warner JJP, (eds). Review of Sports Medicine and Arthroscopy, Philadelphia: Saunders. 2002.
- Bisset L, Beller E, Jull G, et al. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ. Sep 29 2006.
- Boyd HB, McLeod Jr AC. Tennis elbow. J Bone Joint Surg. 1973;55A:1183.
- Burnham R, Gregg R, Healy P, et al. The effectiveness of topical diclofenac for lateral epicondylitis. Clin J Sports Med. 1998;8:78.
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics. Vol 3. 11th ed. Mosby Inc. 2008. pp. 2339-77.
- Cardone DA, Tallia DF. Diagnostic and therapeutic injection of the elbow region. American Family Physician. 1 December 2002.
- Chung B, Wiley JP. Effectiveness of extracorporeal shock wave therapy in the treatment of previously untreated lateral epicondylitis: a randomized controlled trial. Am J Sports Med. 2005;33:461.
- Coonrad RW, Hooper WR. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg. 1973;55A:1177.
- Dlabach JA, Baker CL. Lateral and medial epicondylitis in the overhead athletes. Oper Tech Orthop. 2001;11:46.
- Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surg. 2003;28:272.
- Gellman H. Tennis elbow (lateral epicondylitis). Orthop Clin North Am. 1992;23:75.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. 1st ed. 2007. pp. 25-112.
- John O Neill. Musculoskeletal Ultrasound Anatomy and Technique. Springer Inc. 2008. pp. 20-330.
- Kannus P, Jozsa L. Histopathological changes preceding spontaneous rupture of a tendon: a controlled study of 891 patients. J Bone Joint Surg. 1991;73A:1507.
- Kelley JD, Lombardo SJ, Pink M, et al. Electromyographic and cinematographic analysis of elbow function in tennis players with lateral epicondylitis. Am J Sports Med. 1994;22:359.
- Labelle H, Guibert R, Joncas J, et al. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow: an attempted meta-analysis. J Bone Joint Surg. 1992;74B:646.
- Mills GP. The treatment of “tennis elbow”. BMJ. 1928;1:12.
- Nathan PA. Surgical treatment of ulnar nerve entrapment at the elbow. J Hand Surg. 1992;18B:245.
- Newey ML, Patterson MH. Pain relief following tennis elbow release. J R Coll Surg Edinb. 1994;39:60.
- Nicola TL. Elbow injuries in athletes. Prim Care. 1992;19:283.
- Nirschl RP, Ashman ES. Tennis elbow tendinosis (epicondylitis). Instr Course Lect. 2004;53:587.
- Nirschl RP. Elbow tendinosis/tennis elbow. Clin Sports Med. 1992;11:851.
- Nirschl RP. Lateral extensor release for tennis elbow. J Bone Joint Surg. 1994;76A:951.
- Noteboom T, Cruver R, Keller J, et al. Tennis elbow: a review. J Orthop Sports Phys Ther. 1994;19:357.
- Osgood RB. Radiohumeral bursitis, epicondylitis, epicondylalgia (tennis elbow). Arch Surg. 1922;4:420.
- Porretta CA, Janes JM. Epicondylitis of the humerus. Mayo Clin Proc. 1958;33:303.
- Regan W, Wold LE, Coonrad R, et al. Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med. 1992;20:746.
- Rifat SF, Moeller JL. Basics of joint injection: General techniques and tips for safe, effective use. Postgrad Med. Jan 2001;109(1):157-60, 165-6.
- Rifat SF, Moeller JL; Site-specific techniques of joint injection. Useful additions to your treatment repertoire. Postgrad Med. Mar 2001;109(3):123-6, 129-30, 135-6.
- Rumack C, Wilson S, William J. Diagnostic Ultrasound. Vol 1. 2nd edition. Mosby Inc. 1998. pp. 843-83.
- Silver T. Joint and Soft Tissue Injection: Injecting with Confidence (4th edition) 2007 Radcliffe Publishing. 1992;74:646-51.
- Solbiati L, Rizzatto G, Ultrasound of Superficial Structures, 1st edition. Chirchill Livingstone. 1995 pp. 279-375.
- Trethowan WH. Tennis elbow. BMJ. 1929;2:1218.
- Verhaar JA. Tennis elbow: Anatomical, epidemiological and therapeutic aspects. Int Orthop. 1994;18:263-7.
- Wadsworth TG. Lateral epicondylitis. Lancet. 1972;1:959.
- Watson Buchaman W. Clinical Examination of Musculoskeletal System. Williams and Wilkins. 1st edition. 1997. pp. 25-82.
- Wilk KE, Arrigo C, Andrews JR. Rehabilitation of the elbow in the throwing athlete. J Orthop Sports Phys Ther. 1993;17:305.
Skin on hand and wrist is fixed to bone by septa. There are small ligament running from skin to bone along the lateral and medial sides of fingers (Cleland's and Grayson's ligament).
Palpation of wrist begins with palpation of radial styloid process (easily palpable), laterally when hand is in anatomical position (palm facing anteriorly).
Flexor carpi radialis originates from common flexor origin on medial epicondyle of humerus and inserted at bases of second and third metacarpals. Its action is flexion and radial deviation of wrist, supplied by median nerve.
Flexor digitorum superficialis originates from medial epicondyle of humerus, medial ligament of elbow, medial border of coronoid process of ulna, fibrous arch connecting coronoid process of ulna with anterior oblique line of radius and inserted to volar aspect of middle phalanges of fingers. Its action is flexion of proximal interphalangeal joints, metacarpophalangeal joints, and wrist joint supplied by median nerve.
Flexor pollicis longus originates at middle part of anterior surface of radius and inserted into distal phalanx of thumb. It is main flexor of thumb and supplied by anterior interosseous nerve.
Pronator quadratus originates at lower fourth of volar surface of ulna and inserted into lower fourth of lateral aspect of radius. Its action is weak pronation of forearm. It is supplied by anterior interosseous nerve.
Palmaris longus originates at common flexor origin on humerus and is inserted to palmar aponeurosis. It is weak flexor of wrist supplied by median nerve.
Flexor digitorum profundus originates at upper three-fourths of anterior surface of ulna and inserted to distal phalanges of fingers. It is flexor of distal interphalangeal joints, proximal interphalangeal joints, metacarpophalangeal joints and wrist joint. It is supplied by median and ulnar nerves.82
The ulnar artery usually enters the forearm deep to the pronator teres before angling medially across the forearm and passing under the fibrous arch of the flexor digitorum superficialis, where it runs just deep to the median nerve.
From the ulnar to the radial side of the forearm, they consist of the anconeus, the extensor carpi ulnaris, the extensor digiti minimi, and the extensor digitorum communis.
Three muscles cross forearm from ulnar to radial side, and two of them (the abductor pollicis longus and the extensor pollicis brevis) gaseous matter around lateral aspects of radius.
Brachioradialis originates from upper two-thirds of lateral supracondylar ridge of humerus and inserted to styloid process of radius. Its action is flexion of elbow and pronation and supination of forearm, supplied by radial nerve.
Mobile wad of three is formed by brachioradialis, extensor carpi radialis brevis and longus. Initially palpated on lateral epicondyle.
For brachioradialis, patient is made to close fist placed in neutral position under edge of table and then lift up against weight of table.
Superficial radial nerve runs down the forearm under the brachioradialis muscle.
Extensor carpi radialis longus and brevis are palpated by asking patient to make fist and resist extension of flexed wrist. They are traced distally to proximal part of 2nd and 3rd metacarpal.
Abductor pollicis longus originates at posterior surface of ulna, and posterior interosseous membrane, and inserted to base of thumb metacarpal. It is abductor and extensor of thumb. It is supplied by posterior interosseous nerve.
Extensor pollicis brevis originates at posterior surface of radius and interosseous membrane and inserted to base of proximal phalanx of thumb. It is extensor of proximal phalanx of thumb.
Extensor carpi radialis brevis originates at common extensor origin on lateral epicondyle of humerus and radial collateral ligament of elbow. It is inserted to base of third metacarpal. It is extensor and radial deviator of wrist. Supplied by radial nerve.
Radial artery crosses wrist joint on its lateral aspect. Lister's tubercle lies on dorsum of wrist. When palpated from radial styloid process, it is felt as a bony prominence medial to it. Radius articulates with proximal carpal row. Tendon of extensor pollicis longus muscle angles around its distal end, changing direction about 45°. It overlies distal radioulnar joint.
Tendon of palmaris longus distal end bisects anterior surface of the carpal tunnel. It is easy to palpate in distal forearm, if the patient is instructed to pinch the fingers together and flex the wrist. Flexor retinaculum is a thickening of deep fascia across in front of wrist. Its upper border corresponds to distal transverse skin crease in front of wrist and is continuous with deep fascia of forearm. Its lower border is attached to palmar aponeurosis, medially it is attached to pisiform bone and hook of hamate, and laterally to tubercle of scaphoid and trapezium bones where its forms tunnel for passage of tendon of flexor carpi radialis.
Motor branch of median nerve usually arises from anterolateral side of the median nerve just as the nerve emerges from carpal tunnel. It then curves radially 83and upward to enter thenar musculature between abductor pollicis brevis and flexor pollicis brevis.
Palmar cutaneous branch of median nerve arises 5 cm proximal to wrist joint and runs down along ulnar side of tendon of flexor carpi radialis muscle before crossing the flexor retinaculum.
Recurrent branch of median nerve to muscle of thenar eminence curves around lower border of flexor retinaculum and lies about 1 finger breadth distal to tubercule of scaphoid.
Superficial palmar arch crosses the palm at the level of distal end of the outstretched thumb. Carpal tunnel is a fibro-osseous canal on volar surface of carpus. Its base is formed by the volar aspect of carpal bones, and its roof is formed by the flexor retinaculum. Within carpal tunnel, the tendons to middle and ring fingers are superficial to tendons of index and little fingers.
Tendons of flexor digitorum profundus (FDP) lie deep to tendons of flexor digitorum superficialis (FDS). Trapezium lies on radial side of carpus, where it articulates with first metacarpal. To palpate ridge, identify joint between trapezium and thumb's metacarpal bone by moving joint passively. Ridge feels like a prominent lump on trapezium.
If patient is asked to flex the wrist against resistance, thicker and radially located tendon of flexor carpi radialis can be palpated. Flexor carpi ulnaris (FCU) originates from two heads. Humeral head: from common flexor origin on medial epicondyle of humerus. Ulnar head: from medial border of olecranon and inserted to hamate and fifth metacarpal, it is flexor and ulnar deviator of wrist. Also weak flexor of elbow, supplied by ulnar nerve.
Pisiform is a sesamoid bone of flexor carpi ulnaris tendon, so flexor carpi ulnaris is traced distally to find pisiform bone. Ulnar nerve runs down the medial side of forearm, on volar surface, between flexor digitorum profundus and flexor digitorum superficialis, and under flexor carpi ulnaris. Ulnar nerve enters the hand superficial to the flexor retinaculum within canal of Guyon.
Ulnar artery lies on its radial side. Just proximal to wrist, ulnar artery and nerve emerge from under muscle to pass over flexor retinaculum (transverse carpal ligament) of wrist.
Artery is the most lateral structure, then nerve, and, finally, tendon of flexor carpi ulnaris. Canal of Guyon has four boundaries: A floor, the flexor retinaculum (transverse carpal ligament); a medial wall, pisiform; a lateral wall, hamate; and a roof, volar carpal ligament. There is superficial transverse carpal ligament anteriorly; deep transverse carpal ligament is posterior, pisiform and pisohamate ligament medially.
It is covered by pisohamate ligament, contains ulnar nerve and artery. It is found between two transverse crease on medial side of anterior aspect of wrist. Hook of hamate is slightly distal and radial to pisiform felt on deeply palpating hypothenar eminence.
Within carpal tunnel, median nerve lies superficial to tendons of flexor digitorum profundus and flexor pollicis longus muscles. Superficialis tendons lie toward ulnar side of the nerve.
Volar digital artery runs with digital nerve on its inner side.
- A1 pulley lies over metacarpophalangeal joint. A2 pulley lies over proximal end of proximal phalanx. A3 pulley lies over proximal interphalangeal joint.
- C1 pulley lies over middle of proximal phalanx.
- Tendons enter each fibro-osseous canal with superficialis tendon on top of profundus tendon.
- Profundus tendon.
- Short vinculum runs to tendon close to distal phalanx.
- Long vinculum passes to tendon from superficialis tendon at the level of proximal phalanx.
- Superficialis tendon.
- Short vinculum runs to tendon onto middle phalanx.
- Long vinculum is a double vinculum passing to tendon from palmar surface of proximal phalanx.
Volar aspects of flexor tendons are largely avascular; nutrition is derived from synovial fluid: distal palmar crease corresponds roughly to palmar location of metacarpophalangeal joints and location of proximal (A1) pulley, palmar digital crease marks palmar location of A2 pulley, proximal interphalangeal crease marks proximal interphalangeal joint, and thenar crease outlines the thenar eminence.
Metacarpals: The 2nd and 3rd metacarpals are closely anchored firmly to carpus, they are immobile for stability. The 4th and 5th metacarpals serve purpose of making fist, palpated on ulnar side of hand useful for grip. The 1st metacarpal is palpated from anatomical snuff box to metacarpophalangeal joint.
ANATOMICAL SNUFF BOX (FIG. 4.41A)
It lies just dorsal and distal to radial styloid. Thumb is extended for making its borders prominent. Scaphoid lies in floor of snuff-box. Radial pulse is palpable in floor of snuff-box, just on scaphoid. First metacarpal is palpated between snuff-box and metacarpophalangeal joint.
Superficial radial nerve is at risk in approaching this area. Because it lies directly over tendon of extensor pollicis longus muscle.
On radial side is abductor pollicis longus and extensor pollicis brevis. At ulnar border of snuff box lies extensor pollicis longus and navicular contents are deep branch of radial artery and superficial radial nerve. In this zone lies 1st tunnel of wrist containing abductor pollicis longus and extensor pollicis brevis at their insertion. Extensor pollicis brevis lies ulnar to abductor pollicis longus.
Tubercle of scaphoid is small protuberance, difficult to palpate just distal to distal end of radius on volar aspect of wrist joint. On the volar aspect of wrist serially are radial artery, flexor carpi radialis tendon, palmaris longus tendon, flexor digitorum superficialis tendon, ulnar artery, flexor carpi ulnaris tendon and ulnar nerve medial to ulnar artery.
Interphalangeal crease of thumb is surface marking for thumb interphalangeal joint. It lies just proximal to the distal end of the fibrous flexor sheath of thumb.
Wrist creases: There are 2 creases just proximal to thenar and hypothenar eminence; proximal is at level of proximal portion of transverse carpal ligament.85
Superficial palmar arch is 3 finger breadths distal to this crease and deep arch is two finger breadths distal to crease.
Metacarpophalangeal creases lie 2 cm distal to metacarpophalangeal joint. Interphalangeal creases lie at level of interphalangeal joint. The metacarpophalangeal joint is 1.3 cm distal to prominence of knuckle. Proximal interphalangeal joint is 0.6 cm distal to prominence of joint. With finger flexed to make a fist, prominences at joint are formed by proximal bone.
Lister's tubercle (dorsal tubercle of radius) is palpable as a bony prominence on dorsal surface of radius proximal to radiocarpal joint space, at junction of radial and middle third of wrist. Lunate bone lies distal to tubercle. Extensor pollicis longus tendon lies either within a groove on tubercle or on its ulnar aspect and can be felt moving on extension of thumb. Pisiform bone lies between the two transverse creases on the volar and medial aspect of wrist.
Proximal transverse crease on the volar wrist lies at level of wrist joint, and distal crease lies at proximal aspect of flexor retinaculum.
Apposition of thumb and fifth finger will accentuate a plane between thenar and hypothenar muscles. Median nerve is located between this plane and wrist crease.
The dorsal hoods are present over dorsal “knuckles”.
Extensor retinaculum attaches to pisiform and triquetral bones, but not to ulna. It functions as an anchor, restraining the extensor tendons of the forearm distally, extensor retinaculum divides into fibrous septa that pass compartment 1 is most radial or lateral compartment. It lies over lateral surface of distal radius tip and contains abductor pollicis longus and extensor pollicis brevis (EPB) tendons lying in separate synovial sheaths. Groove on the ulnar side of Lister's tubercle contains extensor pollicis longus tendon, compartment 3, invested with its own synovial sheath. Compartment 2 harbors tendons on radial aspect of Lister's tubercle, extensor pollicis longus and brevis, with brevis closest to tubercle. Each tendon is contained in its own synovial sheath.
On radial side of tubercle, we initially encounter radial extensors and as we approach the thumb, pollicis tendons. Compartment 4 is located on ulnar aspect of extensor pollicis longus (EPL) in a groove in which all four tendons of common extensor tendon lie. These are in intimate contact over the extensor indicis tendon; all surrounded by a common synovial sheath.
Compartment 5 lies over distal radioulnar joint and contains extensor digiti minimi in its own synovial sheath. Compartment 6 is located in groove near the base of ulnar styloid through which extensor carpi ulnaris (ECU) passes.
Superficial extensor tendons of fingers extend over dorsum of hand and attach to deep fascia and interconnect near the metacarpal heads by oblique fibrous bands.
FLEXOR COMPARTMENT WRIST
Palmar aponeurosis is an extension of degenerated tendon of palmaris longus from the distal border of the flexor retinaculum. It expands toward the bases of fingers. It divides into four separate slips going to each finger. Each slip divides 86into two bands, inserting into proximal phalanges, flexor sheaths and deep transverse ligament. Dupuytren's contracture involves contraction of aponeurosis or slip resulting in a fixed flexion deformity.
The radial aspect of flexor retinaculum splits into two layers, forming a tunnel through which tendon of flexor carpi radialis pass. Many muscles of thenar and hypothenar eminences arise from the retinaculum. Ulnar aspect of retinaculum joins pisiform-hamate ligament. Flexor carpi ulnaris tendon lies separately within Guyon's canal adjacent to ulnar nerve and medial to ulnar artery.
Four superficial flexor tendons pass through it in two rows with middle and ring finger tendons lying to index and little finger tendons. Tendons of flexor digitorum profundus, however, all lie in the same plane. Tendon to index finger is separate, while other three tendons are joined and split free only when they reach the palm. All flexor tendons are encased in a common synovial sheath. Median nerve enters carpal tunnel and deep to flexor retinaculum anterior to the flexor tendons, covered by a fibrofatty layer. An important normal variant is presence of a persistent prominent median artery that is often accompanied by a bifid median nerve. Tendon of flexor pollicis longus in its own synovial sheath and passes through radial side of carpal tunnel.
Median nerve lies closer to radial aspect of carpal tunnel and superficial to flexor tendons during dynamic flexion and extension of the fingers.
FINGER FLEXOR TENDON PULLEY SYSTEM
Flexor synovial sheath extends from neck of metacarpal to distal interphalangeal joint. Retinacular structures are thicken sheath at five specific points, form annular pulley system (pulleys A1-A5). Additional fibers that crisscross between annular pulleys create cruciate pulley system (pulleys C1-C3). These combine to prevent excursion of flexor tendons from metacarpophalangeal and interphalangeal joints during finger flexion.
The A1 pulley begins in region of volar plate of metacarpophalangeal joint and extends to level of base of proximal phalanx.
TRIANGULAR FIBROCARTILAGE COMPLEX
The triangular fibrocartilage complex (TFCC) is composed of dorsal and volar radioulnar ligaments, articular disc or triangular fibrocartilage (TFC), ulnolunate ligament, lunotriquetral ligament, ulnar collateral ligament, and meniscus homolog. It is part of extrinsic carpal ligament group. The dorsal and volar radioulnar ligaments reinforce peripheral portion of articular disc, which is thinned centrally and thickened peripherally.
The TFC has a variable appearance and attaches to sigmoid notch of radius and to ulnar styloid process. Ulnolunate ligament extends from volar radioulnar ligament to volar aspect of lunate; lunotriquetral ligament originates ulnar to ulnolunate ligament and attaches to volar aspect of triquetrum. Ulnar collateral ligament represents a thickening of capsule that extends from ulnar styloid process 87to triquetrum and pisiform. Meniscus homolog is composed of connective tissue that forms distal to ulnar aspect of TFC, between dorsal radioulnar ligament and radial aspect of extensor carpi ulnaris (ECU) tendon.
Patient is positioned with elbow flexed, forearm in pronation, and wrist in a neutral position or slightly flexed, resting on a roll of towel or sponge.
Muscle position examined.
- Abductor pollicis longus, extensor pollicis brevis, abductor pollicis brevis—Wrist in neutral position with transducer radially.
- Adductor pollicis—Transducer dorsally using oblique angle between bases of first and second metacarpals with thumb extended.
- Extensor pollicis longus Compartment 3—Dorsal approach on the ulnar side of Lister's tubercle.
- Extensor indicis Compartment 4— Transducer dorsally with common extensor tendons; move index finger to isolate the tendon.
- Flexor digiti minimi brevis— Transducer volarly with hypothenar component of hand.
- Flexor pollicis brevis—Volar approach with thenar component of hand.
- Flexor pollicis longus—Volar approach at level of carpal tunnel.
- Dorsal interosseous muscles of the hand—Dorsal approach at level of metacarpal heads.
- Palmar interosseous muscles of the hand— Transducer volarly at level of metacarpal shafts.
- Confirmation that correct tendon had being identified can be determined by dynamically moving its attachment area.
FLEXOR TENDONS AND CARPAL TUNNEL
Transducer should be perpendicular to tendons, in transverse plane, as anisotropic effect will cause the tendons to appear hypoechoic, simulating synovial fluid and leading to an erroneous diagnosis of tenosynovitis. Median nerve is located superficial to flexor tendons, and its size, shape, echogenicity, and relationship to underlying tendons and overlying retinaculum be noted. Dynamic movement, including flexing and extending fingers, shows that median nerve is less mobile than adjacent tendons and can be seen “bouncing” on tendons below. If there is doubt, it can be traced proximally into the forearm where it can be seen emerging from between superficialis and profundus tendon layers. Circumference of median nerve can be measured at proximal and distal carpal tunnel in transverse plane. Proximal carpal tunnel is defined in transverse plane by scaphoid tubercle and pisiform and distal carpal tunnel is defined by trapezium and hook of hamate. Mean cross-sectional area of median nerve is usually obtained at proximal carpal tunnel and should be less than or equal to 10 mm. Maximum flattening ratio of nerve (ratio of maximum transverse diameter to its anteroposterior diameter) is best obtained in transverse plane at level of hamate. This is at level of distal carpal tunnel and reflects maximum, flattening and constriction of nerve between flexor tendons and transverse carpal ligament. Normal ratio should be less than 3. Bifid median nerve, a normal variant usually accompanied by a persistent median artery, will give false-positive results. 88
Guyon's Canal
Bony landmarks are pisiform proximally and hook of hamate distally. It is easiest to first locate ulnar artery with Doppler and then proceed to locate nerve.
Triangular Fibrocartilage Complex
Patient is positioned elbow flexed, forearm in pronation, and wrist in mild radial deviation.
Scanning is performed initially locating bony landmarks—distal ulna proximally and triquetrum distally, then angle probe toward radial aspect, and finally move sweep toward ulnar aspect of articular cartilage. A hyperechoic triangle, TFC, seen with base closest to ECU and apex attaching to radius comparison with opposite side is necessary for diagnosis of subtle tears. Not to mistake more proximal homolog, having a triangular echogenic appearance similar to articular disc. A hypoechoic line is commonly seen between homolog and true articular disc. This results in diagnosis of a false tear. In transverse plane, it is important to examine ECU for pathology that can cause pain. ECU tendon should be used as a window to assess TFC. Tip of TFC, resembles an echogenic triangle, should be traced to tip of radius pathology to ECU can simulate a tear to TFC.
In trigger fingers, transducer should be placed usually at level of distal metacarpals, using controlled extension against resistance. Tendon and/or tendon synovium can be seen caught under A1 flexor pulley during dynamic real time motion. Flexor and extensor tendons of fingers should be examined dynamically.
Pulley injury seen with flexor tendon displaced from underlying phalanx, resembling a bow.
Radial nerve is identified at lateral epicondyle, on radial aspect of elbow. It lies in a groove between brachialis and brachioradialis muscles. From this position, its branches can be followed into proximal forearm. The posterior interosseous nerve course in proximal forearm. At elbow joint, the ulnar nerve is identified adjacent to the medial epicondyle in cubital tunnel, and can be followed into the forearm. In distal half of the forearm, ulnar nerve is superficially located, just below skin and fascia, accompanied by ulnar artery. It is easily identified at wrist, adjacent to ulnar artery, in Guyon's canal.
The median nerve in forearm is identified at junction of medial and middle third of antecubital fossa at elbow, medial to brachial artery. Distally it can be followed through forearm to decussation at volar aspect of wrist. With forearm positioned in supination, median nerve can be easily traced, either in short or long axis, into cubital fossa region. If difficulty is encountered in identifying nerves versus tendons, in dynamic evaluation note that nerves show far less movement with muscle action than tendons.
Brachioradialis is examined with elbow joint in partial extension. It can be traced from above elbow, as it extends superficially and distally into forearm. Extensor carpi radialis longus (ECRL) and brevis (ECRB) are easier to trace 89proximally from wrist—located in compartment 2. Conjoint flexor tendon is located on the medial epicondyle.
Extensor
Extensor compartment is assessed with the forearm in pronation muscles seen from their common origin at lateral epicondyle. The conjoint extensor tendon is located in a deep position.
- Mobile wad contains two wrist extensors and one forearm flexor.
- Volar compartment contains muscles that flex the wrist and digits and pronate the forearm.
- Dorsal compartment contains muscles that extend the wrist and digits.
Indications: Wrist joint injections are effective in post-traumatic arthritis and rheumatoid synovitis. Those with severe pain and restriction of range of motion and those during rehabilitation periods. These injections have shone not to have long-term efficacy. Usually given under image intensifier guidance. Used for those unfit/not willing for surgery. Always rule infective affection of joint.
Technique
Position: Sitting with hand supported on table and wrist pronated.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Wrist is approached on dorsal side.
- Between 3rd and 4th extensor compartment most commonly used.
- Between 4th and 5th extensor compartment.
Alternatively:
In supine position with arm fully adducted at patient's side and elbow slightly flexed with palm of hand resting on a small pillow.
Here midcarpus at proximal part of indentation of capitate bone is approached. Needle is advanced through this point. Needle is introduced posteriorly immediately below lower end of radius between tendons of extensor indices and extensor pollicis longus.
Alternatively identify lister tubercle and needle is inserted just distal to lister tubercle and ulnar to extensor pollicis longus tendon.91
Ultrasonography is best done in transverse plane because of proximity of multiple affected tendon or compartment is identified on dorsal aspect of lister tubercle.
Transducer is kept at wrist joint line and joint space is visualized. Position of patient and approach remains same as above.
Similarly, wrist joint is visualized under C-arm and needle is inserted under C-arm guidance, approach and position of patient remains same as above chronic retinacular friction lead to painful hypoechoic tendinopathy, tendon swelling and retinacular and synovial thickening (Fig. 4.3).
DISTAL RADIOULNAR JOINT
Indications: Intra-articular injections are effective in post-traumatic arthritis and rheumatoid synovitis for those patients who require surgery, those with severe pain and restriction of range of motion and those during rehabilitation periods. These injections have shone not to have long-term efficacy. Usually given under image intensifier guidance.
Technique
Position: Sitting with hand pronated on table.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml. 1 ½ inch 25 gauge needle.
Head of ulnar is felt by moving ulna back and forth on radius. The line of cleavage can be identified between them. Point is chosen on this line 5 mm proximal to lower edge of ulna.
Here joint space is not more than 1 cm long so insertion is made at midpoint. Needle is thrusted down for 1.5 cm. If no bony resistance felt, then needle is in joint space.
Similarly, C-arm guided injection can be given. Position of patient and approach remains same.
First described by Sir James Paget, median nerve is found at proximal flexor crease of wrist between palmaris longus and flexor carpi radialis tendon, closer to latter; if patient does not have palmaris longus tendon, in which case the nerve is just radial to flexor sublimis tendon of fingers, which usually lies below palmaris longus tendon.
Butchers, mechanics, musicians, dental hygienists, tennis players and golfers are vulnerable. Women are more likely than men to develop it. Individuals with rheumatoid arthritis are also at high risk. It is seen more common in pregnancy. Rheumatoid arthritis, diabetes, gout, myxoedema, acromegaly hypothyroidism, malunited colles fracture, ganglion in carpal region, idiopathic, connective tissue disorders, alcoholism, wrist contusions.92
It is due to compression of median nerve as it passes through carpal tunnel at wrist. Synovitis of tendons in carpal tunnel produces pressure on nerve. Marshall and Tariff showed that local steroid injection for carpal tunnel syndrome provides greater clinical improvement in symptoms 1 month after injection compared to placebo and not thereafter.
Symptoms tend to be worse at night and may disturb sleep, or in the morning. Hanging hand out of bed or shaking it around will often relieve pain and tingling.
Patient may have symptoms throughout day. Hand may feel weak, or the fingers numb, or both and patient may have a tendency to drop things.
Positive Phalen's test and tourniquet test help in diagnosis. Electrodiagnosis in form of EMG NCV is useful.
It provides relief of symptoms up to 3 months after treatment compared to oral steroids. Results are not good when there is generalized synovitis and in late stages of disease.
In carpal tunnel syndrome, local steroid does not provide complete relief for greater than nine months compared to NSAIDs and splinting technique.
Injection of steroids into carpal tunnel an effective method of treatment in short-term; local steroid injection is just as effective as surgery for long-term symptomatic relief of carpal tunnel syndrome—for a year, at least—and actually more effective over the short-term.
If steroid is injected directly into median nerve, dysesthesias may occur and persist for several weeks. Note that steroid injections into carpal tunnel may temporarily “normalize” nerve conduction studies, and therefore the physician may consider delaying a steroid injection until the NCS is completed.
Indications:
- No profound sensory loss
- No thenar atrophy
- Only slightly prolonged nerve-conduction latencies.
Patients with intermittent symptoms with no sensory deficits or thenar weakness with duration of complaints less than 1 year. Injection with splinting is helpful. Steroid will reduce inflammation to tendons and thereby decrease pressure on 95median nerve. Ultrasonography guided injections are affective. Usually steroids are preferred. It will not be useful for solid/cystic swelling like ganglion. Useful in those not fit for surgery.
Technique
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
First, locate the flexor carpi radialis (FCR) and palmaris longus (PL) tendons. The palmaris longus tendon is medial to flexor carpi radialis and is best located by opposing the thumb and fifth digit while the wrist is flexed. Wheal ulnar to the palmaris longus and proximal to proximal wrist crease avoid going directly into nerve, and if paresthesias are elicited, needle should be withdrawn and placed more ulnarly or radially; Insert needle 1 cm proximal to wrist flexion crease and 3–5 mm from ulnar side of palmaris longus if palmars longus is absent. Direction of needle may be aligned with ring finger (Fig. 4.4).
If contact is made with the palmaris longus tendon while advancing the needle, retract slightly and redirect. The use of a needle smaller in diameter may require increased effort and slower injection time but dramatically reduces pain at the site of injection.
Direct needle towards hand at 30°–45° angle.
Flex finger fully into palm. Advance needle approximately 1–15 cm until resistance is felt. If paresthesias are felt, redirect the needle. Instruct patient tips of ring and little finger. If slight movement of tip of needle occurs, needle is safely positioned.
Ask patient to extend finger while applying pressure to syringe.
Distal excursion of ring and little flexor tendon will carry needle into carpal tunnel.
If tingling occurs, needle has entered nerve; do not continue with injection.
Inject 1–2 ml of local anesthesia into carpal canal.
If resistance is encountered in injecting, it indicates that tip of needle is embedded in flexor tendon.
Maintain same pressure in syringe while serially withdrawing needle until anesthetic drug flows freely. Leave needle in place and change syringes. Inject 1 ml of corticosteroid into carpal canal; and remove needle.
Risk: Intraneural injection.
After care: Finger may be numb for 1–2 hours following injection and takes several days to take effect.
Injection for carpal tunnel USG guided.
Nerve is less echogenic then tendon. This phenomenon can be used in identifying carpal tunnel and median nerve in it.
Probe kept at wrist with wrist in minimal flexion show tendons in ulna bursa (which is less echogenic) with overlying median nerve with moderate echogenoicity and over which lies flexor retinaculum (Figs 4.5 to 4.8).96
Normal palm of hand show echogenic superficial and deep flexor tendons of fingers adjacent to hypoechoic lumbrical muscle and Doppler imaging show adjacent digital arteries.
Entry point of needle, approach and position of needle remains same as above.
FIRST CARPOMETACARPAL JOINT (FIG. 4.9)
Indications: Intra-articular injections are effective in post-traumatic arthritis and rheumatoid synovitis, for those patients who require surgery with severe pain and restriction of range of motion and those during rehabilitation periods. These injections have shone to have long-term efficacy. Usually done accurately under image intensifier guidance.
Technique
Syringe: 3 ml and 25 gauge ¾ inch needle.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Mark the level of first carpometacarpal joint on dorsum of hand with your thumbnail at interval between base of thumb metacarpal and trapezium.
Clean skin over carpometacarpal joint; pull on end of thumb.
Advance needle into the joint and inject 0.5 to 1 ml of anesthetic solution. If resistance is felt, redirect the needle into joint and reinsert. Anesthetic solution is pushed. Leave needle in place and change syringe.
Postoperatively patient can wear thumb spica splint for 2–3 days after injection and experience pain relief within 5–7 days after injection.
Alternatively injection can be given under C-arm guidance position of patient, approach and entry point of needle remains same as above (Fig. 4.9).
Indications: Intra-articular injections are effective in osteoarthritis and rheumatoid synovitis (more effective) for those patients who require surgery, those with severe pain and restriction of range of motion and those during rehabilitation periods. Usually done accurately under image intensifier guidance.
Technique
Preparation: Part is painted with antiseptic solution and draped.
Syringe: 3 ml and 25 gauge ¾ inch needle.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Injection is given at the extensor aspect of both metacarpal and proximal interphalangeal joint.
Entry site for metacarpophalangeal joint is small sulcus just below the prominent metacarpal that is most obvious with finger flexed to 20 degrees.
Identify joint by flexing and extending it. Similarly, proximal interphalangeal joint is also identified. Dorsal rim of middle phalanx is easily identified with this joint in extension. A 25 gauge needle is inserted at joint level on dorsolateral side of joint. 0.5 ml of local anesthetic is injected and syringe is changed. With a new syringe, inject 0.5 to 1 ml of 40 mg/ml corticosteroid preparation with slight pressure against plunger.
Alternatively injection can be given under C-arm guidance position of patient, approach and entry point of needle remains same as above (Figs 4.11 and 4.12).99
Most commonly seen in rheumatoid arthritis and repetitive trauma caused by a nodule or thickening of flexor tendon which catches on proximal edge of first annular pulley when finger is actively flexed.
It is characterized by inflammatory changes in retinacular sheath and peritendinous tissue rather than tenosynovium itself common in adults. When severe, finger may lock in flexion requiring patient to use other hand to release finger. Flexor tendon as a consequence, develops a constriction under retinaculum and bulge distal to it. Flexor muscles may force the bulge through retinaculum but extensors are unable to do it.
Patient will have pain over finger with painful snapping at night with locking of fingers. In these patients, local steroid is injected in flexor tendon sheath at level of A1 pulley. Similarly, trigger thumb also has manifestation, but is more severe due to tighter flexor sheath. They are common in females.
Fig. 4.15: Ultrasonographic appearance of flexor tendon and metacarpophalangeal joint. The arrows show left side in long flexor and the right side in A 1 pulley
Trigger fingers usually seen in tennis player they have inability to extend the flexed digit usually seen in those more than 50 years when associated with collagen diseases. Note in palm nodule is present at entry of tendons into proximal at level of metacarpophalangeal joint. Sometimes transverse fibers of palmar aponeurosis may cause persistent triggering.101
Fig. 4.19: Ultrasonographic appearance of flexor tendon and metacarpophalangeal joint PP—proximal phalanx
Local tenderness may be present and accentuation on pressure.
After 1st dose, steroids are effective in 60%.
Recurrence was seen digit in 2 patients and transient in 2 of 84 operated patients.
The results of injection steroid are better than placebo initially at 1 month.
None of patients need to be treated surgically.
Fig. 4.20: Ultrasonographic appearance of flexor tendon and metacarpophalangeal joint. The arrow shows flexor tendon
Splinting, NSAIDs are useful in nonargument of condition. Injection of intermediate acting cortisone or long acting is utilized as first line of treatment. Complete resolution of symptoms has been reported in 60% to 90% patients treated with this fashion.
Young age, insulin dependent DM, involvement of multiple digits and history of other tendinopathies of upper extremities were associated with higher rate of treatment failure.
Kocin Sorensen reported resolution of symptoms in 67% of 106 digits so treated and subsequent studies demonstrated successful outcomes in 50% to 90% patients. They were symptom free one year later.
Indications: Injections for trigger finger are shown to be effective for both short and long-term also this can be accompanied with percutaneous release with help of same needle. USG guided injections are helpful. Steroids given in tendon sheath or peritendinous. Not to give steroids for trigger finger associated with rheumatoid arthritis as cause is diffuse tenosynovitis which needs to be tackled. It is useful for those who are unwilling to undergo surgical procedure.
Technique
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 3 ml and 25 gauge ¾ inch needle.
Identify lump on tendon and infiltrate skin at distal palmar crease which directly overlies tendon (Fig. 4.13). It is useful to flex metacarpophalangeal joint for 10°–15° for this.
Inject 0.5 ml of anesthetic solution into subcutaneous tissue. Advance the needle into tendon sheath and inject rest of anesthetic drug.
Continue to insert needle as patient moves affected finger through slight flexion and extension. When needle touches moving tendon, patient will experience scratchy sensation. If needle moves it has penetrated tendon; it should be partially withdrawn until scratchy sensation occurs.103
Finger USG seen over superficial and deep flexor tendons along phalanges.
There may be falsely hyperechoic segments that lie oblique to beam.
In tendonitis there is small amount of fluid in tendon sheath. In transverse section, tenosynovitis is seen as thickened hyperechoic synovial sheath surrounding tendon.
A1 is located at MCP joint, A3 at PIP joint and A5 at DIP.
Transducer is kept along direction of long flexors. Proximal end at respective metacarpal and distal end at proximal phalanx.
Annular and cruciform pulleys extend from the metacarpal heads to base of distal phalanges at specific points along flexor tendon sheath. Annular pulleys appeared thicker than cruciform so easier to visualize. A1, A2 pulleys are clearly seen as hyperechoic structures. A1 is visualized on transverse USG scan at MCP joint as thin ring shaped structure inserting into volar plate.
On long USG scan, A1 is seen as linear thickening of flexor tendon sheath except for distal part of pulley latter appeared thicker with thin hypoechoic line separating hyperechoic layer of pulley and flexor tendon sheath. Annular pulleys are formed by thick arciform fibers.
During flexion of finger criss cross bands loosen as well as volar plates of finger, bowstringing of flexors is seen so free finger flexion is possible.
Trigger is either blockage or triggering of finger from flexion to extension and most cases involve MCP joints.
Corticosteroid is injected in palpable nodule or A1 pulley.
Position of patient, entry point of needle and approach remains same as above transducer is kept transversely distal to distal palmar crease.
A1 pulley appears as hypoechoic band over flexor tendon sheath in axial plane lateral expansions are oblique. It shows anisotropy on transverse scan.
A1 pulley is visualized at level of metacarpophalangeal joint as thin ring shaped structure inserting in volar plate. It appears as linear thickening of flexor tendon above volar plate and metacarpal head cartilage on longitudinal scan.
DE QUERVAIN TENOSYNOVITIS (FIGS 4.21 TO 4.30 AND 4.41C) ALSO KNOWN AS STENOSING SYNOVITIS OF FIRST DORSAL COMPARTMENT
Tendons of abductor pollicis longus and extensor pollicis brevis are palpated at styloid process of radius pass through thick tendon sheath. This becomes stenosed and inflamed and this produces the symptoms. It is seen usually in association with collagen vascular disease, recurrent mild trauma, infection, etc.
Most commonly it presents with pain over radial styloid process radiating distally along the thumb movement and increases when tendon is angulated at wrist by dorsiflexion, volar flexion or abduction at hand and wrist (Figs 4.21 and 4.22). Seen more commonly between 30 to 40 years of age. Also seen more in those with rheumatoid arthritis. Failure of conservative treatment is because of presence of anomalous tendons or multiple subcompartments within first wrist compartment.
Pinch and grasp are often weakened. There is tenderness and swelling over radial styloid. Diagnostic test is Finkelstein test (Figs 4.23 and 4.24) in which 104patient is asked to make a fist with fingers over thumb and then bent towards the ulnar side.
Fig. 4.29: Ultrasonographic appearance in De quervain's tenosynovitis. The arrow shows the abductor pollicis
Patient feels pain over radial styloid process.
Anderson BL, Moothey R and Brouns MC: 85 patients treated were followed up for 4 years in which 58% were given single injection and 33% multiple. About 17 recurrences after 11–9 months of injection and 3 had minor flares. Rest responded. 10% were subsequently operated. No tendon ruptures, local infection occur so they should be preferred 1st line of treatment. Others responded and 10% were subsequently operated, no tendons ruptures/local infection occurred so they should be preferred 1st line of treatment. Vanderwint DA, Winters JC, Peters Venuthengal found that steroid injection is superior to splinting. But trial was small and number of patient included was few methodological qualities were poor and only pregnant and lactating mothers were included in study.
Study results of the local steroids and immobilization in splint showed 62% satisfactory outcome in mean of 18 months and minimum follow-up of 12 month. Total number of patients were 95 and most were injected with 1% of lignocaine solutions and methylprednisolone. 10 patients lost follow-up and 54 patients had satisfactory response. 33 patients had unsatisfactory outcome and 30 were treated operatively.
After release of 1st dorsal compartment 22 had separate compartments for extensor pollicis brevis and its prevalence is higher for general population shown by J Witt and Gelberman in their study.
De quervain tensynovitis was studied and results showed that injection steroid and mobilization with splint showed 62% satisfactory outcome for more than 18 months with minimum follow-up of 12 months.
Females are most susceptible, it is most common in 30–50 years age, more common due to exercise or rheumatoid arthritis DD : Arthritis of trapeziometacarpal, scaphotrapezial joint, radiocarpal joint superficial radial nerve entrapment tenosynovitis at crossing of extensor pollicis brevis and AB Pl extensor carpi radialis longus and brevis can cause similar symptoms.108
Injection is most useful in first 6 weeks of onset.
There may be separate compartments or duplicated aberrant tendons. These insert more proximally and radially EPB is absent in 5% patients.
According to Harvey et al, 11 of 63 patients require surgery and 10 of these were found to have extensor pollicis brevis in separate compartment and septum may divide a compartment in 73% patients.
Number of patients were 95, number of wrist were 99 and they were injected within 1% xylocaine solution and 4 mg of methylprednisolone 33 patients had satisfactory outcome and 30 were treated operatively by release of 1st dorsal compartment 22 patients had separate compartment for extensor pollicis brevis. And its prevalence is higher than general population.
Proximally intersection syndrome involving ECR tendon where they are crossed by 1 extensor compartment USG Guided injection for De quervian's tenosynovitis. Position of patient approach and entry point remains same and above transducer is kept longitudinally over abductor pollicis longus and extensor pollicis brevis tracing from its insertion and transversely at radial styloid process. Indications: Injections for De quervian's tenosynovitis are shown to be effective for both short and long-term but multiple doses can be needed with splinting and exercises. USG guided injections are helpful. Platelet rich plasma may be useful in intratendinous and steroids given in tendon sheath or peritendinous.
Technique
Patient supine forearm supported. Assistant holds thumb in full flexion, wrist in full flexion either deviated in slight extension or stretched. Preparation: Parts are painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone
Syringe: 2 ml/1½ inch with 25 gauge needle.
Parts are prepared, painted and draped.
Mark the site of two tendons, extensor pollicis brevis and abductor pollicis longus. A 25 gauge needle at 45° angle to skin in line of 2 tendons. If paresthesia is felt into thumb needle has pierced sensory branch of radial nerve.
Move needle 2–3 mm dorsal/volar
Create skin wheal and 0.5 ml of 1% lignocaine and advance needle until it strikes one of underlying tendons.
Inject remaining anesthetic while slowly withdrawing needle until anesthesia flows freely (Fig. 4.26).
Leave needle in place and change syringes. Ask patient to more thumb.
Inject 2 ml of corticosteroid preparation into tendons sheath. Palpation of tendon sheath proximal to point of injection. Should reveal swelling as corticosteroid is injected alternatively operator pinches tendon between thumb and index finger and passes the needle along almost parallel to tendon and sheath no resistance being encountered sausage shape can be felt along the course of tendon extending to groove of radius, so full syringe is injected (Figs 4.27 to 4.40).109
Develops due to fibrous encapsulation of leaked synovial fluid through tendon sheath or capsule of joint.
Most commonly seen in those with repetitive stress and injury. It is also seen more in females. Most of cases are of dorsal wrist (where in mostly there is abnormality with scapholunate ligament). Next common sites are volar ganglion at flexor tendon, sheath of A1 pulley. Seen mostly in second to fourth decade, women > men mucin filled cyst attached to joint capsule/tendon sheath lined by collagen pain and palpable.
Trauma is seen in 10 % people.
According to Angelides et al, stretching of ligaments causes secretion of mucin. USG— hyperechogenicity, septations, lobulations and ill-defined walls.
Ganglion is evaluated for size location, neck, echogenicity, echotexture, posterior acuostic enhancement, internal reflections, septations lobules, calcifications and marginal wall thickness. Presence of infection and hemorrhage is seen.
Anechoic unilocular well-defined margins thin wall variable acoustic enhancement.
Simple ganglia—Entirely of soft tissue with identification margins no identifiable walls. May or may not show color Doppler flow due to solid appearance and most 111complex cystic show septate locules internal reflections, thick walls, ill-defined margins color Doppler flow, acoustic enhancement, partial solid component, static and dynamic scan is done to show its relationship to underlying structures is done.
When there is tenosynovitis of flexor carpi radialis, it can mimic as ganglion. USG shows tendon irregularities and thick synovium with fluid accumulation. It is essential to differentiate it from synovial proliferation, benign neoplasm and collapsed ganglion, volar and dorsal wrist ganglia tend to be of more size and flexor tendon of less size thick wall cyst suggest chronic inflammatory process/ collapsed ganglia due to formation of new subcyst. There is repeated cycle of rupture and expansion. Internal reflection is due to presence of mucin and change with age of ganglion.
Low level echo in small simple cyst due to thickness artifact near field reverberations. Internal echoes may have represented artifact and most small ganglia is simple and not complex. Collapsed ganglion can be misdiagnosed as giant cell tumor on MRI DD nodular fasciitis, benign neoplasm, proliferative synovitis, small complex cystic ganglion, would show increased blood flow.
Nonpalpable ganglia had smaller mean volume than palpable but were always of simple in appearance. Small complexes are common which were deep causing pain and tenderness, predynamic scapholunate instability avoid recurrence, it is important to identify the neck. Dorsal wrist ganglia are attached to scapholunate ligament may originate from scaphoradial/scaphotrapezial joint capsule.
Ganglion cyst is seen volar to tendon is well defined nonechogenic structure, usually oval/circular.
Indication: Usually excision of ganglion is preferred, but it is useful to rule out other causes of swelling with use of ultrasound and also rule out tuberculosis (compound palmar ganglion) before injection, patients not willing for excision are usually given injection with simultaneous aspiration of cyst.
Technique
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle. 22 gauge needle can be also used.
Ganglia is very superficial, it is usually clearly visible, so direct entry is made in to ganglion as it lies in subcutaneous tissue. First aspirate and look for the thick mucoid material, then consider injecting steroid. USG guided injection is useful for ganglion cyst.
Transducer is kept transversely direct over the swelling and its extent is visualized also nearby. Neurovascular structures are visualized; position of patient, entry point of needle and approach remains same as above (Fig. 4.33).
Exact level of compression determines whether symptoms are motor or sensory. Compression distal to tunnel affects the deep branch of ulnar nerve, which suppress intrinsic triangular fibro-osseous canal of about 1.5 cm long.112
Fig. 4.37: Guyons canal on ultrasonographyAbbreviations: UA = Ulnar artery, TS = Tendon sheath, FCU = Flexor carpi ulnaris
It is useful to differentiate it from herniation of cervical disc, thoracic outlet syndrome.
Raynaud syndrome is produced in 3 digits because of sympathetic nerve fibers to these digits pass along ulnar artery.
Cause: Due to sub-clinical collagen vascular disease. Recurrent mild trauma.
Stenosis occurs where the direction of tendon change and friction occurs. It is important to rule out infection that will get floured.
Indications: Patients with intermittent symptoms with no sensory deficits or hypothenar weakness with duration of complaints less than 1 year. Injection with splinting is helpful. Steroid will reduce inflammation to tendons and thereby decrease pressure on ulnar nerve. USG guided injections are effective. Usually steroids are preferred. It will not be useful for solid/cystic swellings like ganglion. Useful in those not fit for surgery.
Technique
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
First, locate the flexor carpi ulnaris (FCU) and palmaris longus (PL) tendons. The palmaris longus tendon is lateral to the flexor carpi ulnaris and is best located by opposing the thumb and fifth digit while the wrist is flexed. Although ulnar to the palmaris longus and proximal to the proximal wrist crease avoid going directly into nerve, and if paresthesias are elicited, needle should be withdrawn and placed in more ulnarly or radially.
Insert needle 1 cm proximal to wrist flexion crease and 3–5 mm from ulnar side of palmaris longus. If palmars longus is absent, direction of needle may be aligned with ring finger (Fig. 4.34).
If contact is made with the palmaris longus tendon while advancing the needle, retract slightly and redirect.
The use of a needle smaller in diameter may require increased effort and slower injection time but dramatically reduces pain at the site of injection. Alternatively pisiform is to be traced.
Ultrasonography guided injection is given in the same manner with probe longitudinal and pisiform is taken as point where one end of probe is kept and other end visualizes the FCU tendon (Figs 4.35 to 4.37).
Position of patient, approach and entry point of needle remains same as above.
Accessory abductor digiti minimi is most common accessory muscle of wrist. It is found in 24% of normal individuals, it lies in guyons canal in close contact with ulnar artery and nerve during contraction. It appears hypoechoic with internal muscle echotexture oval shape of ulnar nerve adjacent to it suggest nerve compression and on dynamic examination during abduction of little finger increase muscle thickness and impingement of ulnar nerve color and Doppler sonography allows accurate evaluation of ulnar artery.
Extensor digitorum brevis manus is seen in 1% to 3% healthy subjects it arises from dorsal aspect of distal radius and inserts into index or middle finger.
It appears as fusiform lump along extensor tendon of index finger that can mimic ganglion, extensor tenosynovitis or soft tissue tumor dynamic USG gives appearance of changes during movements (Figs 4.38 to 4.41).115
Fig. 4.39: Site of pain in various hand disordersAbbreviations: OA = Osteoarthritis, PsA = Psoriatic arthritis, RA = Rheumatoid arthritis
Figs 4.41A to C: Schematic representation of (A) USG picture of abductor pollicis longus; (B) USG picture of guyons canal; (C) Anatomical snuff boxAbbreviations: UA = Ulnar artery, UN = Ulnar nerve, FCU = Flexor carpi ulnaris
FUTHER READING
- Abe Y, Watson HK, Renaud S. Flexor tendon sheath ganglion: analysis of 128 cases. Hand Surg. 2004;9:1-4.
- Anderson BGJ, Manthey R, Brouns MC. Treatment of De Quervain's tenosynovitis with corticosteroids. A prospective study of the response to local injection. Arthritis Rheum. 1991;34:793-8.
- Arons MS. De Quervain's release in working women: A report of failures, complications, and associated diagnoses. J Hand Sure. 1987;12A:540-4.
- Beekman R, Visser LH. Sonography in the diagnosis of carpal tunnel syndrome: a critical review of the literature. Muscle Nerve. 2003;27:26-33.
- Benson LS, Ptaszek AJ. Injection versus surgery in the treatment of trigger finger. JHand Surg [Am]. 1997;22:138-44.
- Bianchi S, Martinoli C, Abdelwahab IF. High-frequency ultrasound examination of the wrist and hand. Skeletal Radiol. 1999;28:121-9.
- Bloem SL, Sartoris DJ. MRI and CT of Musculoskeletal System. Williams &Wilkins, Baltimore Churchill Livingstone, London, 1992.pp.795-832.
- Boutry N, Titecat M, Demondion X, Glaude E, Fontaine C, Cotten A. High- frequency ultrasonographic examination of the finger pulley system. J Ultrasound Med. 2005;24:1333-9.
- Bozkurt MC, Tagil SM, Ozcakar L, et al. Anatomical variations as potential risk factors for ulnar tunnel syndrome: a cadaver study. Clin Anat. 2005;18:274.
- Braun RM, Davidson K, Doehr S. Provocative testing in the diagnosis of dynamic carpal tunnel syndrome. J Hand Surg [Am]. 1989;14:195-7.
- Buchberger W. Radiologic imaging of the carpal tunnel. Eur J Radiol. 1997;25:112-7.
- Buchberger W, Judmaier W, Birbarher G, Lener M, Schmidauer C. Carpal tunnel syndrome: diagnosis with high resolution sonography. AJR Am J Roentgenol. 1992;159:793-8.
- Buchberger W, Schon G, Strasser K, Jungwirth W. High-resolution ultrasonography of the carpal tunnel. J Ultrasound Med. 1991;10:531-7.
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics, Vol 4. 11th ed. Mosby Inc. 2008;3761-79.
- Chen P, Maklad N, Redwine M, Zelitt D. Dynamic high-resoiution sonography of the carpal tunnel. AJR Am J Roentgenol. 1997;168:533-7.
- Christie, BGB. Local hydrocortisone in de Quervain's disease. British Med JI. 1955;1501-3.
- De Quervain, F. Uber eine Form von chronischer tendovaginitis. Corresp Blatt Schweizer Arzte, 1895;25:389-94.
- Dumitru D. Zwarts MJ. Focal peripheral neuropathies. In: Dumitru D, Amato AA, Zwarts MJ (Eds). Electrodiagnostic Medicine. Philadelphia, PA: Hanley and Belfus. 2001;1043-125.
- Duncan I, Sullivan P, Lomas F. Sonography in the diagnosis of carpal tunnel syndrome. AJR Am J Roentgenol. 1999;173:681-4.
- Enger WD, Gmeiner JG. Palmar cutaneous branch of the ulnar nerve. J Hand Surg. 1980;5A:26.
- Fahrer M, Millroy PJ. Ulnar compression neuropathy due to an anomalous abductor digiti minimi: clinical and anatomic study. J Hand Surg. 1981;6A:266.
- Finkelstein Harry. Stenosing tendovaginitis at the radial styloid process. J Bone and Joint Surg. July 1930;12:509-40.
- Fornage BD, Rifkin MD. Ultrasound examination of tendons. Radiol Clin North Am. 1989;26:27-107.
- Freiberg A, Mulholland RS, Levine R. Nonoperative treatment of trigger fingers and thumbs. J Hand Surg [Am]. 1989;14:553-8.
- Giles, KW. Anatomical variations affecting the surgery of de quervain's disease. J Bone and Joint Surg. 1960;42-B(2):352-5.
- Glowacki KA, Breen CJ, Sachar K, Weiss A-PC. Electrodiagnostic testing and carpal tunnel release outcome. J Hand Surg [Am]. 1996;21:117-22.
- Gonzalez del Pino J, Delgado Martinez AD, Gonzalez I, Lovic A. Value of the carpal compression test in the diagnosis of carpal tunnel syndrome. J Hand Surg [Br]. 1997;22:38-41.
- Green DP. True and false traumatic aneurysms in the hand: report of two cases and review of the literature. J Bone Joint Surg. 1973;55A:120.
- Grundberg AB. Carpal tunnel decompression in spite of normal electromyography. J Hand Surg [Am]. 1983;8:348-9.
- Gunnarsson LG, Amilon A, Hellstrand P, Leissner P, Philipson L The diagnosis of carpal tunnel syndrome: sensitivity and specificity of some clinical and electro- physiological tests. J Hand Surg [Br]. 1997;22:34-7.
- Hagberg M, Morgenstern H, Kelsh M. Impact of occupations and job tasks on the prevalence of carpal tunnel syndrome. Scand J Work Environ Health. 1992;18:337-45.
- Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29-36.
- Harvey FJ, Harvey PM, Horsley MW. De Quervain's disease: surgical or nonsurgical treatment. J Hand Surg. 1990;15A:83-7.
- Hauger O, Chung CB, Lektrakul N, et al. Pulley system in the fingers: normal anatorny and simulated. J Ultrasound Med. 2004;23:1301-6.
- Henriguerini et al. USG appearance of trigger finger. Journal of Ultrasound Medicine. 2008;27:1407-13.
- Hoffmann Phil. Stenosing tendovaginitis at the radial styloid process. J Bone and Joint Surg. Jan 1931;13:89-90.
- Jackson WT, Viegas SF, Coon TM, Stimpson KD, Frogameni AD, Simpson JM. Anatomical variations in first extensor compartment of the wrist. A clinical and anatomical study. J Bone and Joint Surg. July 1986;68-A:923-6.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. Edition 1. 2007;25-112.
- John O Neill. Musculoskeletal Ultrasound Anatomy and Technique. Springer Inc. 2008;20-330.
- Johnson EW. Diagnosis of carpal tunnel syndrome: the gold standard. Am J Phys Med Rehabil. 1993;72:1.
- Keberle M, Jenett M, Kenn W, et al. Technical advances in ultrasound and MR imaging of carpal tunnel syndrome. Eur Radiol. 2000;10:1043-50.
- Keon-Cohen, Bryan. De Quervain's disease. J Bone and Joint Surg. 1951;33-B(l): 96-9.
- Lacey Thomas II, Goldstein LA, Tobin CE. Anatomical and clinical study of the variations in the insertions of the abductor pollicis longus tendon, associated with stenosing tendovaginitis. J Bone and Joint Surg. April 1951;33-A:347-50.
- Lamphier TA, Long NG, Dennehy Timothy. DeQuervain's disease. an analysis of 52 cases. Ann Surg. 1953;138:832-41.
- Lapidus PW, Guidotti FP. Stenosing tenovaginitis of the wrist and fingers. Clin Orthop. 1972;83:87-90.
- Leao Luiz. De Quervain's disease. A clinical and anatomical study. J Bone and Joint Surg. Oct 1958;40-A:1063-70.
- Lee SJ, Pho RW. Report of an unusual case of trigger finger secondary to phalangeal exostosis. Hand Surg. 2005;10:135-8.
- McCarthy RE, Nalebuff EA. Anomalous volar branch of the dorsal cutaneous ulnar nerve: a case report. J Hand Surg. 1980;5A:19.
- McKenzie JM. Conservative treatment of de Quervain's disease. Br Med J. 1972,4:659-60.
- Mnrnhy D, Failla JM, Koniuch MP. Steroid versus placebo injection for trigger finger. J Hand Surg [Am]. 1995;20:628-31.
- Murata K, Shih JT, Tsai TM. Causes of ulnar tunnel syndrome: a retrospective study of 31 subjects. J Hand Surg. 2004;29A:160.
- Nakamichi K, Tachibana S. Ganglion-associated ulnar tunnel syndrome treated by ultrasonographically assisted aspiration and splinting. J Hand Surg. 2003;28B:177.
- Nakamichi K, Tachibana S. Ultrasonographic measurement of median nerve crosssectional area in idiopathic carpal tunnel syndrome: diagnostic accuracy. Muscle Nerve. 2002;26:798-803.
- Nathan PA, Keniston RC, Meadows KD, Lockwood RS. Predictive value of nerve conduction measurements at the carpal tunnel. Muscle Nerve. 1993;16:1377-82.
- Pascarelli EF, Hsu YP. Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil. 2001;11:l–21.
- Read RL. Stress testing in nerve compression. Hand Clin. 1991;7:521-6.
- Rhoades CE, Gelberman RH, Manjarris JF. Stenosing tenosynovitis of the fingers and thumb: Faults of a prospective trial of steroid injection and splinting. Clin Orthop Relat Res. 1984;190:236-8.
- Rumack C, Wilson S, William J. Diagnostic Ultrasound. Vol 1. 2nd edition. Mosby Inc. 1998:843-83
- Sarria L, Cabada T, Cozcolluela R, Martinez-Berganza T, Garcia S. Carpal tunnel syndrome: usefulness of sonography. Eur Radiol. 2000;10:1920-5.
- Solbiati L, Rizzatto G. Ultrasound of Superficial Structures. 1st edition. Churchill Livingstone. 1995;279-375.
- Steinbach G. The carpal tunnel syndrome. J Emerg Med. 1999;17:519-23.
- Suematsu N, Hirayama T, Takemitsu Y. Trigger wrist caused by a giant cell tumoiir of tendon sheath. J Hand Surg [Br]. 1985;10:121-3.
- Tamara D. Trigger finger: prognostic indicators of recurrence following corticosteriod injection. J Bone Joint Surg (Am). 2008; 90(8): 1665-72.
- Taras JS, Raphael JS, Pan WT, Movagharnia F, Sotereanos DG. Corticosteroidinjections for trigger digits: is intrasheath injection’ necessary? J Hand Surg [Am]. 1998;23:717-22.
- Tohyama M, Tsujio X Yanagida I, Trigger finger csjsed by an old partial flexor tendon laceration: a case report. Hand Surg. 2005;10:105-8.
- Watson Buchaman W. Clinical Examination of Musculoskeletal System. Williams & Wilkins. 1st edition. 1997;25-82.
- Weiss AP, Akelman E, Tabatabai M. Treatment of de Quervain's disease. J Hand Surg [Am]. 1994;19:595-8.
- Wilson DJ, Fornage BD, Bossi MC, Nessi R. Musculoskeletal system and skin. In: Cosgrove D, Meire M, Dewbury K (Eds). Abdominal and General Ultrasound. 1993;227-8.
- Witt J, Pess G, Gelberman RH. Treatment of de Quervain tenosynovitis. J Bone Joint Surg (Am). 1991;73:219-22.
- Yuichi Y, Villarraga HR, Henderson J, Zhao C, An KN, Amadio PC. Ultrasound assessment of the displacement and deformation of the median nerve in the human carpal tunnel with active finger motion. J Bone Joint Surg (Am). 2009; 91(12):2922-30.
- Zingas C, Failla JM, Van Holsbeeck M. Injection accuracy and clinical relief of de Quervain's tendinitis. J Hand Surg [Am]. 1998;23:89-96.
Note: It is important to rule out tuberculosis before providing any injection for a joint.
Indications: Costosternal joint injection is considered in cases of suspected inflammation. Steroids are preferred. It is usually provided in stage when oral anti-inflammatory drugs are not effective.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml/1½ inch 25 gauge needle.
Identify costosternal joints by palpation, costosternal area is seen easily as slight bulge at the point where rib attaches the sternum. This is area of tenderness.
Needle is inserted in slightly medial and on cephalad direction. If needle hits bone then withdraw the needle and redirect it medially. Inject the contents of syringe gently (Fig. 5.2).
TIETZE'S SYNDROME
It was described as acute painful swelling of costal cartilage. 2nd and 3rd costal cartilage are more commonly involved. Occurs in 2nd and 3rd decades onset is usually acute.123
Indications: Costosternal joint injection is considered in cases of suspected inflammation. Steroid are preferred. It is usually provided in stage when oral anti- inflammatory drugs are not effective.124
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml/1½ inch 25 gauge needle.
Identify 2nd and 3rd costosternal joints by carefully palpating the costosternal area. It is seen as slight bulge at point where the rib attaches the sternum. Needle is inserted close to joint in slightly medial and cephalad direction.
If you hit the bone, withdraw needle and redirect it more medially.
MANUBRIOSTERNAL JOINT PAIN SYNDROME
It is essential to rule out pain of cardiac origin.
Indications: Manubriosternal joint injection is considered in cases of suspected inflammation of same. Steroid are preferred. It is usually provided in stage when oral anti-inflammatory drugs are not effective.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml/1½ inch 25 gauge needle.
Technique: Identify the angle of sternum. Manubriosternal joint should be easily palpable at this point.
Insert the needle close to joint in a slightly medial and cephalad direction.
If hit a bone withdraw needle and redirect it more medially.
STERNALIS SYNDROME
Sternalis lies anterior to sternal end of pectoralis major and runs parallel to sternum. Pain is similar to cardiac pain if myofascial pain syndrome and trigger points could be found in the sternal area.
It is found in midline over sternum. Pain is not increased by movement of shoulder and chest wall.
There could be coexisting trigger point in pectoralis major muscle and sternal head of sternocleidomastoid.
Differential diagnosis is costosternal syndrome.
Indications: Injection is considered in cases of suspected inflammation of same steroid are preferred. It is usually provided in stage when oral anti-inflammatory drugs are not effective.125
Technique
Position: Supine.
Preparation: Chest is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml/1½ inch 25 gauge needle.
Identify midline of sterum and palpate sternalis muscle, mark trigger point on muscle. Pressing of which positive jump sign could be elicited.
Inject the contents of syringe gently after firmly fixing the needle.
Indications: Sternoclavicular joint injection is considered in cases of suspected inflammation. Steroids are preferred. It is usually provided in stage when oral anti-inflammatory drugs are not effective.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml/1½ inch 25 gauge needle.
Identify sternoclavicular joints by palpation, sternoclavicular area is seen easily as slight bulge at the point where rib attaches the sternum. This is area of tenderness.
Needle is inserted in slightly medial and on cephalad direction. If needle hits bone then withdraw the needle and redirect it medially. Inject the contents of syringe gently.
Figs 5.4A and B: (A) Sternoclavicular joint on USG; (B) USG appearance of sternoclavicular joint synovitis
XIPHODYNIA SYNDROME (FIG. 5.5)
It mimics the pain of cardiac and upper abdominal origin. Patient complaints of severe intolerant anterior chest wall pain in xiphoid process which increases on overeating, bending and stooping and coughing.
Tenderness and swelling over xiphisternal joint is present.
Indications: Xiphisternal joint injection is considered in cases of suspected inflammation of same. Steroid are preferred. It is usually provided in stage when oral anti-inflammatory drugs are not effective.127
Technique
Position: Supine.
Preparation: Shoulder is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 1 ml/1½ inch 25 gauge needle.
Palpate xiphisternal joint.
Insert needle close to center of joint in slightly cephalad direction.
It hits the same, withdraw needle and redirect if gone medially.
LUMBAR MYOFASCIAL PAIN SYNDROME
Chronic pain syndrome that affects a focal or regional portion of body. More common in muscle of back. Characteristic feature is presence of trigger points in affected muscle.
Patient usually presents with pain in affected muscles referred to other parts of body.
Pain on trigger point increases on pressing the point firmly and it increases on stretching, usually associated with depression and other psychological problems.
Indications: Injection is considered in cases of suspected inflammation of same. Steroid are preferred. It is usually provided in stage when oral anti-inflammatory drugs are not effective.
Technique
Position: Supine.
Drugs: 0.25% preservative free bupivacaine and 40 mg of methylprednisolone.
Syringe: 1 ml/1½ inch 25 gauge needle.
Prone position helps to prevent vasovagal attack.
Identity the trigger point by careful palpation trigger point injections are directed at primary trigger point and not in area of referred pain.
Insert needle brought to the center of trigger point by inject about 0.5 ml to 1 ml of solution into each trigger point.
FURTHER READING
- Adler RS. Future and new developments in musculoskeletal ultrasound. Radiol Clin North Am. 1999;27:623–31.
- Gottlieb NL, Riskin WG. Complications of local corticosteroid injections. JAMA. 1980;243:1457–548.
- Hamilton JH, Bootes A, Phillips PE, Llywoka J. Human synovial fibroblast plasminogen activator. Modulation of enzyme activity by anti-inflammatory steroids. Rheum Arthritis. 1981;24:1296–303.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. 1st Edition. 2007;113–48.
- John O Neill. Musculoskeletal Ultrasound Anatomy and Technique. Springer Inc. 2008;20–330.
- Rifat SF, Moeller JL. Site-specific techniques of joint injection. Useful additions to your treatment repertoire. Postgrad Med. Mar 2001;109(3):123-6, 129-30, 135-6.
- Rumack C, Wilson S, William J. Diagnostic Ultrasound. Vol 1. 2nd Edition. Mosby Inc. 1998;843–83.
- Solbiati L, Rizzatto G. Ultrasound of Superficial Structures. 1st edition. Churchill Livingstone. 1995;279–375.
- Watson Buchaman W. Clinical Examination of Musculoskeletal System. Williams & Wilkins. 1st Edition. 1997;25–82.
Spinous processes of L4-L5 correspond to iliac crest level are excellent reference points.
S2 spinous process lies at level of posterosuperior iliac spine.
Posterior aspect of coccyx can be felt directly.
In thin individuals, sacral promontory (L5-S1 articulation) can be felt below umbilicus anteriorly, and at umbilicus the level is L3-L4.
Spinal cord in adults extends down to level of lower border of spine of L1; in young children, it may extend to L3.
Subarachnoid space with its cerebrospinal fluid (CSF) extends down to lower border of S1 which lies at the level of posterosuperior iliac spine.131
- Pain sources may be diskogenic, facetal, spondylogenic, referred, radicular, myofascial, vascular and retroperitoneal.
- Facet joints are innervated by medial branch of dorsal primary rami.
- Structures within neural canal are—sinovertebral nerve, disk, a branch of rami communicates and ventral primary ramus.
Pain is mediated by TNF-alpha, IL-1, substance P and vasoactive intestinal peptide (VIP). Laslett et al and Manchikanti et al (2001) have described discography as a way of diagnosing.
ALBERT SCHWEITZER
“We must all die but that, I can save him from days of torture that's what, I feel is my goal and ever new privilege. Pain is more terrible long of mankind than even death itself.”
Harshall et al—prevalence of chronic pain is 10% to 55% and in elderly it is 23.7% to 50.2%.
“Patients suffering from chronic pain often have damage to a nerve and that nerve is in a constant state of aggravation sending pain messages up and down its entire length,” said Kim J Burchiel, MD.
In some cases, painful nerve damage cannot be repaired.
Low back pain and sciatica:
- Has nociceptive inflammatory pain mechanism
- There is activation and sensitization of nerve root (nervi nervorum) from root compression or traction
- There is sensitization of nociceptors of annulus fibrosus, periosteal spinal structures and ligaments due to acute inflammation
- Hyperalgesia (deep spinal and dermatomal) due to central sensitization
- Radicular and diskogenic, neuropathic pain:
- Mechanism
- Ectopic activity of nerve root nervi nervorum; sensitization and ectopic activity of nociceptive innervating spinal periosteal structures.
- There is possible role of abnormal nociceptors overgrown within intradiskal space, postsurgical epidural scars and degenerated facet joints
- There is CNS sensitization and reorganization.
Bulging disk:
- 3/4 MRI bulging disks are normal.
- In 1/2 with persistent sciatica, MRI is show only a bulge.
- 10% show nerve root compression.
- 50% painful disk missed by CT.
- 2/3 asymptomatic have spine MRI abnormalities.
Low back pain similar to preoperative symptoms, noted in 70% patients after stimulation of posterior annulus or posterior longitudinal ligament, local anesthetic injection obliterated pain.
Facet joint pain have no objective findings except tenderness. It could have back pain not aggravated by movements.
Hypertrophied facet joints are less likely to hurt (Kalichman L et al).
There is no significant relation in imaging findings and facet pain (Cohen S et al 2007).
Disk herniation causes:
- Spinal nerve root compression
- Spinal nerve root inflammation
- Spinal stenosis.
Correlating physical findings with imaging decides level and type of injection.
With sharp pain and spasm at site of herniation, pain shoots down extremity. Patient walks with list.
Spinal stenosis:
- Back and leg pain after walking a limited distance and increasing as distance increases.
- There is leg weakness or numbness with or without sciatica.
- Negative straight leg raising test.
- Pain present on prolonged extension decreasing on flexion.
Facet joint arthropathy:
- Pain over facet joint on spinal extension
- Exacerbation by ipsilateral trunk lateral flexion.
Always keep in mind compression from piriformis:
- Symptoms similar to lumbar disk conditions except for absence of true neurological finding.
- Pain increases with medial rotation of thigh.
Pathology
- High levels of phospholipase A2(PL-A2) enzyme that helps to regulate the initial inflammatory cascade. It causes local demyelination of nerve roots with ectopic diskharges.
- Inflammatory products leukotriene-B4 and thromboxane-B2 have also been recovered in herniated human disk after surgery.
- Spinal stenosis causes nerve root vascular flow inhibition with resulting nerve root edema, nerve root dysfunction and decreased nerve root nutrition.
- Chronic nerve root compression can induce axon ischemia, impede venous return, promote plasma protein extravasation.
- Decreased capillary permeability.
- Decreased neural transmission in nociceptive ‘c’ fibers.
- When nerve roots exit the thecal sac, they are covered by a short expanse of dural membrane, they are enveloped within the epidural fat.
- Nerve roots and associated radicular vessels and lymphatics then course in an oblique fashion in lumbar spine, inferior to the corresponding pedicle and through neural foramina.
- At exit zone of neural foramina lies dorsal root ganglion which has preponderance of pain distal to it. Spinal nerve quickly separates into ventral and dorsal rami.
- All these are enveloped by perineural fat which is contiguous with epineural fat. Catugo in 1764 described sciatica; for the first time it was to differentiate sciatic pain from dull aching pain.
Andre was first to perceive disk as source of pain and Eslberg had described it for the first time.
Mixter and Barr proposed that mechanical pressure exerted by nerve not causes pain.
Genetics may also play role in inflammation is another factor. Especially phospholipase A2, IL-6, IL-8, PG B2.
Corticosteroids most likely are related to decrease in PL-A2 and inflammation.
Most patients are unsatisfied about counseling. 86% of chronic pain sufferers report inability to sleep. 60% have breakthrough pain one or more times daily. 14% are satisfied. 22% patients change physicians.
Facet joint pain:
- Unilateral or bilateral paravertebral pain there is increased pain on trunk rotation, stretching into full extension or on lateral bending.
In herniated disk:
- Radiating leg pain > back pain. Pain increase on sitting and leaning forward, coughing, sneezing and straining. Muscle spasm and loss of lordosis seen.
- Ipsilateral straight leg raising test: positive.
Myogenic/muscle related disease:
- Morning pain and muscle stiffness.
- Pain is unilateral or bilateral not midline.
- Pain extends into buttock and thigh region only. Pain is reduced with resisted prolonged muscle contraction and passive stretching of muscle.
- There is contralateral side pain with side bending.
- Even though macroscopically visible and histologically evident it was not always possible to demonstrate experimental annulus injuries by contrast enhanced MRI—spine 2002.
- Due to insensitivity of clinical tests sacroiliac induced pain requires diagnostic injections.
- Myelography is insensitive in lateral recess lesions.
Cohen PM and Oaja PK had showed that use of historic and physical findings to diagnose lumbar zygapophyseal joint pain is not supportive.137
Nociceptive pain generator model works for patients with mixed nociceptive/hypersensitization complexes. Radicular pain is single and subjective clinical feature that may be part of radiculopathy.
- Diskogenic low back pain which is pain at or above L5, loss of full range of motion and pain while rising from sitting (Yang et al, 2003) more centralized.
- Radicular pain may be due to disk herniation/inflammation or neural compression or vascular compromise.
- Chronic inflammation result in edema, wallerian degeneration and fibrotic changes in neural tissue.
- Radiculopathy is pathological disorder affecting the function of nerve roots.
- Depending on fibers affected there are features as sensory loss, motor loss, reflex loss, paresthesia and pain.
- Radicular pain is 95% due to disk herniation/foraminal stenosis.
- But in condition where somatic pain could occur due to epiduritis and perceived pathology is located ventrally in epidural space is not immediately assessible to conventional lumbar/caudal/epidural injection. Which delivers drugs to epidural space posteriorly/inferiorly.
Herniated nucleus prolapse is incipiently herniated disk at ventral surface of dural sac. If epiduritis is to be treated by epidural steroids, a transforaminal approach is most appropriate.
RISK FACTORS FOR LOW BACK PAIN
- Age peak between 40–60 years, occupational factors, poor physical fitness, low social class, smoking.
For chronicity
- Pain intensity, interference with usual activities, with family and household activities, number of sites of pain.
- Radicular pain is band like shooting, lancinating, electrical pain. Distal > proximal and cutaneous component. It is essential to differentiate it from psoas myofascial pain and sciatic nerve inflammation, extraforaminal spinal nerve entrapment.
- Diagnosis by signs of nerve root tension by reproducing pain radiating to the patient's buttock, thigh or calf pain by straight leg raising, only this type of pain should be treated. Precludes use of steroids for somatic referred pain. With somatic referred pain backache > leg pain deep seated and aching in quality constant and covers wider areas than narrow bands of radicular pain.
- It is unusual for referred pain to extend distal to knee/elbow.
- Signs of nerve root tension are negative. Straight leg raising may be restricted due to backpain and not due to reproduction of buttock or leg pain.
Only radicular pain is compatible with nerve root inflammation and for use of epidural steroids must be distinguished from somatic referred pain.
- Neuropathic pain is usually described as burning, electric, tingling and shooting which cannot be controlled by traditional oral drugs management of neuropathic pain include other medications and multiple treatment modalities.
- Nociceptive pain, is localized pain which is sharp, aching and throbbing, postoperative, pain associated with trauma and arthritic pain which usually responds to NSAIDs and opioids.
Chronic pain is multidimensional problem with multiple etiologies.
Approach to pain management currently includes psychological behavioral, functional and interventional pain therapies.
- Origins of neural blockage and regional anesthesic dates back to 1884 - Koller reported the numbing effect of cocaine on tongue. It was used in ophthalmology, urology and general surgery in 1999.
- Caudal epidural injections were described in 1901(77-79); trigeminal alcohol blockade was reported by Schlossers in 1903.
- While Steindler and Luck in 1938 described applications for diagnostic interventional techniques.
- Steindler and Luck employed procaine hydrochloride injections for identifying sources of pain in low back pain disorders.
- Bogduck was responsible for our current understandings of clinical anatomy of spine.
- Hogan and Abram described several clinical situations including characteristic of chronic spinal pain, which are subjective and uncertain pathophysiology.
- Precision diagnostic blocks are used to define these clinical situations to determine pathophysiology of pain, site of nociception and pathway of afferent neural signals.
- Deyo and Weinstein reported that anatomic diagnosis is pivotal in low back pain and history, physical examination and imaging provide limited information.
- Anatomical diagnosis is possible in only 10% to 15% people.
- Following introduction of gate control theory, important observation made on descending modulation of pain perception. Brown and Mandl 1924—Block was used in management of visceral pain.
- Royle 1924 described blockade of sympathetic nerve supply to musculature of affected limbs in relieving deformity, contraction and spastic paralysis in Little's disease.
- Swetlav described prolong pain relief by neurolytic injection of alcohol to paravertebral sympathetic nerves in treatment of severe pain.
- Doglotti injected absolute alcohol in subarachnoid space to produce chemical posterior rhizotomy.
- Sicard 1901 injected cocaine through sacral hiatus into epidural space for patient with severe sciatic pain.
- Cathelin also described caudal administration of local anesthesia not only for surgical procedures but also for relief of pain due to inoperable carcinoma of rectum.
- Pasquier and Ler in 1901 reported use of caudal epidural injection for relief of sciatic pain.
- In 1912, Kappis showed paravertebral somatic blocks for pain relief and surgery.
- In 1953, John Bonica stimulated interest in pain medicine.
- Vandam and Eckenhoff described multidiskiplinary approach to relief of pain.
- IASP (International Association for Study of Pain) was established in 1974, the American Pain Society and American Chapter of IASP was established in 1977. American Academy of Pain Medicine was founded in 1920.
- Established in 1988 World Society of Pain Clinics and World Institute of Pain also emerged in 1990.
- American Society of Interventional Pain Physicians was founded in 1998.
- Lippe—Physicians specializing in pain medicine may work in variety of setting and are competent to treat the entire range of painful disorders encountered in delivery of health care.
- Pahol et al found that pain relief is particularly elusive for older women with disabling back and lower extremity problems similarly elderly patients also have same problems.
- Bonica defined pain as pain when persist a month beyond the usual course of acute disease or reasonable time for any injury to heal that is associated with chronic pathological process that causes a continuous pain or pain at intervals for months or year.
- Chronic pain syndrome is associated with major psychological and behavioral problems with or without a physical problem.
- Recurrent pain is precursor of it. It is disproportional pain related to behavior. It is frequently seen in elderly.
- Hendler et al found organic basis of pain in about 98% of patients.
Subsequently Hendler and Kolodny estimated that incidence of psychogenic pain seen in 1:3000 patients.
- For a structure to be implicated it should have been shown to be a source of pain in patients, proved using diagnostic technique of known reliability and validity.
- Disk herniation, strained muscles or torn ligament have been attributed to most spinal pain either in upper extremities, upper and midback or low back and lower extremities. Disorders of spinal joints which includes facet joints have implicated in 50% of pain.
- The 2nd most common source is that of intervertebral disk due to disk degeneration.
- Myofascial pain syndromes are not supported by prevalence of epidemological data.
- Nociceptive pain is caused by irritation of spinal nerve endings, it can be dull or sharp. Mild to severe neuropathic pain is caused by malfunction of nervous system. It occurs due to inflammatory agent, arthrosis, capsular tear cartilaginous degeneration.
- Chronic pain is considered as persistent pain which is not ameable to routine pain control methods.
- Halellus studied natural history of sciatica and found that at 4 weeks after a course of bedrest and bracing 93% had major improvements. Many studies showed that patients who underwent disk surgery might have better results than persons who did not have surgery at 1 year to 4 years but at 10 years there is no statistical difference in results, in this regards spine injections can be used.
- Wilberger described that time was required for mechanical deformation to cause this silent nerve compression.
- About 90% of ruptured disk at L4–5 and L5 S1 level and 90% of patients with backpain and sciatica will recover without surgery, at least 50% within 6 weeks.
- Sciatica might be associated with inflammation since steroid is used to relieve pain.
Bogduck postulates:
- Structure should have nerve supply.
- Be capable of causing pain.
- Susceptible for disease that are known to be painful.
- Source of pain in patient using diagnostic technique of known reliability and validity.
- Diagnostic block should have accessibility.
- Subjected to validity—criterion standard.
Rationale for therapeutic interventional techniques include, neural blockade in spine is based on:
- Source of chronic spinal pain namely disks and joints are accessible to neural blockade.
- Removal/correction of structural abnormalities of spine may fail to cure and may even worsen painful conditions.
- Degenerative processes of spine and origin of spinal pain are complex.
If a joint is determined to be source of pain long-term relief can be obtained by directing intervention at that joint.
Relief of pain is accepted criterion. Diagnostic blockade and ability to generate pain can be performed to test hypothesis that target structure, is a source of pain. Radiography confirms diagnosis but may be normal.
Clinical features and imaging/neuro-studies do not permit accurate analysis of causation of spinal pain in majority of patient in absence of disk herniation. Presence of organic origin of pain in 98% cases is mistakenly branded as psychogenic in origin.
Chronic low backache is diagnostic dilemma in 85% patient and disk and facet joint are accessible to neural block used for diagnosis.
Removal/correction of structural abnormality of spine may fail to cure and worsen the origin of spinal pain.
It is mandatory before any type of spinal block to have intravenous assess ECG, nasal O2, noninvasive BP, fluoroscopy. If possible position patient in most procedures: prone with bolsters below trunk.
Mechanism of action of local anesthetic: Interrupt pain spasm cycle and reverberating nociceptor transmission, whereas steroids decrease inflammatory either by the synthesis/release of number of proinflammatory substances.
Mechanism of action of steroids: Membrane stabilization decrease neural peptide synthesis/action.
Blockage of phospholipase A2 decrease sensitization of dorsal horn neuron reversible LA effect
Local anesthesia prolong dampening of “c” fiber activity.
They are divided into:
(1) Diagnostic and (2) Therapeutic technique.
Diagnostic consist of selective nerve root block, facet joint blocks and provocative discography.
Therapeutic consist of facet joint injection, epidural injections and implantable therapies.
EPIDURAL STEROIDS (FIGS 6.13 TO 6.16 AND FLOW CHARTS 6.1 TO 6.4)
Epidural space is space between dural lining of spinal cord and nerve roots and osseoligamentous complex.
- Anteriorly, boundaries are vertebral body. Intervertebral disk and posterior longitudinal ligament.
- Posteriorly boundaries are thecal sac and ligamentum flavun.
- Spinal nerve exists within as intervertebral foramen bordered by vertebral body and disk and by facet joints superiorly and inferiorly pedicles of adjacent vertebrae.
First epidural medication injected was cocaine with caudal approach for lumbago and sciatica, steroid was used for the first time in 1952.
- Definitive numbers are still not available regarding percentages of low back pain caused by disk herniation or facet joints.
- Meta-analysis for interlaminal injection carried out by Abdi et al used 12 randomized trials for transforaminal injections.
Those with radiculopathy respond 3 times better than those without it. It does not work much in patients with backache.
- Nerve root inflammation always manifest as pain in limbs or around trunk wall.
- Studies have showed that epidural injections are excellent therapy for managing pain. About 30% of patients originally reported as candidate for surgery decided against surgery after injection.
Hirsch in 1963 described intra-articular injections for pain relief.
- Ryan and Taylor performed to intrathecal and epidural injection and obtained CSF samples the response of steroid in those patient with sciatica alone was far better than those with compressive symptoms and still better when duration of illness was short.
- About 75% of responders had higher than normal levels of proteins as compared to only 25% of nonresponders. So, are useful in stage of inflammation, hence best indicated in patients with radicular pain.
Important Indication is Radicular Pain
- Lancinating pain that travels down along the affected limb or around trunk wall.
- There is paresthesia in dermatomal distribution and deep seated pain in myotomal distribution. Pain extends distal to knee/elbow. In buttock, pain is deep seated cramp like aggravated on sitting and sometimes as paresthetic diskomfort.
Epidural steroid injection intend to place steroid in epidural space. Epidural steroid is used for treatment and prognostic procedures.
These injections were performed with blind approach, with advent of fluoroscopy. These injections in form of transforaminal blocks were given.
- Caudal epidural steroid involves introducing needle into epidural space through sacral hiatus. More amount of fluid needs to be given via this route.
- It is easy to perform and decrease risk of inadvertent dural puncture and inadvertent intrathecal injection. Local anesthetic has been shown to be convenient vehicle for introduction of steroid. It provides temporary relief of pain and onset of numbness in appropriate dermatome can be used as indication such that correct spinal segment has been infiltrated.
Lumbar Epidural Steroids
- Needle is passed through interlaminar space along midline through interspinous ligament needle must penetrate ligamentum flavum but fall short piercing the dural sac.
- Disadvantage is penetration of dural sac, so needle should be safely be advanced precisely into epidural space.
- Advantage directed closely to assumed site of pathology. Drug to being injected is delivered to its target. Lesser volume needs to be injected to assume that target site is reached.
- Results with small doses 2 ml are equivalent to those with large (10–45 ml) or intermediate volumes. Frequency—one to three injections some have used up to 6 months; if benefits perceived.
Efficacy of epidural steroids is controversial.
- Bernan et al—epidural steroids does not cure the disease but provide prolonged pain relief.
- Abrahm and Flopwood et al—factors with poor outcome were also associated with poor results with epidural steroid.
- These are low socioeconomic status, smoking, lack of employment, constant pain: Sleep disruption, nonradicular pain, delayed diagnosis, prolonged duration of pain; change in recreational activity, extreme values on psychological scales.
Lumbar epidural injections—large number of previous medicine for pain, high intake of medication, pain not necessarily increased by activity, increased by coughing, unemployment due to pain, pain that does not interfere with daily activities. Normal SLR before treatment.
Age, duration of pain, pattern and frequency of pain intensity, results of physical examination, presence or absence of structural pathology. There is no relationship between emotional distress and outcome.
- Best results were found in patient with subacute/chronic leg pain with no prior neurological deficit and worst with those with motor or reflex abnormality. Negative myelogram is associated with good result.
- Cuckler et al did double blind, randomized study for disk herniation and stenosis and found no difference in result between placebo and single epidural injection.
- Patients with severe changes or with instability are least benefitted.
After epidural steroid injections are successful in relieving pain, thereafter muscle strengthening physical therapy can be started. Epidural steroids are mainly used for diskogenic disease and other sources of pain local effects has been shown to last at least 3 at a desired level.
Epidural steroids should be used in those patients in whom there is medical contraindication to certain oral analgesics and limited ability to engage in therapeutic exercises and those not fit for surgery.
Use of epidural steroid in conjunction with a rehabilitation program may play a very important role in the conservative management of patients with severe radicular pain, improving their quality of life and function.
Disadvantage of caudal entry.
- Need for more volume of drug
- Unrecognized placement of needle outside epidural space.
Epidural should be given fluoroscopically with interlaminar entry due to following problems:
- Extradural placement of needle
- One may erroneously miss targeted interspace by one or two levels.
Advantage of Interlaminar Technique
Disadvantages of Interlaminar Technique
- Blind injection
- Drug injected usually fails to reach
- Desired ventral epidural space is not reached
- Unable to use if postsurgery.
So, fluoroscopy guided epidural injection should be preferred.
Caudal
- Advantage: Drug injected to ventral epidural space and less risk dural puncture.
- Disadvantage: Large volumes needed so low concentration of steroid used blind injection up to 30%, do not reach the target site.
- Post-injection there might be backache, postural headache (0.5–1% for lumbar interlaminar injections and 0.6% for caudal epidural injections), nausea, vomiting, dizziness, and vasovagal reaction. There might be bleeding along the trajectory of the injection, including in proximity to the nerve roots and/or the spinal cord.
- Infection is common in immunocompromised patients and this can include epidural abscess and meningitis. Nerve root injury has also been reported. Other rare complications include anterior cord syndrome, presumably resulting from the injection of particulate steroid into the artery of Adamkiewicz.
- There is the risk of spinal cord trauma if the operator performs direct injection into the spinal cord via an interlaminar approach (a risk that is essentially absent at the lower lumbar spine, since the spinal cord terminates at the level of L2).
Cord trauma can also result from compression of the spinal cord from an epidural abscess or an epidural hematoma. These complications can be averted by using fluoroscopic guidance and contrast enhancement to avoid vascular uptake. (Vascular injection of particulate steroid matter is postulated to increase the risk of central nervous system infarct.)
Critical arteries are found in the posterior aspect of the intervertebral neural foramina and that they may be vulnerable to injection or injury during transforaminal epidural steroid.
Early use of epidural steroid injections (ESIs) can be considered in patients with severe radicular pain that does not respond even to opioid medication or in whom the pain is severely interfering with sleep habits and daily functioning.
Early ESIs also carry theoretical benefit of controlling inflammation at early stage and of preventing permanent neural damage, such as nerve fibrosis from prolonged inflammatory process.
Patients need to be re-evaluated postinjection for need of further injection up to 3–4 injections may be used for acute radicular pain syndromes.
Epidural injections are used in various types of spinal pain. In lumbar canal stenosis, it had mixed results and good with caudal epidural steroids.146
Epidural Steroid are Useful
- If leg pain retains more than 4 weeks, use 3 injections yearly.
- If disk height is maintained and age is less, conservative treatment is to be carried out.
Response Vary Greatly
- Hagen 2002, showed short-term effect 40%, no significant long-term effect.
- Wiesel 1995, showed that 82% had relief for 1 day, 50% for 2 weeks 16% for 2 months. 77% avoid surgery after injection.
- Curette 2002: There is neither significant functional benefit nor reduction in need for surgery.
Epidural steroid are most effective in presence of acute nerve root inflammation.
Patient is asked to grade the degree of pain in 0–10 scale before and intervals after subjective spinal injection.
- Epidural injections provide pain relief during recovery of injury with/without radiculopathy.
- Information obtained is helpful in confirming pain generators and source of patient diskomfort.
- Structural abnormality do not always cause pain and diagnostic injections can help to correlate abnormal imaging studies with associated pain.
- Epidural injection—pain relief during recovery of disk, nerve root injuries in patients during their level of physical activities, severe pain from acute disk. Therapeutic injection help to manage pain and may alleviate or if need for oral analgesics. Disadvantage—not well controlled studies.
- Many steroid injections were done without fluoroscopic guidance position of needle, and interpretion is doubtful. Several studies reported usefulness of transforaminal epidural corticosteroid to identify origin of specific root as pain generator.
- It appears to be most beneficial in patients with radicular pain, fluoroscopy guidance may be helpful, if bloody tap is obtained or if CSF is encountered procedure is to be aborted.
- Vijay Vad and Atul Bhat had shown that fluoroscopically guided transforaminal injection serve as important tool in nonsurgical management of lumbosacral radiculopathy with success rate of 84% as compared to 48% for group receiving trigger point injections.
Everett et al showed that flushing as side effect of following lumbar transforaminal injection in up to 11% patients.
Epidural steroids are less effective and multiple level injections are more effective than are single level was described by Tae kyu Park and Ji Hee Hong.
For post-laminectomy patients, J Huang showed that transforaminal injections has better pain relief than caudal.
Transforaminal injections are more effective than epidural.
- Those given transforaminal steroids acheived complete relief of pain in 50% at end of one month (54% patients) against those treated with local anesthetic or transforaminal injection of saline (19%). Intramuscular steroids (21%) or intramuscular saline (13%). Relief of pain was proportional to improvement in disability.
- Transforaminal epidural steroid for lumbosacral radiculopathy with a preganglionic approach is more effective than transforaminal epidural steroid and ganglionic approach at short-term follow-up—Hee Sum Jeong et al.
- Jennig HS also showed similar results, transforaminal injections are superior to placebo as surgery sparing intervention and superior to interlaminal epidural steroid injection, ESI for radicular pain.
- Transforaminal epidural steroid injection is not diagnostic.
Lumbar ESIs may be indicated for lumbar radicular pain associated with any of the following conditions:
- Symptomatic acute or acute or chronic PID.
- Spinal stenosis with radicular pain (central canal stenosis, foraminal and lateral recess stenosis)
- Compression fracture of the lumbar spine with radicular pain
- Facet or nerve root cyst with radicular pain.
Cervical epidural steroid have been used to treat following conditions:
- Pain associated with acute disk herniation and radiculopathy
- Postlaminectomy cervical pain
- Cervical strain syndromes with associated myofascial pain.
Thoracic epidural steroids have been reported in the medical literature as treatment for pain associated with following conditions:
- Acute thoracic disk pathology
- Thoracic radicular pain secondary to disk herniations
- Trauma
- Degenerative scoliosis
- Thoracic compression fracture.
Fluoroscopy should not be used in epidural injections for women who are pregnant.
- Benefits of epidural steroids include relief of radicular pain and low back pain (with leg pain generally relieved more than back pain), facilitation of the ability to participate in physical therapy, improvement of quality of life, reduction of analgesic consumption, and improvement in the maintenance of work status.
- Patients with symptoms of shorter duration have more sustained relief than those with chronic pain.
- Patients with chronic back pain will generally have better response if they develop an acute radiculopathy.
- In a cross-sectional study design at a university spine center, 76 patients with sciatica were followed for a mean of 122 days after receiving transforaminal ESIs. Of these patients, 47% experienced improvement, 28% were unchanged, and 16% worsened.
If the radicular pain is form a recurrent herniated nucleus pulposus after lumbar spinal surgery, epidural steroid is beneficial.
- In 2002, Lutz and colleagues reported a prospective randomized study comparing transforaminal lumbar epidural injection with lumbar paraspinal trigger-point injection.
The success rate in the transforaminal injection group was 84%, compared with 48% in the saline group.
- Botwin and colleagues demonstrated the efficacy of transforaminal epidural injection in their retrospective cohort study in patients with sciatica (caused by lumbar spinal stenosis). 34 patients who did not respond to nonsteroidal anti-inflammatory agents and oral analgesics received 1.9 injections (average). At 1 year, 75% of patients had greater than 50% pain reduction, 64% improved their walking duration, and 57% increased their standing tolerance. The injections can obviate the need for hospitalization and surgery in many patients.
- Riew et al reported results from a prospective, randomized, double-blinded, controlled clinical trial on 55 patients with severe sciatica from spinal stenosis or lumbar disk herniations. These patients had not responded to 6 weeks of conservative treatment and were considered to be surgical candidates.
- The study demonstrated that only 23% of patients in the group that received lumbar epidural steroids needed surgery, while 67% of patients in the bupivacaine injection group underwent surgery.
There is more evidence favoring the use of transforaminal epidural steroids in the lumbar spine, compared with the cervical spine.
- Barre et al reported that in patients with symptomatic lumbar spinal stenosis who received caudal epidural steroids.
Long-term treatment success was seen in 35% of patients after a mean follow-up of 32 months.
Management of chronic pain from postlumbar laminectomy syndrome and spinal stenosis, the evidence is level II-1 or II-2 for caudal epidural injections.
- Rhee et al found that those patients who underwent transforaminal injections had a 46% reduction in their pain score, and 10% needed surgery. In contrast, patients who had interlaminar injections had a 19% reduction in pain, and 25% required surgery.
- Evidence is limited for blind interlaminar epidurals in managing lumbar pain, but there is short-term relief of pain secondary to disk herniation and radiculitis.
- The delay in surgical decompression was not found to be detrimental to neurologic recovery at time of follow-up.
- A prospective study by Rowlingson and Kirschenbaum described significant reduction in upper limb pain after cervical epidural steroids, transforaminal cervical epidural steroids are preferred over the interlaminar approach.
- Negative aspiration of blood does not ensure a lack of vascular uptake. Similarly, in the cervical spine, vascular uptake injections occurred at a rate of nearly 20% even with the use of fluoroscopy (confirmed by contrast injection), via a transforaminal approach.
- Study involving 191 patients who underwent single-level lumbar transforaminal epidural injection, simultaneous epidural and vascular injections were found to be 8.9%.
- In a randomized study comparing the effectiveness of dexamethasone and triamcinolone used in cervical transforaminal epidural injection, found that at 4 weeks postinjection, both groups exhibited statistically and clinically significant improvement. Although the dexamethasone was slight less effective than triamcinolone.
- Epidural injections without fluoroscopy showed level II-2 evidence for short-term relief of pain of radiculitis utilizing blind interlaminar epidural steroid injection and level III for long-term disk herniation and radiculitis.
- Evidence is level III for short and long-term relief for spinal stenosis and diskogenic pain without radiculitis/disk herniation utilizing blind epidural injections.
- Evidence of effectiveness of epidural steroids in managing chronic spinal pain ranged from limited to strong is shown by Abdi S, Datta S.
- Evidence is limited in post-laminectomy syndrome and moderate for chronic low backache as described by Abdi S, Datta S.
- Bush and Hiller evaluated outcome and periradicular and epidural corticosteroid injection for cervical myelopathy, 93% obtained symptomatic relief for 7 months with average of 2.5 injections per patients to obtain adequate pain control.
- Rull et al evaluated 249 patients with lumbar root compression by means of epidural injection. Injectate include 10 ml of 0.25% bupivacaine and 80 mg of methylprednisolone. 63% with prolapsed intervertebral disk and 37% spinal stenosis, results were good in 66%, however, 78% of patients showed complete relief after a year.
- Cagler et al administered 80 mg of methylprednisolone in 25 patients at 2 weeks interval all had lumbar disk herniation.
After first injection there was some response to treatment, after second, improvement continued. However, after third there was no change in objective or subjective pain relief.
- Fukasaki et al showed that interlaminar epidural steroid injections were not effective for spinal stenosis.
- Manchikanti described cost effectiveness of caudal epidural and transforaminal over interlaminar block.
- Strans studied evidence for overall effectiveness of interlaminar epidural steroid injection in managing chronic low backache is moderate for short-term relief and limited for long-term.
- Evidence for interlaminar epidural steroid is strong for short-term and limited for long-term relief in managing lumbar radiculopathy whereas for cervical radiculopathy it is moderate.
- Evidence for transforaminal epidural steroid is strong for short-term and moderate for long-term improvement in managing lumbar nerve root pain whereas moderate for cervical.
- Evidence for transforaminal epidural injections/sensory nerve root block in preoperative evaluation of patients with negative/in conclusive imaging studies is moderate.
- For nerve root pain and pain secondary to lumbar post-laminectomy-percutaneous epidural adhesiolysis, spinal endoscopic adhesiolysis evidence is strong for short-term relief and moderate for long-term relief.
Fluoroscopy and the use of contrast media are clearly necessary for cervical epidural injections.
- Validity of selective nerve root blocks is not established. No difference in effect were found between lidocaine and bupivacaine.
- In cervical and thoracic epidural injections, a total of 3–5 ml may be used for ESIs employing the interlaminar approach. However, in cervical and thoracic transforaminal, clinicians generally use a total volume of only about 1.5–2 ml. Volume used for lumbar ESIs is slightly greater, generally being 6–10 ml for interlaminar ESIs, up to 20 ml for caudal ESIs, and 3–4 ml for transforaminal ESIs.
For epidural injections, many physicians prefer to use steroid preparations without preservatives. Single-dose vials of the corticosteroids, generally do not contain benzyl alcohol.
Becker and colleagues studied the use of autologous conditioned serum containing enriched IL-1 antagonist, for lumbar transforaminal epidural injections for radiculopathy. In comparison with triamcinolone 10 mg, the autologous conditioned serum injection had the same efficacy at 22-week follow-up with respect to pain reduction.
- It was first used by Robecchi and Capra, who injected steroid in spinal nerve root—earliest use of transforaminal route for epidural steroid.
Contraindications
- Altered anatomy, congenital anomalies or previous surgery.
- Patient with bleeding diasthesis, fluid retention, adrenal function may be decreased in 2–3 weeks.
Unwilling patients, untreated infections, pregnancy, allergy to medications and dye, concurrent use of anticoagulant medications, systemic infections, immunosuppression, severe cardiovascular compromise, structural anomaly preventing access to epidural space.
Congenital anomalies/previous surgery may have altered normal anatomy of epidural space, neurological disease. Cauda equina syndrome, rapidly progressive neural deficit.151
- Price and colleagues (2000) have found that 35% of caudal and interlaminar injections performed without fluoroscopic guidance were not made in appropriate location.
- Difficulty may be encountered with placement of injectate below. For S1 nerve root there is risk of dural puncture.
- Post-puncture headache.
- Trauma of the needle to spinal cord.
- Anterospinal artery syndrome is complicaiton of transforaminal epidural injections.
- Other complicatins—transient hypotension, severe paresthesia.
- Adrenal function may be suppressed for 2–3 weeks.
Risks associated with inserting needle is spinal headache from dural puncture, bleeding, infection, allergic reaction and nerve damage and paralysis, steroids side effects may also be seen.
Numbness/weakness must resolve within 8 hours in affected arm/leg.
- Steroids flush—flushing of face and chest that can last several days and accompanied by feeling of warmth on low grade increase in temperature, anxiety, trouble sleeping, changes in menstrual, temporary water retention, these side effects are mild and resolve with treatment.
- Kushner and Olson reported retinal hemorrhage in 5 patient, with bleeding diasthesis.
- Desio et al—facial flushing and erythema in patient after epidural steroid most serious was bacterial meningitis most others are transient.
- Rapid admission of large doses of steroid is also contraindicated.
- Most common problem is 25% rate of failure to place material.
- Intrathecal injection is a technical problem.
Complications
Related to improper needle placement
- Pain at injection site
- Nerve root, spinal cord injury
- Epidural hematoma, epidural abscess
- Meningitis
- Osteomyelitis
- Postural puncture headache.
General side effects:
- Weakness in lower extremity due to motor block
- Cardiac arrhythmias
- Seizure
- Hypertension
- Steroid side effect like transient weight gain, hyperglycemia, hypertension, facial flushing.
- Intra-arterial injections are associated with paraplegia reported in three cases.
Spinal arachnoiditis is associated with epidural depo-medrol. These complications are caused by celestone in solution. Triamcinolone acetonide provides immediate 152and long-term duration of action, soluble with no harmful preservative. Isotonic saline is only other injectable medium used frequently around spine.
Useful Tips for Injection Technique
- Palpate bony landmarks and soft tissue, and mark site of injection.
- Do thorough skin preparation.
- Skin should be infiltrated and local anesthetic, with quick insertion of needle into joint causes minimum pain.
- Most procedure should be done in supine positions.
- There should be gap of at least 3 weeks preferably between the injections. If there is possibility of sepsis/septic arthritis or localized infection, do not inject.
- Always aspirate before injection and always needle should be properly fitted to syringe. Warn patient of pain and counsel regarding post-procedure protocol.
- Maximum benefit will be in initial days postinjection with better response to smaller joints. Large joints should not be injected simultaneously.
- Not to inject into vessel/nerve/damage articular cartilage.
- Strict asepsis with no touch technique and disposable needle and syringe are important.
- Direct needle to target.
- Confirm needle tip position with contrast.
- Inject medication slowly.
- Tissue feel soft tissue and bone.
- Fluoroscopic visualization, AP later and oblique view, radiopaque contrast used for confirmation.
- Tissue feel is important when in bone one is rest assured that it has not penetrated blood vessel/nervous tissue.
Technique
- Epidural needle 18–20 gauge 3–5 inch (Fig. 6.17)
- Spinal needle 22–25 gauge 5 inch short bevel needle
- 23 gauge 5 inch for giving local anesthetic
- 5 ml syringe
- 10 ml glass syringe (Fig. 6.20)
- Contrast
- Intravenous sedation can be used
- Medications corticosteroid preparation
- Volume: Interlaminar total volume 6–8 ml
- Transforaminal: Total dose per level 4 ml (both side).
Interlaminar Approach (Fig. 6.19)
Position: Prone with bolsters over lateral aspects of abdomen and flanks and abdomen hanging free, this opens up interlaminar space.
- Parts are painted and draped and local anesthesia is given after palpating interlaminar space and marking it.
- It position the needle one level below the site of suspected pathology due to cranial flow of solution in epidural space. There is no potential for deviation of needle toward the nondependent side.
- A 20 gauge epidural needle is advanced into lamina, using superior border of inferior lamina for support by walking off the lamina till ligamentum flavum is punctured. At this point there is loss of resistance. Carefully advance needle till loss of resistance is detected after entering epidural space. 1–2 cc of radio- contrast dye is injected to confirm the position (Fig. 6.18).
- Depth of insertion at point at which lamina is contacted, called critical depth. If done under C-arm guidance needle advanced to upper edge of lamina lateral to midline.
- After contact with lamina, needle is turned toward lamina and slowly advanced cephalad medially until contact is appreciated with ligamentum flavum. Once needle has engaged ligament, resistance to syringe pressure is tested.
- Loss of resistance to injection is tested intermittently as needle is slowly advanced through the ligamentum flavum. Indicates entry into epidural space is abrupt loss of resistance.
- When syringe diskonnected nothing should flow from needle.
- If CSF leaks due to punctured thecal sac, procedure is abandoned.
- Aspiration should be done before injection. 1–3 ml of nonionic contrast medium should be injected. Pattern of dispersal of contrast medium confirms spread to epidural space.
- Once correct placement of needle is confirmed, steroid anesthetic mixture should be given.
Note: In interlaminar fluoroscopically guided injections, C-arm is oriented at 5–10 degree to open the interlaminar space. In the caudal approach one thing to be kept in mind is that needle should not be advance to higher than S2–S3 junction, if so, then there can be potential intrathecal spread/neural toxicity and post-procedure headache.
Transforaminal Approach (Figs 6.12, 6.21 to 6.28 and Flow Chart 6.5)
Position: Prone with bolsters over lateral aspects of abdomen and flanks and abdomen hanging free. Starting in AP position and confirm the position and level of vertebrae.
- Then move C-arm to 15–30 degree such that proper scotty dog picture can be visualized.
- Target is 6 clock position of pedicle.
- Skin marking is done and skin and subcutaneous tissue is infiltrated with local anesthetic 2% lidocaine.
- Contrast medium should not be allowed to reach next spinal nerve. 1 ml is sufficient to outline target nerve. If flow is in peripheral direction, the needle should be adjusted such that it is in central.For this, it is required that 2–3 ml syringe be used and injected slowly at 1 ml per 30 second approximately. There would be evoked pain.
- Caution: No spread into dura or intravascular spread, once dye spread is confirmed, steroid anesthetic mixture is injected.
TRANSFORAMINAL BLOCK
Target point is base of pedicle above target nerve 5°–30° position on right and 6°–30° position on left, target point lies at apex of safe triangle. The needle is directed in an oblique approach to a target point on the apex of an imaginary triangle (the “safe triangle”), formed by a line tangential to the lower margin of pedicle, a line tangent to the lateral margin of the pedicle, and the hypotense passing obliquely inferiorly and laterally from the inferior medial corner of the pedicle. Advancement is made under lateral and anteroposterior views to provide a 3-dimensional spatial representation.
- Needle tip directed into this triangle will be above and lateral to nerve will not incur damage to any other structure or significant risk of morbidity.
Tips for Injection
- Spinal needle is inserted through skin and back muscles along an oblique approach.
- Puncture point in oblique view of target foramen apex of superior articular process of ipsilateral segmental facet joint points directly upward towards target pedicle. Needle is passed just above and lateral to apex.
- Needle is advanced towards base of pedicle until further advance is arrested tip position should be confirmed on AP and lateral view.
- Once in correct position injections is made. Appropriate pattern of spread is important in which the contrast medium spreads ventral to nerve root sleeve curving upward and medially around pedicle, extending medially into epidural space. Peripherally the contrast medium outlines coarse of ventral ramus. Then steroid anesthetic mixture is injected.
In transforaminal block, key to needle placement is to see pedicle enface:
- Needle is directed toward undersurface of pedicle, since nerve roots are oriented obliquely it is better to be as close to undersurface of pedicle as possible.
- Needle is advanced to the posterior aspect of neural foramen and then advanced slowly anteriorly.
- Once needle is in midportion of neural foramen. AP view should be taken to show extension of contrast medium along perineural fat and into epidural space.
- Most authors believe that placement of needle at 6 O'clock position allows ample spread of therapeutic agent along nerve root sheath into epidural space without entering the thecal sac contacting dorsal root ganglion. Many place needle at 5 O'clock–7 O'clock depending on laterality, believe that this placement gives greater distribution to dorsal root ganglion. Lateral epidural space spread—anesthesis two levels at a time.
Position: Prone with bolsters over lateral aspects of abdomen and flanks and abdomen hanging free.
Parts are painted with antiseptic solution and draped. With help of C-arm in lateral position useful to feel for sacral hiatus normally and then skin and subcutaneous tissues are anesthetized.
- Needle is advance cephalad towards sacral hiatus at 45° angle. Skin point of entry is such that it is more distal to the visible sacal hiatus and try to walk the needle into the sacrococcygeal ligament with slight resistance followed by loss of resistance. All these steps are carried out under C-arm visualization (Fig. 6.29).
- At this point radiocontrast dye is injected and appropriate spread is reconfirmed in hiatus with C-arm in lateral and AP position (Fig. 6.30).
- Negative aspiration is done before dye is injected to ensure that there is no blood/CSF aspirate.
- Nonionic contrast medium should be injected under C-arm guidance. Localized dense and poor spread of injected indicates needle is superficial.
- Lateral view is taken. If spread is not satisfactory needle should be repositioned and its location once again checked by free flow of contrast media cephalad.
- Volume of approximately 15 ml is used to reach to target segment and 10 ml to reach L5.
Caudal Epidural Steroids (Blinded)
Position: Prone target sacral hiatus palpated between cornu of sacrum. First find coccyx. Finger is then moved cephalad until 2 prominences are felt. Advance needle while infiltrating surrounding overlying tissue, the needle encounter superficial dorsal sacrococcygeal ligament covering hiatus, needle is advanced through ligament and 1–2 ml of lignocaine is injected 22 gauge spinal needle is advanced through sacral hiatus in sacral canal with bevel facing ventrally, once needle is perceived to have entered the sacral canal injectate is provided.
Studies show that interlaminar and epidural injections of steroids are as effective as local anesthetic alone.
Postprocedure
- Monitoring vital parameter is essential.
- It is instructed to apply ice packs if there is blushing and increasing pain, rest is advised and abstinance from driving for 24 hours and increased activity.
Cervical Epidural Steroid
- More safely done under C-arm control was first was given in 1972 through transforaminal approach.
- As there is no control of dispersal of drug into epidural space which depends on anatomy, injection volume and speed of injection and adding to it scarring may obstruct the passage into epidural space. This procedure involves injecting drug into epidural space surrounding the nerve root.
- Because of use of contrast medium and other control it is far more accurate.
Conservative treatment of low backache: Cognitive and behavior, NSAIDs, TENS, biofeedback, pain medicines, rehabilitative therapy second tier: systemic opioids, nerve blocks.
Spinal cord stimulation, cryoanalgesic—apply extreme cold to disrupt their ability to transit pain.
- Radiofrequency lesioning—apply radiofrequency generated heat to nerves to disrupt pain transmission.
- Intradiskal electrothermal therapy—apply heat to seal fissure and dehydrated disk.
- Neuroablation destroy nerve tissue near source of pain. Implantable drug pump to CSF in intrathecal space surrounding spinal cord.
- Neurostimulator—whole level electric impulses to interface with transmission of pain signals to brain.
FACET JOINT (FLOW CHARTS 6.1 TO 6.4)
Facet joint is encapsulated with thin fibrous layer that forms superior and inferior recesses that are filled with small synovial villi or fat pads approximately size of grain of rice. These become inflamed/entrapped between articular process producing pain.
Facet when distended by contrast reproduces pain.
- Articulating facets of C1, C2 are horizontal.
- L2–3 are oblique from horizontal to anchor vertebrae.
- Foramen transverse give passage to vertebral artery and vein and plexus of sympathetic nerves.
- Thoracic vertebrae has articular facet that are directed backward and little lateral ward and upward. In thoracic spine facet joints are in coronal plane permitting rotation and in lumbar spine they are in sagittal plane making rotation impossible.
Vertebral canal is average 17 mm for C3, 4 C6, 7 cord average diameter is 9.5 at C3 and 8 mm at C6.
Intervertebral canals are about 5–9 mm diameter.
Facet joint is cause of pain in 15–45% patient with low backache and 36–67% of patients with neck pain.162
Pathology: Synovitis of Facet Joint
- Gradual onset of swelling.
Facet joint dysfunction follow conditions that forces joint beyond its normal restraints of capsule in synovitis, mechanical locking, osteoarthritis and painful entrapment.
Hemarthrosis
- Swelling within minutes, passive ROM is sluggish, painful.
Manual therapy 120 days.
May involve subluxation or dislocation of facet joint/degeneration of facet itself, exact pathophysiology is unclear.
Chronic persistent neck pain is seen after initial episode of neck pain or whiplash injury.
- There was belief in facet joint as cause of pain since 1933 when Ghormley coined term facet syndrome.Innervation is derived from median branch of posterior primary ramus.
- Patient presents with nonspecific low back, hip and buttock pain which is deep and aching with pain radiating to posterior thigh, but not below knee, pain aggravated by rest and hyperextension, relieved by repeated motion, flattening of lumbar lordosis and point tenderness.
- Rees described radiofrequency denervation in 1971 and Shealy modified technique in 1975.
- Lau and Bogduck described the needle placement parallel to nerve root.
- Goldthwaite believed that lack of symmetry caused irregular movements and subsequent “backache”.
- Badgley—anatomy of L5S1 facet with inferior articular surfaces of L5 widened and more vertically oriented to S1 superior articular facets.
- Persol in 1930 described ligamentun flavum as contiguous structure with facet joint capsule.
- Jeffies 1988 suggested that multilevel innervation is probably one reason why facet joint pain frequently has broad referral pattern.
- Facets are most common source of chronic neck pain—Bomsley et al.
- Hirsch et al and Yomashika et al also reported rich innervation of facet joint altered intersegmental and segmental joint motion and postural distortions create aberrant traffic in nerve pathway.
- Bogduk 1993—used selective block for facet alone 23%, disk alone 20%, disk and facet 41%.
Symptoms of facet joint syndrome in the lower back include:
Pain or tenderness in lower back, that increases with twisting or arching the body, that moves to buttocks or back of thighs—this pain is usually a deep, dull ache, stiffness or difficulty with certain movements, such as standing up straight or getting up out of a chair. Joint injection/interruption of nerve supply is standard for diagnosis.163
Symptoms of facet joint syndrome in neck include:
- Neck pain, shoulder pain, difficulty in rotating the head.
There are several possible causes of pain that originates in a facet joint.
- An injury and/or changes associated with aging might cause cartilage to wear away causing pain.
- Irritation of median branch of dorsal ramus nerves also lead to pain.
- Poor posture, causes malalignment, is a factor in development of pain from the facet joints. Trauma, inflammation, infection, and disk degeneration are other causes of facet joint pain.
Delphi Experts Diagnostic Criteria for Facet Arthropathy
- Positive response to facet joint injection.
- Localized unilateral low back pain.
- Positive medial branch block.
- Pain upon unilateral palpation of lumbar zygapophyseal joints or transverse process.
- Lack of radiation features.
- Pain eased by flexion.
- Pain if defined, located above the knee.
Arthritis of Facet Joint was Defined by James in 2007
- Neuronal sensitization, neurogenic inflammation, injured facets heighten the pain sensitivity. Tight muscle secondarily brings facetal arthritic changes.
- Myofascial back pain is the 2nd most common cause Long et al 1996.
- Glial cells develop facilitatory circuits that magnify pain.
In early degeneration there is subchondral sclerosis and cyst and osteophytes with joint space narrowing and medial angulation of posterior joint.
In Disk Height Reduction
- Facet joint capsule becomes lax
- Increase load transfer to facet joint
- Accelerate degeneration
- Joint subluxation hypertrophy osteophyte formation.
Facet joint syndrome—synovial joint innervated by nerves, degenerate in concert with disk space.
Pain and extension that include standing, working overhead use of sweeper, not aggregate/relieved by sitting, walking and lying down and morning stiffness.
Stiffness in flexion and increase pain on extension especially lateral position, no sign of nerve root tension, irritation or compression.
Ghormley was firstly declared that lumbar facet joints could be a source of back pain.
- Von Wijk and colleagues shown procedure on combined outcome measures but improved outcome was seen in selected individuals only.
- Intra-articular injection shows 46–75% of short-term pain relief, 20–36% following a single injection.
Sciatic type of symptoms in facetal arthritis alone has a lifetime incidence of between 15% and 40%.
Hildebrandt et al—Pathology causing pain is located in exact peripheral location.
- Local anesthesia totally abolishes sensory reflex of nerves and does not affect other nerves.
- Relief and attributed to block only.
- Relevance of nerve block in treatment and diagnosis of LBP is quality decisive.
Comparative LA blocks may not be implementable for intra-articular blocks for it is not known whether placement of LA in vascular environment effected its expected duration of action.
Positive Revel's tests increase the likelihood to modest degree that pain is from facet joint and negativity reveal that likelihood of positive result from block is low.
- In old population there is 40% chance of facet joint pain.
Facet joint block requires multilevel screening, i.e. negative predictive value and then screening. Single level at a time, if there is partial response to multilevel blocks in screening as facet pain may originate at multiple levels.
Facet joints are innervated and capable of causing pain similar to that seen clinically and are source of pain in patient with chronic spinal pain. Controlled diagnostic facet joint block can be used to establish diagnosis of facet joint pain.
Diagnostic accuracy of facet joint block is strong to be conclusive, based on compliance with criteria evaluating diagnostic test.
- False positive rate of pain relief in facet joint is 27–63% in cervical spine, 42–58% in thoracic and 17–50% in lumbar spine.
- Intra-articular injection of facet joint is more difficult; it might cause over distension of joint and may be associated with significant leakage of intra-articular injected fluid into epidural space and spillage over to the nerves.
- Median branch block is diagnostic procedure of choice if radiofrequency ablation is to be done.
Radiofrequency neurotomy might be necessary to relieve pain and improve mobility. It is more effective than intra-articular block and requirements of steroid is much low.
Accuracy is strong in diagnosis of lumbar and cervical facet joint pain and moderate in thoracic facet joint pain.
- Cook and Robinson et al 2008 described that, for facet joint pain single injection has 30% placebo response and reference standard is double fluoroscopically guided injections.
- Clinical features usually do not match with diagnostic blocks, age > 65 years, pain relieved in supine, lying, absence of pain aggravated by coughing/flexion/return from flexion/extension.
- Manchikanti et al 2000, showed sensitivity 13–17% and specificity 34–92% for diagnosis of facetal pathology by facet joint blocks.
- Falco FJ Erhart S showed that evidence for diagnosis of cervical facet joint is level I or II-1 same is for therapeutic cervical medial branch. Block showed level II-1, evidence is lacking for intra-articular injection, level II-1 or II-2 for radiofrequency neuroablation.
- Evidence for diagnosis of cervical facet joint pain with controlled comparative local anesthetic block is level I or II-1 and evidence for therapeutic block is also the same.
- Multiple uncontrolled reports of percutaneous radiofrequency neurotomy in cervical spine are encouraging.
Radiofrequency Techniques
- Implies facet joint denervation—has temporary efficacy.
- In comparison with sham procedure, it is better than sham procedure shown by Van Kleef—Spine 1999.
- Anatomic study suggests that penetration into epidural space occurs following rupture of joint capsule. This provides explanation by which therapeutic results can be obtained if large volume is used.
- In intra-articular facet joint block there is short and long-term pain relief. Medial branch blocks evidence is moderate for short and long-term pain relief, for median branch neurotomy evidence is moderate. Short and long-term pain relief—Boswell et al. Relief is better for lumbar pain then cervical.Among diagnostic intervention accuracy of facet joint nerve block is strong in diagnosis of lumbar and cervical facet joint pain whereas moderate in diagnosis thoracic facet joint pain.
- Response in form of relief from low back pain varies from 52% to79% at 3 months and 35% to 75% at 12 months.
- Facet joints and both disk and facet may be the cause of backache. No historic/physical examination finding can reliably predict response to diagnostic facet blocks. Patient could just have back pain not aggravated by movement, i.e. there are no objective findings except tenderness.
- Manchikanti and Vijay Singh followed up patients for 2 years.
Therapeutic lumbar facet joint blocks show significant improvement in pain > 50%, functional improvement of > 40% for 82 of 100 patients with 5–6 doses and average relief for 19 weeks. In treatment of 438 patients prevalence of facet joint pain was 39% cervical spine, 34% in thoracic pain and 27% lumbar spine, false-positive with single block in cervical region is 45% in thoracic region 92% and lumbar region 45%.
Evidence for therapeutic intra-articular facet injection is moderate for short and long-term improvement and limited for cervical facet joint injection.
Manchikanti et al—Psychological factors failed to influence the diagnostic validity of facet block. No difference is noted diagnosing facet joint pain with LA alone or with mixture of sarapin/sarapin and depo-medrol.
Peterson et al showed that articular branch of lumbar facet joint were too small but parent trunks of articular branch proved suitable for this purpose.
- Evidence for efficacy of cervical and lumbar median branch block is moderate and median branch neurotomy is moderate.
For denervation for facet joint Bogduck angled the image intensifier about 10°–15° so that junction of the super-articular process and transverse process or junction of sacral ala and articular process of S1 is well seen. This allows electrode to be aligned parallel to medial branch with parallel orientation. A greater diameter of lesion has potential to ablate the implicated medial branch.
- Electrodes should not pass the posterior boundary of neural foramen.
- This ensures that entire nerve root and dorsal root ganglion are not ablated inadvertently.
- Unilateral or bilateral denervation typically are based on patient symptomatology.
- For medial branch 60 sec ablation with 80/6C is used.
Indications of facet joint block:
- Focal tenderness over facet joint
- Low backache without sciatica
- Post-laminectomy
- Recurrent disk disease
- Persistent low backache after stable posterior lateral spinal fusion.
Performed Under Image Intensifier
- Position: Prone with bolsters over lateral aspects of abdomen and flanks and abdomen hanging free.
- Needle is inserted through puncture site and directed under image intensifier guidance to target joint. It is worthwhile to rest the needle tip on either inferior or superior articular process of joint, for this establishes critical depth of insertion. Subsequently needle needs to be readjusted slightly to enter joint space and needs to be inserted just beyond initial depth (Fig. 6.35).
Fig. 6.32: Site of injection for facet joint block and transforaminal block in oblique view of spine
It becomes difficult if needle becomes embedded in articular cartilage.
Needle should just penetrate capsule. In chondromalacia, rheumatoid arthritis, PV NS, entering on superior aspect of joint space deep through the capsule but peripheral to margins of articular cartilage is preferred. Less than 0.3 ml of contrast medium is used for confirmation with small syringe.168
In oblique view dumbbell shape is characteristic—slender tract of contrast medium outlines the intercartilaginous joint space and connect collection of contrast medium in superior and inferior subcapsular pockets (Fig. 6.36).
Lateral view—diskoid silhouette is outlined, if not in joint cavity then medium is seen to spread beyond vicinity of joint in a radiating pattern (extension between fibers of multifidus contrast media spread out of joint cavity through capsular foramina into extracapsular superior and inferior joint recesses) (Fig. 6.36).
Such extension is not sign of extravasation/joint rupture. It is due to lobulated smooth edge collection consistent in outline of the fat deposits in inferior and superior articular recesses. Not more than 1 ml of agent is injected. If difficulty is in entering the joint at its midpoint, needle is redirected to superior/inferior subcapsular pockets at superior and inferior pole of joint. The capsule is lax leaves subcapsular pockets.
Needle should be readjusted to upper and lower edge of joint, still contacting bone of articular process and then readjusted, so that it passes tangential to joint margin. Penetrate just enough to reach capsule.
Deep penetration risks spread to the subcapsular pocket and re-emerge from joint ventral to joint cavity.
LUMBAR MEDIAN BRANCH BLOCK
Position: Prone with bolsters overlateral aspects of abdomen and flanks and abdomen hanging free.
- With help of C-arm anteroposterior view is taken and level is confirmed.
- In AP fluoroscopic imaging, identify transverse process, e.g. L1 through L1, median block; penetrate the skin using 22 gauge or 25 gauge 3’3 inch spinal needle at and superior to target location.
- The C-arm is rotated in ipsilateral oblique fashion till scotty dog configuration is seen.
- For medial branches the target position for needle is at junction of base of transverse process and superior articular processes (contact is made with dorsal superior and medial aspect of base of transverse process so that needle rests against the periosteum) (Fig. 6.34).
- Under C-arm guidance needle is advanced to this target position. Once the needle hits bone at this point, it is walked off the bone. Needle position is then checked in lateral position 1 ml of radioconstant dye is injected to confirm that it is not intravascular. Steroid anesthetic mixture is then injected.
- Avoid penetrating the intermediolateral foramen with inadvertent paresthesia of nerve root on spread of injectate to epidural space.
- For intra-articular blocks similarly C-arm is rotated obliquely from 15–45 degree looking out for facet joint space (at the ear of scotty dog) and facet joint is identified after which needle is penetrated up to the middle portion of superior articular process as we reach the bone and hit the needle is slide medially and after resistance of facet joint capsule is felt there is sudden give 171away. Care is to be taken to prevent inadvertent rupture of capsule by giving small amount of injectate (0.5 ml).
Procedure for blocking the medial nerve at L5 differs from the above since target point here is the superomedial aspect of sacral ala.
If one wants to block the facet joint L4–L5, medial branches to be blocked will be l3 and l4 which runs at the level of L4 and L5 transverse processes respectively.
Due to dual innervation, two medial branch blocks are required. At transverse process of L4 and L5 medial branch at transverse process of L5. S1 medial branch passes across sacral ala.
For S1 identify sacral ala rotate C-arm 15–20 degree ipsilateral obliquely to get exposure between ala and superior articular process of S1.
A 22–25 gauge, 3/2 inch spinal needle into osseoligaments landmarks rest spinal needle on periosteum and position the bevel of spinal needle medial and away from foramina. Inject 0.5 ml.
Procedure is simple, safe and easy; contrast medium is use with no reported ill effects.
Postprocedural Care
Fever, new onset weakness in extremities. Severe unrelieved pain, etc. is to be looked out for.
Patient should also keep follow-up to record their improvements in pain.
They should refrain from driving or operating heavy machinery on day of procedure.
Complications
Bleeding, infection, postprocedural radicular pain, the dural sac puncture and subsequent spinal headache, allergic reaction to medication possible vasovagal reactions.
Procedure related complications:
- Wrong level
- Transient in pain
- Transient radicular sensory change
- Dural puncture and headache
- Complication cervical: Puncture of vertebral artery
- Penetration of epidural and subarachnoid space and parasites and leakage of LA.
- Ataxia/unsteadiness
- Steroid weight gain, water retention, flushing, mood swings, insomnia.
Myofascial Pain
- Is referred pain that emanates from myofascial trigger point common sites piriformis muscles and quadratus lumborum.
- Aching and deep pain which increase with activity or prolonged sitting with hip adducted flexed and internally rotated.
- Myofascial pain of quadratus lumborum—false sign of disk syndrome.
- Superficial fibers—sharp aching in low back; iliac crest, greater trochanter can extend to abdominal region. Deep fibers—SI joint or low buttock region.
SACROILIAC JOINT BLOCK (FIG. 6.38 AND FLOW CHART 6.5)
- Fluoroscopically guided articular blocks are preferred.
- One must eliminate lumbar spine and hip pain before considering SI joint pain. Sensitivity 94% and specificity 78% for 3 or more test.
- Sacroiliac joint pain might have placebo response to single blocks. Sacroiliac joint has diffuse innervation and nerves do not have fixed course, hence SI joint pain can be approached through SI joint block.
It is innervated by ventral roots of sacral plexus anteriorly and posteriorly by dorsal rami of S1 to S4.
When sacroiliac pain is unilateral it is better.
- With continued gluteal pain there is possibility of sacroiliac arthropathy which can mimic radicular symptoms or secondary myofascial pain.
For SI intra-articular injection moderate for short-term relief and limited for long-term relief.
Risk of infection, bleeding and allergic reaction should be diskussed prior to the procedure.
Radiofrequency neurotomy for SI joint pain is limited.
Procedure
Position: Prone with bolsters over lateral aspects of abdomen and flanks and abdomen hanging free.
In view, SI joint showing multiple shoe lines running parallel to each other. In semiparallel fashion more medial of these lines are formed by posterior margins. C-arm should be rotated usually to contralateral side so as to have all margins superimposed along caudal 1/3 of joint line.
Target point 1–2 mm cephalad of inferior end of joint line. After identifying target point local anesthetic is injected to skin and subcutaneous tissue to target point.
A 22–25 gauge curved tip needle is targeted to hit sacrum, felt hard locate the needle at joint line, needle first touches iliac or sacral side of joint, needle is then slide into the joint.
Once needle has struck the sacrum it should be withdrawn slightly and redirected towards joint space.
Entry into joint is recognized by loss of bony resistance as tip slips between sacrum and ilium.
Needle should not go too deep as it may emerge into presacral tissue anteriorly and injure artery.
Once in joint space intra-articular injection is confirmed with contrast medium. If needle is correctly positioned injection of 0.3 to 0.5 ml of contrast medium would be flowing cephalad in lateral view. Contrast medium densely outlines the joint margins.
Under fluoroscopic guidance steroid anesthetic mixture is injected.
Discography
- As disk height increases relative to vertebral body height so does ROM.
- Shape of disk varies per region.
- In thoracic spine, anterior and posterior have same measurement disk to vertebrae ratio is low so movement is limited in C spine. The disks are wedge shaped and are all anteriorly thick especially C5.
- First described by Lindblem in1948 elaborated by Hirsch in 1948.
- Wise in 1957—fluoroscopically guided injection of radiopaque contrast into lumbar intervertebral disk is used as means of treatment planning for initial or repeat lumbar spine surgery. It was widely accepted as diagnostic aid by radiologist and neurosurgeons.
- Myelography provides little information regarding architecture and integrity of intervertebral disk.
Diskogenic back pain is seen in internal disk disruption, degenerative disk disease and segmental instability.
Olmasta (1995, Spine)—Disk herniation pain is due to inflammation, mechanical and vascular compression.
- Disk material is perceived as antigen, intense inflammatory response is put up.
- Neurofilament protein and S100 increase in CSF there is axonal and Schwan's cell damage. But no reduction of NCV.
- Vascular compromise at nucleus pulposus to nerve root may be the cause. Increase endoneural pressure, causing compartment syndrome. There may be decrease blood flow in dorsal root ganglion.
- Discography would thus be useful in evaluation of both disk morphology and clinical relevance.Central portion of disk is mucoid in structure and outer annulus fibrosis is composed of dense collagen, as disk degenerates the nucleus becomes less fluid in nature and vertical stress upon the disk are altered in their distribution due to which fissuring and tearing of annulus may occur and this will cause significant patient diskomfort, it may cause adjacent nerve root compression. Anatomic correlates of high intensity zones seen in MRI are strongly correlated with pain.
- There may be multiple level of disk pathology. Pain, elicited or not, with individual disk space injection was an accurate reproducer of patient.
- As disk height increases relative to vertebral body height so does ROM.
- Shape of disk varies with region.
- In thoracic spine, anterior and posterior disk heights are same. Disk to vertebrae height ratio is low so movement is limited in lumbar spine. The disks are wedge shaped and are all anteriorly thick especially L5.
- Pain treatment could be directed only at level of concern and remaining disks though they may appear abnormal radiographically could be ignored.
- During myelography mass effect on spinal nerves is all that could be visualized.
- Entire outer 1/3 of annulus fibrosus and posterior longitudinal ligament and anterior aspect of thecal sac and nerve roots is innervated by nociceptive fibers.
- These also extend peripherally along annulus at foraminal levels so can explain symptoms related to foraminal and lateral disk pathology, when there is no actual nerve root contact by disk material. So pain originating from process that involves outer 1/3 of annulus and posterior longitudinal ligament appears justified.
- Whether pain elicited during discography that correlates with patients. Baseline pain is secondary to mechanical/biochemical/inflammatory/combination is less certain.
- Injection of radiopaque contrast helps CT evaluation of intradiskal anatomy and MR imaging has also been proposed in this regard subtle annular tears and disk protrusions not visualized on radiography can be seen.
- Eliciting the nature of pain during intradiskal injection is vital. Pain concordent with baseline pain is valuable in determining which levels to be injected.
- Some believe that intradiskal pressure measurement during procedure may be of some value.
- To determine if intervertebral disk is source of chronic spinal pain.
Components
- Sterile needle placement into the center of IVD.
- Radiocontrast instillation to provoke pain.
- Radiological assessment of disk morphology.
- Clinical assessment of intensity of evoked pain in related to baseline.
Lumbar Discography Identifies Symptomatic and Pathological IVD's
- Helpful in patient with low back or lower extremity pain
- Information obtained may not be sufficient to guide invasive treatment for diskogenic pain
- CT discography is more accurate then myelography
- Discography is superior to plain CT
- Discography is a good as MRI.
Relationship of discography to outcomes including conservative management minimally invasive surgery and open procedures remains controversial.
Disk as source of pain (centralized) is an argument against surgery, described by Berthelof et al (2007).
There is no substantial difference in outcomes of long-term nonoperative treatment and fusion was shown by Mirza and Deyo (2008).
- Discography is usually asked for wherein need to avoid other joint block internal disk disruption (IDD) is most common cause of diskogenic pain 49% in those with abnormal disk on MRI. IDD is most likely if diskogenic pain is present, if disk stimulation shows painful disk at multilevel, then it should not be targeted for treatment.177Patient with bilateral back pain are highly unlikely to have bilateral SI joint pain and SI joint pain is always caudal to L5.
- Discography is often used to determine how many levels should be included in planned fusion in failed back syndrome in which patient have continued or worsened pain without imaging correlate or artifact due to metallic fixation.
- Discography is of value in visualizing disk anatomy and pathology whether disk at level of possible pseudoarthrosis or other abnormality are symptomatic.For intradiskal electrothermal therapy evidence is moderate in managing chronic diskogenic low back pain, for annuloplasty the evidence is limited.
Technique
Approach patient from contralateral side of pain. Patient is placed in comfortable position. To avoid confusing the patient with pain due to needle placement along adjacent nerve root.
With patient in prone position the X-ray beam is oblique to visualize end on at disk and visualize middle 1/3 of intervertebral disk space just anterior to superior articular process.
Coaxial system is utilized in with a 20 gauge introducer needle in outer margin of annulus fibrosus of disk and advance of 25 gauge needle through this outer needle and into middle 1/3 of disk using C-arm guidance.
Position of needle is confirmed by C-arm in both planer reviews.
Contrast is injected to view nucleus pulposus, annulus injections occur due to needle positioned too far ipsilaterally and anteriorly due to difficulty in placing needle from posterior osseous structures.
In severe degeneration distinction between nucleus pulposus and annulus is lost. This can be suspected and anticipated from preprocedure CT or MR.
Prior surgical fusion hardware or bone graft.
The L5-S1 disk level proves to be most challenging due to small osseous window between posterior elements and iliac crest. CT discography shows hamburger/cotton ball appearance of disk.
Nucleus injection can be confirmed by discography whereas annular injection provides detail disk anatomy but misleading and inaccurate pain evaluation.
Some annular tears are painful and this might cause confusion in diagnosis.
Injection into a normal nucleus pulposus without annular tear/other disruption will not elicit pain. Not all abnormal appearing disks are symptomatic.
The amount of contrast injected and joint at which symptoms were reproduced is recorded discogram at a particular level is noted to be concordant or diskordant.
Pressure at initiation of patient's pain and maximum pressure measurement achieved during discogram is measured.
Pain at very low pressure during the injection are related to chemical pain and associated with annular tears resulting in decreased containment of injectate within the nucleus.
Risks associated with procedure are infection, hematoma, nerve injury, to avoid it smaller gauge needle is preferred.178
Most feared complication is diskitis, use of preprocedural antibiotics and coaxial needle technique have decreased risk of infection.
- Diskitis—Persistent pain different from usual patient pain, fever, or abnormal laboratory studies as WBC count and C reactive protein. MRI is useful to rule out postprocedure diskitis and repeat CT also is valuable in evaluation of endplate osteomyelitis.
Use of preprocedure antibiotics is controversial. Adherence to sterile technique is vital.
Avoid sedation as it may hamper the pain provocation test and also avoid giving local anesthetic at outer annulus.
VALUE OF DISCOGRAPHY
- There is lack of gold standard for assessment of a successful post-surgical outcome and role discography played in achieving that outcome.
Procedure is safe and there are rare cases of infection, nerve injury and bleeding complications.
Carnagee and Colleagues in 2004 showed that there is possibility of long-term nerve pain secondarily to injection.
- Some studies showed that discography is of clinical utility in surgical planning and used to determine operative levels. It is of value in preoperatively planning for spine surgery.
- There was considerable uncertainty over the validity of findings obtained by discography.
First study was done by Holt in 1968 to challenge against discography.
In 1990, Walsh presented results of discography in symptomatic and asymptomatic subjects when pressure of injection is controlled and low back pain is rare and pain does not occur generally the result of discography were proven to correlate with image of IV disk.
- North American Spine Society also released a review in 1991 that discography is valuable tool.
- Madan and colleagues found no significant difference in operative outcomes between groups who have undergone discography and those not.
Diagnostic blockade of a structure with nerve supply which can generate pain can be performed to test hypothesis that target structure is source of patient's pain.
Testing hypothesis by provoking pain in any structure is unreliable criterion except provocative discography. Relief of pain is essential criterion in all except lumbar disks. When source of pain is at multiple sites then picture is confusing.
Controlled block must be used, but due to ethical reasons it is prohibited.
Placement of local anesthetic and different pain duration may not be effective in a vascular intra-articular environment, with medial branch blocks use of comparative local anesthetic blocks has been validated and found to be valid.
Double blocks and comparative LA are required as diagnosis cannot be rendered reliable on basis of single blocs. Interval of 1 week should be used for most of intervention except for cancer pain can be to months or longer between each injection provided, at least 50% relief is obtained for 6 weeks.179
Treat all regions at some time safely for all types of blocks. Number of injection per year should not exceed 4 and for sympathetic block 6/year.
For maintenance only as necessary maximum 6 times for LA with or without steroids per year and intervention like radiofrequency ablation 4 times per year.
For percutaneous nonendoscopic adhesiolysis with a 3-day protocol 2±3 interventions per year are recommended with 1 day protocol.
Blocks may be repeated after 6 weeks if need arises.
No more than 5 procedures should be carried out at a time in different regions and four in single region.
False positive rate may be as high as 40% in facet joint blocks.
PROTOCOL FOR DIAGNOSTIC AND THERAPEUTIC SPINE INJECTIONS FOR BACKACHE (FLOW CHART 6.1 TO 6.4)
- Diskogenic pain is confirmed within one step
- SI joint pain is excluded within one block or confirmed with 2 blocks
- In those whom SI joint pain is not suspected facet joint pain is excluded within one step, screening block or diagnosed within four steps, i.e. 1 screening block, one or two blocks at single level to pin point responsible joint and one confirmatory.
Majority of patients (approximately 40%) will have disk symptoms will undergo discography 60% remaining not all will require SI joint block but 30% will be positive and rest 30% will require it.
- In about 30% of cases SI joint pain will be diagnosed within one block plus a confirmatory block.
- In about 15% cases, investigation will exclude SI joint pain and facet joint pain within 2 blocks only, 15% of cases may require up to four or five blocks to pinpoint painful facet joint.
- On MRI first tumors/infection/metabolic disease are ruled out and if disk is normal in appearance discography should not be undertaken at first instance, also there is low yield of discography in normal looking disk on MRI, so in screening facet joints/SI joints are investigated and if both of these are negative return to considering disk again as source of pain.
If pain located to midline exclude disk pain.
Pain is bilateral exclude SI joint pain which is caudal to 15.
Revel's test increases the likelihood to modest degree of affection of facet joint.
In young age, facet joints are less likely to be source of pain there is negative predictive valve of multilevel facet joint block.181
Single sitting both joints L4-L5.
Multiple joints blocked followed by one joint at a time.
If partial pain relief, then next level is blocked in confirmatory blocks facet joint pain is established in 5 steps.
- Exclude SI joint pain
- 1 screening block to implicate facet joint pain
- 1 or 2 block to pinpoint the responsible joint
- 1 to confirm response.
Manchikanti et al attributed 50% pain from facet joint and 5–10% spinal pain from disk degeneration other than spinal/facet pain, post-laminectomy—scar tissue, disestablished joints, recurrent or repeated disk herniation maximum dose of steroid is 210 mg per year in average person. Multiple injections demonstrate staircase phenomenon that plateaus after 3–4 interventions.
Implantable intrathecal drug administration systems indications: Control of chronic refractory, malignant and nonmalignant therapy.
Intervention should be safe accurate, painless, fast, ethical and wise.
For safety the needle tip position should be known before injecting it.
Particulate steroid should not be injected into artery.
In general, first position patent, then position the image intensifier, and focus on target.
- Percutaneous epidural endoscopic adhesiolysis for refractory low backache secondary to multitude of causes including postlaminectomy syndrome lumbar epidural fibrosis.
- Multilevel disk disruption.
- Multilevel degenerative arthritis.
- It is to be used in failure of conventional caudal and transforaminal epidural injections.
- Indication for disk injection and thermonucleolysis is a positive stimulation and analgesic response in cervical spine and positive disk stimulation in lumbar spine.
FURTHER READING
- Abdi S, Datta S, Trescot AM, et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007;10(1):185–212.
- Abel MS. The radiology of chronic neck pain: sequelae of occult traumatic lesions. CRC Crit Rev Diagn lmag. 1982;20:27.
- Abel MS. Occult traumatic lesions of the cervical vertebrae. CRC Crit Rev Clin Radiol Nucl Med. 1975;6:469.
- Abram SE, Cherwenka RW. Transient headache immediately following epidural steroid injection. Anesthesiology. 1979;50:461.
- Abram SE, Hopwood MB. What factors contribute to outcome with lumbar epidural steroids. In Bond MR, Charlton JE, Woolf CJ, editors: Proceedings of the Vlth World Congress on Pain. Amsterdam, Elsevier. 1991;495.
- Abram SE. Perceived dangers from intraspinal steroid injections. Arch Neurol. 1989;46:719.
- Andersen KH, Mosdal C. Epidural application of corticosteroids in low-back pain and sciatica. Acta Neurochir. 1987;87:52.
- Andersen KH, Mosdal C, Vaernet K. Percutaneous radiofrequency facet denervation in low-back and extremity pain. Acta Neuwcbir. 1987;87:48.
- Aprill C, Bogduk N. The prevalence of cervical zygapophyseal joint pain: a first approximation. Spine. 1992;17:744.
- Aprill C, Dwyer A, Bogduk N. Cervical zygapophyseal joint pain patterns. II: a clinical evaluation. Spine 15:458, 1990. & 6. Ayers CE: Lumbo-sacral backache, N Engl J Med K. 1929;200:592.
- Badgley C. The articular facets in relation to low back pain and sciatic radiation. J Bone Joint Surg (Am). 1941;23(2):481–96.
- Ball J. Enthesopathy of rheumatoid and ankylosing spondylitis. Ann Rheum Dis. 1971;30:213.
- Banerjee T, Pittman HH. Facet rhizotomy: another armamentarium for treatment of low backache. N C Med J. 1976;37:354.
- Barnsley L, Bogduk N. Medial branch blocks are specific for the diagnosis of cervical zygapophyseal joint pain. Reg Anesth. 1993;18:343–50.
- Barry PJC, Kendall PH. Corticosteroid infiltration of the extradural space. Ann Phys Med. 1962;6:267.
- Beliveau P. A comparison between epidural anaesthesia with and without corticosteroids in the treatment of sciatica. Rheum Phys Med. 1971;11:40.
- Benzon HT. Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain. 1986;24:277.
- Beyer W. Das zervikale and lumbale Bandscheiben-syndrom und seine Behandlung mit Novocain-Prednisolon-Injektionen an die Nervcnwurzeln. Munch Med Wochenschr. 1960;102:1164.
- Biella A, Cicognini P. L'acetato di idrocortisone nel trattamento della sindrome sciatalgica. Min Med. 1954;1:1863.
- Billiard JR, Houghton FM. Epidural treatment of acute herniated nucleus pulposus. Anesth Analg Curr Res. IS 1977;56:862.
- Binet EF, Moro JI, Marangola JP, Hodge CJ. Cervical spine tomography in trauma. Spine. 1977;2:163.
- Bogduk N, Colman RRS, Winer CE. An anatomical assessment of the “percutaneous rhizolysis” procedure. MedJAust. 1977;1:397.
- Bogduk N. Clinical Anatomy of the Lumbar Spine and Sacrum. 3rd edition. Edinburgh (UK): Churchill Livingstone. 1997.
- Bogduk N, Macintosh J, Marsland A. Technical limitations to the efficacy of radiofrequency neurotomy for spinal pain. Neurosurgery. 1987;20:529–34.
- Bogduk N, Marsland A. On the concept of third occipital headache. Neurol Neurosurq Psychiatry. 1986;49:775.
- Bogduk N, Valencia F. Innervation and Pain Patterns. Australia: 1991, Churchill-Livingstone considerations. 9th Edition. Philadelphia: J B Lippincott Co; 1930.
- Bogduk N. Greater occipital neuralgia. In Long DM, editor: Current Therapy Neurological Surgery. ed 2, Philadelphia, BC Decker, Inc. 1989;263.
- Bogduk B, Cherry D. Epidural corticosteroid agents for sciatica. Med] Aust. 1985;143:402.
- Bogduk N, Long DM. The anatomy of the so-called “articular nerves” and their relationship to facet denervation in the treatment of low back pain. J Neurosurg. 1979;51:172.
- Bogduk N, Marsland A. The cervical zygapophyseal joints as a source of neck pain. Spine. 1988;13:610–7.
- Bogduk N, Wilson AS, Tynan W. The human lumbar dorsal rami. J Anat. 1982;134:383.
- Bogduk N. A narrative of intra-articular corticosteroid injections for low back pain. Pain Med. 2005;6(4):287–96.
- Bogduk N. Back pain: zygapophysial blocks and epidural steroids. In Cousins MJ, Bridenbaugh PO, editors: Neural Blockade in Clinical Anaesthesia and Management of Pain. ed 2. Philadelphia, JB Lippincott. 1988;935.
- Bogduk N. Local anaesthetic blocks of the second cervical ganglion: a technique with an application in occipital headache. Cephalalgia. 1981;1:41.
- Bogduk N. The anatomy of occipital neuralgia. Clin Exp Neural. 1980;17:167.
- Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine. 1982;7:319.
- Bogduk N. The innervation of the lumbar spine. Spine. 1983;8:286.
- Bogduk N, Twomey LT. Clinical Anatomy of the lumbar Spine. ed 2. Melbourne. 1982;1:224.
- Bonica JJ, Buckley FP. Regional analgesia and LA. In Bonica JJ (ed). Textbook of Management of Pain. Lec & Febriger Philadelphia. 1990;2:1883–996.
- Bonica JJ. Local anesthetic and regional blocks. In: Wall PD, Melzack R (Eds). Textbook of Pain. 2nd ed. Churchill Livingstone, Edinburg. 1989;924:743.
- Bough B, Thakore J, Davies M, Dowling F. Degeneration of the lumbar facet joints: arthrogra-phy and pathology, J Bone Joint Surg. 1990;72B:275.
- Brenner L. Report on a pilot study of percutaneous rhizolysis. Bull Postgrad Contwi Med Univ Sydney. 1973;29:203.
- Bridenbaugh PO, Greene NM. Spinal (subarachnoid) neural blockade. In Cousins MJ, Bridenbaugh PO, editors: Neural Blockade in Clinical Anaesthesia and Management of Pain. ed 2. Philadelphia. JB Lippincott. 1988;213.
- Brown FW. Management of diskogenic pain using epidural and intrathecal steroids. Clin Orthop. 1977;190:72.
- Brownridge P. The management of headache following accidental dural puncture in obstetric patients. Anaesth Intensive Care. 1983;11:4.
- Burke JG, Watson RW, McCormack D, et al. Intervertebral disks which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg (Br). 2002;84-B:196-201.
- Burn JMB, Langdon L. Lumbar epidural injection for the treatment of chronic sciatica. Rheum Phys Med. 1970;10:368.
- Burn JMB, Langdon L. Duration of action of epidural methyl prednisolone. A study in patients with the lumbosciatic syndrome. Am J Phys Med. 1974;53:90.
- Burton CV. Percutaneous radiofrequency facet denervation. Appl Neurophvsiol. 1976/1977;39:80.
- Bush K, Hillier S. A controlled study of caudal epidural injections of triamcinolone plus procaine for the management of intractable sciatica. Spine. 1991;16:572.
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics. Vol 2. Mosby Inc. 2008;1955–2029.
- Campbell AJ, Wells IP. Pigmented villonodular synovitis of a lumbar vertebral facet joint. J Bone Joins. 1982;564A:145.
- Carette S, Marcoux S, Truchon R, et al. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engi J Med. 1991;325:1002.
- Carrera GF, Williams AL. Current concepts in evaluation of the lumbar facet joints. CRC Crit Rev Diagn Imag. 1984;21:85.
- Carrera GF. Lumbar facet arthrography and injection in low back pain. Wise Med J. 1979;78:35.
- Carrera GF. Lumbar facet joint injection in low back pain and sciatica: preliminary results. Radiol-W. 1980;137:665.
- Catchlove RFH, Braha R. The use of cervical epidural nerve blocks in the management of chronic head and neck pain. Can Anaesth Soc J. 1984;31:188.
- Chan ST, Leung S. Spinal epidural abscess following steroid injection for sciatica: case report. Spine. 1989;14:106.
- Cicala RS, Westbrook L, Angel JJ. Side effects and complications of cervical epidural steroid injections. J Pain Symptom Manage. 1989;4:64.
- Clark CR, Igram CM, ei Khoury GY, Ehara S. Radiographic evaluation of cervical spine injuries. Spine. 1988;13:742.
- Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophyseal (facet) joint pain. Anesthesiology. 2007;106(3):591–614.
- Cohen SP, Stojanovic MP, Crooks M, et al. Lumbar zygapophyseal (facet) joint radiofrequency denervation success as a function of pain relief during diagnostic medial branch blocks: a multicenter analysis. Spine J. 2008;8(3):498–504.
- Collier BB. Treatment for lumbar sciatic pain in posterior articular lumbar joint pain. Anaesthesia. 1979;34:202.
- Cronen MC, Waldman SD: Cervical steroid epidural nerve blocks in the palliation of pain secondary to intractable tension-type headaches. Pam Symptom Manage. 1990;5:379.
- Cuckler JM, Berini PA, Wiesel SW, et al. The use of epidural steroids in the treatment of radicular pain. Bone Joint Surg. 1985;67A:53.
- Cuckler JM. Correspondence. J Bone Joint Surg. 1986;68A:789.
- Daly P. Caudal epidural anesthesia in lumbosciatic pain. Anaesthesia. 1970;25:346.
- Davidson JT, Robin GC. Epidural injection in lumbosciatic syndrome. Br JAnaesth. 1961;33:595.
- Delaney TJ, Rowlingson JC, Carron H, et al. Epidural steroid effect in nerves and meninges. Anesth Analg. 1980;59:610–4.
- Derby R, Kine G, Saai J, et al. Response to steroid and duration of radicular pain as predictors of surgical outcome. Spine. 1992;17:S176.
- Destouet JM, Gikiia LA, Murphy WA, Monsees B. Lumbar facet joint injection: indication, technique, clinical correlation, and preliminary results. Radiology. 1982;145:321.
- D'Hoogue R, Compere A, Gribmont B, Vincent A. Peridural injection of corticosteroids in the treatment of the low back pain/sciatica syndrome. Acta Orthop Bels. 1976;42:157.
- Dilke TFW, Burry HC, Grahame R. Extradural corticosteroid injection In management of lumbar nerve root compression. BMJ. 1973;2:635.
- Doit MA. Arthrography of the cervical facet joints. Radiology. 1983;148:379.
- Dooley JF, McBroom BJ, Taguchi T, McNab I. Nerve root infiltration in the diagnosis of radicular pain. Spine. 1988;13:79.
- Dory MA. Arthrography of the lumbar facet joints. Radiology 140:23, 1981. Presentation of an operative procedure. JAMA. 1933;101:1773.
- Dougherty JH, Fraser RAR. Complications following intraspinal injections of steroids. Neurosurg. 1978;48:1023.
- Dugan MC, Locke S, Gallagher JR. Occipital neuralgia in adolescents and young adults. N Engi J Med. 1962;267:1166.
- Dussault RG, Nicolet VM. Cervical facet joint arthrography. J Can Assoc Radiol. 1985;36:79–80.
- Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: a study in normal volunteers. Spine. 1990;15:453.
- Eisenstein SM, Parry CR. The lumbar facet arthrosis syndrome. Bone Joint Surg. 1987;69B:3.
- El-IChoury G, Ehara S, Weinstein JW, et al. Epidural steroid injection: a procedure ideally performed with fluoroscopic control. Radiology. 1988;168:554.
- el-Khoury G, Renfrew D, Walker C. Interventional musculoskeletal radiology. Curr Probl Diagn Radiol. 1994;23:161–203.
- Eslberg CA. The extradural ventral on ondromas (eccondroses) their favourite sites, the spinal cord and root symptoms they produce and their surgical treatment. Bull Neurosurg Inst. 1931;1:350–66.
- Evans W. Intrasacral epidural injection in the treatment of sciatica. Lancet. 1930;219:1225.
- Fairbank JCT, Park WM, McCall IW, O'Brien JP. Apophyseal injection of local anesthetic as a diagnostic aid in primary low-back pain syndromes. Spine. 1981;6:598.
- Florez G, Erias J, Ucar S. Percutaneous rhizotomy of the articular nerve of Luschka for low back and sciatic pain. Acta Ncurochir Suppl. 1977;24:67.
- Fox JL, Rizzoli LTV. Identification of radiologic coordinates for the posterior articular nerve of Luschka in the lumbar spine. Surg Neurol. 1976;1:343.
- Fragasso V. II prednisolone idrosolubile per via epidurale sacrale nelle lombosciatalgie. Gaz Med Ital. 1959;118:358.
- Friedenberg ZB, Miller WT. Degenerative disk disease of the cervical spine. Bone Joint Surg. 1963;45A:1171.
- Frymoyer JW. Lumbar disk disease epidemiology. Instr Course Lect. 1992;41:217-23.
- Gates EM, Benjamin DJ. Studies in cervical trauma. Cervical fractures. 1967;48:368.
- Ghormley R. Low back pain with special reference to the articular facets, with presentation of an operative procedure. JAMA. 1933;101:1773–7.
- Ghormley RK. Low back pain with special reference to the articular facets, with Glover JR, Arthrography of the joints of the lumbar vertebral arches, Orthop Clin North Am. 1977;8:37.
- Gofeld M, Jitendra J, Faclier G. Radiofrequency denervation of the lumbar zytgapophyseal joints: 10-year prospective clinical audit. Pain Physician.
- Goldthwaite J. The lumbosacral articulation: an explanation of lumbago, sciatica, and paraplegia. Bosf Med Surg. 1911;164:365–72.
- Grant R, editor. Physical Therapy of the Neck and Thoracic Spine. New York. 1988.
- Hadley LA. Subluxation of the apophyscal articulations with bony impingement as a cause of back pain. AJR Am J Roentgenol. 1935.33:209.
- Hadley LA. Apophyseal subluxation. Bone Joint Surg. 1936;18:428.
- Hakelius A. Prognosis in sciatica. A clinical follow-up of surgical and non-surgical treatment. Acta Orthop Scand Suppl. 1970;129:1–76.
- Heikkila JK, Koskenvuo M, Heliovaara M, et al. Genetic and environmental factors in sciatica. Evidence from a nationwide panel of 9365 adult twin pairs. Ann Med. 1989;21:393–8.
- Helbig T, Lee CK. The lumbar facet syndrome. Spine. 1983;13:61.
- Heller CA, Stanley P, Lewis-Jones B, Heller RF. Value of X-ray examinations of the cervical spine. BMJ 1983;287:127.
- Hickey RFJ, Tregonning GD. Denervation of spinal facets for treatment of chronic low back pain. N Z Med J. 1977;8S:96.
- Hildebrandt J, Jansen J. Vascular compression of the C2 and C3 roots-yet another cause of chronic intermittent hemicrania? Cephalalgia. 1984;4:167.
- Hildebrandt J, Argyrakis A. Percutaneous nerve block of the cervical facets-a relatively new method in the treatment of chronic headache and neck pain: pathological-anatomical studies and clinical practice. Manual Med. 1986;2:48.
- Hirsch D, Ingelmark B, Miller M. The anatomical basis for low back pain. Acta Orthop Scand. 1963;33:1.
- Hirsh C, Ingelmark B, Miller M. The anatomical basis for low back pain. Studies on the presence of sensory nerve endings in ligamentous, capsular, and intervertebral disk structures in the human lumbar spine. Acta Orthop Scand. 1963;33:1–17.
- Houston JR. Study of subcutaneous rhizolysis in the treatment of chronic backache. R Coll GenPract. 1975;25:692.
- Hove B, Glydensted C. Cervical analgesia facet joint arthrography. Neuroradiology. 1990;32:456.
- Jansson H Jr, Bring G, Rauschning W, Sahistedt B. Hidden cervical spine injuries in traffic accident victims with skull fractures. Spin Dis. 1991;4:251.
- Jansen J, Markakis E, Rama B, Hildebrandt J. Hemi-cranial attacks or permanent hemicraniasequel of upper cervical root compression. Cephalalgia. 1989;9:123.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. Edition 1. 2007;149–73.
- Jayson MIV. Degenerative disease of the spine and back pain. Clin Rheum Dis2:SS7t 1976.
- Key JA. Low-back pain as seen in an orthopaedic clinic. Am J Med Sci. 1924;168:526.
- King JS, Lagger R. Sciatica viewed as a referred pain syndrome. Surg Neurol. 1976;5:46.
- Knight G. Post-traumatic occipital headache. Lancet. 1963;1:6.
- Korhonen F, Karppinen J, Malmivaara A, et al. Efficacy of infliximab for disk herniation-induced sciatica: one-year follow-up. Spine. 2004;29:2115–9.
- Lau LSW, Littlejohn GO, Miller MH. Clinical evaluation of intra-articular injections for lumbar facet joint pain. MedJAwt. 1985;143:563.
- Lau P, Mercer S, Govind J, et al. The surgical anatomy of lumbar medial branch neurotomy (facet denervation). Pain Med. 2004;5:289–98.
- Lawrence JS, Sharp J, Ball J, Bier F. Rheumatoid arthritis of the lumbar spine. Ann Rheum Dis. 1964;23:205.
- Lawrence JS, Bremner JM, Bier F. Osteoarthrosis: prevalence in the population and relationship between symptoms and X-ray changes. Ann Rheum Dis. 1966;25:1.
- Lewin T. Anatomical variations in Iumbosacral synovial joints with particular reference to subluxation. ActaAnat. 1968;71:229.
- Lewin T, Moffet B, Viidik A. The morphology of the lumbar synovial intervertebral joints. Acta Morphol Neerland Scand. 1962;4:299.
- Lewinnek GE, Warfield CA. Facet joint degeneration as a cause of low back pain. Clin Orthop. 1986;213:216.
- Lilius G, Laasonen EM, Myllynen P, et al. Lumbar facet joint syndrome: a randomised clinical trial. J Bone Joint Surg. 1989;71B:681.
- Lilius G, Harilainen A, Laasonen EM, Myllynen P. Chronic unilateral back pain: predictors of outcome of facet joint injections. Spine. 1990;15:780.
- Lindahl O, Rexed B. Histological changes in spinal nerve roots of operated cases of sciatica. Acta Orthop Scand. 1951;20:215–25.
- Lippit AB. The facet joint and its role in spine pain: management with facet joint injections. Spine. 1984;9:746.
- Lora J, Long DM. So-called facet denervation in the management of intractable back pain. Spine. 1976;1:121.
- Lynch MC, Taylor JF. Facet joint injection for low back pain. Bone Joint Surg. 1986;68B:138.
- Magora A, Schwartz TA. Relation between the low back pain syndrome and X-ray findings. Scand J Rehab Med. 1976;S:115.
- Maigne R. Low back pain of thoracolumbar origin. Arch Phys Med Rehab. 1980;61:389.
- Manchikanti KN, Boswell MV, Singh V, et al. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004;5:15.
- Mayer ET, Herrmann G, Pfaffenrath V, et al. Functional radiographs of the craniocervical region and the cervical spine: a new computer-aided technique. Cephalalgia. 1985;5:237.
- McCormick CC. Arthrography of the atlanto-axial (C1-C2) joints: technique and results. J Intervent Radiol. 1987;2:9.
- McCulloch JA, Organ LW. Percutaneous radiofrequency lumbar rhizolysis (rhizotomy). Can Med AssocJ. 1977;116:30.
- McCulloch JA. Percutaneous radiofrequency lumbar rhizolysis (rhizotomy). Appl Neurophvsial. 1976/1977;39:87.
- Mehta M, Salmon N. Extradural block. Confirmation of the injection site by X-ray monitoring. Anaesthesia. 1985;40:1009–12.
- Mehta M, Sluijter ME. The treatment of chronic back pain. Anaesthesia. 1979;34:768.
- Mehta M. Facet joints and low back pain. BMJ. 1978;1:1624.
- Mixter WJ, Barr JS. Rupture of the intervertebral disk with involvement of the spinal canal. N Engl J Med. 1934;211:210–5.
- Mooney V, Robertson J. The facet syndrome. Clin Orthop. 1976;115:149.
- Mooney V. Facet joint syndrome. In Jayson MIV, editor: The Lumbar Spine and Back Pain, ed 3, Edinburgh, Churchill-Livingstone, 1987.
- Moran R, O'Connell D, Walsh MG. The diagnostic value of facet joint injections. Spine. 1986;12:1407,123.
- Murtagh FR. Computed tomography and fluoroscopy guided anaesthesia and steroid injection in 125 facet syndrome. Spine. 1988;13:686–9.
- Nelson D. Dangers from methylprednisolone acetate therapy by intraspinal injection. Arch Neural. 1988;45:804, 1988;27:905.
- Nelson DA, Vates TS, Thomas RB. Complications from intrathecal steroid therapy in patients with multiple sclerosis. Acta Neurol Scand. 1973;49:176.
- Norlen G. On the value of the neurological symptoms in sciatica for the localisation of a lumbar disk herniation. Acm Chit Scand Suppl. 1944;95:1.
- Ogsbury JS, Simon RH, Lehman RAW. Facet denervation in the treatment of low back syndrome. 126. Pain. 1977;3:257.
- Okada IC. Studies on the cervical facet joints using arthrography of the cervical facet joint. Jpn Orhop Assoc. 1981;55:563.
- Oudenhoven RC. Articular rhizotomy. Surg Neuro. 1974;2:275.
- Oudenhoven RC. Paraspinal electromyography following facet zhizotomy. Spine. 1977;2:299.
- Oudenhoven RC. The role of laminectomy, facet rhizotomy and epidural steroids. Spine. 1979;4:145.
- Pai S, Sundaram L. Low back pain: An economic assessment in the United States. Orthopedic Clinics of North America. 2004;35:1–5.
- Park WW, Watanabe RYO. The intrinsic vasculature of the lumbosacral spinal nerves. Spine. 1985;10:508.
- Pawl RP. Results in the treatment of low back syndrome from sensory neurolysis of lumbar facets (facet rhizotomy) by thermal coagulation. Proc Inst Med Chicago. 1974;30:150.
- Pedcrsen HE, Blunck CFJ, Gardner E. The anatomy of lumbosacra) posterior rami and meningeal branches of spinal nerves (sinovertebral nerves): with an study of their functions JBJS. 1956;38(2):377–91.
- Pheasant HC, Dyck P. Failed lumbar disk surgery: cause, assessment, treatment. Clin Orthop. 1982;164:93.
- Piersol G. Human Anatomy Including Structure, Development, and Practical Considerations. 9th edition. Philadelphia: J B Lippincott Co; 1930.
- Price CM, Rogers PD, Prosser AS, et al. Comparison of the caudal and lumbar approaches to the epidural space. Ann Rheum Dis. 2000;59:879–82.
- Purkis IE. Cervical epidural steroids. Pain Clin. 1986;1:3–7.
- Rashbaum RF. Radiofrequency facet denervation: a treatment alternative in refractory low back pain with or without leg pain. Orthop Clin North Am. 1983;14:569.
- Raymond J, Dumas J-M, Lisbona R. Nuclear imaging as a screening test for patients referred for intra-articular facet block. Can Assoc Radiol. 1984;35:291.
- Raymond J, Dumas J-M. Incra-articular facet block: diagnostic test or therapeutic procedure? Radiol 138. W. 1984;151:333.
- Rees W. Multiple bilateral subcutaneous rhizolysis of segmental nerves in the treatment of the intervertebral disk syndrome. Am Gen Prac. 1971;26:126–7.
- Rees WES. Multiple bilateral percutaneous rhizolysis. MedJ Aust. 1975;1:536.
- Rees WES. Multiple bilateral subcutaneous rhizolysis of segments! nerves in the treatment of the intervertebral disk syndrome. Ann Gen Pract. 1971;16:126,141.
- Renier JC. Linfiitration epidurale par le premier trou sacre poscerieur. Rev Rhutn Ma-lad Osteoartic. 1959;26:526.
- Rhee JM, Schaufele M, Abdu WA. Radiculopathy and the herniated lumbar disk. Controversies regarding pathophysiology and management. J Bone Joint Surg (Am). 2006;88(9):2070–80.
- Riew K, Yin Y, Bridwell K, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. Joint Bone Spine. 2000;82:1589–93.
- Roberts WA. Pyogenic vertebral osteomyelitis of a lumbar facet joint with associated epidural abscess, Spine. 1988;13(8):948–52.
- Robertson JA. Facet joints and Jow back pain. BMJ. 1978;1:1283.
- Rosen CD, Kahanovitz N, Bernstein R, Viola K. A retrospective analysis of the efficacy of epidural 509. Steroid injections. Clin Orthop. 1988;228:270.
- Rossi U, Pernak J. Low back pain: the facet syndrome. In Lipton S, et al. editors: Advances in Pain Research and Therapy, Vol 13, New York, Raven Press. 1990;p. 231.
- Rowlingson JC, Kirschenbaum LP. Epidural analgesic techniques in the management of cervical pain. Anesth Analg. 1986;65:938, 105.
- Roy DF, Fleury J, Fontaine SB, Dussault RG. Clinical evaluation of cervical facet joint infiltration. Can Assoc Radiol. 1988;39:118.
- Rush J, Griffiths J. Suppurative arthritis of a lumbar facet joint. J Bone Joint Surg. 1989;71B:161.
- Ryan MD, Taylor TKF. Management of lumbar nerve-root pain. Me4 JAust. 1981;2:532.
- Rydevik B, Brown MD, Ludborg G. Pathoanatomy and pathophysiology of nerve root compression. Spine. 1984;9:7.
- Saal JS, Franson RC, Dobrow R, et al. High levels of inflammatory phospholipase A2 activity in lumbar disk herniation. Spine. 1990;15:674.
- Saal JS, Franson RC, Dobrow R, et al. High-levels of inflammatory phospholipase A2 activity in lumbar disk herniations. Spine. 1990;15:683–6.
- Schaerer JP. Radiofrequency facet rhizotomy in the treatment of chronic neck and low back pain. Int Surs. 1978;63:53.
- Schwarzer A, Aprill C, Derby R, et al. The relative contributions of the disk and the zygapophyseal joint in chronic low back pain. Spine. 1994;19:801–6.
- Schwarzer A, Wang S, Bogduk N, et al. Prevalence and clinical features of lumbar zygapophyseal pain. Ann R Heum Dis. 1995;54:100–6.
- Sheaiy C. Percutaneous radiofrequency denervation of spinal facets: treatment for chronic back pain and sciatica. J Neurosurg. 1975;43:448–51.
- Shealy CN. Dangers of spinal injections without proper diagnosis. JAMA. 1966;197:1104.
- Shealy CN. Facets in back and sciatic pain. Minn Med. 1974;57:199.
- Shealy CN. The role of the spinal facets in back and sciatic pain. Headache. 1974;14:101.
- Shealy CN. Facet denervation in the management of back sciatic pain. Clin Orthop. 1976;115:157.
- Shealy CN. Percutaneous radiofrequency denervation of spinal facets. J Neurosurg. 1975;43:448.
- Shealy C. Percutaneous radiofrequency denervation of spinal facets: treatment for chronic back pain and sciatica. J Neurosurg. 1975:43:448-51.
- Shen FH, Samartzis D, Andersson GB. Nonsurgical management of acute and chronic low back pain. J Am Acad Orthop Surg. 2006;14(8):477–87.
- Shulman M, Nimmagadda U, Valenta A. Cervical epidural steroid injection for pain of cervical spine origin. Anesthesiology. 1984;61:A223.
- Shulman M. Treatment of neck pain with cervical epidural steroid injection. Regional Anesth. 1986;11:92.
- Sigwald J, Jamet F. Occipital neuralgia. In Vinken PJ, Bruyn GW, editors: Handbook of Clinical Neurology, Vol 5. New York, Elsevier, 1968;p.36S.
- Silvers HR. Lumbar percutaneous facet rhizotomy. Spine. 1990;15:36.
- Simon D, Carron H, Rowlingson J. Correspondence. Bone Joint Surg. 1985;67A:981.
- Simon DL, Kunz RD, German JD, Zivkovich V. Allergic or pseudoallergic reaction following epidural steroid deposition and skin testing. Regional Anesth. 1989;253.
- Sims-Williams H, Jayson MIV, Eaddely H. Small spinal fractures in back patients. Ann Rheum Dis. 1978;37:262.
- Sims-Williams H, Jayson MIV, Baddely H. Rheumatoid involvement of the lumbar spine. Ann-Rheum Dis. 1977;36:524.
- Siuijter ME, Mehta M. Treatment of chronic hack and neck pain by percutaneous thermal lesions. In Lipton S, Miles J, editors: Persistent Pain: Modern Methods of Treatment, vol. 3, London, Academic Press. 1981;p.141.
- Siuijter ME, Koetsveld-Baart CC. Interruption of pain pathways in the treatment of the cervical syndrome. Anaesthesia. 1980;35:302.
- Smith GR, Becldy DE, Abei MS. Articular mass fracture: a neglected cause of post traumatic neck pain? Clin Radiol. 1976;27:335.
- Smyth MJ, Wright V. Sciatica and the intervertebral disk: an experimental study. J Bone Joint Surg. 1959;40A:1401.
- Snoek W, Weber H, Jorgensen B. Double blind evaluation of extradural methyl prednisolone for herniated lumbar disks. Acta Orthop Scand. 1977;48:635.
- Stambough JL, Booth RE, Rothman RH. Transient hypercorticism after epidural steroid injection. J Bone Joint Surg. 1984;66A:1115.
- Staniey D, McLaren MI, Euinton HA, Getty CJM. A prospective study of nerve root infiltration in the diagnosis of sciatica: a comparison with radiculog-raphy, computed tomography, and operative findings. Spine. 1990;15:540.
- Stanton-Hicks M. Therapeutic caudal or epidural block for lower back or sciatic pain. JAMA. 1980;243:369.
- Stoddard A. Cervical spondylosis and cervical osteoarthritis. Manual Med. 1970;8:31.
- Swerdlow M, Sayle-Creer W. A study of extradural medication in the relief of the lumbosciatic syndrome. Anaesthesia. 1970;25:341.
- Taylor JR, Twomey LT, Corker M. Bone and soft tissue injuries in postmortem lumbar spines. Paraplegia. 1990;28:119.
- Toakley JG. Subcutaneous lumbar “rhizolysis” - an assessment of 200 cases. Med J Aust. 1973;2:490.
- Tuel SM, Meythaler JM, Cross LL. Cushing's syndrome from epidura] methylprednisolone. Pain. 1990;40:81.
- Twomey LT, Taylor JR, Taylor MM. Unsuspected damage to lumbar zygapophyseal (facet) joints after motor vehicle accidents. Med J Aust. 1989;151:210.
- Uyttcndaele D, Verhamme J, Vercauteren M. Local block of lumbar facet joints and percutaneous radiofrequency denervation: preliminary results. Acta Ortbop Bcl# 1981;47:135.
- Van Wijk RM, Geurts JW, Wynne HJ, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005-21;(4):335-44.
- Warfieid CA. Correspondence. Bone Joint Surg. 1985;67A:980.
- Warr AC, Wilkinson JA, Burn JMB, Langdon L. Chronic lumbosciatic syndrome treated by epidural injection and manipulation. Practitioner. 1977;209:53.
- Weber H. Lumbar disk herniation. A controlled, perspective study with ten years of observation. Spine. 1983;8:131.
- Wedel D], Wilson PR. Cervical facet arthrography. Reg Anesth. 1985;10:7.
- Weinberger LM. Cirvico-occipital pain and its surgical treatment. Am Surg. 1978;135:243.
- White AH. Injection techniques for the diagnosis and treatment of low back pain. Orthop Clin North Am. 1983;14:553.
- White AH, Derby R, Wynne G. Epidural injections for diagnosis and treatment of low-back pain. Spine. 1980;5:78.
- Wilkinson M. Symptomatology. In Wilkinson M, editor: Cervical Spondylosis, ed 2. London, Heinemann 1971.
- Williams KN, Jackowski A, Evans PJD. Epidural haematoma requiring surgical decompression following repeated cervical epidural steroid injections for chronic pain. Pain. 1990;42:197.
- Wilson PR. Thoracic facet syndrome-a clinical entity? Pain Sttpp. 1987;4:S87.
- Wiltse LL. Therapeutic caudal or epidural block for lower back or sciatic pain. JAMA. 1980;243:369.
- Winnie AP, Hartman JT, Meyers HL, et al. Pain clinic II: intradural and extradural corticosteroids for sciatica. Anesth Ana-lg. 1972;51:990.
- Woodring ]H, Goldstein SJ. Fractures of the articular processes of the cervical spine. AJR Am J Roentgenol. 1982;139:341.
- Yamazaka N. Interspinal injection of hydrocortisone or prednisolone in dye treatment of intervertebral disk herniation. J Jpn Orthop Assoc. 1959;33:689.
- Yates DW. A comparison of die types of epidural injection commonly used in the treatment of low back pain and sciatica. Rheum Rehab. 1978;17:181.
- Young IA, Hyman GS, Packia-Raj LN, et al. The use of lumbar epidural/ transforaminal steroids for managing spinal disease. J Am Acad Orthop Surg. 2007;15(4):228–38.
Greater trochanter is prominence on lateral aspect of thigh below iliac tubercles. Its posterior edge is easily palpable, anterior and lateral aspects are covered by tensor fascia lata and gluteus medius.
Flexing the leg about 30° and adducting it such that it lies across opposite knee makes trochanter prominent and moves tensor fasciae latae anteriorly.
A bursa lies between iliotibial tract and the bone over bare portion of trochanter.
Posterior superior iliac spine is located beneath sacral dimples. Posterior superior iliac spine is situated at posterior end of iliac crest. It lies at bottom of small skin dimple and at a level of 2nd sacral spine which is lower limit of subarachnoid space.
Sacroiliac joint is not palpable. The center of joint at S2 is crossed by imaginary line through superior iliac crests. The iliac crest is palpated from posterior to anterior.
The anterior superior iliac spine is subcutaneous and is easily palpable.
Coccyx: Inferior surface and tip of coccyx can be palpated in cleft between buttocks about line (2.5 cm) behind anus. The anterior surface of coccyx can be palpated with gloved finger in anal canal.
Sacral hiatus is present in posterior aspect of lower end of sacrum, where extradural space terminates hiatus lies 2 inch above tip of coccyx and beneath skin of cleft between buttocks.
Spinous process of sacrum form middle sacral crest and it can be felt beneath skin in uppermost part of cleft between buttocks.
Lateral cutaneous nerve of the thigh reaches thigh by passing over sartorius muscle, about 2½ cm below anterior superior iliac spine.
It descends through pelvis on surface of the iliacus muscle. It enters the thigh under the inguinal ligament anywhere between anterior superior iliac spine and mid-inguinal point. Nerve pierces the fascia lata just below and medial to anterior superior iliac spine. Path it takes may vary considerably.
Femoral nerve is most laterally placed structure in neurovascular bundle in femoral triangle. Femoral nerve lies almost directly anterior to hip joint.
Gluteus medius originates into outer aspect of ilium between anterior and posterior gluteal lines and inserted on lateral surface of greater trochanter. Its action is abduction and medial rotation of hip. It is supplied by superior gluteal nerve.
Superior gluteal nerve crosses intermuscular plane between gluteus medius and tensor fasciae latae.195
Gluteus maximus originates from posterior gluteal line of ilium, posterior surface of lower part of sacrum and from side of coccyx; and from fascia covering gluteus medius and inserted into iliotibial band of fascia lata and into gluteal tuberosity. Its action is extension and lateral rotation of thigh supplied by interior gluteal nerve.
Psoas major originates from anterior surface of transverse processes and bodies of the lumbar vertebrae and corresponding intervertebral discs and inserted into lesser trochanter of femur. Its action is flexion of hip and flexion of lumbar spine when leg is fixed. It is supplied by segmental nerves from second and third lumbar roots.
Iliacus origins from upper two-thirds of iliac fossa, inner lip of iliac crest, anterior aspect of sacroiliac joint, and from lumbosacral and iliolumbar ligaments. Insertion of lesser trochanter of femur by common tendon with psoas action in flexor of hip. Tilts pelvis forward when leg is fixed, it is supplied by femoral nerve.
Iliopsoas tendon is tendon of the psoas major and iliacus. Iliopectineal bursa separates part of tendon from hip joint. Bursa may communicate with joint. It is usually obliterated in degenerative disease of hip which makes tendon anchored to anterior and medial portions of joint capsule. Femoral artery is at midpoint of inguinal ligament thus directly anterior to hip joint, with psoas muscle interposed between them.
Superior gluteal nerve runs between gluteus medius and minimus muscles approximately 3 to 5 cm above upper border of greater trochanter.
Adductor longus is only muscle of adductor group that can be palpated.
Anterior division of obturator nerve runs down medial side of thigh between adductor longus and adductor brevis, bound to latter. It supplies adductor longus, adductor brevis, and gracilis in thigh. The medial femoral circumflex artery passes around medial side of distal part of psoas tendon.
Adductors do not cover the hip joint, since they all originate below the level of the joint itself.
HIP JOINT (FIGS 7.3 TO 7.5 AND FLOW CHART 7.1)
Indications: Hip joint aspiration is considered in cases of suspected septic arthritis of hip and if collection is nonpurulent, consider giving steroid if noninfective condition is suspected. Consider giving injections under image intensifier guidance. Usually steroids are preferred. It is usually to bye time before surgery for rehabilitation and for medically ill patients.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 80 mg or 120 mg of methylprednisolone.
Syringe: 4 ml and 22 gauge spinal needle.
Hip joint space is identified two inches below and lateral to the midpoint of inguinal ligament lateral to femoral artery, needle is inserted to joint space directly posteriorly and if hit bone then needle is withdrawn and redirected to move superiorly. Alternatively needle is entered at upper border of greater trochanter in mid lateral line and directed inwards and slightly upwards in line parallel with femoral neck.
HIP INJECTIONS: C-ARM GUIDED (FIG. 7.4)
The C arm could be useful for finding proper joint space. First aspirate and look for bleeder, if not then either aspirate the contents or inject steroid.197
Hip injections USG guided:
Hip joint injections are technically more challenging because of danger of penetrating neurovascular bundle. Needle placed using surface landmarks accurately enter the joint only in 52% to 80% cases and it may pass within 4–5 mm of femoral nerve.
Ultrasound can reveal intra-articular and periarticular fluid collection.
Longitudinal approach is used. Transducer is kept parallel to femoral neck and needle is passed into synovial recess at femoral head neck junction.
Position of patient is supine with hip in neutral alignment with mild flexion. Visualize femoral neurovascular bundle, femoral neck, hip joint capsule and anterior synovial recess.
Target location is within anterior synovial recess at femoral head neck junction. In this position, femoral neurovascular bundle is located medial to scan plane.198
A 22 gauge spinal needle is then advanced under direct USG guidance into anterior synovial recess at head neck junction. Small amount of local anesthesia is injected to confirm its free flow.
Duc et al reported increased volume contrast extravasation compared with placement at level of femoral head. Berran et al showed no major complications after USG guided injections. Similarly Sofka et al also reported safety of procedure.
Soft tissue and gluteus maximus crosses the bony posterior portion of greater trochanter. On posterolateral aspect they are protected from it by trochanteric bursa. It is common in female runners. Provocative position is external rotation and adduction. Ober's test may be positive.
Pain is present at greater trochanter. It is palpable only when inflammed/distended. Cause can be pyogenic infection or tuberculosis.
Occurs in acute pyogenic and tuberculosis.
Tuberculosis of bursa does not necessarily involve bone but can be involved from small tuberculous focus in trochanter.
Trochanteric tendinitis—Calcium is first located in tendon adjacent to trochantric bursa with calcification of hip abductors or even in origin of vastus lateralis in distal margin of trochanter. Clinically presents with pain referred to posterolateral aspect of thigh with ruptured lumbar intervertebral disc. Usually responds to heat/injection of appropriate steroid preparation at most multiple perforations with needle with patient under local anesthesia.
Indications: Most of the times bursa is aspirated for purpose of diagnosis. If arthritic etiology is suspected and discharger is nonpurulent then consider giving steroid injection since it is usually accessible. When patient does not want surgery/not fit for surgery these are considered. Injections are preferred in a stage when all other conservative therapies are tried. Pain and inflamed bursa instead of excising can be aspirated.
Figs 7.7A and B: (A) USG appearance of trochanteric bursitis (B) Schematic representation of USG appearance of trochanteric bursitis
Position: Lateral with affected side up and affected hip and leg flexed at knee.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Identify the swelling and insert needle perpendicular to it, till it gives a give- away. Aspirate and if negative and no persistent paresthesia then needle is in bursa (Figs 7.6 and 7.7).
ADDUCTOR TENDINITIS (FIG. 7.8)
Indications: Mostly results from overuse, sports or trauma. If noninfective condition is suspected, consider giving injections under ultrasound guidance. Used in adjuvant to exercises. Usually steroids are preferred.200
Technique
Position: Supine with leg slightly adducted and internally rotated allows access to tendinous insertion of hip adductor muscle. Adductor longus form a distinct ridge from the area of pubic symphysis towards the middle of thigh so palpated when legs are abducted away.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Identify the origin of adductor tendons that lies 1 ½ inch lateral to pubic symphysis from pubic bone (Fig. 7.8).
Insert the needle perpendicular to skin at this point till it touches the bone withdraw the needle by 1–2 mm and inject contents of syringe gently.
Palpate for adductor longus and direct the needle towards the origin of muscle point of needle entry is just below the pubic symphysis in upper part of thigh feel for moderate resistance.
Ultrasonography guided injection is useful for this procedure. Probe is kept both longitudinally and transversly to the contracted muscle and injectate is given at the peritendinous region.
Compressive neuropathy of lateral femoral cutaneous nerve by inguinal ligament. Its supply is L2 and L3. It passes through tunnel formed by small split in lateral end of inguinal ligament. It emerges at lateral border of psoas muscle and crosses iliacus. It is usually caused by repeated external pressure on nerve—leaning against workbench, braces, pregnancy, obesity. Psoas hematoma, mass in iliac fossa, or postoperative scarring of iliac fascia. Symptoms are worsening by prolonged standing or walking. Differential diagnosis includes femoral neuropathy and L3 radiculopathy (Fig. 7.11).201
Patient will present with pain, numbness, dysesthesia and burning over lateral proximal thigh and sensory deficit and tenderness over lateral femoral cutaneous nerve at anterior superior iliac spine.
Indications: Injection steroid are seen to have short-term effect and medium term effect. But conservative treatment is seen to be effective in majority and in order to avert painful episodes these injections are preferred. USG guided injections are preferred to avoid complications, patient not willing/unfit for surgery. They are usually prescribed at the stage when all types of conservative treatment are ineffective or as adjuvant.
Technique
Position: Supine and knee slightly flexed.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted through a point 3 cm medial and inferior to anterior superior iliac spine and inguinal ligament, directly into skin, till pop of piercing internal oblique muscle is heard. After this, drug is injected in fan like manner (Fig. 7.9).
Position of patient and the entry point of needle remains same as above. Transducer is placed such that it is parallel to inguinal ligament 2 cm above it. One end of transducer is towards ASIS and other end is medial to the first, nerve is visualized in cross section and injection is provided surrounding nerve sheath.
ISCHIAL BURSITIS/ISCHIOGLUTEAL BURSITIS (TAILOR'S OR WEAVERS BOTTOM) (FIG. 7.14A)
Lies between ischial tuberosity and gluteus maximus muscle, it may be single or multiloculated.
Ischial tuberosity is located in middle of buttock at approximate level of gluteal fold with fingers over greater trochanter. The thumb is moved from posterior superior iliac spine to ischial tuberosity.
It is easy to palpate it when hip is flexed. It is seen more in occupations involving sitting for long-time.
Patient will usually complain of pain at base of buttock and is brought about by resisted extension of thigh. Pain is localized over ischial tuberosity and it could be referred to hamstrings of affected side.
Patient will have tenderness over ischial tuberosity with pain sharp and catching especially when extending and flexing hip, after this injection there is immediate increase in pain followed by gradual decrease in pain.
Any tenderness while examining the hamstring may result from ischial bursitis.
The anterior and lateral portions are covered by tensor fascia lata and gluteus medius muscle is less accessible to palpation.
Indications: Most of the times bursa is aspirated for the purpose of diagnosis. If arthritic etiology is suspected and discharge is nonpurulent then we can consider giving steroid injection, since it is usually accessible.203
Technique (Fig. 7.12)
Position: Lateral with affected side up and affected leg flexed at knee.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Identify the ischial tuberosity and insert needle perpendicular to it, till it touches bone.
Patient will experience paresthesia in lower limb due to impingement of needle on sciatic nerve.
Withdraw needle and place it medially.
Aspirate and if negative and no persistent paresthesia then needle is in bursa.
GLUTEAL BURSITIS
Bursal fluid rarely found in patients more than 40 years. Bursae lie between gluteus maximus, medius and minimus and well as between these muscle and underlying bones. It is uniloculated/multiloculated.
Pain is present on upper outer region of buttock referred to region of sciatic notch and pain increases on active resisted abduction and extension of lower extremity and by passive flexion and abduction. Greater trochanter and short rotators are present anteriorly. Pain is referred on posterior aspect of hip joint.
Indications: Most of the times bursa is aspirated for the purpose of diagnosis. If arthritic etiology is suspected and discharger is nonpurulent then we can consider giving injection steroid since it is usually accessible. Injections are preferred in a stage when all other conservative therapies are tried.
Technique
Position: Lateral with affected side up and affected hip and leg flexed at knee.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Identify the swelling and insert needle perpendicular to it, till it gives a give away. Aspirate and if negative and no paresthesia present then needle is in bursa.
USG Guided Injection (Fig. 7.12)
Transducer is placed such one end of transducer is at greater trochanter and other end is toward iliac tubercle. If distended bursa is seen, approach and position remains same as that for blind injections.
PSOAS BURSITIS PAIN (FIG. 7.14A)
It lies medially in femoral triangle, between anterior aspect of neck of femur and psoas tendon. In femoral triangle it may be uniloculated or multiloculated.
Cause can be pyogenic and tubercular. It is usually associated with iliopsoas tendinitis seen more commonly in overuse, rheumatoid arthritis, acute trauma, and after total hip replacements.
Patient will present with pain on hip flexion, tenderness, snapping, clicking, grinding and catching. CT guided do not give real time picture and does not allow needle manipulation. It is also used in diagnosis and if there is failure to get relief with this injection other causes of pain should be sought-after.
Once the primary sources of hip pain are ruled out, hip flexors and abductors are next most common. There is inflammation of tendon between pelvis and hip joint capsule anteriorly.
In post THR patients, tendons are shifted more anteromedially. Positive patients are also candidates for surgical release. There may be other causes like labral degeneration/anterior impingement. In patients post-arthroplasty after ruling out aseptic loosening and infection for anterior thigh pain next thing to be done is injection at iliopsoas bursa. It is useful for patients not willing for surgery.
Indication: Mostly bursa is aspirated for the purpose of diagnosis. If arthritic etiology is suspected and discharger is nonpurulent then we can consider giving steroid injection, since it is usually accessible. Injections are preferred in a stage when all other conservative therapies are tried.
Technique
Position: Supine with leg slightly flexed or neutral, allows access to tendinous insertion of psoas muscle.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Approach from anterior aspect of hip. Point of entry is just lateral to the femoral neurovascular bundle and below the inguinal ligament. Feel for moderate resistance and then sudden give away when psoas tendon sheath is reached. Needle needs to go deep approximately 1½ inch. First aspirate to look out for blood, if not, then carry on with further procedure.
Ultrasonography guided injection is useful as psoas bursa is deep and approach is difficult. Position of patient and entry point of needle is same as above. Transducer is kept parallel to the inguinal ligament with one end of probe to the femoral vessels and other end laterally to look for muscle belly.
OSTEITIS PUBIS SYNDROME
Most commonly following surgery over bladder/prostate, less commonly due to rheumatoid arthritis and ankylosing spondylitis with tenderness over pubic symphysis which radiated over inner thigh with waddling gait which can cause secondary problem elsewhere.
Indications: Joint injection is considered when pain is not controlled with all other conservative methods and it is interfering with normal activities of patient. Usually given blinded.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Midpoint of pubic symphysis is palpated and needle is inserted to center of pubic symphysis at right angle to skin till fibroelastic cartilage is reached. If no paresthesia, then inject safely.
COCCYDYNIA (FIG. 7.13)
Pain in coccyx radiating to sacrum and perineum. More common in females usually associated due to trauma like fall/kick usually fracture of coccyx is present. Patient complaints of pain while sitting with tenderness over coccyx and paresthesia over rectum.
Indications: Joint injection is considered when pain is not controlled with all other conservative methods and it is interfering with normal activities of patient. Usually given blinded or under image intensifier control.
Position: Prone and head on a pillow turned away with internal rotation of leg and heel with abduction of leg. This makes sacrococcygeal joint identification easy.206
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Place finger into natal cleft and palpate sacrococcygeal joint at base of sacrum. Needle is inserted at 45 degree to sacrococcygeal ligament and joint, after insertion give away sensation is felt and heard. Drug is then injected (Fig. 7.13). It is useful to use image intensifier guided injection with same approach by visualizing joint.
COXA SALTANS
Iliopsoas snapping is due to overuse and impingement of abnormal acetabular margin.
There is band which is usually thickened posterior border of iliotibial band or anterior border of gluteus maximus. There is iliotibial band friction.
Lateral margin of thigh fascia lata is thick and forms band passing from iliac crest to upper border of tibia. It stabilizes knee in extension and partial flexion.
There is audible/palpable/visible snap when tense fascial band slides over superior margin of greater trochanter as the hip is flexed adducted/internally rotated.
It may be painful/habitual.
It is classified as external: Involving greater trochanter and soft tissue over it.
Internal: Iliopsoas tendon and structure behind it.
Intra-articular—synovial chondromatosis, loose bodies. Fracture fragments and habitual subluxation.
External derangement: Thickened posterior border of IT band and anterior border of gluteus maximus.
Internal derangement: Flexion of hip, iliopsoas shift laterally in relation to center of femoral head. When extended it slides medially across femoral head.207
It is produced due to snapping against prominence of iliopectineal ridge/ exostosis of lesser trochanter over prominent iliopsoas bursa.
Indications: Injection steroid are seen to have short-term effect. But conservative treatment is seen to be effective in majority and in order to avert painful episodes these injections are preferred. It is also provided in symptomatic patients with repeated clicks. Preferred in those who do not wish to get operate/unfit for surgery. For snapping IT band, it is useful to inject on the origin of IT band.
Technique
Position: Lateral with affected side up and affected leg flexed at knee.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Injectate is provided over the origin of iliotibial band.
Ultrasonography guided injections are helpful especially dynamic studies can help in visualizing the offender and injections can be given site specific.
FUTHER READING
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics. Vol I, 11th ed. Mosby Inc. 2008;885-905.
- Govaraert LHM, van der Vis HM, Marti RK, et al. Trochanteric reduction osteotomy as a treatment for refractory trochanteric bursitis. J Bone Joint Surg. 2003;85B:199.
- Howard CB, Vinzberg A, Nyska M, et al. Aspiration of acute calcareous trochanteric bursitis using ultrasound guidance. J Clin Ultrasound. 1993;21:45-7.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. Edition 1. 2007;201-90.
- John O Neill. Musculoskeletal Ultrasound Anatomy and Technique. Springer Inc. 2008;20-330.
- Rumack C, Wilson S, William J. Diagnostic Ultrasound, Vol 1. 2nd edition Mosby Inc. 1998;843-83.
- Slawski DP, Howard RF. Surgical management of refractory trochanteric bursitis. Am J Sports Med. 1997;25:86.
- Solbiati L, Rizzatto G. Ultrasound of Superficial Structures. 1st edition. Churchill Livingstone. 1995;279-375.
- Tynjala P, Honkanen V, Lahdenne P. Intra-articulac steroids in radiologically confirmed tarsal and hip synovitis of juvenile idiopathic arthritis. Clin Exp Rheumatol. Sep-Oct 2004;22(5):643-8.
- Van Mieghem IM, Boets A, Sciot R, et al. Ischiogluteal bursitis: an uncommon type of bursitis. Skeletal Radiol. 2004;33:413.
- Watson Buchaman W. Clinical Examination of Musculoskeletal System. Williams & Wilkins. 1st edition. 1997;25-82.
Flexed knee is easier to palpate from anterior aspect, first the patella is seen. Joining patella and tubercle of tibia lie within patellar ligament. On medial aspect of upper part of patellar ligament in flexed knee lies medial and lateral knee joint line and below. It lies medial tibial plateau and lateral tibial plateau, medial femoral condyle is similarly palpated medial to patella; lateral femoral condyle is more covered with patella. But palpated as distinct edge more in flexion. Head of fibula is palpated below the lateral tibial plateau.
Note: Bursal swelling is localized and intra-articular swelling is generalized, it causes knee to remain in flexion.
Prepatellar bursa aids in stretching of skin over patella especially in flexion it gets inflamed in excessive kneeling and leaning forward.
Prepatellar and superficial infrapatellar bursae are not commonly visualized with ultrasound. Pes anserinus can be seen.
Femur has three borders—the linea aspera and two lateral borders—and three surfaces—anterior, medial and lateral.
Greater trochanter is eminence along posterolateral aspect of proximal thigh. Rectus femoris extends distally as quadriceps tendon. Musculotendinous origin of vastus intermediates is distal to rectus femoris.
Knee joint arthritis or infections are most common reasons for injection intra-articularly. Patient will have pain in knee joint more on getting up from sitting position and sitting cross legged. Patient will have difficulty in climbing, running or contact sports. Knee joint infective synovitis or effusion is associated with distension seen as parapatellar fullness, also patient may present as baker cyst or flexion deformity.
Indications: Knee joint aspiration is considered in cases of suspected septic arthritis of knee and if collection is nonpurulent, consider giving steroid.213
If noninfective condition is suspected, consider giving injections. Usually steroids are preferred. For those patients who require surgery those with severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used to buy time before surgery. Usually given under image intensifier guidance.
Technique
Position: Supine with knee flexed at 45 to 90 degree.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 80 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
For aspiration superolateral aspect of patella (vastus lateralis) is an entry point needle inserted into joint such that it lies between patella inferior aspect and femoral trochlea as it (suprapatellar pouch) is a site of fluid collection and there is no danger of any neurovascular structure getting damage. First aspiration is done and then if fluid is nonexudative, injection steroid is usually provided through same needle (Figs 8.2, 8.3 and 8.5).
For injection, joint line of knee is palpated and needle is inserted through lateral joint line through soft spot besides patella tendon. First aspirate and see and if there is no neurovascular involvement then injection is provided (Figs 8.4, 8.5 and 8.12).
Ultrasonography of knee is also usually done in flexion position (90 degree) for visualizing patellar tendon. Things to be looked out for—synovial hypertrophy, neovascularity of synovial membrane, Hoffa's fat pad. Synovial thickening (thickest measurement is chosen), amount of effusion, extent of effusion in suprapatellar, medial and lateral parapatellar recess. For measuring volume it is important to calculate the sectional area.
Neovascularity seen on Doppler is quantified as 1-minimal 1 or 2 vessels involved, 2-moderate 3 or more vessels and < 50 % of sectional area in vascularized part present, 3 or more vessels and > 50 % of sectional area in vascularized part.216
Keep the transducer over patellar ligament at mid distance between patella and tibial tuberosity of visualization of patellar ligament.
Secondary to inflammation occurs at tendo-osseous junction at inferior pole of patella by repetitive overuse and compressive forces injury [focal mucoid degeneration, fraying, microfoaming].
It is most commonly seen in volleyball and basketball players. It is associated with abnormal patella tracking, chondromalacia, Osgood-Schlatter disease/mechanical malalignment.
Inferior pole may become elongated with periosteal reaction of anterior patellar surface (tooth sign) tendon calcification may be seen.
Stress fracture or disruption of extension mechanism may occur. Tenderness is worse with extension.
Anteroposterior, lateral and tangential view of patella shows radiolucency of involved pole of patella.
The MRI shows findings of degeneration and pathological changes of angioblastic tendinosis, medial thickening is greater on medial portion of extensor mechanism.
Cortisone may increase risk of tendon rupture, delay in treatment result in worse outcomes 2 weeks after tendon rupture, muscle retraction of 5 cm may be present.
Sclerosing injections resulted in significant improvement in function and reduced pain.
Injection treatment is most successful in stage where there is increasing difficulty in performing satisfactory sports activity.
Indications: Injection steroid (given in tendon sheath and peritendinous) or autologous blood or platelet rich plasma (given intratendinous) are seen to have short-term effect and medium-term effect. For long-term exercises and splinting are preferred.
But conservative treatment is seen to be effective in majority and in order to avert painful episodes, these injections are preferred. USG guided injections are useful.
Local injections work in all stages of disease whether rest pain or night pains or pain on activity is present.
Technique
Position: Supine or sitting with knee flexed at 90 degree.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Most tender site near tibial tuberosity is palpated and needle is inserted with moderate resistance felt into the soft tissue and not in patellar ligament. At the 223same time infiltrating into the periphery. If resistance is felt then injection site should be changed.
Patellar tendinitis—USG reveals a hyperechoic area within the tendon. Sagittal and axial plane images acquired with knee in 45 degree of flexion, visualized for hypoechoicity, maximum diameter of area is measured at 3 levels, i.e sagittal plane height, axial plane height, and axial plane width. They are used clinically. Hypoechoic areas can expand/diminish over time and these changes are not always associated with clinical symptoms approach and entry point of needle remains same as above (Figs 8.16 and 8.17).
Position: Hip and knee flexed and foot flat, patella has cortical irregularity, unlike Achilles tendon. Paratendon edema rarely seen but small amounts of deep infrapatellar bursal fluid are normally seen between tendon, tibia and fat pad.
The proximal tibiofibular articulation is an arthrodial joint. The synovium and capsule of this joint may communicate posteriorly with the knee joint. It surrounded by the capsular ligament and the anterior superior and posterior superior ligaments; these extend superomedially from the fibula to the tibia. The posterior aspect of the joint is covered by the popliteus tendon.
Indications: For those patients who has severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance.
Technique
Position: Supine or sitting with knee flexed at 30 degree.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Position is maintained with folded towels. This will widen proximal tibiofibular joint through relaxation of fibular collateral ligament and biceps. Fibular head is palpated, needle is inserted over medial aspect of fibula till give away feel is achieved and contents of syringe are injected (Fig. 8.20).
Alternatively C arm can be used for providing injections. Approach, position of patient and entry point of needle remains same as above.
The USG guided fibular head is palpated and lateral end of transducer is placed over fibular head, medial end is oriented towards inferior pole of patellar. Axis of transducer is perpendicular to proximal tibiofibular joint. Lateral end of transducer is kept steady and medial end is rotated—anterior superior tibiofibular ligament is visualized. Needle is inserted perpendicular to long axis of transducer. The needle tip will lie deep to anterior proximal tibiofibular ligament. Approach, position of patient and entry point of needle remains same as above (Figs 8.18 and 8.19).
Probe is moved inferiorly in an oblique transverse plane to the position where tibia and fibula are in close contact. Tiny vascular structures are present deep to ligament.
TIBIAL COLLATERAL LIGAMENT FIBROSITIS AND BURSITIS
Present between tibial collateral ligament (longitudinal part) and capsule of knee joint. It moves anteriorly with extension and posteriorly with flexion. Fibers are taught in extension and do not relax in flexion.
Patient will present with tenderness over tibial collateral ligament without symptoms of instability, always rule out intra-articular derangement and stress of medial tibial plateau. It presents similar to Pellegrini Stieda disease. There are occasional cases of calcification of bursae.225
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes; these injections are preferred, usually in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications
Technique
Position: Supine or knee in flexion.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Tibial collateral ligament is palpated for tenderness and most tender area is noted. Steroid anesthetic mixture is then infiltrated surrounding the ligament.
FIBULAR COLLATERAL LIGAMENT BURSITIS
It is extrasynovial and lies beneath anterior/posterior to fibular collateral ligament.
Patients will present with pain over lateral aspect of knee, burning aching and stabbing like increase on exercise and decreased on rest. Discomfort exists for months, there might be slight instability but absent locking, there will be pain on full extension, increased mass, radiating to leg motion is full.
Resisted full extension and adduction is painful but signs and symptoms of internal derangement of knee are absent. Always rule out cyst of lateral meniscus and biceps tendinitis. There is no evidence of change in fibrocartilage. There might be multiple small bursae. It may be multiloculated in appearance with surrounding fibrous tissue with flat cells.
If mass are not evident local steroid needs to be given and if evident excise it.
Posterolateral popping is caused by injury to posterolateral corner or by bony tubercle which cause popping of popliteus tendons.
Indications: Same as above.
Technique
Position: Supine or knee in flexion.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Fibular collateral ligament is palpated for tenderness and most tender area is noted. Steroid anesthetic mixture is then infiltrated surrounding the ligament.
Ultrasonography guided: In lateral decubitus position knee flexed to 30 degree and leg internally, rotated upper end of transducer is placed at proximal fibular collateral ligament. Approach entry point of needle and procedure is same as above.226
There are 3 medial bursae, i.e. one separating sartorius, gracillis and semitendinosus from tibial collateral ligament they cross it and second and third separate tendon of semimembranosus from tibial collateral ligament medially and condyle of tibia laterally.
There are 3 lateral bursa, i.e. between biceps and fibular collateral ligament, fibular collateral ligament and popliteus and between popliteus and lateral condyle of femur which is like a tube of synovial membrane around popliteus like that around long head of biceps at shoulder. This bursa communicates with joint.
MEDIAL GASTROCNEMIUS BURSITIS
Presents with mass that extends beneath the head of gastrocnemius and medial head of semimembranosus tendon, usually post-traumatic.
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Supine or knee in flexion.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Patient is asked to contract gastrocnemius by resisted flexion of knee or resisted plantiflexion.
Mass is palpated at medial gastrocnemius origin. Most tender point is marked. Steroid anesthetic mixture is then infiltrated surrounding the tender site.
Ultrasonography guided transducer is kept with one end over the posteromedial aspect of distal end of femur and other end towards posteromedial aspect of tibial plateau. Thickening of tendon and irregular hypoechogenicity is also visualized. Approach entry point of needle and position of patient remains same as above.
SEMIMEMBRANOSUS BURSITIS
Mostly seen in young when associated with overuse and secondarily in old people where associated with degeneration in medial compartment.
It is seen in chondromalacia patellae where gait abnormalities are seen or degenerative medial meniscus tear is seen.
In this condition there is pain over posteromedial aspect of knee.
Bursa is present on medial aspect of poplitial space on either medial or more usually lateral side of semimembranosus tendon.
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes, these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Supine or knee in flexion.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Patient is asked to flex the knee against resistance.
Mass is palpated at semimembranosus insertion. Most tender point is marked. Steroid anesthetic mixture is then infiltrated surrounding the tender site.
Ultrasonography guided injection is useful. Transducer is kept with one end over the medial aspect of tibial tuberosity and other end towards direction of palpable tendon and irregular hypoechogenicity is also visualized. Approach, entry point of needle and position of patient remains same as above.
HAMSTRING TENDONITIS (FIG. 8.21)
Four muscles form hamstring group, i.e. Biceps femoris, adductor magnus, semitendinosus and semimembranosus. They primarily cause flexion at knee joint. Hamstring injury causes prolong recovery time as they are associated with reinjury.
228
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes; these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Prone and knee in slightly flexed position and ankle elevated.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
The needle is inserted after making tendon tight by flexing the knee against resistance and needle is directed towards origin of tendon needle is struck at site of maximal tenderness. Check for paresthesia over tibial and common peroneal nerve and also aspirate before injecting.
Ultrasonography guided transducer is kept with one end over the insertion of tendon and other end towards direction of palpable tendon and irregular hypoechogenicity is visualized. Volume of tendon, fluid collection and distal involvement can be visualized. Normal tendon has echogenic sheen—useful to differentiate it from edema and hemorrhage. It is scanned from insertion to origin of tendon can cause confusion. On USG scarring can be misinterpreted as acute injuries. Recovery of symptoms from tendinitis takes 1 to 2 weeks but USG picture of tendinitis may remain for a long-time. Approach entry point of needle and position of patient remains same as above.
It is defined by biceps femoris tendon superolaterally and semitendinosus muscles medially and gastrocnemius muscles inferiorly. When knee is extended the Baker's cysts are more readily palpated.
Just above medial and lateral femoral condyles the origin of gastrocnemius can be palpated with flexion of knee.
William Morrant Baker described for the first time in England in 1877.
It can arise from each head of gastrocnemius, between hamstrings and collateral ligaments and between hamstrings and tibial condyles.
It is due to herniation of synovial membrane through posterior part of capsule, escape of fluid through normal communication of bursa with knee is known.
Most commonly seen in those with rheumatoid arthritis. These bursae lie between medial head of gastrocnemius and capsule of knee as prolongation between gastrocnemius and semimembranosus. It can present as bursa over medial side of semimembranosus.
In children, it is mostly extra-articular with less recurrence and good prognosis whereas in adults, it communicates with joint and recurrence is seen.229
Intra-articular communication is seen in 50% people of which half are associated with lesion in medial meniscus.
It presents similar to internal derangement of knee.
Ultrasound has sensitivity of 100% in diagnosis. During inflammation, Baker's cyst frequently shows partial thickening, internal septa, echogenic debris, fibrin clots and microcalcifications.
Popliteus tendon can be subjected to peritendinitis.
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes-these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Prone.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 80 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
The popliteal bursa is identified and needle is inserted into the center of bursa in popliteal fossa and first do aspiration to see if needle is in popliteal space and not hit an artery/vessel then after aspiration, inject local steroid.
USG Guided Injection
Popliteal sulcus of lateral femoral condyle is visualized just inferior to proximal fibular collateral ligament (FCL) attachment (Figs 8.24 to 8.26).
Proximal part of popliteus tendon appear oblique in transverse view and traced along its course to posterior aspect of lateral femoral condyle parallel to long axis of popliteus and transducer. Needle inserted enters sheath anterior to FCL and passes deep to FCL. Needle remains cephalic to common peroneal nerve. In transverse view it lies in interval between popliteus and posterolateral femoral condyle (with longitudinal approach this had been difficult). Needle is advanced anterocaudal to posterocephalad directly into sheath anterior to FCL. Position of patient remains same as above.
It lies between anterior surface of lower end of femur and deep surface of quadriceps. Extends up to 3 finger breadths above upper border of patella when limb is at rest in extension. It communicates with joint. Usually seen in those whose job pertains to crawling on knee, like housemaids carpet layers, etc. patient will be unable to kneel or walk downstairs. Patients will complain of sharp 232catching pain with active extension and flexion.
Tenderness will be present just above patella. Boggy swelling in suprapatellar region.
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes; these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Supine and knee in 15°–20° flexion.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Procedure: Patella is pushed to medial side. Identify the superior margin of patella, needle is inserted horizontally beneath quadriceps tendon. Needle is directed more anteriorly and advanced into joint space. If there is significant resistance, needle is in wrong place.
Suprapatellar bursa is very superficial and USG guided injection is usually not required.
PREPATELLAR BURSA (HOUSEMAIDS KNEE) (FIG. 8.29)
It lies in front of lower half of patella and upper half of patellar ligament in area. In this area patellar nerve plexus is present between bursa and skin, it can enlarge to great extend and can give appearance of being dropped. It lies between the subcutaneous tissue and patella. Usually seen in jobs requiring crawling.
Pain in this condition radiates both superiorly and inferiorly over knee as against suprapatellar bursa in which pain radiates superiorly into thigh.
Pyogenic bursitis is common in children who need aspiration; it may communicate with knee joint.
It usually responds to conservative treatment.
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes; these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Supine with flexion of knee 15°–20°.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted horizontally and subcutaneous into prepatellar bursa which is anterior and inferior to patella.
INFRAPATELLAR BURSITIS (CLERGYMAN'S KNEE, PARSON'S OR CARPET-LAYER'S KNEE) (FIG. 8.30)
It is similar to prepatellar bursitis but it is both superficial and deep to ligamentum patellae situated between tuberosity of tibia and patellar tendon and separated from synovium of knee by pad of fat.
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes; these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Supine and flexion of knee 15–20 degree on medial side of lower border of patella, this deep bursa is situated.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted at 45° angle to the skin and needle is inserted at 90° angle to the skin for deep infrapatellar bursa.
Bursal infection presents similar to septic arthritis/osteomyelitis of tibia and loss of full extension of knee with resistance to full flexion. There is tenderness over patellar ligament seen.
It can always be seen as flat 2–3 mm thick anechoic structure.
Proximal tibial metaphysis should be looked for osteomyelitis; bursal effusion should be drained/aspirated without entering knee joint.
Pes anserine bursa lies beneath common insertion of sartorius, gracillis, and semitendinosus on medial side of proximal tibia (Fig. 8.32).
Indications: Injection steroid or autologous blood or platelet rich plasma are seen to have short-term effect and medium-term effect. For long-term, exercises and splinting are preferred. But conservative treatment is seen to be effective in majority and in order to avert painful episodes; these injections are preferred in conjugation with or after other conservative treatments. USG guided injections are preferred to avoid complications.
Technique
Position: Supine and flexion 15°–20°.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Knee is flexed against resistance as pes tendons are flexors of knee; this is how pes anserinus insertion is identified and needle is inserted at angle of 60° to tibia (Figs 8.31 and 8.33).
Ultrasonography guided injection is usually helpful.
Popliteus—main dynamic stabilizer laterally. At ultrasound, tendon is identified at groove and transducer is then moved inferiorly followng oblique course of muscle.
Originates at posteromedial aspect of tibia and curves superolaterally where the tendon passes under arcuate ligament and lateral collateral ligament to insert in popliteal groove at lateral femoral condyle.
Popliteofibular Ligament (Fig. 8.35)
Static stabilizer of external rotation of knee. During flexion lateral collateral ligament becomes lax. USG with knee flexed shows linear hypoechoic structure extending from lateral aspect of popliteus near musculotendinous junction to medial aspect of fibular apex.
Lateral Collateral Ligament
Prevents varus angulation and limits internal rotation of knee. It has a femoral attachment at a point posterior to lateral condyle and anterior to origin of lateral head of gastrocnemius. Distally it forms conjoint tendon with biceps to insert to fibular head.
Knee is extended with varus. Linear alignment with fibrillar pattern is identified by scanning over the popliteal groove, where it is seen passing superficially to the popliteus muscle and then following it distally to the fibular apex.
Biceps Femoris
Identified by its insertion at anterolateral collateral ligament.
Lateral Head of Gastrocnemius (Fig. 8.35)
Function is plantar flexion, but lateral head also acts as dynamic posterolateral stabilizer. It lies posterior to fibular condyle.
Ultrasonography: It is identified by its insertion immediately posterior to lateral collateral ligament and enclose fabella when present. The tendon can then be traced inferiorly to hypoechoic muscle belly.
Sometimes fabellofibular ligament is also identified.
On USG it appears as small rounded hyperechoic structure with posterior acoustic shadowing in gastrocnemius tendon.238
Linear hypoechoic fabellofibular ligament is identified passing to lateral fibular apex.
Arcuate Ligament (Fig. 8.35)
Not a true ligament. It is formed by popliteus tendon, it has Y shaped medial and lateral limbs sharing an origin on fibular apex and acts as a static stabilizer. Proximally it joins oblique popliteal ligament and ultimately with femur.
First metatarsal flares slightly at its base and meet first cuneiform. First cuneiform projects distally 1/2 inch further than other. It articulates with base of 1st metatarsal forming simple plane joint. Proximally is navicular tubercle. Proximally head of talus is felt by inverting and everting forefoot, bisecting a line drawn from medial malleolus to navicular tubercle.
Talar head: Medial malleolus articulates the medial side of talus.
Thumb on most anterior portion of lateral malleolus, keeping foot in plantiflexion, causes palpable talar dome.
Sustentaculum tali is small and finger breadth from distal end of medial malleolus.
When patient foot is stabilized just anterior to lateral malleolus, there is a depression called sustentaculum tali filled with exterior digitorum brevis.
Medial tubercle lies on plantar aspect of calcaneus is broad and long and give attachment medially to abductor hallucis muscle, flexor digitorum brevis and plantar aponeurosis.
It is palpated along medial longitudinal arch towards base of first metatarsal to metatarsophalangeal joint.
If press firmly over first metatarsal—2 sesamoids can be palpated at base. They provide mechanical advantage of flexor hallucis brevis.
Plantar position of talar head articulates with sustentaculum tali and anterior portion with posterior aspect of navicular.
Abductor digiti minimi tendon is at lateral aspect of sole, is superficial and palpable. Along medial aspect of sole, abductor hallucis muscle is visible as a prominence at concave surface. Capsule of ankle is attached anteriorly distal to cartilage, along talar neck and posterosuperior capsule, attached to posterior tibiofibular ligament. Lateral calcaneal surface is vertical and flat. A small crest, peroneal trochlea, from which inferior peroneal retinaculum extends, under which lies inframalleolar part of peroneal tendons.
Talus has a prominent body, anterior neck and head. Convex articular surface on superior surface of body—trochlea. Behind trochlea is posterior process, grooved in midline for FHL tendon. Metatarsal heads are joined by transverse ligaments.
Anterior recess is studied in a longitudinal or sagittal plane. Joint capsule inserts onto neck of the talus. It is seen as a thin hyperechoic band. Articular cartilage is identified as a smooth hypoechoic covering, 2–4 mm in thickness. 241Cortical bone lies deep to cartilage and on ultrasound appears as a smooth hyperechoic continuous line.
Synovial membrane is attached to articular margins of joint and lies deep to medial, lateral, and posterior ligaments.
Tendons may contain an ossicle or sesamoid, should not be confused as an avulsed bone fragment.
Posteromedial ankle: Patient lies supine with leg in a “frog-leg” position, hip abducted, knee flexed to 45°, and foot resting on its lateral margin.
SOLE
Sole has thick subcutaneous tissue with fibrous bands anchoring it to plantar aponeurosis—dense bands arranged largely along long axis of foot. Its proximal origin is medial process of calcaneus, after which it fans out dividing into five bands, one to each toe, attaching to superficial transverse metatarsal ligament.
Muscles along the sole of foot are divided into four layers deep to plantar aponeurosis.
First layer is composed of three muscles. Most central is flexor digitorum brevis, which gives off four tendons to second through fifth toes, dividing and inserting into sides of middle phalanx of each digit. Most medial muscle is abductor hallucis. Abductor digiti minimi runs along lateral aspect of the sole.
Second layer—long flexor tendons include flexor hallucis longus and flexor digitorum longus. Lumbricals originate from tendons of the FDL. They run distally along medial aspect of four lateral toes inserting into extensor expansions at the base of the metatarsophalangeal joint.
Third layer has three muscles. First two affect great toe and third affects fifth toe. Flexor hallucis brevis is adjacent to undersurface of first metatarsal. It has multiple origins and divides and inserts into medial and lateral aspects of base of first proximal phalanx. Adductor hallucis originates from two heads. Oblique head runs superficial to peroneus longus and transverse head joins oblique head to insert into lateral aspect of base of proximal phalanx of great toe. Flexor digiti minimi brevis arises from base of fifth metatarsal and inserts into base of fifth proximal phalanx adjacent to plantar surface of fifth metatarsal bone.
Fourth layer—interosseous within intermetatarsal spaces.
Ankle is stabilized medially by deltoid ligament, triangular, with base originates proximal to medial malleolus. It has superficial component divided into three parts: Anterior tibionavicular, intermediate tibiocalcaneal, and posterior tibiotalar ligaments. From anterior to posterior it contains anterior tibiotalar, tibionavicular, calcaneonavicular, tibiocalcaneal, and posterior tibiotalar.
Patient is positioned with plantar flexion of foot for evaluation of anterior components and dorsiflexion for posterior components.
Move probe in same plane medially and laterally to see muscle bellies of abductor hallucis and abductor digiti minimi.
Deep to abductor digiti minimi muscle, peroneus longus tendon seen superficial to hyperechoic cortex of cuboid bone. Deep to this is hypoechoic muscle of flexor accessories/quadratus plantae in second layer.242
Flow Chart 8.9: USG protocol for extensors of ankle (Fig. 8.109)
Probe kept in line with long axis of first metatarsal, hyperechogenic cortex seen smooth and continuous. Joint space is metatarsophalangeal joint, followed by interphalangeal joint. Joint spaces are similar, with smooth cortical rounded surface covered by a thin hypoechoic rim of articular cartilage.
Most commonly used approach is anterior.
Indications: For those patients who has severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Used to buy time before surgery for joint arthritis and for ill patients medically unfit for surgery. Usually given under image intensifier or USG guidance.
Technique
Position: Supine and foot in moderate plantar flexion, tibia and fibula are identified and below tibiofibular joint just above talus.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 80 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is directed superolaterally from anteromedial puncture point. Needle should go posterior to tibialis anterior tendon and anterior border of medial malleolus or needle is inserted between talus and tibia bounded medially between tibialis anterior and laterally extensor hallucis longus which are identified by applying resistance to dorsiflexion, needle directed tangentially. Another way is approach between extensor digitorum longus and peroneus tertius. Important is to avoid dorsalis pedis artery.
Alternatively C arm can be used for providing injections. Approach, position of patient and entry point of needle remains same as above.
USG Guided Ankle Joint Injections
The USG of ankle joint shows tendon of peroneus longus and brevis laterally, and tibialis posterior medially. Flexor halucis longus and flexor digitorum longus can be identified posterior to medial malleolus.
Anteriorly all extensors can be seen and extensor retinacula over distal tibia can also be seen.
Dynamic examination during flexion and extension maneuver of ankle and foot identifies the tendons.
Entry point of needle and position of patient remains same. Transducer is kept along the joint line of ankle joint.
Causes are arthritis or infection but in majority post-fracture talus or calcaneus. Pain present on walking in hind part of foot and relieved on rest. Tenderness is present on deep fingertip pressure over sinus tarsi at lateral malleolus. Patient holds foot in eversion due to spasm of peroneus.
Most commonly used is lateral approach.
Indications: For those patients who has severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Used to buy time before surgery for joint arthritis and for ill patients medically unfit for surgery. Usually given under image intensifier or USG guidance. Always rule out tuberculosis/Charcot/septic ankle affection.251
Technique
Position: Prone.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 80 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Point of entry is 1 inch above and 1 cm lateral to tip of lateral malleolus.
Another approach is anteromedial.
Position: Supine and leg slightly in abducted position identify medial malleolus and sustentaculum tali, subtalar joint lies above and posterior to sustentaculum tali. Needle is advanced into this region superiorly and anteriorly.
Image intensifier is used to accurately find the joint space. Ultrasound can be used to avoid injecting steroid into tendon or in blood vessels.
Midtarsal Joint (Fig. 8.57)
In this joint, pain arising from it is localized to dorsum of foot more on inversion and adduction.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Used to buy time before surgery. Always rule out tuberculosis/Charcot/septic ankle affection. Patients medically unfit for surgery. Usually given under image intensifier guidance.
Technique
Position: Supine with foot in neutral position, point of entry is space between navicular and cuneiform bones.253
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle. Talonavicular joint palpated while tracing from first metatarsal proximally.
Local area of tenderness is identified simultaneously avoiding anterior tibial artery.
Image intensifier is used to accurately find the joint space. Approach, position of patient and entry point of needle remains same as above.
Posterior heel pain from exercise injuries/overload injuries. Usually occurs 3–6 cm above tendon insertion is usually less vascular. Cause of pain is loading of fatigued muscle tendon unit from overtraining, while climbing, poor shoes, walking on uneven surface, over pronation. Functional overpronation causes whipping action on tendocalcaneus.
With sedentary people incidence is 5.9 % and 50 % with athletes, at mid portion of tendon injury is more common. Pain present on increased eversion.
From its insertion to its junction with gastrocnemius, it is surrounded with thin peritenon. Its medial portion is 5–6 mm thick and 8–10 mm wide. The bursa of tendoachilles is adjacent to tendoachilles. Overlying skin is keratotic reddened and fissured. Bursal swelling may be midline. Swelling impinges the edge of shoe.
Achilles peritenon is highly vascularized while its Achilles fibers have very poor vascularization. Insertional tendinopathy is seen in association with inflammatory arthritis or ill-fitting footwear or retrocalcaneal bursitis/Haglund's deformity.
Differential diagnosis is plantar rupture, history is acute and torn tendon ends are seen at either margins of edema. As tendinopathy develops tendons become swollen. Dynamic study is important.
Fig. 8.56: Schematic representation of Achilles tendon and flexor halluis longus (FHL) tendon on ultrasonography
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance.
Technique
Position: Prone and ankle over pillow and dorsiflex foot.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 to 60 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Approach laterally. Just above calcaneus. Needle is directed medially and downwards toward bursa. Identify the narrowest portion above 5 cm above insertion of tendoachilles. Assistant holds foot in dorsiflexion. Tendon is stretched and provide stiff surface along which the needle is inserted. It can also be approached from posterior aspect of leg distal, most part by directly palpating tendoachilles.
A 2 ml syringe filled steroid and fitted 5 cm long needle should be inserted away from lesion. It is then pushed parallel to tendon till it reaches the lesion. Steroid should not be injected into the tendon substance.
Ultrasound guided injection is useful.
Favorable outcome is seen for USG guided intra-articular injection of hyperosmolar dextrose for chronic insertional tendinitis and mid portion Achilles tendinosis.
The USG shows intratendinous tearing, change in echotexture neovessel infiltration, intratendinous calcification and irregularities of bony cortex.
Also useful for plantar fasciitis.
Grading for hypoechoic area 1. Irregular collagen fibers and mild hypoechogenicity 2. Large hypoechoic and anechoic region in insertional tendinitis. 257There is marked hypoechogenic and anechoic region, intratendinous calcification and irregularity of cortical bone of calcaneus and inflammation of periostium is seen. Patient given refrain from heavy activity for 1 week. Response is decrease of size of hypoechoic area with neovascularization in midsubstance tears whereas in insertion group, it remains as it is.
Dextrose can be used for sacroiliac joint injections, knee instability, osteoarthritis anterior talofibular sprain-increase fibroblast production of extracellular matrix. It causes cellular dysfunction and loss of integrity increases osmotic pressure.
It is not shown to be better than dry needling in humans, but in animals shown better than normal saline.
Increase fibroblast repair, type I collagen and growth factors give increase echogenicity with normal fibrillar pattern as time passes vascularity increases in tendinosis leads to neovascularization. Correlation of efficacy with number of injection and patient willingness for future return for injection is more.
Alfred and Ohberg used polidocanol into peritendon found to be successful at follow-up of 1 year.
Repeated twisting and untwisting increases stress, anisotropy occurs where fibers of tendon curve at calcaneal insertion.
Paratenon changes and tendinopathy are most common on medial aspect of tendon. Degree of separation during dorsiflexion and approximation on plantiflexion is measured. Ankle tendons due to their curved course are more easy to visualize on short axis, malleoli are starting landmarks for peroneal and posteromedial tendons.
Tendon does not move linearly and all three components rotate medially so that soleus component moves from deep to medial aspect.
Probe is placed in sagittal plane of posterior ankle on to palpable Achilles tendon.
Deep to Achilles tendon Kager fat pad, appears as hypoechoic structure deep to tendon and adjacent to tibia a part of flexor hallucis longus muscle seen. Peritenon appears thick and hyperechoic. Inflammatory changes extend to deep retrocalcaneal bursa. Kager's fatty pad becomes hyperechoic. In absence of artifacts Achilles tendon is echogenic and exhibits characteristic fibrillar texture.
Anteriorly lies hypoechoic flexor hallucis longus and echogenic posterior surface of tibia. Hypoechoic subtendinous flattened calcaneal bursa is seen at angle formed by tendon and calcaneum.
Tendon fibers at bony insertion show hypoechogenicity due to short oblique course. Caution: repeated injections into the tendon (intrasubstance) are known to cause tendon rupture.
Flexor Hallucis Longus (Figs 8.110 to 8.113)
From midline position probe is slightly displaced medially from Achilles tendon on to flexor hallucis longus tendon remaining in strictly sagittal plane on USG. 258It is seen posterior to talus. Tibiotalar joint effusion is also extend in synovial sheath of flexor hallucis longus.
Caused by rheumatoid arthritis, poor fitting footwear, flat feet presents with pain, swelling, great toe valgus decreased range of motion of great toe and hammer 2nd toe. X-ray is helpful. Most commonly seen in gout (Figs 8.99 to 8.108).
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Useful in those medically unfit for surgery. Usually given under USG guidance. Also investigate for gout.
Technique
Position: Supine with foot in neutral position and knee in flexion.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Insert needle at right angles in joint space next to extensor tendons with help of distracting the affected toe and flexing it. Most commonly seen in gout.260
The C arm can be used for providing injections. Approach, position of patient and entry point of needle remains same as above. Sometimes interphalangeal joint needs to be injected for arthritis pain (Figs 8.58 and 8.98).
It is prominence on lateral side of 5th metatarsal head. It is position in which tailors would sit on floor with their legs crossed forcing the lateral border of foot against floor. Often seen in splayfoot and hallux valgus.
Shaft of metatarsal is angulated making, head is more prominent.
Main source of discomfort is constricting shoes (ulceration may ensue). Keratosis may develop in diabetes, advanced Charcot Marie tooth disease of spinal dysraphism may lead to loss of entire 5th ray.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier guidance.
Technique
Position: Supine and foot is abduction.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted directly against 5th metatarsal head till it reaches bone point of entry is laterally.
Inflammation to plantar fascia, more commonly seen in women, can occur in rheumatoid arthritis, Reiter's syndrome or gout. Bare foot walking or high impact exercises predispose to this condition. It is most common cause of heel pain.
Most common in middle aged women, runners, younger male.
Imaging is useful in follow-up. Morning pain is present that decrease with activity. Nodules are palpable over proximal medial border of plantar fascia.262
Pain is present on dorsiflexion and toe extension, with weak foot intrinsic and tight gastrocnemius.
Also seen in 40 to 50 years active males with unilateral symptoms.
Patients usually have obesity, pes planus/cavus.
Patient is comfortable during day toward end of day discomforts with aching which decreases in absence of weight bearing.
Heel fat pad, cushions heel strikes and allow skin to resist forces.
Thickness of fat pad decreases after age of 40 years with loss of shock absorption. Mild thick heel fat pad in symptomatic patients might also be due to local inflammatory process affecting this area. Plantar fascia is most important component of dynamic arch support.
Tenderness is present at inferomedial aspect of calcaneal tuberosity.
Calcaneal spur is seen in 50% patients. Repetitive stress on plantar fascia cause microscopic tear at origin of plantar fascia and flexor digitorum longus immediately deep to it. Lateral plantar nerve branch may be compressed by flexor digitorum brevis and heel spur and adjacent quadratus plantae. As dorsiflexion occurs the arch of foot also gets elevated causing stress over calcaneal tuberosity —stress fracture of anterior lip of tubercle and attempt to heal—spur formation in flexor digitorum brevis.
Bone scan in many cases show equivocal diagnosis.
Electromyography is done if patient is symptomatic for several weeks and nerve entrapment is suspected.
Calcaneal spur is common at site of insertion of plantar fascia on calcaneal tuberosity. It is seen in those with abnormal gait.
Anatomical landmarks are:
- Proximal base of longitudinal arch at medial side
- Distal to medial process of tuberosity of calcaneus.
Plantar fasciitis can be treated with shoe inserts and NSAIDs and local steroids. Local steroids are responded by majority. Follow-up of 24 months showing 50% good to excellent results and 50% had average to poor scores and in orthosis group 85% of patient had pain in 6 months > 90% were symptom free by 9 months.
Sometimes there is rupture of plantar fascia after corticosteroid injection and calcaneal pitch angle decreases.264
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance.
Technique
Position: Prone knee flexed to 90 degree.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
One hand of surgeon encircles the heel pressing hard on lesion with index finger.
Needle can be inserted both from medial and plantar aspect of heel.
Needle is advanced till it hits bone then withdrawn. Assistant dorsiflexion foot so as to render plantar fascia taut and easy to identify when needle touches it.
Plantar skin overlying tendon is thick so oblique approach through skin is necessary.
A 2 ml syringe is fitted with 5 cm needle. Spot is chosen along medial side of foot 3–4 cm on to most painful site. Needle is thrust in pointing downwards from horizontal and advanced until it traverses resistant fascie and touches bone. Affected area is infiltrated with minor withdrawal and reinsertions.
On USG, it gives appearance of tendons—homogenous echogenic band with internal linear interfaces on longitudinal section. Mechanical stress and inflammation results in tendon thickening with hypoechoic areas within plantar fascia peritenon fluid collection.
Position: Prone with toe hanging freely lover end of couch and ankles dorsiflexed to 90 degrees.
Sagittal imaging of plantar fascia is performed and thickness > 4 mm is considered abnormal.
Probe is placed inferiorly in sagittal plane at dorsal aspect of foot. Slight medial displacement gives best visualization. On USG it appears as band like fibrillar structure attaching to inferior aspect of calcaneus. Normal thickness is 2–4 mm in asymptomatic.
Thickening of plantar fascia, reduced echogenicity loss of edge sharpness.
Changes at insertion site termed as enthesopathy, changes extend too many centimeters through central part or body of plantar fascia.
Rupture is defined by loss of internal longitudinal fibrillar pattern with thickening or blurring of edges.
Plantar fascia is similar to Achilles tendon and patellar tendon, it has paratenon. Fluid distension of paratenon is associated with perifascial edema. Change in echogenicity and loss of edge sharpness, localized tenderness without swelling can be present over anteromedial portion of plantar surface of calcaneus. USG rules out conditions like subcalcaneal bursitis, calcaneal stress fracture, tarsal tunnel syndrome and calcaneal osteomyelitis.265
Repeated friction over posterior aspect of heel (associated with retrocalcaneal spur) outgrowth from posterior tuberosity of calcaneus. Men are more affected than females. It lies between tendoachilles insertion and skin. Pain is diffuse present over medial and lateral aspect of calcaneus. Pain is increased on dorsiflexing the foot
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under USG guidance.
Technique
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Around Achilles tendon the subcalcaneal deep and superficial subcutaneous bursae can be located. Below Achilles tendon lies fat called Kager's fatty triangle.
Caution: Do not inject into substance of Achilles tendon. Approach from lateral side to most prominent/painful point.
Seen more commonly in middle aged or older population, associated with degenerative rupture or a sesamoid bone causing pain high arch foot.
Caused due to injuries due to eversion and improper stretching of peroneal muscle. Pain is more on eversion at posterior ankle. In inversion sprain there is swelling and ecchymosis below lateral malleolus.
Fig. 8.74: Position of transducer for lateral structures of ankle for ligaments of ankle on lateral side and peroneus longus and peroneus brevis
Peroneal retinaculum is avulsed. Subluxation of tendons is seen on forceful dorsiflexion of inverted foot.
Peroneus longus and brevis are evertors of foot and stabilizers of ankle as well as pronator and abductors of foot, they help in plantiflexion. They occupy lateral compartment of leg and become tendons before reaching ankle joint.
Peroneus brevis descends anteromedially to peroneus longus. Both pass through common tendon sheath 4 cm proximal to lateral malleolus and pass through fibro-osseous tunnel. That is stabilized posterolaterally by superior 269peroneal retinacula; medially by posterior inferior tibiofibular ligament and anteriorly fibular groove.
Major stabilizing structure is superior peroneal retinacula which converts fibular groove into fibro-osseous tunnel. Peroneus brevis assumes relatively anterior position compared to longus as tendon pass distal relative to superior peroneal retinacula. They are again enveloped by individual tendon sheath.
Subluxation usually involves one or both tendons moving anteriorly over lateral malleolus snapping may be palpated (retrofibular intrasheath subluxation).
Post-traumatic or chronic subluxation in flat or convex fibular groove occurs in athletic injury like skating, skying soccer, misdiagnosed as sprain. It has retromalleolar swelling and pain over posterior lip of fibula.
Peroneal retinacula is tired after subluxation. Chronic recurrent peroneal subluxation and lateral ankle pain with recurrent subluxation. These occur when foot is dorsiflexed and everted. This causes longitudinal tear of peroneus brevis, peroneus longus is protected by it from mechanical attrition which in turn causes peroneal splits syndromes and secondarily hypertrophy of peroneus longus.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance. Injection is given as last resort before surgery in form of tendon sheath release.
Technique
Position: Prone.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Evert foot and trace peroneal tendon anteriorly. Needle is inserted at an angle of 30 degree to ankle directed towards lateral malleolus into combined tendon sheath.
Ultrasonography guided injections are helpful. Position of patient and approach is same as above. Patient is made to evert the foot to identify the tendons. Probe is positioned parallel and perpendicular to malleolar calcaneal axis or, is kept transversely posterior to lateral malleolus.
Probe is placed slightly superior to distal aspect of lateral malleolus. Peroneus brevis is adjacent to bone and peroneus longus is located superficially.
Tendon causes plantar flexion and inversion and important supporter of medial longitudinal arch of foot.
Caused due to acute eversion injury. Pain is localized to inner side of ankle. History of rubbing skin of ankle to shoe.
Accessory navicular cause repeated stress on tendon causing tenosynovitis. Pain, localized over tendon on medial side of ankle. Heel valgus abduction of mid foot and pronation of foot are noted.
Collapse of arch can occur in long standing cased causing pain on lateral aspect of ankle due to pressure on sinus tarsi by lateral process of talus. Similarly tibialis anterior tendon also show attritional or tenosynovitis changes. Site of inflammation is beneath inferior extensor retinacula in the latter and there is weakness in dorsiflexion.
It needs to be differentiated from sesamoid in tibialis posterior—there is pain on resistive inversion and plantar flexion. Prominence of navicular tuberosity is seen due to fusion of navicular with accessory one.
Tibialis posterior is larger than other tendons, tendinopathy progress to longitudinal splits at malleolus and immediately proximal to its insertion at navicular. Distal insertion is difficult to visualize due to tendon fanning out broad.
Flexor hallucis tendinopathy is seen in kick up athletes and ballet dancers.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under USG guidance. Injection is given as last resort before surgery in form of tendon sheath release.
Technique
Position: Supine and foot is abduction.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted 1 cm distally in direction of medial malleolus, till it reaches medial malleolus. Needle is withdrawn and contents of syringe are injected.273
Dynamically—decrease in movement of tendon on USG. Peroneus brevis, traced from lateral malleolus to 5th metatarsal. Before longitudinal splitting there is cross-sectional enlargement of tendon.
USG Guided Injection
Position of patient, approach and entry point of needle remains same as above.
Adequate gel is applied at malleolus so that tendons are not pushed hard. Patient is asked to evert foot against examiner. Transducer is kept with one end over medial malleolus and other end over the posterior aspect of medial malleolus transversely.
Probe is placed slightly superior to medial malleolus. Structures seen serially are tibialis posterior, flexor digitorum, artery and vein, posterior tibial nerve and flexor hallucis tendon. Tibialis posterior is seen as slightly larger than others in small groove on tibia. It serves as reference point. Vascular structures be identified as hypoechoic rounded structures Doppler USG help in localization. Nerve located adjacent to vessels is hyperechoic. It is superficial to flexor hallucis longus (visualized by flexing and extending the great toe).
Most commonly seen in runners due to sudden pronation of ankle. Pain is felt below medial malleolus.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance. Used in irreparable tears in patients unfit for surgery.
Fig. 8.84: Schematic representation of tibiotalar ligament and flexor halluis longus tendon on ultrasonography
Technique
Position: Supine and foot in neutral position foot is adducted.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Advance needle through 1 cm below this medial malleolus and directed towards medial malleolus.
Posterior Deltoid Ligament
Probe is placed in coronal plane posteriorly at medial aspect of palpable tibia. A short deep and long superficial tibiotalar portion of deltoid ligament seen.
Superficial band is thinner.
At USG both bands are perpendicular to probe and appear as relatively hypoechoic structure in normal ankle.
Anterior Deltoid Ligament
Probe is placed at medial ankle more anteriorly than previous site the longer tibiocalcaneal portion of deltoid ligament is seen. Medial tendons are located more superficially and consist of tibialis posterior, flexor digitorum and flexor hallucis longus.
The USG long tibiocalcaneal part of deltoid ligament is seen, but it may not be possible to visualize this.
CHRONIC ANTERIOR TALOFIBULAR LIGAMENT INJURY (FIG. 8.85)
It is also seen in miners due to sudden inversion. Pain is felt below lateral malleolus.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance. Used in irreparable tears in patients unfit for surgery.
Technique
Position: Supine and foot in neutral position foot is abducted.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is advanced through 1 cm below lateral malleolus and directed towards lateral malleolus. As needle reaches the ligament moderate resistance is felt. If bony resistance is felt withdraw the needle slightly. Entire area is infiltrated.
Probe placed in sagittal plane at anterior aspect of ankle. Joint space is located superiorly to palpable lateral malleolus. Fat pad is present in anterior tibiofibular joint and identified at ultrasonography.
The fat pad is located at tibiotalar joint.
Joint capsule is attached distally over talar neck.
On USG fat pad is seen a slightly hyperechoic triangular area anterior to tibiotalar joint line.
Fig. 8.88: Schematic representation of deltoid ligament on ultrasonographyAbbreviations: FHL = Flexor halluis longus, FDL = Flexor digitorum longus, TP = Tibialis posterior
Fig. 8.89: Schematic representation of posteromedial structures of ankleAbbreviations: FHL = Flexor halluis longus, FDL = Flexor digitorum longus, TP = Tibialis posterior
Cartilage over the talus is identified as hypoechoic appearance. In tibiotalar effusion joint, fluid is depicted in anterior joint recess and may displace the anterior fat pad. Cartilage interface sign is seen.
Anterior Talofibular Ligament
Probe at transverse plane at lateral ankle lateral malleolus is clinically palpable and probe is placed at distal aspect of lateral malleolus in longitudinal axis of foot. Small amount of joint fluid can be seen in normal ankle.277
Fig. 8.91: Schematic representation of posteromedial structures of ankleAbbreviations: TP = Tibialis posterior, FDL = Flexor digitorum longus, FHL = Flexor halluis longus
Due to sudden inversion. Pain felt over anterior and distal to lateral malleolus which increases on inversion. Ecchymosis usually present.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance. Used in irreparable tears in patients unfit for surgery.
Technique
Posterior: Prone
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted 1½ inch below tip of lateral malleolus towards lateral malleolus.
Calcaneofibular ligament
Probe is placed at oblique coronal plane. Ligament is seen from fibula to calcaneus. The peroneal tendons are in close proximity to the ligament.
TARSAL TUNNEL SYNDROME (FIG. 8.115B)
It is compression neuropathy of posterior tibial nerve. It may be because of injury, thrombophlebitis of posterior tibial artery.
It is made of neurovascular bundle, posterior tibial and flexor digitorum longus and flexor hallucis longus tendon covered with flexor retinaculum from medial malleolus of tibia to calcaneum. Components are separated within the tunnel by septum.
It is caused by trauma, fracture calcaneum or ankle fracture. Foot deformities, vericose veins, ganglia, or talocalcaneal coalition. Externally by tight footwear, tight plastercast, ganglia or tendon sheath cyst. It may be secondary to excessive pronation.
Patient will present with pain, numbness, paresthesia of sole of foot that radiates towards medial ankle. Tenderness is present behind medial malleolus. Inversion produces pain, positive tinel sign and intrinsic muscle weakness present. Pain is burning like night pain and swelling. Pain increase on walking, passive dorsiflexion or eversion. Tendon reflex and range of motion are not affected. EMG is helpful. It is necessary to rule out diabetic neuropathy and neuroma.
In subtalar portion of foot sinus tarsi is located, medial calcaneonavicular and lateral bundles of bifurcated ligament or Y ligament lies close to sinus. The tarsal tunnel is crossed by neurovascular bundles and flexor tendon. Tarsal tunnel can appear severely narrowed as result of sheath thickening in tenosynovitis.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance. Injection is given as last resort before surgery in form of neurolysis. Usually effective when there is compression from adjacent structures/tenosynovitis from adjacent tendons. Not much effective when adhesions have already occurs.
Technique
Position: Lateral decubitus leg flexed. Affected leg is in dependent position.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted towards posterior superior border of medial malleolus towards posterior tibial artery and advance needle towards posterior groove of medial malleolus direct it towards posterior tibial nerve. Direct needle cephalad till paresthasia in distribution of tibial nerve is obtained and after that withdraw it by 1 cm till paresthesia disappear.
Keck was first to use USG guidance for injection. Probe is positioned parallel and perpendicular to malleolar calcaneal axis. Small ganglia not accessible clinically can be visualized by USG and its aspiration can also be performed if nerve is located at bone side of tendon.280
MALLET TOE PAIN SYNDROME
Most commonly in females may develop to bursa/callus/ulcer. It presents as painful flexion deformity of distal interphalangeal joint.
Patient will present with constant dull aching pain of affected toe which increases with walking and characteristic flexion deformity.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted into affected distal phalanx till it hits bone and injected.
Similarly as in hammer toe pain syndrome.
Most commonly due to wearing of tight shoes and high heels. Bilaterally seen more commonly in female. It involves flexion deformity of proximal interphalangeal joint with pain, typical hammer toe develops.
Position: Supine.
Needle is advanced slowly to proximal phalanx head and injected. Point of entry is lateral to the affected phalanx.
MORTON'S NEUROMA (FIG. 8.96)
Most commonly involve 3rd and 4th toes; females are mostly affected. In 1876, Thomas G Morton described that neuroma resulted due to pinching of lateral plantar nerve to fourth web space between heads of third and fourth metatarsals, instability of adjacent joints, falling of transverse arch can also cause this condition.
Commonly found is perineural fibrosis demyelination or degeneration of nerve fascicles endoneural edema with no inflammatory changes with or without presence of bursa along with thickened walls of nerve.
It is usually secondary to high heel shoes, excessive pronation, high arch, lateral compression of forefoot. There is usually intrinsic weakness. It is important to rule out stress fracture and EMG is not of much help.
Patients will complaint of pain in plantar surface of foot with paresthesia. Patients give history of wearing improperly fitting shoes with antalgic gait.
Pain at metatarsal head, cramp like burning pain increased on walking and after wearing shoes. It can also disturb sleep.
Useful tests: Cardinal test—locally compressing the web space and Mulder click—compressing the metatarsal heads manually with no objective numbness, it is essential to rule out rheumatoid arthritis.
In Morton's neuroma medial and lateral manual compression of foot cause the neuroma to displace in plantar direction and produce symptoms—Mulder sign.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance. Injection is given as last resort before surgery.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Interdigital space is used for point of entry which is proximal to metatarsal head at site of maximal tenderness. Needle is directed towards heel from dorsal to plantar surface injecting drug (Fig. 8.114).
Condition caused due to repetitive trauma from dancing and running and playing football.
More common at 1st metatarsal head. Differential diagnosis: Turf toes and bipartite sesamoid. There is pain with passive dorsiflexion of metatarsophalangeal joint, impairment of push off, antalgic gait, swollen 1st metatarsal joint.
Patient will have sensation of pain while walking and tender area moves with active flexion of toes.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance.
Technique
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Needle is inserted directly into bone from plantar surface at the site of maximal tenderness.
METATARSALGIA (FIG. 8.115A)
Patients presents with tenderness over metatarsal head which remains on same site on moving toes. Pain increases on walking for long time and wearing tight footwear usually there is flattering of arch of foot.
Indications: For those patients who have severe pain and restriction of range of motion and those during rehabilitation periods. These injections have been used after other conservative methods are tried. Usually given under image intensifier or USG guidance.
Position: Supine.
Preparation: Part is painted with antiseptic solution and draped.
Drugs: 2% preservative free lignocaine and 40 mg of methylprednisolone.
Syringe: 2 ml/1½ inch 25 gauge needle.
Affected metatarsal head is marked and needle is inserted on dorsal surface of the tenderest site and the mixture is injected.
Figs 8.115 A and B: (A) Area of tenderness on sole in various conditions; (B) Area of tenderness on medial ankle in various conditions
FUTHER READING
- Aisen A M, McCune W J, MacGuire A, et al. Sonographic evaluation of the cartilage of the knee. Radiology. 1984;153:781-4.
- Astrom M, Westlin M. Blood flow in chronic Achilles tendinopathy. Clin Orthop. 1994;308:166-72.
- Balen P, Helms C. Association of posterior tibial tendon injury with spring ligament injury, sinus tarsi abnormality and plantar fasciitis on MR imaging. AJR Am J Roentgenol. 2001;176:1137-43.
- Bellamy N, Campbell J, Robinson V, et al. Intra-articular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. Apr 19 2006;(2)?CD005328.
- Bianchi S, Zwass A, Abdelwahab IF, Banderali A. Diagnosis of tears of the quadriceps tendon of the knee: value of sonography. AJR Am J Roentgenol. 1994;162:1137-40.
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics. Vol I, 11th ed. Mosby Inc. 2008;895-905.
- Curl WW. Popliteal cysts: historical background and current knowledge. J Am Acad Orthop Surg. 1996;4:129-33.
- Davies SG, Baudouin J, King JB, et al. Ultrasound, computed tomography and magnetic resonance imaging in patellar tendonitis. Clin Radiol. 1991;43:52-6.
- De Flaviis L, Nessi R, Leonardi M, Ulivi M. Dynamic ultrasonography of capsulo-ligamentous knee joint traumas. J Clin Ultrasound. 1988;16:487-98.
- De Flaviis L. Ultrasonic diagnosis of Osgood-Schlatter and Sinding-Larsen- Johnson diseases of the knee. Skeletal Radiol. 1989;18:193-7.
- Erickson SJ, Cox IH, Hyde JS, et al. Effect of tendon orientation on MR imaging signal intensity: a manifestation of the “magic angle” phenomenon. Radiology. 1991;181:389.
- Gagnerie F, Taillan B, Bruneton JN, et al. Three cases of pigmented villonodular synovitis of the knee. Ultrasound and computed tomographic findings. ROFO 1986;145.
- Holmes GB, Mann RA. Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle. 1992;13(2):70-9.
- Hughston JC, Baker CL, Mello W Popliteal cyst: a surgical approach. Orthopedics. 1991;14:147.
- Jacobson JA. Musculoskeletal sonography and MRI: a role for both imaging methods. Radiol Clin North Am. 1999;37:713-35.
- Jaysmith MD, et al. Accuracy of USG guided intraarticular injection in native adult: the posterior tibial tendon. Foot Ankle. 1992;13:70-9.
- Jennifer Black B et al. Intertester reliability of USG in patellar layered configuration and its importance in cases of tendon rupture. AJR Am J Roentgenol. 1992;159:1031-4.
- John Ebnezar. Step by Step Injection Techniques in Orthopaedics. Jaypee Brothers Medical Publishers. Edition 1. 2007;201-90.
- John O Neill. Musculoskeletal Ultrasound Anatomy and Technique. Springer Inc. 2008;20-330.
- Kainberger FM, Engel A, Barton P, et al. Injury to the Achilles tendon: diagnosis with sonography. AJR Am J Roentgenol. 1990;155:1031-6.
- Kaneko K, DeMouy EH, Brunet ME, Benzian J. Radiographic diagnosis of quadriceps tendon rupture: analysis of diagnostic failure. J Emerg Med. 1994;12:2,25-229.
- Kleinman M, Gross AE. Achilles tendon rupture following steroid injection:Report of three cases. J Bone Joint Surg (Am). 1983651345-1347. Canadian Family Physician. November 2006.
- Laine H R, Harjula A, Peltokallio P. Ultrasound in the evaluation of the knee and patellar regions. J Ultrasopnd Med. 1987;6:33-6.
- Lazarus ML, Ray Jr CE, Maniquis CG. MRI findings of concurrent acute DVT and dissecting popliteal cyst. Magn Reson Imaging. 1994;12:155.
- Lockman LE. Knee joint injections and aspirations: The triangle technique. Canadian Family Physician. Nov 2006;52(11):1403-4.
- Lucas PE, Hurwitz SR, Kaplan PA, et al. Fluoroscopically guided injections into the foot and ankle: localization of the source of pain as a guide to treatment-prospective study. Radiology. Aug 1997;204(2):411-5.
- Maschironagaoka MD, et al. USG of tarsal tunnel. J Ultra Med. 2005;24:1035-40.
- Movin T, Kristoffersen-Wiberg M, Rolf C, et al. MR imaging in chronic Achilles tendon disorder. Acta Radiol. 1998;39:126.
- Nance EP, Kaye JJ. Injuries of the quadriceps mechanism. Radiology. 1982;142:301-7.
- Newman JS, Adler RS, Bude RO, et al. Detection of soft tissue hyperemia: value of power Doppler sonography. AJR Am J Roentgenol. 1994;163:385-9.
- Peh WC, Chan JH. The magic angle phenomenon in tendons: effect of varying MR echo time. Br J Radiol. 1998;71:31.
- Ramsey RH, Muller GE. Quadriceps tendon rupture: a diagnostic trap. Clin Orthop. 1970;70:161-4.
- Richardson ML, Selby B, Montana MA, Mack LA. Ultrasonography of the knee. Radiol Clin North Am. 1988;26:63-75.
- Rumack C, Wilson S, William J. Diagnostic Ultrasound. Vol 1, 2nd edition. Mosby Inc. 1998;843-83.
- Schweitzer ME, Karasick D. MR imaging of disorders of the Achilles tendon. AJR Am J Roentgenol. 2000;175:613.
- Scuderi C. Ruptures of the quadriceps tendon. Am J Surg. 1958;95:626-35.
- Sell S, Schulz R, Balentsiefen M, et al. Lesions of the Achilles tendon: a sonographic, biochemical and histological study. Arch Orthop Trauma Surg. 1996;115:28-32.
- Shrier I, Matheson GO, Kohl HW 3rd. Achilles tendonitis: are corticosteroid injections useful or harmful? Clin J Sport Med. Oct 1996;6(4):245.
- Siwek CW, Rao JP. Ruptures or the extensor mechanism of the knee joint. J Bone Joint Surg (Am). 1981;63:932-7.
- Solbiati L, Rizzatto G. Ultrasound of Superficial Structures. 1st edition. Churchill Livingstone. 1995;279-375.
- Tallia AF, Cardone DA. Diagnostic and therapeutic injection of the ankle and foot. Am Fam Physician. Oct 1 2003;68(7):1356-62.
- Unverferth LJ, Olix ML. The effect of local steroid injection on tendon. J Sports Med. 1973;l(4):31-7.
- Van Holsbeeck M, Van Holsbeeck K, Gevers G, et al. Staging and follow-up of the arthritis of the knee. Comparison of sonography, thermography and clinical assessment. J Ultrasound Med. 1988;7:561-6.
- Wallen M, Gillies D. Intra-articular steroids and splints/rest for children with juvenile idiopathic arthritis and adults with rheumatoid arthritis. Cochrane Database Syst Rev. Jan 25 2006;(1):CD002824.
- Watson Buchaman W. Clinical Examination of Musculoskeletal System. Williams & Wilkins. 1st edition. 1997;25-82.
- Yu JS, Petersilge C, Sartoris DJ, Pathria MN, Resnick D. MR imaging of injuries of the extensor mechanism of the knee. Radiographics. 1994;14:541-51.
- Zanetti M, Metzdorf A, Kundert HP, et al. Achilles tendon: clinical relevance of neovascularization diagnosed with power Doppler US. Radiology. 2003;227:556-60.
- Zeiss J, Saddemi SR, Ebraheim NA. MR imaging of the quadriceps tendon: normal layered configuration and its importance in cases of tendon rupture. AJR Am J Roentgenol. 1992;159:1031-4.
294
297Index
Pathology | Entry point of needle for injections |
Sbudeltoid bursitis | 2–3 cm inferior and medial to posteriolateral corner of acromion with needle directed superiorly |
Acromioclavicular joint | Just over acromioclavicular joint |
Bicipital tendinitis | Most tender area over bicipital groove |
Shoulder joint | 2–3 cm inferior and medial to posteriolateral corner of acromion with needle directed straight into the joint |
Pathology | Entry point of needle for injections |
Lateral epicondylitis | 2 cm/most tender area over common extensor origin |
Medial epicondylitis | 1 cm/most tender area over common flexor origin |
Olecranon bursitis | Most prominent point over bursa |
Elbow joint arthritis | Posteriorly between capitelum and radial head |
Cubital tunnel syndrome | Proximal to sulcus between medial epicondyle and olecranon |
Pathology | Entry point of needle for injections |
Distal radioulnar joint | 5 cm proximal to ulna lower edge between radius and ulna |
Carpal tunnel syndrome | Between FCR and palmaris longus proximal to wrist crease needle directed distally |
1st carpometacarpal joint arthritis | At the joint line from radial side |
Metacarpophalangeal and interphalangeal joint arthritis | Dorsolateral side of joint at joint line |
Trigger finger | Into flexor tendon sheath just proximal to A1 pulley |
De quervian's tenosynovitis | Into tendon of abductor pollicis longus distal to radial styloid |
Ganglion | Most prominent portion of ganglion |
Guyons canal | Between palmaris longus and FCU just medial to flexor carpi ulnaris |
Pathology | Entry point of needle for injections |
Hip joint arthritis | 2 inch below and 1 cm lateral to midpoint of inguinal ligament /just lateral to femoral artery |
Trochanteric bursa | Most prominent point over bursa |
Adductor tendinitis | 1 inch lateral to pubic synthesis |
Meralgia paresthetica | 2 cm medial and 1 cm inferior to ASIS |
Ischial and gluteal bursa | Most prominent point over bursa |
Psoas and iliopectineal bursa | 2 inch below and 1 cm lateral to midpoint of inguinal ligament /just lateral to femoral artery |
Coccydynia | Natal cleft |
Snapping IT band | Over lateral condyle of femur |
Pathology | Entry point of needle for injections |
Knee joint | In lateral joint line |
Patellar tendinitis | Above the tibial tuberosity |
Tibiofibular joint | Medial aspect of fibula head |
Tibial and fibular collateral ligament | Over the respective medial most and lateral most aspect of joint line |
Medial gastrocnemius and semimembranous bursitis | Over the respective origin of gastrocnemius and insertion of semimembranosus |
Popliteal, suprapatellar infrapatellar, pes anserine bursa | Over most prominent aspect of bursa |
Ankle joint | Posterior to tibialis anterior tendon and anterior border of medial malleolus or between talus and tibia, medially between tibialis anterior and laterally extensor hallucis longus |
Subtalar joint | Above and posterior to sustentaculum tali |
Mid tarsal joint | Talonavicular joint palpated while tracing from 1st matatarsal proximally |
Achilles tendinitis | Posterior aspect of leg distal most part by directly palpating tendoachilles |
Hallux valgus | In joint space next to extensor tendons with help of distracting the affected toe and flexing it |
Bunionette | 5th metatarsal head till it reaches bone joint |
Plantar fasciitis | Needle inserted both from medial and plantar aspect of heel at most painful point |
Retrocalcaneal bursitis | Around Achilles tendon, subcalcaneal deep and superficial subcutaneous bursae located approach from lateral side to most prominent/painful point |
Peroneal tendinitis | Evert foot and trace peroneal tendon anteriorly. Needle is inserted at an angle of 30 degree to ankle directed towards lateral malleolus |
Tibialis posterior tendinitis | Needle is inserted 1 cm distally in direction of medial malleolus, till it reaches medial malleolus |
Deltoid ligament, calcaneal fibula ligament | 1 cm below this respective malleolus and directed towards same malleolus |
Tarsal tunnel syndrome | Needle is inserted towards posterosuperior border of medial malleolus towards posterior tibial artery |
Mallet toe pain syndrome | Needle is inserted into affected distal phalanx |
Morton's neuroma | Proximal to metatarsal head at site of maximal tenderness |
Sesamoiditis | Directly into bone from plantar surface at the site of maximal tenderness |
Metatarsalgia | Metatarsal head is marked and needle is inserted on dorsal surface of the most tender site |
Page numbers followed by f refer to figure
A
Abductor
digiti minimi
pollicis
brevis
longus , , ,
Achilles
tendinitis ,
tendon , , ,
Acromioclavicular
injection
joint , , ,
arthritis ,
ligaments
Acute and chronic bursitis
Adductor
hallucis
longus
pollicis
tendinitis ,
Adhesive capsulitis
Allergy
Anatomical snuff box ,
Anatomy of
spine
vascular supply of leg and ankle
Ankle
arthritis ,
joint ,
injections
Ankylosing spondylitis , ,
Anterior
deltoid ligament
knee structures
superior iliac spine ,
talofibular ligament
tibiotalar joint
Anteromedial structures of knee
Arcuate ligament
Arthritis ,
of facet joint
Autologous
blood injection for tennis
elbow ,
platelet rich plasma
Avascular necrosis
of cartilage
B
Bacteriologically sterile
Baker's cyst
Behcet's syndrome
Biceps
brachii
femoris
tendinitis
Bicipital
aponeurosis
tendinitis
tenosynovitis
Bilateral
knee arthritis
olecranon bursitis
Blind injection
Blood collection for injection platelet rich
plasma
Bones fracture
Bony landmarks of pelvis and hip
Brachioradialis
Bunionette ,
Bursae around knee
Bursitis
and ligament sprain
around calcaneus
C
Calcaneal
fibula ligament
spur , ,
Calcaneofibular ligament ,
Calcific tendinitis ,
Canal of Guyon 298
Capsulitis of joint
Cardiac arrhythmias
Carpal tunnel syndrome , ,
Carpet-Layer's knee
Caudal epidural steroids
Cerebrospinal fluid
Cervical
epidural steroid
spondylosis
Charcot's arthropathy ,
Cheiralgia paresthetica
Chondromalacia
Chronic
and refractory tennis elbow
anterior talofibular ligament injury
deltoid ligament injury
fatigue syndrome
fibulocalcaneal ligament injury
low back pain
Claw toe
Clergyman's knee
Coccydynia ,
Color Doppler
Common
extensor
group and lateral epicondyle
origin , ,
sites of lesions
Concave subdeltoid fat counter
Coracoacromial ligament
Costochondritis
Costosternal
joint
syndrome
Coxa saltans
Crystal induced
arthritis
arthropathy
Cubital
fossa ,
tunnel syndrome ,
Cystic tumor
D
De Quervain's tenosynovitis , ,
–,
Degenerative
lumbar spine
spondylolisthesis
Deltoid ligament ,
Discography
Disk height reduction
Diskitis
Dislocation of elbow
Distal
interphalangeal joint arthritis
radioulnar joint ,
Dorsal interosseous muscles
Draftsman's elbow
Dupuytren's contracture ,
E
Elbow
arthritis
joint
arthritis
aspiration
Eosinophilia
Epidural
abscess
hematoma
injection
needle ,
steroid
injections
Extensor
carpi radialis
brevis
longus , ,
carpi ulnaris
of ankle
pollicis
brevis ,
longus ,
F
Facet
arthropathy
joint
injection of dye
Facetal arthritis
Fasciitis ,
Fibroblast growth factor
Fibular collateral ligament
bursitis ,
Finger flexor tendon pulley system
299First
carpometacarpal joint
metatarsal flares
Flexor
carpi
radialis ,
ulnaris , , ,
compartment wrist
digiti minimi brevis ,
digitorum
longus , ,
profundus ,
superficialis ,
hallucis
brevis
longus , , , , ,
pollicis
brevis
longus ,
tendon
Fluoroscopically guided discography ,
Focal tenderness over facet joint
Fracture of forearm
Frankenstein test ,
G
Ganglion ,
cyst
on middle finger
Genu valgum
Glenohumeral joint
injection
Gluteal bursitis
Golfer elbow
Great toe pain
Greater trochanter
Guyon's canal , , ,
H
Hallux valgus , , , , ,
,
Hammer toe –
Hamstring tendonitis
Hemarthrosis
Hemophilia
Hip
and pelvis
injections ,
joint
arthritis ,
pain
Housemaids knee
Hyaline cartilage
Hyaluronidase
Hypertension
I
Infrapatellar bursitis ,
Infraspinatus
tear
tendon infiltration
Injectable corticosteroids
Interlaminar technique ,
Internal disk disruption
Interphalangeal
creases
joint
arthritis
Intra-articular
aspirations
injection for
distal interphalangeal joint
proximal interphalangeal joint
wrist joint
lumbar facet joint blocks
Ischial
and gluteal bursa
and trochanteric bursitis
bursitis ,
Ischiogluteal bursitis
J
Jumpers knee
K
Knee
and ankle
arthritis
effusion
joint , ,
aspiration
injection
L
Lateral
collateral ligament ,
cutaneous nerve of thigh
300epicondylitis
femoral cutaneous nerve
head of gastrocnemius
structures of knee
ulnar collateral ligament
Left subacromial-subdeltoid bursa
Leukemia
Ligaments injury
Lister's tubercle
Low backache without sciatica
Lumbar
epidural
injections
steroids
median branch block
myofascial pain syndrome
Lunotriquetral ligament
Lupus erythematosus
Lyme disease
M
Mallet toe pain syndrome ,
Manubriosternal joint pain syndrome
Medial
collateral ligament
epicondylitis
gastrocnemius
bursitis
Median nerve ,
Meningitis
Meralgia paresthetica , ,
Metacarpophalangeal
creases
joint ,
Metatarsalgia ,
Metatarsophalangeal joint ,
arthritis
Method of
palpating
head of radius
radial head
palpation of
bicipital groove
bony landmarks of shoulder
tracing flexor carpi ulnaris
Midtarsal joint ,
Miners elbow
Morning
pain
stiffness
Morton's neuroma ,
palpation
Motor branch of median nerve
Mulder sign
Myofascial pain
syndrome
Myositis ossificans
N
Nerve root
Nervi nervorum
Neuroma
Nonchronic neck pain
Nonradicular pain
O
Olecranon bursitis , , ,
Osteoarthritis , ,
Osteochondritis dessicans
Osteomyelitis
P
Palmar
cutaneous branch of median nerve
interosseous muscles
Palmaris longus , ,
tendons
Palpation of
bones of foot
bony landmarks of knee ,
Bunionette
Hamstrings
lateral structures of knee
medial structures of knee
pelvis and hip
popliteal fossa
sesamoids
shoulder
sinus tarsi and talus
talar dome and ankle joint
talonavicular joint
Patellar
tendinitis ,
tendon ,
Periarthritis
Peritendinitis
degeneration
301Peroneal
retinacula
tendinitis , ,
Peroneus tendon
Pes anserinus
bursa
bursitis
injection
Placement of needle in
epidural space
transforaminal block
Plantar
fascia ,
fasciitis , , ,
Platelet rich plasma ,
Polymyalgia
Popliteal
bursa ,
cyst
Popliteofibular ligament
Position of
biceps tendon
needle
in injection transforaminal
block
placement in caudal epidural
injection
transducer
for medial structures of ankle
ultrasound transducer for
lateral epicondyle
medial epicondyle
Posterior
deltoid ligament
interosseous nerve , ,
syndrome
knee structures
Posterolateral corner of knee ,
Posteromedial
ankle
structures
structures of ankle
Postural puncture headache
Prepatellar
bursa
bursitis
Primary osteoarthritis
Pronator quadratus
Proximal
phalanx
transverse crease
Psoas
and iliopectineal bursa
bursitis pain
Psoriatic arthritis , ,
Psychogenic rheumatism
Q
Quadrilateral space
R
Radial
artery
collateral ligament
nerve , ,
tunnel syndrome
Radicular pain ,
Radiocapitellar joint
Radiofrequency techniques
Radiohumeral joint
Reactive arthritis
Recurrent disk disease
Regional myofascial pain
Retrocalcaneal bursitis , , ,
Rheumatoid
arthritis , , , , ,
feet
hands ,
nodules
Rotator cuff
arthropathy
disorders
syndrome
S
Sacroiliac joint block
Scotty dog sign
Secondary
deformities of foot
osteoarthritis
Semimembranosus bursitis
Septic arthritis
Sesamoiditis ,
Shoulder
abduction
extension
flexion
injection ,
302joint ,
arthritis ,
injection
Sickle cell disease
Site of injection
for Achilles tendinitis
injection for peroneal tendinitis
of ankle joint
Spinal
cord
injury
stimulation
nerve root
compression
inflammation
stenosis
Staphylococcus aureus
Stenosing
synovitis of first dorsal
compartment
tenovaginitis
Sternalis syndrome
Sternoclavicular joint ,
Subacromial
bursitis ,
subdeltoid bursa –
Subacromion bursa
Subdeltoid
bursa , ,
bursitis
Subscapularis tendon infiltration
Subtalar
arthritis
joint , ,
Superficial
palmar arch
transverse carpal ligament
Suprapatellar
bursa
bursitis
Supraspinatus
infiltration
tear
tendinitis
tendon
Surface
anatomy of
elbow
shoulder
landmark of
cervical and thoracic spine
common flexor origin
lateral epicondyle
lumbar spine
Sustentaculum tali
Swimmers elbow
Symmetrical arthritis
Synovial fluid
analysis
aspiration
Synovitis of facet joint
T
Tailors bunion
Talar head
Talofibular ligament
Tarsal tunnel syndrome ,
Tendinitis ,
of Achilles tendon
Tendon ,
sheath ,
Tennis elbow
Tenoperiosteal junction
Tenosynovitis
Teres minor
Tibial
and fibular collateral ligament
collateral ligament fibrositis and
bursitis
Tibialis posterior
insertion ,
tendinitis , , ,
Tibiofibular
joint ,
ligament ,
Tibiotalar ligament ,
Tietze's syndrome
Total knee
arthroplasty
replacements
Transforaminal block ,
Traumatic arthritis
Triamcinolone acetonide injection
Triangular
fibrocartilage complex ,
space
Trigger finger , ,
303Trochanteric
bursa ,
bursitis ,
tendinitis
Tuberculosis of bursa
U
Ulnar
artery , , ,
nerve , , ,
tunnel syndrome
Ulnolunate ligament
Ultrasonographic appearance of
common
extensor origin
flexor origin
flexor
tendon ,
tenosynovitis
ganglion cyst
popliteal cyst
rim rent sign and cartilage interface
rotator cuff tear
subdeltoid bursa
tendons
Ultrasonography guided injection ,
for golfer elbow
for tennis elbow
for trigger finger
V
Value of discography
Vascular endothelial growth factor
Vasoactive intestinal peptide
Villonodular synovitis
Volkmann's ischemic contracture
W
Wrist
and hand
creases
extensor group
joint
synovitis
X
Xiphisternal joint
Xiphodynia syndrome
X-ray of
Achilles tendinitis
elbow joint arthritis
rheumatoid hand
sacroiliac joint