Human beings are placed at the peak of the evolution pyramid with five senses, i.e. vision, hearing, smell, taste and touch. Out of these the vision is most developed in human beings because they have precise distant vision, near vision, color vision, field of vision, depth perception and contrast sensitivity. Though human far vision is good yet it does not surpass the distant vision of may birds and animals. Some birds have near vision so well developed that they can pick up useful tiny food particles from grass or sand. Almost all animals have sharp night vision (scotopic vision) but most of the day flying birds have almost no night vision. Humans too have poor night vision. The color vision is unique among humans, animals and birds either have very poor color sense or they lack it altogether.
Theoretically a person with normal eye should have enough vision to see up to infinity provided the object is large and bright enough. An infant can see the smallest point from less than 5” but have poor distant vision.
The human beings have been endowed with a pair of almost identical eyes. Each capable of functioning independently but are coordinated with each other neurologically. The advantage of having two coordinated eyes are: Increased field of vision, increased depth of focus and improved vision. A person who can read two lines on Snellen's chart in one eye and three lines in the other separately, will be able to read five or six lines when both eye are used. Loss of vision in one eye does not strain the other eye. The only drawback is loss of field on the affected side. An one eyed man may have good depth sense.
To have such a versatility and diversity human eyes must have elaborate focusing system, highly developed neural coordination between two eyes, large range of vision, highly developed color sense.
The focusing system comprises of:
The neural coordination is brought about by:
- Various reflexes
- Light
- Accommodation
- Convergence
Which are governed by
- Neural centers and tracts
- Supra nuclear path
- Coordinated binocular movement
- Accommodation and convergence
ANATOMY OF THE EYE
The anatomy of the eyes can be broadly divided into:
- The orbit and its contents
- The eyeball (globe)
- The adnexa of the eye
- The intraocular structures
Orbits
The orbits are two irregular spaces placed one on each side of the midline of the face, under the forehead (frontal bone) above the cheek bone (maxilla) below. The nasal cavity lies in between the two orbits. The orbits are surrounded all-round by bones except on the outer side.
The orbits are two irregular pyramids. The apex of each pyramid is directed backwards. The sides are formed by thin bones. The walls are neither of equal length nor thickness. The medial wall of one side is parallel to the medial wall of the other side. The lateral (outer) wall is inclined towards the apex. The base of the pyramid is formed by a large circular opening in front. There are three apertures of unequal size and shape in each orbit. They are—Apex, superior orbital fissure and inferior orbital fissure. The first two communicate with the brain and transmit important nerves and vessels. Through the apex pass the optic nerve and the ophthalmic artery (Fig. 1.1).
The superior orbital fissure transmits the third, fourth and sixth cranial nerves along with lacrimal, frontal and nasociliary branch of the fifth nerve. The superior and inferior ophthalmic veins also pass through the superior orbital fissure (Fig. 1.2).
The inferior orbital fissure communicates with the maxila. It transmits few branches of inferior ophthalmic vein and maxillary division of the fifth nerve.
The orbit is lined by periorbita that continues with periosteum of skull and face. Besides there are various fascias in the orbit that divide the orbit in separate surgical space.3
The orbital contents are:
- The globe
- The muscles
- The cranial nerves: The second, third, fourth nerves, branches of fifth nerve and the sixth nerve
- The branches of ophthalmic artery
- The superior and inferior ophthalmic veins
- The branches of sympathetic chain
- The ciliary ganglion
- The orbital fat
- The orbital fascia
- There are no formed lymphatics in the orbit
The border of the base of orbital pyramid is called the rim of the orbit. It is formed by bones stronger than the walls.
- Tenon's capsule—It covers the globe from limbus to optic nerve. The space between the Tenon's capsule and the globe is called Tenon's space.
- Coverings of the extraocular muscles—They cover the extraocular muscle from all sides. Sheaths of adjacent recti are joined to each other by a thin membrane called intermuscular membrane. This form a conical space in between the muscles. The space between the bony wall and the inner conical space is called extraconal or peripheral space (Figs 1.3 and 1.4) respectively.
- The check ligaments—They are two in number, one extend from the medial rectus to the medial orbital margin and the other from lateral rectus to lateral orbital margin. They prevent excess movement of the globe.
- The transverse suspensory ligaments are also two. The first is called superior transverse ligament, the second is called inferior transverse ligament.
- The periorbita is the periosteum of the orbit. It lines the inner surface of the orbital bones. It is continuous with periosteom of the skull and dura of the brain.
- Orbital septum—It extends from the orbital margin to the tarsal plate. This divides the orbit into two unequal spaces:
- Small preseptal space
- Large postseptal space
It prevents infection from lid to pass into the orbit.
Extraocular Muscles
There are eight striated extraocular muscles and one plane muscle. Out of eight extraocular muscles, six are attached to the globe. They are:
- Superior rectus
- Medial rectus
- Inferior rectus
- Lateral rectus
- Superior oblique
- Inferior oblique
The remaining two, i.e. the levator palpebral superior and orbicularis are not attached to the globe.
The muscles that originate at the apex of the orbit are: Levator palpebral superior, the superior oblique, the superior rectus, the medial rectus, the inferior rectus and the lateral rectus.
The muscles that originate from the anterior part of the orbit are: Inferior oblique and orbicularis oculi (Table 1.1).
7The levator palpebral superior and orbicularis are not related to movement of the globe. They are concerned with opening and closing of the lids.
The above eight muscles are striated muscles (voluntary muscles) supplied by the cranial nerves.
The Muller's muscle is a non-striated muscle supplied by autonomic nervous system. It does not have a bony origin or insertion. It originates from the inferior surface of levator palpebral superior as a band and is inserted in the upper border of upper tarsal plate.
The cranial nerves in the orbit
The cranial nerves that pass through the orbit are:
- Opticnerve (second nerve)
- Oculomotor nerve (third nerve)
- Trochlear nerve (fourth nerve)
- Trigeminal nerve (fifth nerve)First and second division
- Abducent nerve (sixth nerve)
The orbicularis is supplied by facial nerve (The seventh nerve) from outside the orbit.
Optic Nerve
It is the second cranial nerve responsible for vision, color vision. It also carries afferent fibers for light reflex and near reflex. It differs from other cranial nerves in the sense that it starts in the eye and ends in the brain, while other cranial nerves involved in eye start in the brain and end in the eye.
It starts in the ganglion cells of the retina and ends in the chiasma.
It is divided into four parts—(Fig. 1.7)
- Intraocular
- Intraorbital
- Intracanalicular
- Intracranial
8The intraocular part is called the head of the optic nerve or papilla. It is circular. Its diameter is 1.5 mm (It looks larger in direct ophthalmoscope due to 15 D magnification). It is slightly raised from the surface of the retina. It has a shallow depression in the center called the cup of the optic disc. The bottom of the cup is called the lamina. It has small holes in it. The central artery of the retina enters through the cup and the central vein of the retina leaves through the cup. The central retinal artery divides into four branches on the surface of the optic cup.
Intraorbital Part
Intraorbital part is the largest segment of the optic nerve. It extends from the back of the globe to the apex of the orbit, where it leaves the orbit through the optic foramen. It is covered by dura, arachnoid and pia which extend backwards in the brain. The cerebral fluid circulates between the arachnoid and pia (Fig. 1.8).
The central retinal artery which is a branch of ophthalmic artery enters the optic nerve from below 10 mm behind the globe. The central retinal vein leaves the optic nerve 12 mm behind the globe (Fig. 1.9).
The intraorbital part has a S shapes curve, it lies loose in the orbit hence not stretched during excessive movement of the globe.
The intracanalicular part is the part of the nerve that passes through the optic canal. The optic canal is a rigid bony canal formed by the lesser wing of the sphenoid bone. The anterior end forms the optic foramen. The optic canal joins the orbit to the brain. It also transmits ophthalmic artery.
The intracranial part of the optic nerve extends from the end of the optic canal to beginning of the optic chiasma.
Oculomotor Nerve
The oculomotor nerve is meant for movement of the eyeball. It supplies all the muscles of the eyeball except the superior oblique and lateral rectus. It is also involved in constricting the pupil (miosis) and constricting the ciliary muscle (accommodation). The nerve starts in its nuclei in the midbrain, leaves the midbrain to form its basilar part then passes in the cavernous sinus after which it enters the orbit. Before entering the orbit it divides into two divisions, the upper division that supplies the superior rectus and the levator palpebral superior. The lower division supplies the medial rectus, the inferior rectus and the inferior oblique. It also gives a twig to the ciliary ganglion (Figs 1.10 and 1.2).
The ciliary ganglion is an important ganglion of the eye. It contains parasympathetic, sympathetic as well as pain fibers of internal structures of the eye. It is a pinhead sized structure situated inside the muscle cone in front the apex of the orbit between the optic nerve and the lateral rectus.
It 10lies 1.5 mm behind the globe. Paralysis of this ganglion leads to dilatation of the pupil and abolition of pain from uvea. This property is used to produce anesthesia by retrobulbar injection of anesthetic agent in the ganglion for intraocular surgeries (Fig. 1.11).
Trochlear Nerve
It is the fourth cranial nerve. It supplies only one muscle, the superior oblique. The nerve has a small nucleus in the midbrain. The fibers from one nucleus cross over to the other side to form the nerve of the other side. For example the fibers from the right nucleus forms the left trochlear nerve and the left for right nerve.
This is the only cranial nerve that come out of the midbrain on the back side (dorsal). After it leaves the midbrain it does not come near any other structure until it reaches the cavernous sinus. After the cavernous sinus the nerve enters the orbit through the superior orbital fissure outside the circle of zinn and remains outside the muscle cone. It is not paralyzed by usual retrobulbar block.
Abducent Nerve
It is the sixth cranial nerve. Like trochlear nerve it too supplies only one extraocular muscle, i.e. the lateral rectus muscle. It has a long intracranial course. The nucleus of the sixth nerve is situated in the lower part of the pons. The nerve comes out of the brain at the lower border of the pons. In the cavernous sinus it lies in the substance of the cavernous sinus and not the wall like the third and the fourth nerves. It enters the orbit through the superior orbital fissure inside the circle of zinn to supplies the lateral rectus of the same side.
Globe
This is also called the eyeball. It is a spherical structure but not a perfect sphere. Its circumference is not equally curved all over. The anterior one fifth which is 11called cornea is more curved than rest of the globe, which is called the sclera or the white of the eye. The anteroposterior diameter is more than other diameters. At birth the globe is smaller with a diameter of 16 mm. The diameter increases for first few years to reach 24 mm by tenth- year and remains so for rest of the life. If the diameter is less than 24 mm the eye becomes hypermetropic and if the diameter is more than 24 mm the eye becomes myopic (Fig. 1.12).
The globe is divided into two parts:
- A large white opaque part—The sclera
- A smaller transparent parts—The cornea
Sclera
The sclera forms the posterior 5/6 of the globe. It extends from the optic nerve up to the cornea. The function of the sclera are:
- Keep the inside of the globe dark.
- Protect the intraocular structures.
- Act as attachment for extraocular muscles.
- Act as passage for nerves, arteries and veins to and from the inner structures.
- It is not involved with vision.
- It is less pain sensitive than cornea.
- The thickness of sclera is not uniform through out. It is thickest round the optic nerve. It is almost equally thick at the junction of cornea with sclera. It is thinnest at the insertion of the recti muscles.
- There are hardly any blood vessels in the sclera but long and short posterior ciliary vessels pass through the sclera.
- The long and short ciliary nerves pierce the sclera to reach the uvea.
- The sclera is covered by a loose vascular structure on the outer surfaces the conjunctiva which is separated from the globe by Tenon's capsule.
Cornea
The cornea forms the anterior one-fifth of the outer coat of the eye (globe). The main function of the cornea is optical. The other function is protective. The optical function of the cornea can be divided into two parts:
- It acts as a strong convex lens of + 40 D when rays pass through the cornea (refracted). Its refractive index is 1.37.
- It also acts as a convex mirror, when light rays are reflected from its surface. The reflected image formed by the cornea is small, erect and virtual.
Though the cornea looks circular, it is not so in fact its vertical diameter is less than horizontal diameter. The horizontal diameter is 12 mm and vertical diameter is 11 mm. This makes the vertical meridian more curved than the horizontal meridian.
The two surfaces of the cornea are not of the same curvature. The back (posterior) surface is more curved than the front surface. Thus, the cornea is thicker on the periphery and thin the center. Thus, the central cornea is weaker than the peripheral cornea.
The cornea is always wet. It is bathed in tear film in front and aqueous behind. The tear film supplies oxygen to the cornea and the aqueous gives other nutrients to the cornea.
The surface of the cornea is always bright. Loss of brightness is a sign of disease and cause fall of vision.
The cornea is almost devoid of blood vessels except near the limbus. Presence of blood vessels in the cornea denotes disease of the cornea.
The cornea is one of the most pain sensitive parts of the body. It is supplied richly by pain sensitive nerve endings which arise from the nasociliary branch of the trigeminal.
The cornea is five layered structure. The layers are (Fig. 1.13):
- Epithelium
- Bowman's membrane
- Stroma
- Descemet's membrane
- Endothelium
1. Epithelium
The epithelium itself is three-layered. The epithelium is continuous with conjunctiva hence infection from conjunctiva can easily pass into the cornea. The epithelium is covered by tear film. The epithelium can be pealed off the cornea with ease. A breach in the epithelium heals quickly. A breach in epithelium can be demonstrated by instilling fluorescein drop two percent as bright green area. The diseased epithelial cells stain with other dyes also they are rose bengal one percent and lissamine green.
Tear Film
The eyes should always remain moist for clear vision. This is brought about by healthy tear film that covers not only cornea but also the conjunctiva. An abnormal tear film causes dryness of the cornea and conjunctiva. The condition is called dry eye. The tear film has three distinct layers each with special function.
The layers are—(Fig. 1.14).
- Oily layer (lipid)
- Watery layer (aqueous)
- Mucus layer
The oily layer is most superficial. It is secreted by glands at the lid margin. It prevents evaporation of watery layer. The watery layer is the middle layer. It is thickest out of the other two layers. It is secreted by lacrimal and accessory lacrimal glands. It forms the greatest bulk of tear film.
The mucus layer is the innermost layer. It is secreted by goblet cells of the conjunctiva. Its function is to anchor the aqueous layer to the corneal epithelium.
- It keeps the cornea and conjunctiva wet.
- It removes unwanted materials from the cornea and conjunctiva.
- It forms an essential part of the optics of the cornea.
- It provides oxygen to the cornea.
- It provides some nutrition to the cornea.
- It has mild anti-infective property.
Production of Tear
The main bulk of the tear is produced by the lacrimal gland. To this are added the oily secretion from the lids and mucus secretion from the goblet cell of conjunctiva. The tear is constantly produced and eliminated from the eye at a well regulated quantity. The tear production is brought by a delicate balance between the fifth nerve and the seventh nerve.
Drainage of Tear
The drainage of tear is brought about by constant blinking of the lids and pump action of the lacrimal sac. For this it is essential to have normal puncta, canaliculi, lacrimal sac and nasolacrimal ducts.
The quantity of tear present in the eye is roughly measured by a simple test called Schirmer test.
2. Bowman's Membrane
The Bowman's membrane is a thin membrane of uniform thickness. It is a strong membrane that prevents passage of infection and toxin to the deeper layer. It can not be repaired once it is destroyed.
3. Stroma
This accounts for ninety percent of bulk of cornea. It is formed by many lamellae made of collagen. They are very compact and are arranged in such a way that they do not obstruct passage of light through them. The stroma blends with the sclera hence inflammation from sclera can travel to cornea with ease.
4. Descemet's Membrane
It is a strong membrane under the stroma. It differs from Bowman's membrane in the sense that it has a capacity to regenerate.
5. Endothelium
Endothelium is the innermost layer of the cornea. The single-layered endothelium is attached to the Descemet's membrane. The endothelial cells have poor power of regeneration. The endothelial cells of the cornea are continuous with endothelial cells of the iris. The main function of the endothelium is to prevent the aqueous from getting into the stroma. The aqueous reaches the stroma when the endothelium is damaged. This results in swelling of the stroma.15
Limbus
The limbus is also called corneo scleral junction. It is a meeting place of cornea on one side and conjunctiva and sclera on the other side. It is not well demarcated. It is roughly 1 mm wide area all around the cornea. The corneal epithelium which is four to five layered on the cornea becomes eight to ten layered on the limbus and becomes continuous with the bulbar conjunctiva. The Bowman's membrane does not reach up to the limbus but the stroma blends with the sclera. The Descemet's membrane stops as thickened band inside as Schwalbe's line. The endothelium does not reach the limbus. The limbus is highly vascular structure.
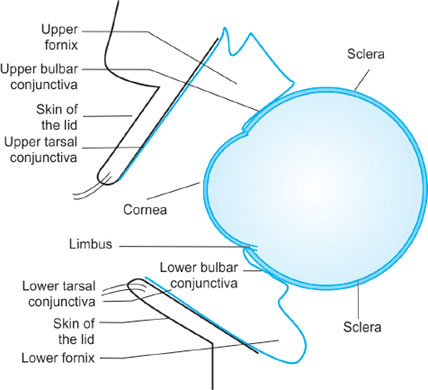
Conjunctiva
The conjunctiva may be considered as the mucous membrane of the eyeball. It spreads from the limbus to the lid margin. It is almost transparent. The sclera is visible through the normal conjunctiva. The conjunctiva is highly vascular. The vessels are very thin in normal eye. They become prominent in diseases of the conjunctiva and make the eye look red. The conjunctiva is moist. It is richly supplied by sensory nerves. It has rich lymphatic supply as well.
- Palpebral conjunctiva
- Bulbar conjunctiva
- Fornix
- The palpebral conjunctiva extends from the lid margin up to the fornix. The conjunctiva that covers the lid margin is called marginal conjunctiva. It can not be separated from the lid margin. On the outer surface it is continuous with the skin of the lid margin.
The tarsal conjunctiva extends from the inner lid margin to the fornix. It is divided into two parts:
- Tarsal conjunctiva
- Orbital conjunctiva
The tarsal conjunctiva is firmly adherent to the tarsal plate. The attachment is so firm that the conjunctiva can not be separated from the tarsal plate. In normal conjunctiva the tarsal glands are visible as translucent lines. The tarsal glands are not visible in diseases of the conjunctiva. Tarsal conjunctiva is the place where papillae and follicles develop. It is a common site for fibrosis.
The orbital conjunctiva extends from the border of the tarsal plate to the fornix. The junction on either side is not well marked. It contains Wolfring glands that secrete mucus. The conjunctiva of the fornix is very loose. The upper fornix is larger and deeper than lower.
- The bulbar conjunctiva is the largest and most visible part of the conjunctiva. It extends from the limbus to upper fornix above, to lower fornix below, medial canthus towards to nose and lateral canthus towards the ear. It can be moved over the sclera except 3 mm round the limbus, where it is firmly attached to the sclera. Due to its looseness lots of fluid can accumulate under the conjunctiva. The space under the conjunctiva is called subconjunctival space, where medicines can be injected. Like other parts of conjunctiva it is always moist. There are hardly any visible blood vessels in the bulbar conjunctiva unless it is diseased. The conjunctiva contains goblet cells that secrete mucus.
- Fornix
The junction of the bulbar and palpebral conjunctiva form the fornices. There are four fornices, the two deep fornices and two very shallow fornices. The deep fornices are upper and lower fornix. The shallow fornices are medial and lateral. Out of two deep fornices, the upper is larger and deeper. 17The conjunctiva here is thrown into folds. The conjunctiva in the fornix is very loose. The ducts of lacrimal glands and Krause's gland open in the upper fornix. Only Krause glands are present in the lower fornix. The upper fornix is not easily visible. It requires a special technique, i.e. double eversion of the upper lid to see the upper formix. The lower fornix can be examined just by pulling the lower lid.
Caruncle
The caruncle is an oval mass of fleshy tissue in between the two lids on the nasal side of the conjunctiva. It is covered by conjunctival epithelium. It contains hair follicles, sebaceous glands and sweat glands that are absent in the conjunctiva. It also contains accessory lacrimal gland, Krause's gland and goblet cells similar the conjunctiva. It does not have any definite function.
Plica Semilunaris
It is a vertical crescent shaped fold of conjunctiva between the caruncle and the limbus. It too does not have any definite purpose.
Ocular Adnexa
The ocular adnexa consists of lids with their lining and the lacrimal apparatus.
Lids
There are two lids on each side. A large upper lid and a small lower lid. The upper lid extends from the eyebrow above to the lashes of the lid up to the canthi. The lower lid extends from the cheek to the lashes at the level of canthi. When the eyes are open and looking straight, the upper lid covers upper 2 mm of the cornea and the lower lid just touches the lower limbus (Fig. 1.17). When the eyes are closed, the upper lid comes down up to the pupil and the lower lid goes up to meet the upper lid. The space between the two lids is called interpalpebral aperture. The junction of the two lids are called canthi. They are two in number one medial and one lateral canthus. The canthi are kept in place by two canthal ligament one on each side extending from the canthus to the orbital rim.
18The lids act simultaneously in harmony. The upper lid covers more area than the lower lid. The main function of the lids is to protect the orbit, the eyeball and the conjunctiva. Its movement spreads the tear uniformly on the cornea and the conjunctiva. The closure of the lids forces the tear out of the conjunctival sac and drain in lacrimal sac.
The structure of both the lids are similar except the presence of a well developed levator palpebral superior and Muller's muscle in the upper lid.
Structures of the lid are (Fig. 1.18):
- The skin
- The fibromuscular layer
- The conjunctiva
- The lid margin
The skin of the lid is very thin and loosely attached to the underlying muscle by areolar tissue. The skin can be moved over the fibromuscular structure and lifted. The upper lid forms a well-marked horizontal crease. The skin blends with the marginal conjunctiva.
The lid margin is the transient zone between the skin in front and conjunctiva at the back. The front end is rounded, the back end is sharp. The front end contains the eye lashes. The lashes are arranged in three to four rows. The lashes of upper lid are more in number and larger than the those of the lower lid. The lashes of the upper lid are curved upwards while the lower lid lashes are curved downwards.
Two types of glands open at the root of the lashes, they are:
- Gland of moll: These are sweat glands.
- Gland of zeis: These are sebaceous gland.
A gray line lies between the anterior and posterior border of the lid margin just in front of the opening of the meibomian glands, which are modified sebaceous gland.
19On the medial side of the lid margin, two millimeter from the medial canthus are two lacrimal puncta one in each lid.
Fibromuscular Layer of the Lid
The fibromuscular layer comprises of:
- The septum orbitale and the tarsal plate
- The muscles of the lid
- The orbicularis
- The levator palpebral superior
- The Muller's muscle
The septum orbital is a fibrous structure that extends from the periorbita of the orbit to the tarsal plate. In fact the tarsal plates are embedded in the septum orbitale. It divides the orbit in two un equal parts. A smaller preseptal part and a larger postseptal part. Its function is to prevent the contents of the orbit to bulge forward. It also gives support to the tarsal plate and prevents pre septal infection to pass into the orbit.
Tarsal Plate
Each lid in its posterior part has a fibrous structure called tarsal plate. The tarsal plate of the upper lid is larger than that of the lower lid. The function of the tarsal plate is to give firmness to the lid and support the lid. It also acts as attachment of levator palpebral superior in the upper lid. The tarsal plate contains the meibomian glands. The meibomian glands of the upper lid are larger and more in number than lower lid.
The levator muscle in the upper lid is attached to the top of the tarsal plate. To the lateral and medial side it is attached to lateral and medial palpebral ligament.
The posterior border of the tarsal plate is firmly attached to the tarsal conjunctiva.
Muscles of the Lid
- The orbicularis oculiThis is a striated muscle that lies in the front part of the orbit in a circular fashion. It has two parts:
- Palpebral part—This is placed in the lid and is used to close the lid lightly.
- The orbital part—This is placed mostly in the front part of the orbit and is used to close the lid tightly.
The action of the orbicularis is to close the lids. This action is opposed by the levator palpebral which opens the lids. The orbicularis is supplied by the seventh nerve. Paralysis of this muscle prevents the lid from being closed and the condition is called lagophthalmos. - The levator palpebral superior
The muscle takes origin from the apex of the orbit passes under the roof of the orbit in a fan shaped manner. The nasal end of the fan is attached to the medial palpebral ligament while the outer end in attached to the lateral canthal ligament.
The muscle is divided into three parts. The most anterior passes through the fibers of the orbicularis and is inserted in the skin of the lid.
The central part is attached to the top of the tarsal plate.
The posterior part is inserted in the conjunctiva of the upper fornix.
The muscle is supplied by the upper division of the third nerve. Its paralysis causes marked drooping of the upper lid. The condition is called ptosis.
The Muller's muscle is a small strip of unstriated muscle. It is better developed in the upper lid. It does not have any bony origin or insertion. It originates from under the surface of the levator and is attached to the orbital margin of the tarsal plate. In the lower lid it arises from the inferior rectus muscle. It is supplied by cervical sympathetic and not by any cranial nerve. Its paralysis causes mild drooping (ptosis) of the upper lid.
Lacrimal System
Lacrimal system consists of two parts (Fig. 1.19):
- Structures producing tear
- Structures draining tear
Structures producing tear consist of:
- Main lacrimal gland
- Accessory lacrimal glands
The main lacrimal gland is the main source of tear in the eye. It is situated at the superotemporal aspect of the orbit. It is neither visible nor can be felt by the finger. The main gland is divided into two parts—(1) orbital part, (2) palpebral part. The former is larger of the two.
There are ten to twenty 21ducts that carry tear from the lacrimal gland to the conjunctiva. The ducts open in the conjunctival sac above the lateral end of the tarsal plate. The lacrimal sac is supplied by trigeminal, facial and sympathetic nerves.
The accessory glands play a minor role in producing tear. They are situated in the conjunctiva. They are
- Krause's gland
- Wolfring's gland
- Glands situated in the plica and caruncle
- Infraorbital glands
The structures draining the tears consist of:
- The lids
- Upper and lower puncta
- Upper and lower canaliculi
- The nasolacrimal duct
The lids by their regular blinking movements push the tear from upper fornix towards the medial canthus across the conjunctiva and the cornea. The sharp inner margin of the lower lid prevents the tear from flowing out, over the lid margin.
Puncta
There are two puncta, one in each lid on the nasal side in the lid margin about 6 mm away from the medial canthus. They are about 1mm in diameter. The lower puncta along with lower canaliculus drain 75% of tear.
Canaliculi
Each puncta has a corresponding canaliculus. Each canaliculus has a vertical and a near horizontal part, both meet at an angle. The canaliculi lie in the substance of the lid. They are not visible. The two canaliculi join each other before entering the lacrimal sac.
Lacrimal Sac
The lacrimal sac lies in the lacrimal fossa in the anterio medial part of the orbit. The upper part is dilated and rounded. The rounded area is called the fundus of the sac. The lower end of the sac opens in the nasolacrimal duct. The sac is 15 mm x 5 mm hollow structure. The sac is surrounded by bone on all sides except the front surface, which lies under the medial palpebral ligament. The normal sac is neither visible nor felt by finger unless distended.
The nasolacrimal duct is a tube that joins the lacrimal sac to the nasal cavity. It is surrounded by bones from all sides and can not be felt by fingers.22
Intraocular Contents
The intraocular contents are (Fig. 1.20):
- Uvea—Iris, ciliary body, choroid
- Retina
- Vitreous
- Lens and suspensory ligament
- Aqueous
Out of the above five the first two are vascular and capable of inflammation and neoplasm. The remaining three do not have any blood supply hence are not inflicted by inflammation and new growth.
Arrangement of Intraocular Contents
The outermost layer of the eyeball is formed by the cornea and sclera, 5/6 by the sclera and remaining by the cornea. It is lined by uvea (choroid) that forms the middle coat. The innermost coat is formed by the retina. The space inside the retina filled by vitreous, lens and the aqueous. The lens along with its suspensory ligament divides the eyeball into two unequal chambers. A large vitreous chamber and a smaller aqueous chamber. The iris again divides the aqueous chamber into two unequal parts; one large anterior chamber and a small posterior chamber. The anterior and posterior chambers communicate through a central hole in the iris—the pupil. The anterior and posterior chamber are filled by a clean fluid called aqueous humor.
The uvea is the middle coat of the eye. It divides into three parts:
- The iris
- The ciliary body
- The choroid
The iris is most anteriorly placed part of the uvea. It hangs like a curtain behind the cornea and in front of the lens. It is dark in color. Its surface is uneven with small pits in it. It divides the aqueous chamber into two parts, a large anterior chamber and small posterior chamber. They communicate with each other through circular hole in the center of the iris called the pupil.
23The normal pupil is about 3.5 to 4 mm in diameter. It is smaller in children and in old age. The pupil is smaller in eyes with darker iris. It is small in hypermetropia. A pupil smaller than 2 mm is called miotic pupil and a pupil larger than 4 mm is called mydriatic (dilated) pupil. The pupil constricts in bright light and dilates in dark. The size of the pupil in both eyes in generally equal. If there is difference in size of the pupil it is called anisocoria. The size of the pupil can be changed by many drugs. The drugs that constrict the pupil are called miotics. Commonly used drug is pilocarpine. The drugs that dilate the pupil are called mydriatics. The commonly used mydriatics are atropine, homatropine, cyclopentolate, tropicamide, adrenaline and phenylephrine.
The function of the pupil are:
- Regulate amount of light entering the eye.
- Allow free flow of aqueous from posterior chamber to anterior chamber.
The iris arises from the ciliary body. The iris is thin at its origin from the ciliary body hence likely to be torn by injury. It is thicker at the pupillary border. The pupillary border is darker than rest of the iris.
The iris has a single-layered endothelium on its front surface. The endothelium is continuous with corneal endothelium. It is absent over the small pits seen on the front surface of the iris. They are called the crypts of the iris. They are the cause of roughness of the iris.
The structure behind the endothelium is called stroma. It is the thickest part of the iris. It contains blood vessels, connective tissue, iris pigment, two nonstriated muscle, the constrictor and the dilator muscles.
The constrictor muscle is situated round the pupil and meant to constrict the pupil. It is supplied by third nerve.
The dilator muscle is situated near the base of the iris. It is meant to dilated the pupil. It is supplied by the cervical sympathetic.
The innermost layer of the iris is the iris epithelium. It has two layers: one pigmented and the other nonpigmented. They are extension of pigmented and nonpigmented layers of the ciliary body. The pigmented layer lies behind the nonpigmented epithelium.
The reflexes that constrict the pupil are:
- Light reflex
- Near reflex
- Accommodation
- Convergence
Before going to understand pupillary reflex it is essential to understand visual path as it is intimately associated with pupillary reflex.
Visual Path
The visual path is a neural tract. It is not a reflex path. However, the afferent arm of the light reflex and the accommodation reflex pass through it (Fig. 1.21).
The visual path extends from the retina up to the visual cortex. The stimuli from the retina pass in the optic nerve; from there they pass in the chiasma. The retinal fibers arising from the temporal (outer side) pass 24straight into the optic tract up to the lateral geniculate body, from there they pass into optic radiation and end in the visual cortex in the brain.
The fibers arising from the nasal retina pass on the other side in the chiasma to pass to the optic tract, lateral geniculate body, optic radiation and visual cortex.
Thus the structures beyond the chiasma contain fibers from both the eyes.
Each reflex has two paths, one from the eye to the brain—this is called afferent path and the other is from the brain to the eye—this is called efferent path.
The afferent path of the light reflex (Fig. 1.22A) starts in the retina and passes through the optic nerve—chiasma and optic tract. From the optic tract it passes to the third nerve nucleus. In the chiasma some of the fibers cross over the other side. Thus each optic tract contains afferent fibers from both eyes. Hence when light is thrown in one pupil both the pupil constrict.
The efferent path starts in the third nerve nucleus, pass along lower division of the third nerve to the ciliary ganglion. From ciliary ganglion it pass into short ciliary nerves and end in sphincter pupillae.
Near Reflex
This consist of two reflexes: (1) the accommodation reflex, (2) the convergence reflex, which happen simultaneously but have different pathways.25
Accommodation Reflex
The term accommodation means ability to see small objects at 30 cm. The afferent path for accommodation passes through optic nerve—chiasma —optic tract of the same side up to lateral geniculate body—striate cortex —para striate (Fig. 1.22B).
26The efferent path starts in the third nerve nucleus, passes through the third nerve to the ciliary ganglion and ends in the ciliary body and iris.
Convergence Reflex (Fig. 1.22C)
The exact path of the convergence reflex is not well understood.
The afferent path most probably starts in the medial rectus from where it passes into the third nerve that takes it to the mesencephalic nucleus of fifth nerve from where it goes to the convergence center from there it goes to the third nerve nucleus and reaches the ciliary ganglion.
The three phenomenon: the constriction of pupil, accommodation and convergence go together when the eyes try to see small objects kept at near point, i.e. 30 cm
Ciliary Body
The ciliary body lies behind the iris and anterior to the choroid. In fact the iris arises from the ciliary body. The junction of the ciliary body to choroid is not well demarcated.
The ciliary body is triangular in shape with its apex towards the choroid and the base towards the lens. To the base are attached the suspensory ligaments of the lens. The outer wall of the triangle is parallel to the sclera with a potential space in between. The outer end of the base of the triangle is firmly attached to the sclera at scleral spur. The inner wall is divided into two parts—the pars plicata which contain ciliary processes and an avascular part called pars plana.
The ciliary body has a large stroma which is lined by epithelium on the inner side.
27The stroma is mostly made up of the ciliary muscles which are surrounded by connective tissue, vessels and nerves. The ciliary body is richly supplied by blood vessels. The ciliary muscles are unstriated. There are three types of muscles in the ciliary body:
- The longitudinal muscles
- The circular muscles
- The oblique muscles
The ciliary muscles are supplied by parasympathetic via short ciliary nerve.
The ciliary body on its inner surface is covered by two layers of epithelium:
- The pigmented epithelium: It is continuation of pigment epithelium of the iris in front and pigment epithelium of the retina behind.
- The nonpigmented epithelium is continuation of nonpigmented epithelium of iris in front and sensory retina behind.
Ciliary Processes
These finger like projection arise from the pars plicata. Each process has a double-layered wall made up of ciliary epithelium. They are 60 to 70 in number. They contain a tuft of blood vessels. The main function of the ciliary processes is to form aqueous.
The functioning of the ciliary body are:
- From its base arise
- The iris anteriorly
- The suspensory ligament of the lens in the middle.
- It is responsible for accommodation.
- It produces aqueous humor.
Aqueous Humor
The aqueous humor is a crystal clear fluid that fills both the posterior and anterior chamber, aqueous is formed in the ciliary processes at a constant rate in the posterior chamber from where it passes into the anterior chamber there it moves by convection current and leaves the anterior chamber via angle of anterior chamber (Fig. 1.23).
The function of the aqueous humor are:
- Optical.
- It provides nutrition to the lens and cornea.
- It maintains intraocular tension.
- It removes waste products.
Chambers of the Eye
As discussed earlier the lens along with its ligaments divide the interior of the eye in two unequal chamber—A large vitreous chamber and a small aqueous chamber. The former contains vitreous and the later contains 28aqueous.
The iris divides the aqueous chamber into two chambers agains a large anterior chamber (AC) and a small posterior chamber (PC) both are joined by the pupil.
The anterior chamber is a space bounded by the cornea in front and the iris, pupil and the lens behind. If the lens is absent the posterior boundary is formed either by anterior surface of IOL after cataract or vitreous as the case may be (see aphakia and pseudophakia). The two surfaces meet on the periphery to form the angle of anterior chamber. The angle is not impervious structure, it contains a sieve like structure called trabecular meshwork which opens in canal of Schlemm which in turn is joined to episcleral vein by a narrow aqueous vein. The anterior chamber does not have an uniform depth. It is deepest in center and is abolished at the angle of anterior chamber.
The posterior chamber is bound by iris, pars plicata of ciliary body, suspensory ligament and lens. The ciliary processes project in the posterior chamber and pour aqueous in the posterior chamber. The posterior chamber communicates with the anterior chamber through the pupil.
Formation of Aqueous Humor
There are three mechanisms involved in its production—Secretion, ultra- filtration and diffusion.
The aqueous is 99% water, remaining part is made up of solids dissolved in it. They are protein, ascorbic acid, sodium, potassium, urea and enzymes to name a few. The aqueous is formed constantly by the ciliary process at constant rate. The aqueous leaves the anterior chamber at a constant rate. There is a delicate balance between production and drainage of aqueous. 29The production can be reduced by many drugs. The drainage can be reduced due to obstruction of the flow. The two common sites of obstruction are pupil and angle of the anterior chamber.
Choroid
The choroid is the largest part of the uvea. It extends from the pars plana to the optic nerve. It lies between the sclera, and the retina. There is a potential space between the choroid and the sclera it is called the suprachoroidal space. The choroid supplies blood to the retina specially the macula.
The choroid is very vascular. The vessels are held together by connective tissue. There is no muscles in choroid. The choroid is heavily pigmented hence black. The blood vessels of choroid are of three sizes, i.e. the large, medium and fine. The latter are called choriocapillaries which are responsible for blood supply to the retina. Between the retina and the chorio-capillaries lies a thin membrane called Bruch's membrane which is attached to the pigment epithelium of the retina.
The function of the choroid are:
- To supply nutrition to outer layers of the retina.
- It keeps the inside of the eyeball dark.
Blood Supply of the Uvea
The uvea gets its blood supply from two sources:
- Posterior ciliary arteries
- Anterior ciliary arteries
Both are branches of ophthalmic artery which is the main source of blood supply to the eye and its adnexa.
Ophthalmic artery has twelve branches in the orbit. Out of which only two, the posterior ciliary arteries and the muscular branches supply the uvea. The twigs of the muscular branches that supply the uvea are called anterior ciliary artery.
The short posterior ciliary arteries are ten to twenty in number. They enter the sclera in a circular fashion round the optic nerve and divide to form choriocapillaries.
The long posterior arteries are two in number, one nasal (inner) and the other temporal (outer). They enter the sclera in front of short ciliary arteries one on each side and reach the ciliary body.
Anterior Ciliary Arteries
They enter the sclera 5 mm away from the limbus in front of the insertion of the recti muscles. They enter the ciliary body and join the posterior ciliary artery to form the major circle of iris. The major circle give branch to ciliary body, the ciliary process and recurrent branch. From the major circle of iris arise smaller branches that form the minor circle of iris. The venous drainage of the uveal tract is via four venae vorticosae.30
Retina
The retina is the most developed neural part of the eye concerned with vision, color vision, vision in bright light (photopic), vision in dull light (night vision or scotopic vision) field of vision.
It is the innermost layer of the three coats of the eyeball and placed between the vitreous and the choroid. It extends from the optic nerve to the periphery of the choroid the ora serrata. The retina is firmly attached in these two places.
The retina is transparent but looks pink due to the pigments in the retinal pigment epithelium, visual purple in the rods and underlying choroidal blood vessels. The retina looses its transparency when diseased.
The retina develops from the two layers of the optic cup with a potential space in between. The retina can be divided into two parts, i.e. the layer of retinal pigment epithelium and sensory retina. The retinal pigment epithelium is attached to the Bruch's membrane.
The sensory retina has three types of cells:
- Visual cells, the rods and cones
- The bipolar cells
- The ganglion cells
It has two limiting membranes, the external limiting and inner limiting membrane.
The two nuclear layers: The outer and inner nuclear layers.
The plexiform layers—The outer and inner and single layer of ganglion cells and nerve fiber layer.
Thus retina is ten-layered structured all over except at the macula and ora serrata. All the layers except the nerve fiber layer stop at the margin of the optic disc. The nerve fibers pass through the lamina to form the optic nerve. As there are no visual cells in the optic nerve head it has no visual sensation and forms the blind spot.
The retina is not uniformly thick all through. It is thinnest at ora serrata and thickest at the posterior pole.
The two visual elements too are not uniformly distributed. The cones which are concerned with central vision, day vision and color vision are maximum at the macula and scanty on the periphery. The rods which are concerned with night vision and peripheral vision are maximum on the periphery. The peripheral retina has very poor color sense.
The macula is an ill defined circular zone 5.5 mm in diameter, is the most sensitive part of the retina. It is situated in the posterior pole on the outer side of the disc. The central 0.35 mm is called foveola, it is surrounded by a zone 1.5 mm in diameter called fovea. The foveola is situated about 3 mm away from the temporal border of the disc. It is a small depression. It has only internal limiting membrane. All other layers are absent at foveola.
31The retina has double blood supply. (1) The outer four layers get blood supply from the choriocapillaries. (2) The inner six layers get their blood supply from central retinal artery and its branches. The retinal arteries do not anastomose (mix) with each other (Fig. 1.24).
The central retinal artery is a branch of ophthalmic artery. It arises from the ophthalmic artery at the apex of the orbit and runs under the optic nerve. It enters the optic nerve from its under surface 10 mm behind the globe and takes central position in the nerve. It enters the globe at the center of the disc and divides into two branches—a superior branch and an inferior branch. Each divide into two branches again—one medial (towards nose) and other temporal (towards the ear) in curved fashion. Each keep on branching till it reaches the ora serrata. The temporal branches curve round the macula but do not give branches to the macula.
The retinal veins correspond with the artery at the places they cross the artery and the area is called arteriovenous junction.
Nerve Supply of the Eye
The uveal nerve supply can be divided into two parts:
- Sensory via trigeminal—Nasociliary
- Motor via oculomotor—Parasympathetic and sympathetic (iris and ciliary body)
- Of all the intraocular structure only iris and ciliary body are capable of movement.
- The choroid and retina do not show any movement.
- The retina has no pain sensation. The nerve supply to the eye can be divided into:
- Sensory supply to cornea and sclera by nasociliary
- Motor supply to iris and ciliary process by:
- Parasympathetic
- Sympathetic
The nerves that supply the uvea are collectively called ciliary nerves. They are of two types:
- Short posterior cililary
- Long ciliary
The short posterior ciliary nerves are about 15 in number. They arise from the ciliary ganglion and carry both sensory as well as autonomic (motor) nerve. They enter the globe round the optic nerve. The long ciliary nerves are two in number. They arise from nasociliary nerve. They are mostly sensory. They are mostly parasympathetic in nature but have few sympathetic fibers as well.
The long ciliary nerves are two in number. They enter the globe one on each side of the optic nerve. They arise directly from the nasociliary nerve and carry mostly sensory fibers and few sympathetic fibers.
Lens
The adult normal lens is transparent structure that concentrates light rays on the retina. It is placed in front of the vitreous and behind the iris. The pupil allows the light to pass through it. It is suspended from the ciliary body. The lens when seen from front looks circular and when seen from sides it is elliptical and biconvex. At birth it is spherical. The diameter of the adult lens is 9 mm to 10 mm and thickness is 4.5 mm in the center. It has a front (anterior) and a back (posterior) surface. The anterior surface is less curved than the posterior surface. The place where the two surfaces meet is called the equator of the lens and is rounded. The center of the anterior surface is called anterior pole. This lies in the center of the pupil. The center of the posterior surface is called posterior pole.
The adult lens is semisolid. The lens of childhood is soft.
- Capsule
- Epithelium
- Fibers
- Cortex
- Nucleus
- Suspensory ligament
The capsule is single-layered structure that surrounds the lens on all the sides. It is not of equal thickness. It is thickest at the equator and thin at the poles. The posterior pole is thinnest. The overall thickness of the front capsule is more than the capsule at the back.33
Lens Epithelium
This comprises of single-layer of cubical cell. It is present only in the front surface under the capsule. The cells of the epithelium become long at the equator. They keep on increasing in length and multiply due to repeated division. The old elongated cells are pushed toward the center.
Fibers
The so called fibers are nothing but elongated epithelial cells. The old cells loose their nuclei. The process of elongation and division continue 34throughout the life. The oldest fibers become central most and compressed to form various zones of nucleus and each zone has a separate name according to time of their development. These are embryonal. They contain the oldest fibers laid down between one to three months of pregnancy. It is the smallest nucleus. The fibers laid over this between birth to puberty form the infantile nucleus. Nucleus formed after this is called adult nucleus.
The remaining part of the fibers that surround the nucleus from all sides is called cortex.
The suspensory ligament (zonules) are not true parts of the lens. There development is different from development of the lens. They originate in the ciliary body arising from both pars plana as well as pars plicata. They are inserted in the capsule at the equator. Their functions are to keep the lens in place. Suspensory ligament and lens form a barrier between the aqueous and vitreous chamber. Contraction of suspensory ligament change curvature of lens.
Action of the Lens
The lens has only one function that is to focus the rays of light on the retina from various distances by changing the curvature of the lens, thus changing the power of the lens. The ability to change the power of the lens is called accommodation. More is the curvature, more is the power. The other causes of increased power is increase in the refractive index of the lens. The refractive index of the transparent lens is 1.43. The total power of the lens is +15 to +16 D. The change in the refractive power can also be brought about if the water content of the lens is increased. This happens in diabetes and immature cataract.
Nutrition of the Lens
The adult lens is avascular. The sole nutrition of the lens comes from the aqueous after birth. During its development it gets its nutrition from a vascular envelop called tunica vasculosa lens that surrounds the lens from all sides.
The lens is 66% water and 33% protein. If the protein is denatured the lens fibers loose transparency.
Vitreous
Of all the intraocular structures the vitreous is largest in volume. It occupies two-thirds of the globe. It is an inert gel that extends from the back of the lens to the optic disc. It comes in contact with the retina from ora serrata to the margin of the disc. It is firmly attached to the ora serrata by a band of vitreous 4 mm wide. This is called the vitreous base. It has weak attachment at the macula. Its attachment to the back of the lens is very strong in children but gradually becomes loose. The bond between the lens and the vitreous is absent after 50 years of age. The vitreous does not have a formed capsule. Its periphery is more condensed than the rest and is called its capsule. 35Rest of the vitreous is called cortex. The vitreous is 90% water to which are dissolved hyaluronic acid and polysaccharides.
The vitreous is a semisolid gel. It gets liquefied in disease and following injury. Its main function is optical. The other important function is to keep the retina in place. It also maintains the shape of the eye. It is avascular after birth. It has a low metabolism. It gets nutrition from the aqueous and the retina.
Development of the Eyes (Embryology)
The eye develops from the central nervous system that itself develops from neuroectoderm. The eye is not fully neuroectodermal in origin. The surface ectoderm and mesoderm also contribute in its development (Fig. 1.27).
The eyes start developing from very early stage of pregnancy when the embryo is only 2.6 mm in length, i.e. between second and third week of conception. The eyes grow out of the developing forebrain.
Out of 36three germinal layers of the developing fetus (embryo): the ectoderm, the mesoderm and the endoderm, only the first two take part in development of the eyes. The ectoderm is divided into two types—the neuroectoderm and surface ectoderm.
To begin with the developing head of the embryo is two layered:
- An outer covering of surface ectoderm.
- A tube of neuroectoderm inside.
As the embryo grows the forebrain develops two pouches one on each side of the forebrain. The pouches are called primary optic vesicles. The primary optic vesicles is continuous with the forebrain by a narrow tube called the optic stalk, which is the future optic nerve.
As the primary optic vesicle grows it reaches the surface ectoderm. This starts two different type of changes (1) one in the primary optic vesicle and the (2) other in the surface ectoderm. The surface of the primary optic vesicle that comes in contact with the surface ectoderm becomes concave and grows backward making the primary optic vesicle two layered, at this stage it is called secondary optic vescicle, which ultimately develops into retina. From the outer wall develops the pigment layer while the inner layer gives rise to sensory retina. The structure is now called as optic cup. The two layers of the optic cup are continuous at the rim of the optic cup. From the tip of the cup develop the ciliary epithelium and pigment epithelium of the iris.
The primary optic vesicle undergoes the following changes:
Primary optic vesicle → Secondary optic vesicle → Optic cup → Retina, ciliary epithelium and pigment epithelium of the iris.
The surface ectoderm undergoes many changes.
The place where the primary optic vesicle touches the surface ectoderm thickness and the thickened area is called the lens plate. The lens plate rapidly grows and becomes concave and the structure is now known the lens pit. This deepens further, the two edges of the pit come together and join each other. Thus a hollow spherical structure is formed. This is called lens vesicle. This separates from the surface ectoderm and is pushed into the optic cup to be converted into a lens.
In the meantime the gap in the surface ectoderm disappears and from this surface ectoderm will develop the corneal epithelium, the conjunctival epithelium and the lid folds.
The optic cup closes from above downward and the gap between the two edges is called the fetal fissure through which the hyaloid artery enters the optic cup to supply nutrition to the lens before birth. The hyaloid artery extends from optic cup to the lens. Once the lens has developed and started getting its nutrition, the hyaloid artery gradually disappear. The vitreous develops from three sources, i.e. the surface ectoderm, the neuroectoderm and mesoderm in three stages, i.e. primary, secondary and tertiary vitreous.
The mesoderm surrounding the optic cup given rise to sclera, extraocular muscles and part of the lower and outer walls of the orbit.