A patient with an ocular motility disorder may present with the following clinical complaints:
- Subjective symptoms of headache, diplopia, asthenopia.
- A manifest strabismus.
- An abnormal head posture.
- Defective ocular movement.
- Decreased vision in one or both eyes.
- Nystagmus.
An accurate and detailed history, and a step-by-step clinical examination not only helps in diagnosing the cause of strabismus but also helps in outlining a management plan.
HISTORY
Many visual problems in children are associated with developmental anomalies, hereditary disorders or diseases of the childhood.
- Detailed medical history: Regarding child's developmental milestones, his progress at school. Any medical illness, e.g. epilepsy, jaundice, diabetes, meningitis may result in poor mental capabilities; history of head injury may result in paralytic strabismus. Child receiving any current medications.
- Obstetric history: Regarding child's gestational age and birth weight, any trauma sustained during labor, mother's health during pregnancy.
- Family history: Regarding refractive errors, particularly myopia, astigmatism and strabismus.
- History of strabismus: Its age of onset, direction (eye turning inwards or outwards), whether intermittent or constant, any increase in the angle of deviation, therapy already received in the form of glasses, occlusion, surgery; diplopia indicates either an increase in the angle of strabismus or a strabismus of recent onset.
EXAMINATION
Idea of examination is to find answers to the following questions:
- Is the Squint really present? Exclude pseudo-strabismus, ± angle kappa.
- Why in this particular patient? Must find the cause of strabismus.
- How much? Need to have a proper objective measurement.
- What will be the Management plan?
- General Appearance: As a patient walks into the clinic, note his gait, posture, appearance.Conditions commonly associated with strabismus in a child are: Hydrocephalus, microcephaly, Down's syndrome, albinism, cerebral palsy commonly associated with congenital esotropia/exotropia of a large and variable angle.In adults: Facial palsy, dysthyroid ophthalmopathy, tremors, ataxia, deafness, trauma.
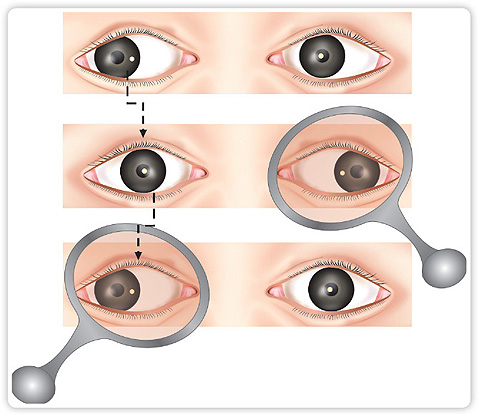
- Abnormal Head Posture (AHP):Face Turn: Indicates a horizontal deviation (Figs 1.1A to C).Head Tilt: Torsional deviation in oblique muscle palsies.Chin Up/down: It indicates a vertical deviation or ptosis (Fig. 1.2). A chin up posture is adopted to increase the field of vision.In a child, AHP indicates good binocular visual potential. In an adult, AHP is adopted to avoid diplopia.Differences between an ocular and a non-ocular cause of AHP:
- The ability to straighten the head in ocular torticollis.
- The presence of squint/nystagmus on straightening the head.
Ocular causes: Paralytic squint, A/V pattern, to obtain better vision in ptosis, nystagmus, field defect, restricted ocular movement (Duane's retraction syndrome). - Position of Eyelids: Epicanthus, telecanthus blepharophimosis syndrome (Fig. 1.2), ptosis (Fig. 1.3A) may result in pseudo-strabismus.Lid retraction: It is seen in facial palsy (Fig. 1.3B) thyroid eye disease may point towards a restrictive myopathy, orbital blow out fractures with muscle entrapment.Ptosis causes amblyopia and may be the result of 3rd nerve palsy, myasthenia, chronic progressive external ophthalmoplegia.Narrowing/widening of palpebral aperture on eye movement indicates lid retraction in restrictive disorders, aberrant 3rd nerve regeneration (Figs 1.4A and B).
- Assessment of Visual Acuity: Aims of examination are:
- To find the functional status of either eye.
- To record patient's vision according to his age.
- Before proceeding on to ophthalmic examination, it is important to get an idea of visual potential of either eye.
Visual assessment in toddlers:- Assessment of fixation and following of light: A fixation light is used at child's eye level, at a distance of 33 cm and the position of corneal reflections from both eyes are observed; the steadiness and persistence of fixation is also noted. Observe if the infant follows the light source with both eyes. Avoid auditory stimuli so that there is no reflex eye movement in the direction of sound.
- Visually directed reaching for small objects: A poorly sighted infant will move his hand in an exploratory manner rather than directly reaching it.
- Presence and type of manifest strabismus: This is detected by noting the position of corneal reflections from both eyes (Hirschberg's test) and then by performing a cover-uncover and alternate cover test to detect the presence of a phoria as well as a tropia.
- Check for amblyopia: If the child protests covering one eye, the other eye may be amblyopic (ask the mother to cover child's eye as this is less threatening to the child than an examiner's hand).
- Preferential looking: This is a quantitative assessment of a child's visual potential using either Keeler cards or Forced Choice Preferential Looking. It is helpful in monitoring progress in amblyopia therapy in infants and mentally subnormal children.
- A 10 PD test: Holding a 10D prism in front of one eye and note a correcting eye movement to diagnose microtropia or orthophoria.
Assessment of visual acuity in illiterate children (3–5 years age group)This is done by matching the symbols or pictures with a replica held in hand to be used at 33 cm or 6 m. These tests include:- Stycar letters: They are in the form of square, circle and triangle shapes, and the first to be recognized and copied by young children (Fig. 1.5).
- E test: Capital letter E can be presented with the limbs directed up, down, right or left as single letters on a card or as a standard chart.
- Allen picture test: Pictures of a car, house, and apple are presented on flip-over cards, which are viewed at 3 m or 6 m distance (Fig. 1.6).
In literate children, record the Snellen's visual acuity for distance as well as near for either eye. This is important to monitor amblyopia therapy as near visual acuity starts improving first than the distance. - Diagnosis of Amblyopia: This usually requires a 2-line difference of visual acuity between the two eyes but a smaller difference should not be ignored.Crowding phenomenon: This is a common characteristic of amblyopia, visual acuity is better for single optotypes rather than the whole line. This is particularly important in patient follow-up once occlusion therapy is instituted as visual acuity improvement for single letters starts earlier than the whole line.Grading of amblyopia: Severity of amblyopia must be graded for planning the management as duration of therapy and visual prognosis depends upon it.Grade 0: No fixation preference; fixation held with either eye on cover test—amblyopia not presents.Grade 1: Fixation held with either eye after removing the occluder and maintained through a blink but not after an ocular movement—mild amblyopia present.Grade 2: Fixation held briefly after removing the occluder and then switches to the other eye after a blink—mild to moderate amblyopia.Grade 3: Fixation held only for a few seconds after removing the occluder—moderate amblyopia.Grade 4: Fixation immediately shifts to the other eye after removing the occluder—dense amblyopia.
- Cover test, cover/Uncover and alternate cover tests:Principle: These tests are based on the principle of “Breaking Binocularity” and then noting how each eye behaves when covered or uncovered. They depend upon the patient's ability to fixate with either eye. It needs patient's attention and cooperation.They are performed for both near and distance fixation with the patient wearing the glasses. An occluder or the examiner's hand can cover the eye.Indications:
- To detect whether the patient is orthophoric or has a latent (phoria) or a manifest (tropia) strabismus.
- Prisms (Prism cover test) use them as a part of measuring total deviation.
- When patients are followed-up for their refractive correction, these tests are used to assess muscle balance; if a patient is wearing his hypermetropic correction and an exophoria is noted by an alternate cover test, the hypermetropic correction has to be reduced. However, if the child is developing an esophoria with his refractive correction, then the amount of plus correction has to be increased.
Similarly, if a patient wearing a myopic correction is noted to have an esophoria, his myopic correction has to be reduced. However, if he has an exophoria, the myopic correction should be increased.Cover Test (Fig. 1.7):It confirms the presence of a manifest strabismus (tropia).Although the patient fixates on a near target, the normal looking eye is covered and the behavior of the uncovered eye is noted as it takes up fixation. If that eye moves inwards, then and exotropia was present and if it moves outwards, then it was esotropic.The test is then performed for distant fixation and behavior of either eye is noted as one eye is covered alternately.If no movement of one eye occurs as the other eye is covered, then there is either no strabismus or the uncovered eye has dense amblyopia.Cover/Uncover Test: This detects a heterophoria (latent deviation). It is performed once cover test does not demonstrate a manifest deviation (Fig. 1.8).Method: While the patient fixates at a distant target, one eye is covered and the behavior of the eye under cover is noted as the cover is removed. If it moves to take up fixation, a heterophoria is present. The direction in which it moves is noted; if it moves outward, an exophoria is present and if it moves inward, an esophoria is present.Alternate Cover Test: This test detects the presence of an alternate or a unilateral deviation (Fig. 1.9).Method: In this test, occluder is placed in front of one eye for a few seconds to dissociate the two eyes while the patient fixates on the light in front of both eyes. While he is fixating, the cover is shifted quickly from one eye to the other to prevent fusion. The examiner should note the movement of the eye as cover is being moved from it to the opposite eye.If either eye moves when cover is removed to take up fixation, an alternate strabismus is present.However, if one eye stays straight and only the other eye moves to take up fixation, a unilateral strabismus is present. - Eccentric Fixation (Fig. 1.10):
- This can be diagnosed by holding a fixation light in the midline in front of the patient and ask him/her to fixate on it while the normal eye is covered; the reflection of light will not be centered.
- The exact site of eccentric fixation can be confirmed by looking through a visuoscope and asking the patient to fixate on the central spot. A visuoscope is a direct ophthalmoscope with a fixation target incorporated into the ophthalmoscope beam.
- The incidence of eccentric fixation is far higher in longstanding esotropia than exotropia.
- The visual acuity depends upon the site of eccentric fixation; the farther it is from the foveola, the lesser is the visual acuity in that eye.
- In the presence of eccentric fixation, full visual recovery by occlusion therapy should not be expected unless the fixation changes to the foveola.
- Refraction: First subjective and then cycloplegic refraction is performed. Usually the more myopic, hypermetropic or astigmatic eye has amblyopia.
- Examination of Pupillary Response to Light: Direct and consensual. Even in dense amblyopia, pupils react normally to light. An organic cause should be suspected if a relative afferent pupillary defect or bilaterally sluggish pupils are detected.A paradoxical response to light: Pupils constrict in the dark and dilate when light is switched on. This is seen in congenital stationary night blindness, cone dystrophy and Leber's congenital amaurosis.
- Color Vision: Presence of defective color vision indicates an organic cause for amblyopia.
- Full Ophthalmic Examination: Slit-lamp examination and fundoscopy to find any organic cause of amblyopia, which may need treating prior to specific amblyopia therapy.
- Imaging Studies: If an organic cause for decrease in visual acuity is suspected in the presence of a normal ophthalmic examination, then further investigation of the visual pathway is indicated, i.e. CT scan, MRI or fluorescein fundus angiography (FFA).
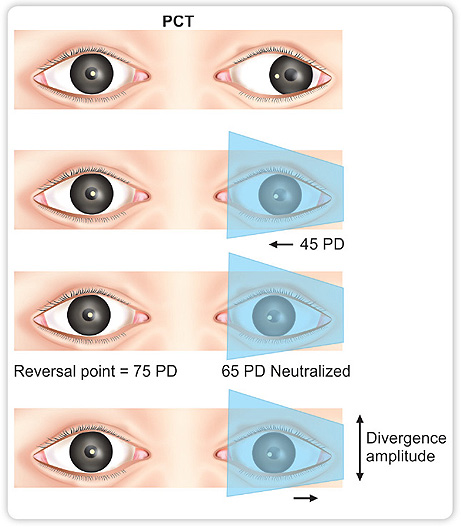
- Measurement of Ocular Deviation:Hirschberg's test: This is a rough estimate of the degree of deviation by comparing corneal reflections in both eyes as the patient fixates on a light source 33 cm away. 9If the light reflection is situated at the temporal border of an undilated pupil, the rough angle of strabismus is 15°; if it is at the limbus, then the angle of deviation is about 45° and in the middle of these two points, it is about 30° (Fig. 1.11).Advantages: It is an easy test and gives a quick estimate of the degree of strabismus. It can be performed easily in uncooperative patients.Disadvantages: It gives a rough measurement. Errors are introduced in a dilated pupil or in the presence of an angle Kappa; it is the angle between the visual axis and the anatomical axis of the eye. Fovea is normally situated temporal to the visual axis so light falling on the cornea will cause a reflection nasal to the center of cornea, hence causing a positive angle kappa. A large, positive angle kappa will give an erroneous impression of an exotropia. Similarly, a negative angle kappa will give a false impression of an esotropia.Krimsky test: In this text, prisms are placed in front of the deviated eye, with the apex of the prism in the direction of deviation, till the corneal light reflexes are symmetrical in both eyes. Its value is mainly in esotropia in children where it is difficult to maintain their fixation in order to perform a prism cover test (PCT).Prism cover test: This provides an accurate measurement of the total deviation (Phoria + Tropia). First a hand held prism of the rough estimate detected by the Hirschberg's test is placed in front of the deviating eye with its apex in the direction of deviation. The measurement is done first for near (33 cm) and then for far distance (>6 m). It should also be done for side-gaze, if possible (Fig. 1.12).For example, in exotropia, prism is placed in front of the deviating eye with its apex outwards. With the other eye fixing, alternate cover test is performed till no ocular movement occurs. This is called the Neutralization Point, (65 PD in above example).In exotropia, patients have a strong divergence, hence the strength of prisms is kept on increasing till a small movement of the eye in the opposite direction occurs, i.e. in exotropia, the point at which the eye starts to move outwards.10Fig. 1.13: Left exotropia. A 45 PD loose prism is placed in front of left eye with its apex pointing outwards; still inward movement of the left eye is noted on alternate cover test. The strength of prism is gradually increased to 65 PD at which no eye movement is detected on alternate cover test (Neutralization point). Then the strength of prisms is further increased till at 75 PD a reversed movement of left eye in outward direction is noted (Reversal Point)This is called the Reversal Point (Fig. 1.13). This point gives the measurement of divergence amplitude in a patient and varies from person to person. Its exact measurement is very important for proper management of exotropia surgically.
- Tests for Stereopsis: The two commonly used tests are Titmus and TNO.Titmus: This consists of two plates in the form of a booklet, which are viewed with poloroid glasses that should be worn over the patient's refractive glasses. The plates contain a three- dimensional picture of a fly or animals and are graded.TNO: This consists of seven plates that contain various shapes like squares, crosses created by random dots in complementary colors viewed with red and green glasses.
- Measurement of Amplitude of Convergence:Significance: Convergence may alter in different conditions presenting either as an insufficiency resulting in symptoms of asthenopia with headache, eye strain and sore eyes. This particularly occurs following prolonged close work in children resulting in an exophoria and diplopia.11Measurement:Near point of convergence: This is the closest point at which an object can be seen clearly. It is usually less than 8 mm. It is measured by a ruler placed at the outer canthus while a fixation target, a pencil, is brought towards the eyes. The point is noted where one eye begins to diverge.Far point of convergence: This is at infinity.Amplitude of convergence: This is measured by a prism bar. The test is performed for near at 33 cm with the patient fixating on a target. The prism bar, base-out is placed in front of one eye and the strength of prisms gradually increased. The eyes converge till a point is reached when the patient develops diplopia. This is called the Break Point.The prism power is gradually reduced till the diplopia disappears. This is called the Recovery Point. The difference between the break point and recovery point gives the amplitude of convergence.