‘You will easily recognize that there is hardly another part of the body which calls for higher qualification on the part of the operator as to anatomical knowledge than the temporal bone.’
Bezold
DEVELOPMENTAL ANATOMY
The embryological development of the ear is best understood by describing separately the individual development of the three major anatomical areas that comprise the ear, i.e. the development of the external ear, middle ear, and inner ear.
External Ear
Development of Pinna begins at 4 weeks when condensation of mandibular (1st branchial arch) and hyoid (2nd arch) arch occur. Hillocks of His in form of 6 ridges appear at the distal portion of first branchial groove (Fig. 1.1). Rudimentary Pinna forms by 60 days. Adult configuration is achieved by 5th month, irrespective of developmental progress in middle ear and inner ear. Darwinian tubercle makes its appearance by 6 month.
External Auditory Canal (EAC)
The external ear develops from the upper portion of the first external pharyngeal groove and becomes an area of highly modified skin. Comprising ectoderm, the cells in this area, termed the meatal plate, continue to divide until they come in contact with cells destined to form the middle ear structure. The cells at this junction will ultimately form the tympanic membrane.
Ectoderm of the groove briefly rest upon the endoderm of the tubotympanic recess (Ist Pharyngeal pouch) but during 6th week mesodermal ingrowth breaks this contact (Fig. 1.2). As development proceeds, the meatal plate thickens and becomes plug-like in form (the meatal plug). Eventually, during the 8th week a cavity forms within the meatal plug (primary EAC) corresponding to the fibrocartilaginous part in adults.
3Cords of the epithelial cells at the depth of the primary EAC grows medially into the mesenchyme to terminate in solid (meatal) plate. The mesenchyme medial to meatal plate gives rise to lamina propria (fibrous layer) of tympanic membrane. At 9th week, it is surrounded by four membranous bone ossification center of tympanic ring. At 10th week, tympanic ring segment fuse except superiorly where defect remains (Notch of Rivinus). These element then expand accompanied by growth of solid epithelial cells.
By 5th month, cord splits open and by 7th month bony EAC is formed. Cells remaining at the periphery forms epithelial lining of bony EAC while those medially forms superficial layer of tympanic membrane (TM). Medial layer of the TM is derived from epithelial lining of first pharyngeal pouch. Lateral extension of tympanic ring occurs postnatally.
Failure of maturation of 1st and 2nd branchial arch structure gives rise to following abnormalities:
- Failure of adequate skin migration with possible ear canal cholesteatoma
- Bat ear
- Accessary auricle, preauricular sinus
- Complete failure of formation of ear canal and middle ear
- First arch fistula (Collaural fistula).
Middle Ear
First pharyngeal pouch expands mainly due to rapid growth of surrounding mesenchyme. This along with contribution of endoderm of second pouch results in formation of Eustachian tube (ET), middle ear and mastoid antrum. The cells form a tubotympanic recess and ultimately form the Eustachian tubes 4and other middle ear structures, including the tympanic cavity. At about the end of the first month of development, the cells surrounding the tubotympanic recess form a primitive middle ear cavity. Eventually, the cells in this area are exposed to the otic capsule.
Endoderm of the slit like sac that is the precursor of middle ear lies against ectoderm of the first pharyngeal groove. Mesenchyme grows in between these two layers (ectoderm of pharyngeal groove and endoderm of pharyngeal pouch) to form future TM. Underlying sac expands and as it reaches developing ossicles, the epithelium is draped over these structure and their associated muscles, tendon and ligaments so that a complex series of mucosal fold develops.
Hypotympanum develops between 22 to 32 weeks as a tripartite bony amalgamation, i.e. tympanic bone, canalicular otic capsule and petrosal ledge. This variegated structure predisposes this area to anomalous development like dehiscent jugular bulb.
Ossicles and Muscles
- First arch (Meckel's or Mandibular) gives rise to malleus, incus and tensor tympani muscle, which is supplied by nerve of 1st arch, i.e. trigeminal nerve.
- Second arch gives rise to stapes suprastructure and stapedius muscle, which is supplied by 7th nerve, a nerve of 2nd arch (Reichert's arch or Hyoid arch).
- Medial surface of footplate and annular ligament develops from otic capsule.
- Adult shape, size and ossification of ossicles are achieved by 25 weeks.
Development of Tympanomastoid Compartment
- Tympanomastoid compartment appear at 3-week stage as an outpouching of the first pharyngeal pouch known as tubotympanic recess. Mastoid pneumatization is evident as early as 33 weeks.
- Factors like heredity, environment, nutrition, bacterial infection, adequacy of ventilation decides and influences pneumatization.
Inner Ear
Phylogenetically older semicircular canal and utricle (Pars superior) precedes development of saccule and cochlear duct (Pars inferior). Phylogenetic antiquity of pars superior is important in its resistance to developmental malformation.
Inner ear initially develops independently of the external and middle ear. Later on two become interconnected by the stapes. Suprastructure being attach to stapes footplate, thus giving continuity to auditory passage.
- Initial development of the generalized structure of membranous labyrinth.
- Period of encasement by the bony labyrinth.
- Production of series of spaces within this bony shell to produce perilymphatic spaces.
Development
The inner ear develops from a thickening of ectoderm near the hindbrain, termed the otic placode. The plate like placode forms an otic pit. When the pit is separated from the surface by further development of surrounding cells, an otic vesicle forms. The otic vesicle is surrounded with a layer of mesoderm to form an otic capsule.
Associated with the otocyst, is the cluster of neural crest cells that become separate Facial (geniculate), Auditory (spiral), Vestibular (Scarpa's) ganglion cell bodies.
Otocyst undergoes series of changes resulting in full-sized outline of adult membranous labyrinth by 25 weeks of gestation (Fig. 1.3).
Membranous Labyrinth
The otic capsule becomes contracted about its middle region to form upper and lower chambers. The upper area forms the utriculosaccular area, and the lower chamber the cochlear area. Semicircular canals develop in the utriculosaccular area. Specialized neural cells develop near ampullae that ultimately contribute to sensory feeling associated with balance. Ultimately, the utriculosaccular area divides into the utricle and saccule that remain connected by an utriculosaccular duct. The lower cochlear region of the otic capsule grows into the spiral shape throw a single pouch like process that grows and begins to coil from base to apex to reach its full two and half turn by 25 weeks.
Sensory cells of three cristae, two maculae and organ of Corti develops from ectodermal origin.
Organ of Corti begins to develop as a single block of heaped up ectodermal cell at about 11 weeks. In this mass, develops inner hair cells, outer hair cells and specialized supporting cells. Cluster of stereocilia and single kinocilium develops on each hair cell. The cochlear kinocilium regresses to leave adult configuration of stereocilia. Differentiation progresses from base to apex.
Bony Labyrinth
Mesenchyme enclosing otocyst becomes chondrified to form otic capsule. As the membranous labyrinth expands, otic capsule remodels and places undergo dedifferentiation to form fluid filled spaces that become perilymphatic space. Perilymphatic space becomes continuous with CSF through development of cochlear aqueduct that runs from posterior cranial fossa to base of cochlea.
Ossification of cartilaginous otic capsule begins in and around 16th weeks from variable number of centers (14) and finally fuses without leaving suture lines. This bone become petrous bone (Petra in Greek connotes Rock like).
ANATOMY OF THE EAR
External Ear
The external ear consists of the expanded portion named the auricle or pinna, and the external acoustic meatus that leads to the outer surface of the drum membrane. The former projects from the side of the head and serves to collect the vibrations of the air by which sound is produced; the latter leads inward from the bottom of the auricle and conducts the vibrations to the tympanic cavity (acoustic antenna of funnel).
Auricle or Pinna
The Auricle (Fig. 1.4) or Pinna presents numerous eminences and depressions. The prominent rim of the auricle is called the helix; where the helix turns downward behind, a small tubercle, the auricular tubercle of Darwin, is frequently seen. Another curved prominence, parallel with and in front of the helix, is called the antihelix; this divides above into two crura, between which is a triangular depression, the fossa triangularis. The narrow-curved depression between the helix and the antihelix is called the scapha. The antihelix describes a curve around a deep, capacious cavity, the concha, which is partially divided into two parts by the crus or commencement of the helix; the upper part is termed the cymba conchae, the lower part the cavum conchae.
In front of the concha, and projecting backward over the meatus, is a small pointed eminence, the tragus, so called from its being generally covered on its under surface with a tuft of hair, resembling a goat's beard. Opposite the tragus, and separated from it by the intertragic notch, is a small tubercle, the antitragus. Below this is the lobule, composed of tough areolar and adipose tissues, and wanting the firmness and elasticity of the rest of the auricle.
Body of the auricle is made up of thin corrugated, continuous sheet of yellow elastic cartilage covered by perichondrium and skin. The auricle is attached to the head by ligaments and anterior, superior and posterior auricular muscles. This cartilage extends about 8 mm down the ear canal to form its lateral one-third of EAC. There is a narrow hiatus between tragus and anterior crus of helix, deficiency utilized surgically for giving endaural incision.
10Cartilage is avascular and derives its blood supply from perichondrium. Skin along with perichondrium is very tightly adherent to lateral surface of pinna. Absence of subcutaneous layer between skin and cartilage anteriorly makes the auricle susceptible to frost bite despite rich supply of superficial vessels. This is also the reason why inflammatory lesions of pinna are very painful. Skin is covered with fine hairs, which are more on the concha and scaphoid fossa. Sebaceous gland openings are present in the root canal of these hairs.
On the posterior surface of auricle, distinct subcutaneous tissue is present. Skin here is loose and rich in sebaceous glands making it frequent site for sebaceous cyst. Lax skin on the posterior surface of auricle makes it a preferred site for obtaining full thickness skin graft for reconstructing small skin defects. Anterior, superior and posterior muscles, which attach auricle to skull are variably developed and when well developed, are capable of moving pinna. They are supplied by posterior auricular nerve, a branch of facial nerve.
Arterial Supply
Superficial temporal and posterior auricular branch of external carotid artery.
Lymphatics
Anterior, posterior and inferior auricular nodes.
Nerve Supply
- Branches of 5th, 9th and 10th cranial nerve provides sensory innervation
- Lesser occipital nerve (C2) supplies medial surface (upper portion)
- Greater auricular nerve (C2, 3) supplies medial side of the auricle
- Lateral surface is supplied by greater auricular nerve and 5th cranial nerve (Auriculotemporal nerve)
- Auricular branch of vagus supplies small portion of EAC.
External Auditory Canal
Elliptical in cross section, EAC in adult is approximately 25 mm long with lateral one-third having cartilage wall and medial two-third, osseous. Anterior and inferior walls are longer than the posterior and superior wall due to obliquity of tympanic membrane (shorter posterosuperior wall is 25 mm and longer anteroinferior wall is 31 mm long). Diameter of EAC varies between individuals and in different races. The volume of the external auditory canal is about 0.85 mL.
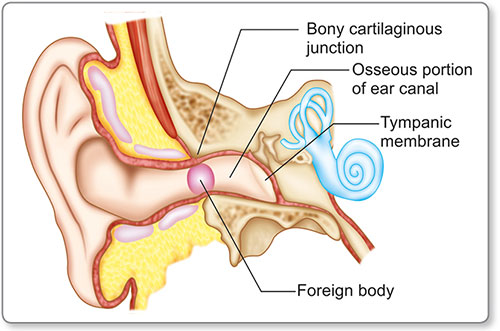
Outer part or lateral cartilaginous part, which is continuous with the auricle while inner, medial and bony parts end at the tympanic membrane. The canal has an ‘S’ shaped configuration with the direction of the cartilaginous canal being upward and backward while bony canal runs downward and forward. The cartilaginous canal can be straightened by pulling the pinna posterosuperiorly enabling better visualization of the ear drum. The narrowest portion of the external canal is at the bony cartilaginous junction (Fig. 1.5). This junction creates a narrow isthmus allowing for impaction of foreign bodies.
The bony canal is composed of a complete cylinder of bone where the anterior and inferior walls are composed of the tympanic portion of the temporal bone and the superior and posterior walls are formed by the squamous and mastoid portions of the temporal bone. Two suture lines are hence visualized; the tympanomastoid suture and the tympanosquamous suture.
Curvature of deep bony canal results in acute angle between drum and anterior canal wall. This is called anterior recess. At the junction of inferior wall with tympanic membrane, a depression exists which is called inferior meatal recess. This area is difficult to inspect, hence discharge, debris and tiny foreign bodies (FB) may go unnoticed. The condyle of the mandible and glenoid fossa also produce a convexity in the anterior bony canal wall limiting the visualization of the ear drum and predispose foreign body entrapment in the anteroinferior portion of the medial end of the external canal.
External canal is lined by skin, which is thin in osseous part and thick and adherent in cartilaginous part. Sebaceous, ceruminous glands and hair follicle are present only in cartilaginous part. Deficiency in the anterior cartilaginous wall is called fissure of Santorini from where infection can travel from meatus to parotid and vice versa.
Contrary to the rest of the skin of the body, oblique and outward growth of epidermis of canal skin and pars flaccida is seen so that surface layer effectively migrates towards opening of canal. Though variable and influenced by many factors, the normal rate of migration is 0.05 mm per day
Ceruminous Glands
They are modified apocrine glands that open into the root canal of hair follicles and produces watery white secretion (Cerumen) that slowly darkens turning semisolid and sticky as it dries. Since they are modified sweat gland, they respond to many stimuli like adrenergic drugs, fever, emotion and mechanical stimulation, which can all produce increased or altered secretion of wax.
Sebaceous Glands
Sebaceous gland produce oily secretion (Sebum) from the breakdown of fat containing cells, which is excreted into root 13canal of hair follicle. The mixture of desquamated cells, cerumen and sebum forms wax which is antifungal, antibacterial and bactericidal. Wax is not usually found in deep ear canal. Thus, wax overlying upper portion of TM (Pars flaccida or attic region) is rarely true wax but associated with underlying cholesteatoma. Therefore, it has been aptly said “Beware of attic wax”.
Blood Supply of External Canal
It laterally supplied by the post-auricular and superficial temporal arteries. Medially it is supplied by deep auricular artery, which is a branch of first portion of the internal maxillary artery. This deep auricular artery supplies the tympanic vascular ring. Veins from the external canal drain into the superficial temporal and post-auricular veins. The post-auricular vein connects to the sigmoid sinus via the mastoid emissary vein, this anastomosis provide a route for infections of the external ear to spread to the intracranial cavity.
Lymphatics
They generally follow the veins and drain into the parotid group of nodes.
Sensory Innervation
Auriculotemporal branch of the mandibular nerve innervates the anterior portion of the pinna, tragus, and the anterior wall of the external canal.
The well of the concha and the posterior wall of the external canal receive innervation from the 7th, 9th and 10th cranial nerves.
This complex innervation of the external canal accounts for several clinical findings involving the external canal, i.e. vesicular eruption in the skin of the external canal with facial palsy is caused by herpetic infection of the geniculate ganglion known as the Ramsay Hunt syndrome. Hyperesthesia of the concha and external canal caused by facial nerve compression from cerebellopontine angle tumors is known as Hitselberger's sign. Instrumentation of the external canal can cause nausea or coughing through stimulation of the vagus nerve via the Arnold's nerve.
Tympanic Membrane
Tympanic membrane (Fig. 1.6) forms the medial wall of external ear and most of the lateral wall of middle ear cavity. Drum head or tympanic membrane, which is semi-transparent and pearly gray in color, is an oval with 9–10 mm being its maximum diameter from posterosuperior to anteroinferior quadrant. It lies obliquely along the long axis of EAC and form an acute angle of 55° with floor of EAC. The peripheral most part of TM gets thickened into a fibrous structure called annulus, which fits into tympanic sulcus (annulus and sulcus is deficient superiorly, bridged by squamous temporal bone. Thickness of TM is 0.074 mm, which is thickest (0.09 mm) near annulus inferiorly and anterosuperiorly and thinnest in posterosuperior quadrant.
Tympanic membrane is divided into pars tensa and pars flaccida by anterior and posterior malleolar folds. Area occupied by the pars tensa, where sulcus is absent is called notch of Rivinus. Overall, TM is concave toward EAC and most concave point is umbo where the tip of the handle of malleus lies. From umbo, triangular bright area, the cone of light emerges and travels downward and forward. Above the pars flaccida, there is bony deep canal wall. This wall is wedge shaped with a sharp inferior edge (like a crescent) known as the outer attic wall or scutum of Leidy (outer epitympanic wall or scutum—in Latin means shield). Scutum along with the pars flaccida forms lateral wall of epitympanum or attic.
Tympanic membrane has three layers
- Outer epithelial layer (continuous with the skin of EAC):Epithelial migration occurs at the rate of 0.05 mm per day in the centrifugal manner.
- Middle fibrous (lamina propria):This has outer radial fibers and deeper transverse, parabolic and circular fibers.Pars flaccida has less marked fibrous layer than pars tensa.
- Inner mucosal layer (continuous with the lining of middle ear cleft).
Blood Supply of Tympanic Membrane (Fig. 1.7)
Laterally: Tympanic branch of deep auricular artery.
Medially: Tympanic branch of internal maxillary artery, stylomastoid branch of posterior auricular artery.
Nerve supply: Supplied by branches of 5th, 7th and 10th cranial nerve.
Middle Ear (Tympanic Cavity)
Middle ear is a six-sided box (Fig. 1.8) akin to a matchbox with a roof, floor, medial, lateral, anterior and posterior walls. It has vertical and anteroposterior dimensions of 15 mm with variable mediolateral dimension, superiorly being 6 mm and at umbo 2 mm. It contains air, ossicles, tendons and ligaments. The air it contains is carried to it from the nasal part of the pharynx through the auditory tube. The ossicles connect its lateral to medial wall, and serve to convey the vibrations from the tympanic membrane across the cavity to the inner ear. Walls of the cavity have nerves running across them. The tympanic cavity also has openings into surrounding structures.
The tympanic cleft comprises of middle ear and its contents, the Eustachian tube, the aditus ad antrum and mastoid air cell system.
It is divided mainly into following compartments (Fig. 1.9).
Epitympanum
This is the space medial to the scutum or the lateral attic wall, which is limited superiorly by the tegmen plate, medially by the prominence of horizontal facial canal and ampullary end of lateral and superior semicircular canal, laterally by scutum and posteriorly this space communicates with antrum via aditus ad antrum.
It contains the head of malleus and body of incus.
Ridge of bone (Cog of Sheehy) extends inferiorly from tegmen plate just anterior to the head of malleus dividing epitympanum in anterior epitympanic and posterior epitympanic space. Cog lies immediately superior to and slightly posterior to processus cochleariformis. Anterior epitympanic space is also called supratubal recess. Communication of epitympanum and mesotympanum is blocked by ossicles and mucosal folds except three air pathways.
Protympanum
It contains opening of bony part of Eustachian tube lying inferior to the canal for tensor tympani. Internal carotid artery, which passes medial and inferior to bony ET, forms medial wall of protympanum.
Mesotympanum
This part of middle ear lies immediately medial to pars tensa, of the tympanic membrane. Important structures in the mesotympanum are promontory, oval window and round window. Jacobson's nerve (tympanic branch of glossopharyngeal nerve) is a constant landmark of promontory. This nerve originates at the junction of the floor and the medial wall of the middle ear through a small opening that allows 18the entry of tympanic branch to pass into the middle ear. It then runs over the promontory to divide in branches near cochleariformis process to form the tympanic plexus. Main Branch passes under the cochleariformis process to supply attic area. Inferior tympanic artery, a branch of ascending pharyngeal artery accompanies Jacobson's nerve.
Posterior Tympanum
Posterior tympanum is the posterior extension of mesotympanum and divided into four sinuses in relation to second genu, vertical segment of facial nerve and pyramidalis process.
- Facial recess: Superior to processus pyramidalis, lateral to vertical segment of facial nerve and medial to chorda tympani.
- Lateral sinus recess: Inferior to processus pyramidalis, lateral to vertical segment of facial nerve and medial to annulus.
- Posterior tympanic sinus: Medial to facial nerve and pyramidalis process and superior to ponticulus (Ridge of bone extending from promontory to pyramidalis process)
- Sinus tympani: Medial to facial nerve, inferior to ponticulus and superior to subiculum (Ridge of bone extending from tip of the round window to styloid eminence).
- Posterior tympanum is one of the inaccessible sites from where removal of cholesteatoma is difficult.
Hypotympanum
It usually consists of group of air cells inferior to labyrinth and extending anterior to the cochlea. It also contains the jugular bulb posteriorly and ICA anteriorly in its medial wall. Jugular bulb and ICA are separated by thin plate of bone called jugulocarotid crest or Crotch. Dehiscence of this bone is radiologically known as Phelp's sign diagnostic of glomus jugulare. Jugular bulb is usually covered by a thin bone, which may be dehiscent, and jugular bulb may be seen in middle ear sometimes as high as the round window thus vulnerable to injury in middle ear surgery.
Walls of Middle Ear
Medial Wall
It assumes surgical importance with many vital structures crowding together on this wall (Fig. 1.10).
Promontory
It is the most prominent structure formed by the basal turn of cochlea. Coursing almost vertically over promontory is the groove for tympanic (Jacobson's) branch of glossopharyngeal nerve. Posterior to promontory this wall is divided into three depressions by two bony structures called subiculum and ponticulus.
Oval Window Niche and Oval Window
This is 3.25 mm long and 1.75 mm wide and during life is covered by footplate of stapes. Deep to stapes footplate is perilymph-filling vestibule. Oval window is situated below the facial nerve and above the promontory.
Round Window Niche
This bony overhanging obscures round window membrane also known as the secondary tympanic membrane.
Triangular in shape, the plane lies at the right angle to plane of stapes footplate facing posteroinferiorly. Its dimensions are 2.3 mm long and 1.9 mm wide. Deep to round window is perilymph of scala tympani. The round window membrane is not at the end of scala tympani but forms part of its floor.
The nerve supplying the ampulla of the posterior semicircular canal (singular nerve) lies close to this secondary tympanic membrane. The secondary tympanic membrane forms a landmark for the position of the singular nerve. This is useful during surgical procedures like singular neurectomy for treatment of intractable vertigo.
Posterior to these windows is the posterior extension of mesotympanum medial to facial nerve. This space called sinus tympani is characterized by:
- Its inaccessible nature (surgically).
- Variable extent.
- Occasional communication with mastoid air cells.
- Cholesteatoma here is extremely difficult to eradicate.
Small mirrors known as the zinne mirror can be used to visualize this area indirectly and to prevent residual cholesteatoma lurking behind during mastoid surgeries.
Facial nerve: It runs across the medial wall separating epitympanic region from the mesotympanum. At geniculate ganglion facial nerve is marked by processus cochleariformis which is important landmark rarely eroded by disease. Microdehiscences in the horizontal part may be seen. When bone is thin and exposed by disease, two or three straight blood vessels are seen. These are the only straight blood vessels in middle ear indicating facial nerve is close by. Posterior to facial nerve is lateral SCC.
Processus cochleariformis: Rarely violated by disease it is an important landmark for ear surgery in general and for facial nerve in particular. The anterior end of the facial nerve canal is marked by this curved projection of bone and it houses the tendon of the tensor tympani muscle as it turns laterally to the handle of the malleus.
Lateral Wall
The lateral wall of the tympanum/middle ear is partly bony and partly membranous (Fig. 1.11). The central portion of the lateral wall is formed by the tympanic membrane, while above and below the tympanic membrane there is bone, forming the outer lateral walls of the epitympanum (attic) and hypotympanum respectively. The lateral wall of the epitympanum (attic) also includes that part of the tympanic membrane lying above the anterior and posterior malleolar folds—pars flaccida.
Petrotympanic Fissure and Canal of Hugier
Zygomatic process projects from lower part of squama and with the squama and tympanic bone helps forming mandibular fossa. Suture line runs though the fossa, the petrotympanic fissure (Glasserian fissure) that leads to middle ear and transmits tympanic branch of internal maxillary artery. Canal separated slightely from the fissure the canal of Hugier transmits the chorda tympani nerve.
Anterior Wall
Anterior wall is narrow and mainly comprises of (Fig. 1.12):
- Semicanal for tensor tympani
- Below the semicanal is opening of ET
- Medial to both the structure is carotid artery as it changes from its vertical to horizontal course through temporal bone.
Posterior Wall (Fig. 1.13)
Posterior wall in its upper part has an opening into the mastoid antrum. This opening is called aditus. This connects antrum with epitympanum.
Below this opening is a depression called fossa incudis that engages short process of incus.
Below the fossa incudis is small outgrowth of bone from posterior wall called pyramid (pyramidal eminence). This is housed stapedial muscle and tendon.
Facial recess is a groove between pyramid superiorly, facial nerve medially and annulus tympanicus laterally.
Sinus tympani lies deep to pyramid and facial nerve and continues into medial wall of middle ear.
Roof
It is formed by thin plate of bone, called tegmen tympani that separates middle ear from middle cranial fossa. It is formed by petrous part and squamous part of temporal bone. Patent petrosquamous suture acts as preformed pathway for spread of infection in children. Along with roof of middle ear, it also forms roof of mastoid antrum called tegmen antrum or tegmen mastoided.
Floor
Floor is formed by bony plate covering jugular bulb and also by bony plate covering internal carotid artery. Floor separates hypotympanic recess from internal carotid artery anteroinferiorly and jugular bulb posteroinferiorly. It is thin and sometimes dehiscent exposing dome of jugular bulb. Tympanic branch of glossopharyngeal nerve enters middle ear cavity through floor.
Contents of Middle Ear
Ossicles
The condensed interbranchial mesenchymal bridge consisting of both first and second branchial arch elements, through cartilage differentiation gives rise to primordial malleus and incus. All of the stapes except footplate develops from hyoid (second) arch. Footplate develops from otic capsule. Development of bone from cartilage model is called endochondral bone development, which has poor reparative capacity after trauma.
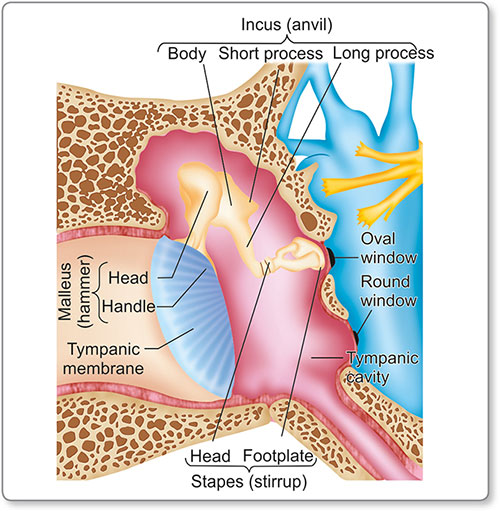
Suspended and partly rigid ossicular chain consists of malleus, incus and stapes (Table 1.1). They are held together by articulation and suspended in middle ear by mucosal folds and ligament (Fig. 1.14).
Additional support is provided by tensor tympani and stapedius muscle. Ligaments that support ossicular chain consist of superior, anterior and lateral malleolar ligament and superior and posterior incudal ligament. Annular ligament articulate stapes with the oval window.
Malleus: Handle of malleus (HOM) lies between middle and mucosal layer of tympanic membrane, which runs downwards, medially and backwards. Although HOM is very closely attached to the membrane at its lower end, there is a fine web of mucosa separating membrane from HOM in upper portion before its get adherent again at the lateral process. This slit like space can be opened surgically.
Lateral process: It is one of the prominent landmark of TM (Fig. 1.15). Deep to this on the medial surface, between neck of malleus above and insertion of tendon of tensor tympani below runs chorda tympani nerve.
Neck of malleus connects handle with head. Head of malleus lies in attic and suspended by superior malleolar ligament from tegmen tympani.
Tip of malleus tends to retract the handle of the malleus into middle ear cavity. Head of the malleus connect with the body of incus by synovial joint.
Incus: Body of incus lies in attic and has two processes projecting from it (Fig. 1.16). Short process runs posteriorly and engages with fossa incudis on the posterior wall of middle ear where a short ligament holds it firmly. Long process descends from attic into mesotympanum posterior to handle of malleus. At the tip of the long process of incus, it has a medially projecting structure called lenticular process. This lenticular process is called fourth ossicle because of its incomplete fusion with tip of long process thus giving appearance of separate bone or sesamoid bone. Lenticular process articulates with head of stapes and is most susceptible to avascular necrosis followed by the short process.
Stapes: The joint between head of stapes and lenticular process of incus is lined by cartilage that provides a plane of cleavage between the two. Of the two crura, anterior is thin and less curved (Fig. 1.17). Both the crura are hollowed out in 27their concave surface. This hollowing gives it twin qualities of strength and lightness. Footplate is 3 mm long and 1.4 mm wide. Its superior margin is convex with a flat inferior margin. Stapedius tendon inserts on the posterior part of neck. Stapes footplate closes oval window and is attached to bony margins of the window by annular ligament.
Oval window is at the bottom of the niche and is surrpounded by facial nerve above, processus cochleariformis in front, promontory below and pyramid of stapedial muscle behind.
Ligaments that suspend ossicles include (Fig. 1.18):
- Superior malleolar and incudal ligament (adhering head of malleus and body of incus to tegmen).
- Posterior incudal ligament (cementing short process to fossa incudis).
- Anterior malleolar ligament (fixing anterior process of malleus to anterior tympanic wall).
Muscles
Tensor tympani: It is 22 mm long muscle that arises from its own semicanal, above ET and partly from greater wing of sphenoid.
The muscle runs backward into tympanic cavity on its medial wall just below the level of facial nerve. At the level of the geniculate ganglion, the muscle gives way to a tendon, which is held in the bony prominence called processus cochleariformis. The tendon of tensor tympani then turns at a right angle to pass laterally to neck of malleus below chorda tympani. Supplied by the mandibular branch of the trigeminal nerve.
Stapedius: It arises from the bony vertical facial canal. Tendon traverses through pyramidalis process to be attached to neck of stapes. Receives nerve supply via nerve to stapedius, branch of facial nerve.
Mucous Membrane
Tympanic cavity is lined by mucous membrane that covers its wall and all its furniture. This continues anteriorly with mucosa of ET and posteriorly with tympanic antrum and mastoid air cell system. While covering various contents of middle ear like muscle, ligaments, ossicles, mucous membrane develops various folds forming various spaces like Prussak's space, anterior and posterior pouch of Von Troeltsch. These mucosal folds divide middle ear into definitive compartments and plays an important role in diseases like cholesteatoma.
Tympanic cavity is lined by mucosa having columnar pseudostratified cells in anteroinferior part, and towards posterosuperior part, it changes from low columnar epithelium to cuboidal epithelium. Attic region is lined by pavement epithelium.
Prussak's Space
This space is present above the lateral process of malleus. It is bounded laterally by pars flaccida, medially by neck of malleus and anteriorly, superiorly and posteriorly by lateral malleolar ligament. Posteriorly it communicates with the epitympanum and this is the first space to be occupied by growing cholesteatoma. Prussak's space is poorly ventilated.
Attic or Epitympanum
It is secluded from mesotympanum by the ossicles and its mucosal folds except few small but significant openings. These are the air pathways between epi and mesotympanum. Obstruction to these pathways is cause for various types of ear diseases.
Eustachian Tube
Also called as pharyngotympanic tube, it is an hourglass shaped tube with adult length of 36–37 mm (Fig. 1.19). It narrows down to isthmus, i.e. junction of osseous (lateral 1/3rd–12 mm) and cartilaginous (medial 2/3rd–24 mm) part. Diameter of isthmus is 1 mm and length is 2 mm.
Bony ET: Its length is 12 mm and comprises of a thin plate of bone that forms roof of ET above, which lies tensor tympani muscle. The carotid artery that lies medially is separated from ET by thin plate of bone.
Cartilage of the ET is mainly elastic except at isthmus where it is hyaline. Most of the posteromedial wall and roof is formed by cartilaginous plate whereas anterolateral wall is formed by muscle sheet and mucosa.
Tube opens into the nasopharynx behind and below posterior end of inferior turbinate. Surrounding the pharyngeal orifice is a ring of lymphoid tissue (Tubal tonsil of Gerlach).
There are two muscles acting on the ET—1. Tensor palate 2. Levator palati.
Tensor palati: This muscle arises from scaphoid fossa (bone) and along the whole length of upper rim of cartilage. Muscle converge into a short tendon that turn around a hook of hamulus (pterygoid plate) and spreads out within soft palate to join corresponding muscle from opposite side.
Levator palati: It is believed that on swallowing the tensor palate muscle contribute to opening of cartilaginous part of ET whereas levator palati, which has slower response may contribute to middle ear ventilation and elastic recoil responsible for keeping the orifice close.
Lining of ET: Bony part is lined by low columnar ciliated epithelium while lining of cartilaginous part is ciliated pseudostratified columnar epithelium. Near pharyngeal orifice are found goblet cells and tubuloacinar glands.
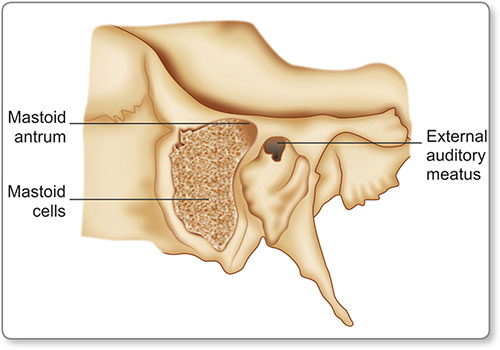
Mastoid Air Cell System
Air filled spaces in the mastoid bone communicate with middle ear. Mastoid antrum is the largest and most constant air cell (Fig. 1.20). It has a volume of 15–30 mL with dimensions of 4 × 7 × 9 mm. On the mastoid cortex, it is identified by suprameatal or MacEvan's triangle. Pneumatization pattern of mastoid air cells varies from highly sclerotic (only antrum is present) to extensively pneumatized (cellular) mastoid (Table 1.2). Diploic pattern has a mixture of cellular and sclerotic air cells. Majority (80%), however have pneumatized mastoid.
It is bounded by:
- Mastoid tip
- Retrofacial region
- Sinodural angle
- Petrous apex
- Arch of zygoma.
|
Blood Supply (Middle Ear)
It is derived from both internal and external carotid artery.
- Stylomastoid artery—a branch of posterior auricular artery supplies posterior part of tympanic membrane and cavity.
- Superficial petrosal artery—a branch of middle meningeal artery supplies facial nerve.
- Inferior tympanic artery—a branch of ascending pharyn-geal artery provides blood supply to mucosa of promontory and hypotympanum.
Nerve Supply to Middle Ear
- Tympanic plexus: It is formed by tympanic branch of glossopharyngeal nerve, i.e Jacobson's nerve and inferior and superior caroticotympanic nerves
- Chorda tympani nerve
- Supply to tensor tympani—5th cranial nerve
- Supply to stapedius—7th cranial nerve.
Course of Chorda Tympani
Chorda tympani enters middle ear just below posterior lip or tympanic sulcus (posterior canaliculus) and runs forward lateral to the long process of incus and then under the neck of malleus just above the attachment of tensor tympani tendon. It exit through petrotympanic fissure after running medial to the anterior malleolar ligament (anterior canaliculus).
Inner Ear Anatomy
The inner ear is the essential organ of hearing and balance, receiving the ultimate distribution of the vestibulocochlear nerve. It is called the labyrinth, from the complexity of its shape, and consists of two parts; the osseous labyrinth, a series of cavities within the petrous part of the temporal bone, and the membranous labyrinth, a series of communicating membranous sacs and ducts. The bony labyrinth contains Perilymph and within it lies the membranous labyrinth filled with Endolymph.
Bony Labyrinth
It is divided anatomically and functionally into three parts (Fig. 1.21).
- Vestibule
- Three semicircular canals
- Cochlea.
These are cavities hollowed out of the substance of the bone labyrinth, and lined by periosteum.
Vestibule
The vestibule is the central part of the osseous labyrinth. It is a flattened ovoid chamber lying between the middle ear and fundus of the internal auditory meatus, behind the cochlea, and in front of the semicircular canals. On its lateral or tympanic wall is the fenestra vestibuli, closed, in the fresh state, by the base of the stapes and annular ligament. Three recesses are found in the medial wall of vestibule:
- Spherical recess for macula of the saccule anteriorly.
- Elliptical recess for macula of the utricle posterosuperiorly.
- Cochlear recess situated between the spherical and elliptical recess carrying the cochlear nerve fibers to the base of cochlea.
Behind are the five orifices of the semicircular canals. Three semicircular canal arises from recesses in the posterior wall of 35vestibule and return to it each forming about two-third of circle. In front is an elliptical opening, which communicates with the scala vestibuli of the cochlea.
Below the elliptical recess, there is an opening for aqueduct of vestibule that transmits endolymphatic duct. The vestibular aqueduct passes through the temporal bone to open in the posterior cranial fossa between bone and dura. Endolymphatic duct passes through this to endolymphatic sac.
Semicircular Canal (SCC)
The bony semicircular canals are three in number, superior, posterior, and lateral, and are situated above and behind the vestibule forming most of its posterior segment. Each measures about 0.8 mm in diameter, and presents a dilatation at one end, called the ampulla, which contains the vestibular sensory epithelium and opens into the vestibule.
Ampulla of superior and lateral SCC are located at anterosuperior aspect of vestibule and that of the posterior canal lies posteriorly near the floor of the vestibule. The non-ampullated ends of the superior and posterior canals meet and join to form the crus commune that enters the vestibule in the middle of its posterior wall. Non-ampullated end of the lateral canal opens just below the crus commune. Crus commune is also the most medial part of the semicircular canal system.
Five openings of bony SCC into vestibule are summarized as;
- Ampullary end of lateral SCC
- Ampullary end of superior SCC
- Ampullary end of posterior SCC
- Non-ampullary end of lateral SCC
- Common non ampullary end of posterior and superior SCC–Crus Commune.
Each canal lies at right angle to one another. In the two ears, the lateral canals lie in the same plane, i.e. 30 degrees to the horizontal in standing position. The other canals are at right angles so that the superior and posterior canals of one ear are parallel with the posterior and superior canals of other ear respectively.
Lateral canal, shortest of the canal, though alternatively called horizontal SCC is situated at an angle of 30 degree to 36horizontal. Lateral canal is intimately related to the horizontal portion of the facial nerve. Labyrinthine fistula due to cholesteatoma most commonly affects lateral SCC while congenital dehiscence is commonly seen in superior SCC.
Cochlea
Situated anteroinferiorly to vestibule, bony cochlea is like a coiled shell, which makes two and half turns around central axis called modiolus, which is the conduit for vessles and cochlear nerve. It points laterally and forward, tapering from a wide base to a narrow apex. Base of cochlea is 9 mm while height is 5 mm. Basal coil forms the bulge of the promontory on the medial wall of the tympanic cavity. Inside, the cochlea has a spiral structure, which is partly bony and partly membranous, the latter being called the cochlear duct or scala media.
The bony spiral lamina, arising from the modiolus is a thin shelf of bone that spirals up within the lumen of the cochlea. From its edge, arises the membranous spiral lamina that meets the outer wall of the cochlea.
Hence, each coil of the cochlea is divided into three compartments (Fig. 1.22):
- Scala vestibule (contains perilymph)
- Scala media (cochlear duct – part of membranous labyrinth containing endolymph)
- Scala tympani (contains perilymph).
At the apex of the cochlea, a communication exists between scala vestibule and scala tympani, which is called Helicotrema. Scala media contains sensory cells of hearing.
The Scala Vestibuli opens into the vestibule at the cochlear base with the oval window (fenestra vestibule) and stapes footplate nearby. The Scala tympani is a blindly ended tube, but has the round window (fenestra cochlea) in its floor closed by the secondary tympanic membrane. The cochlear aqueduct also arises from the basal end of the scala tympani to the subarachnoid space of the posterior cranial fossa. This creates the potential pathway for spread of infection between the labyrinth and the meninges.
Membranous Labyrinth
The membranous labyrinth is lodged within the bony cavities just described, and has the same general form as these; it is, however, considerably smaller, and is partly separated from the bony walls by the perilymph. The membranous labyrinth contains endolymph.
It consists of (Fig. 1.23):
- Cochlear duct
- Saccule and utricle
- Semicircular duct
- Endolymphatic duct and sac.
Cochlear Duct
The ductus cochlearis consists of a spirally arranged tube enclosed in the two and half turns of the bony canal of the cochlea. Cochlear duct is triangular in section extending from a wide base to a narrow apex to end as blind pouch (Cupular Cecum at apex). It averages a length of 35 mm with the range of 29–40 mm.
The three walls comprise of (Fig. 1.24):
- Floor is formed by the bony spiral lamina and basilar membrane,
- Lateral wall by striae vascularis and
- Sloping roof, which is formed by Reissner's membrane.
Floor of the Cochlear Duct
Spiral lamina of cochlea runs around a central bony core like a thread of a screw. The bony spiral lamina separates into two ridges—the upper ridge is the spiral limbus giving rise to the tectorial membrane, the lower ridge gives rise to the membranous spiral lamina (Basilar membrane), which houses the Organ of Corti (sense organ of hearing). The acoustic nerve fibers run through it via the Habenular perforators to reach the sensory hair cells of the Organ of Corti. The membranous spiral lamina is separated from the spiral limbus by the inner sulcus and from the outer wall by the outer sulcus.
Organ of Corti (Fig. 1.25) is band like structure situated on the basilar membrane containing the auditory sensory cells and supporting cells.
These sensory cells are arranged in two distinct groups as inner and outer hair cells. They have hair like stereocilia projected from upper surface and therefore called hair cells.
Outer hair cell (OHC): They are around 12000 in number.
Inner hair cells are arranged in a single row while the outer hair cells are arranged in three, four or five irregular rows. Bodies of inner cells are flask shaped with long axis inclined towards the tunnel of Corti. Outer hair cells are cylindrical in shape with several rows of stereocilia arranged in w-shape at base, v-shape in middle and linear array at apex.
Between the inner and outer hair cells is a triangular space called tunnel of Corti containing cortilymph. Roof of the tunnel is formed by an arch of processes of the inner and outer hair cells. These processes are formed by microtubular elements and seems to give rigidity to overall structure.
Outer hair cells (OHC) contribute little to afferent innervation arising from the cochlea but have a good efferent supply coming from various tunnel crossing fibers that are derived from olivocochlear bundle. IHC are largely responsible for transmision of the afferent signals.
Between the rows of the outer hair cells are rows of supporting cells, called the cells of Deiters. Immediately to the outer side of Deiters’ cells are five or six rows of columnar cells, the supporting cells of Hensen. The columnar cells lying outside Hensen's cells are termed the cells of Claudius. A space exists between the outer rods of Corti and the adjacent hair cells; this is called the space of Nuel.
Stereocilia: Apical surface of OHC and IHC have stereocilia projecting from them into endolymph. The stereocilia are not true cilia with 9+ 2 pattern of microtubule. Very fine bands of adjacent stereocilia link each stereocilia bundle on one hair cell. The tip of the shorter stereocilia also has links to adjacent taller stereocilia and it is these links, which are thought to be responsible for opening ion channels during auditory stimulation.
Tectorial membrane: Arises from a lip or spiral limbus on the edge of the bony spiral lamina. It is a fibrogelatinous structure 41spreading across the organ of Corti and in life attaches to supporting cells that lie on the outer side of OHC. The tip of the longest stereocilia of OHC inserts a little way into the tectorial membrane but in well developed organ of Corti, inner hair cells do not touch tectorial membrane. This layer is extremely sensitive to distortion and shearing forces – lynchpin in auditory transmission.
Ductus reuniens: It passes backward from base of cochlear duct to saccule. It is believed that ductus reuniens, which has only microscopic lumen is probably incapable of transmitting fluid from cochlear duct posteriorly into saccule and utricle.
Striae Vascularis (Lateral wall)
This forms lateral wall of cochlear duct. It is highly vascular and consists of:
- Marginal endolymphatic layer
- Intermediate cell layer
- Basal cell layer.
Marginal endolymphatic layer is covered with microvilli and have tight junction between neighboring cells. This layer is metabolically very active. By its activity, striae vascularis maintains composition of endolymph, i.e. high concentration of potassium and positive endocochlear potential.
Cell group very similar to striae vascularis surrounds sensory cell region of saccule, utricle and ampulla of SCC. This collection of strial like tissue is called ‘dark cell region’ and maintains locally, the composition of endolymph in vestibular portion of labyrinth.
Reissner's Membrane (Roof)
It forms the roof of the cochlear duct separating Scala Media from Scala Tympani. Tight junctions preventing the mixing of endolymph and neurotoxic perilymph joined the cells.
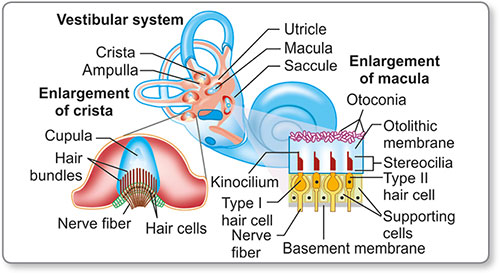
The Vestibular Labyrinth
It consists of a complex series of interconnecting membranous ducts and sacs that contain vestibular sensory epithelium. The sensory cells are present in utricle, saccule and semicircular canals.
Saccule
The saccule is the smaller of the two vestibular sacs; it is globular in form, and lies in the recessus sphericus near the opening of the scala vestibuli of the cochlea. Its anterior part exhibits an oval thickening, the macula that lies in the anterior wall positioned in vertical plane perpendicular to utricular macula. Orientation of hair cell is ‘comma’ shaped. From the posterior wall, the endolymphatic duct is given off; this duct is joined by the utriculosaccular duct, and then passes along the vestibular aqueduct and ends in the endolymphatic sac on the posterior surface of the petrous portion of the temporal bone, where it is in contact with the dura.
Utricle
The utricle, the larger of the two membranous sacs, is of an oblong form, compressed transversely, and occupies the posterosuperior part of the vestibule, lying in contact with the recessus ellipticus. Macula of utricle is situated in the lateral wall of utricle. Macula lies at the horizontal plane, i.e. at the right angle to that of macula of saccule. Macula of utricle is ‘spade‘ shaped.
The cavity of the utricle communicates behind with the semicircular ducts by five orifices. From its anterior wall is given off the ductus utriculosaccularis, which opens into the ductus endolymphaticus. There is a region running approximately along each macula in which the polarity of sensory cells changes abruptly through 180 degree. This region is called Striola (narrow zone dividing macula into two parts). Hair cells of utricular macula are aligned with kinocilium towards striola and hair cell of saccular macula are aligned with kinocilium away from striola.
Both macula contains:
- Sensory cells (Fig. 1.26)
- Supporting cells
From the upper surface of each type I hair cell arises clusters of stereocilia like cochlear hair cells but in addition there is single kinocilium, which is a true cilia (Table 1.3).
|
In case of cochlear hair cells kinocilium that is located on the outer edge of the group of stereocilia recedes as hair cell matures.
44Deflection of hair cell bundle in direction of kinocilium results in stimulation of hair cell and increased neural output whereas deflection in opposite direction results in inhibition. Afferent fibers that arise from type II cells are slightly smaller than those arising from type I cells.
Efferent fibers that supplies the type II cells have granulated button type nerve ending whereas efferent fibers to type I cells appear to end on afferent nerve chalice rather than cell body itself.
Semicircular Ducts
The semicircular ducts are about one-fourth of the diameter of the osseous canals, but in number, shape, and general form they are precisely similar, and each presents at one end an ampulla. They open by five orifices into the utricle. Utricle connects posteriorly with SCC and anteriorly via utricular duct with endolymphatic and saccular duct. Communication between utricle and utricular duct may be limited by utricular fold or valve (of Bast). Saccule communicates inferiorly via ductus reuniens with cochlear duct. At the junction of utricular and saccular duct, endolymphatic duct arises.
In the ampullae, the wall is thickened, and projects into the cavity as a fiddle-shaped, transversely placed elevation, the septum transversum, in which the nerves end. Ampulla of each semicircular canal contains saddle shaped ridge running along the long axis. This ridge is called cristae ampullaris. Each crista has type I, type II cells, and supporting cells.
Lateral semicircular canal: Kinocilium is on the utricular side of each hair cell. Deflection of kinocilium towards utricle (utriculopetal or ampullopetal) results in increased neural output.
Posterior and superior semicircular canal: Kinocilium is on the semicircular canal side of each sensory cell. Deflection of stereociliary bundle away from utricle (utriculofugal or ampullofugal) is required for stimulation.
Otoconial membrane and cupula (Fig. 1.27): Stereocilia of vestibular cell extends into endolymph and are partially embedded in highly specialized fibrogelatinous structure (similar to tectorial membrane in cochlear duct). In saccule and utricle, this structure is called otoconial membrane as it contains otoconia (calcium-based crystals, ear stone). Each otoconia is 30 μm long. In ampulla of SCC, this fibrogelatinous structure is called cupula and it sits on crista of SCC.
Endolymphatic Duct and Sac
Proximal endolymphatic duct is located within vestibular aqueduct and distal one third enveloped in dura adjacent to lateral venous sinus. Intermediate one third or rugose portion that lies partly in vestibular aqueduct and partly in folds of dura has highly differentiated epithelium having resorptive and phagocytic function (It possesses microvilli and pinocytic vesicle ruffled into papillae and crypts).
Blood Supply of Labyrinth
Innervation of Inner Ear
Afferent nerve fibers: These are around 30,000 in number arises from inner hair cells, pass into bony spiral lamina and modiolus. Sensory body of each nerve fiber is found in this region (unlike other sensory ganglion cells this is bipolar and unmyelinated). Acoustic nerve fibers loses its myelin sheath shortly before it enters cell body and again regain it as it passes further into the modiolus. Fibers pass into the acoustic nerve bundle in internal auditory meatus (IAM). Fibers from apex (low tone) lie in the center of the bundle whereas those from base (high tones) form outer layer. The nerve, like basilar membrane is said to have a tonotopic arrangement with different areas representing different frequencies.
Efferent fibers: Efferent fibers to cochlea leave brainstem in the superior vestibular nerve and travel with it in IAM where they cross to acoustic division by way of Ort's anastomosis.
Vestibular Nerve
Large myelinated fibers from type I and type II sensory cells pass into their respective part of the vestibular nerve:
- Utricle, crista of lateral and superior SCC—Superior vestibular nerve
- Saccule—Inferior vestibular nerve
- Posterior SCC—Singular nerve.
These three divisions all join within the IAM and at a variable distance along the canal can be found the vestibular ganglion (Scarpa's ganglion) that contain primitive bipolar cell bodies.