GROSS ANATOMY OF THE EXTRAOCULAR MUSCLES
The six extraocular muscles have names corresponding to their location and the direction they traverse to insert on the globe (Figs 1.1A to C). Four muscles follow a straight course from the apex of the orbit to the eye and are termed “rectus muscles”. Each rectus muscle inserts on the sclera of the eye in a position corresponding to its name, i.e. a superior, inferior, medial and lateral. Two “oblique muscles” also insert on the eye. The superior oblique muscle proceeds forward from the apex of the orbit to become tendinous just before passing through a fibrocartilaginous loop, the “trochlea”, attached to the trochlear fossa of the frontal bone. From here the tendon passes under the superior rectus muscle to insert posterior to the equator of the eye in the superolateral quadrant. The inferior oblique muscle arises from the anterior margin of the floor of the orbit, from the orbital surface of the maxilla, lateral to the nasolacrimal groove. It passes posteriorly, laterally and superiorly to insert posterior to the equator of the eye in the inferotemporal quadrant.
The rectus muscles average approximately 37 mm in length, with tendons 3 mm (medial rectus) to 7 mm (lateral rectus) long. The superior oblique muscle is approximately 40 mm in length and its tendon is 20 mm long. The inferior oblique is the shortest of the extraocular muscles, extending only 37 mm with no or a very short tendon of 1–2 mm. The width of the insertions of the rectus muscles averages 9–10 mm. The width of the insertions of the oblique muscles varies considerably, measuring 7–18 mm for the superior oblique and 5–14 mm for the inferior oblique.
The four rectus muscles arise from the apex of the orbit, along with the origins of the superior oblique muscle and the levator palpebrae (Fig. 1.2). The circular arrangement of their insertions around the optic canal and part of the superior orbital fissure is called the “annulus of Zinn”. The optic nerve and ophthalmic artery as well as the third and sixth cranial nerves pass through the annulus of Zinn into the cone-shaped space (the “muscle cone”) created by the bellies of the rectus muscles.
INNERVATION AND BLOOD SUPPLY TO THE EXTRAOCULAR MUSCLES
Three cranial nerves innervate all the intraocular and extraocular muscles of the eye (Figs 1.3A and B). The brainstem nuclei of these three cranial nerves are shown in Figure 1.3A, from the work of Warwick.
The third cranial nerve (CN III), or the “oculomotor nerve”, innervates the majority of the extraocular muscles and all the intraocular muscles of the eye. The nuclear complex of this nerve is located in the periaqueductal gray matter of the mesencephalon at the level of the superior colliculus. A single midline collection of cells innervates both levator palpebrae muscles. This is the only nucleus that bilaterally innervates extraocular muscles. The nucleus to the superior rectus muscle is the only nucleus in the third nerve complex that innervates a contralateral muscle. After leaving the brainstem, the fibers to the levator palpebrae and superior rectus muscles travel together as the “upper division” of the third cranial nerve (CN III1) (Fig. 1.3B). The medial rectus, the inferior rectus and the inferior oblique muscles are innervated by ipsilateral nuclei, and their fibers travel together as the lower division (CN III2).
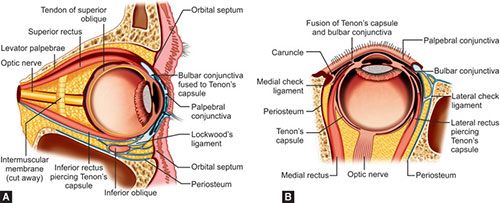
Figs 1.1A to C: The extraocular muscles as seen in: (A) Anterior view of the eye; (B) Lateral view of the eye; (C) Superior view of the eye.
The third cranial nerve also supplies parasympathetic innervations to the intraocular muscles of the eye via the “accessory” or “Edinger-Westphal” nucleus. Parasympathetic fibers travel with the nerve to the inferior oblique muscle, synapse in the “ciliary ganglion”, and enter the eye as the “short posterior ciliary nerves” (Fig. 1.3B). Both divisions of CN III pass through the annulus of Zinn into the muscle cone and innervate extraocular muscles from inside the muscle cone.
The· sixth cranial nerve (CN VI), or “abducens nerve”, innervates only the ipsilateral lateral rectus muscle. The fourth cranial nerve (CN IV), or “trochlear nerve”, innervates only the superior oblique muscle.
Fig. 1.2: Orbital nerves.Source: Figure modified from Warwick R. Eugene Wolff's Anatomy of the Eye and Orbit. Philadelphia: WB Saunders Co;1977.
Fig. 1.3A: Brainstem nuclei.Source: Figure modified from Grant JC: An Atlas of Anatomy. Baltimore: The Williams and Wilkins Co;1951.
This nerve differs from CN III and CN VI in not passing through the annulus of Zinn but rather innervating the superior oblique muscle from the orbital side. The fourth cranial nerve also differs by decussating and existing on the dorsal surface of the brainstem.
The “medial longitudinal fasciculus” (not shown) is a collection of fibers that interconnects these brainstem nuclei. The fasciculus passes medial to the abducens and lateral to the trochlear and oculomotor nuclei. The medial longitudinal fasciculus also connects these nuclei with the vestibular nuclei and is responsible for integrating conjugate movements of the eyes. A disruption of the fibers in this tract between CN VI and CN III results in a disconjugate movement of the eyes termed an “internuclear ophthalmoplegia” (see Chapter 13). In this disorder, there is a decreased ability of the ipsilateral eye to turn in on an attempted contralateral gaze.
The fifth cranial nerve (CN V), or “trigeminal nerve”, has only sensory branches in the orbit. The major branches from the first, or “ophthalmic, division” (CN V1) are the “frontal” and “nasociliary nerves”. The frontal nerve continues as the “supraorbital” and “supratrochlear nerves” to innervate the conjunctival and skin surfaces of the upper eyelid and forehead. The nasociliary nerve gives off two “long posterior ciliary nerves” subserving sensation to the eyeball and continues anteriorly to innervate the ethmoidal air cells and the anterolateral wall of the nose. From the second, or “maxillary, division” (CN V2) the “infraorbital nerve” subserves sensation to both surfaces of the lower eyelid and the skin overlaying the maxilla, the side of the nose, and the lips. It also supplies sensory fibers to the lacrimal gland via the “lacrimal nerve”. Parasympathetic lacrimal secretory fibers from the seventh cranial nerve (CN VII), or “facial nerve”, travel with the lacrimal nerve after synapsing in the pterygopalatine ganglion, to innervate the lacrimal gland.
The “ophthalmic artery” is the first major branch of the internal carotid artery (Fig. 1.3B). Within the optic canal, it lies inferolateral to the optic nerve, but on entering the orbit it crosses over or under the nerve and runs medially. The first important intraorbital branch is the “central retinal artery”, which enters the optic nerve about 12 mm behind the globe. As many as twenty “short posterior ciliary arteries” supplying the choroid and two “long posterior ciliary arteries” are also branches of the ophthalmic artery, as is the “lacrimal artery”.
Fig. 1.3B: Orbital nerves and vessels.Sources: Figure modified from Gray H, Lewis WH: Anatomy of the Human Body. Philadelphia: Lea & Febiger, 1918, and Grant JC: An Atlas of Anatomy. Baltimore: The Williams and Wilkins Co; 1951 and Bossy J. Atlas of Neuroanatomy and special sense organs. Philadelphia: WB Saunders Co; 1970.
Terminal branches of the ophthalmic artery include the “supraorbital”, “supratrochlear” and “ethmoidal arteries”. All the extraocular muscles are supplied by either the “lateral” or the “medial muscular branches” of the ophthalmic artery. From the branches supplying the rectus muscles arise the “anterior ciliary arteries”. The latter anastomose with the long posterior ciliary arteries to supply the anterior globe. Venous drainage mirrors arterial supply except the major veins are located superiorly and inferiorly.
ORBITAL AND FASCIAL RELATIONSHIPS
The “periosteum” of the orbit unites posteriorly with the dura mater and the sheath of the optic nerve and is loosely adherent to the bones except at the bony sutures and apertures of the orbit. At the margin of the orbit, it fuses with the “orbital septum”. The orbital septum attaches along the circumference of the orbit and covers the orbital surface of the base of the eyelids, separating the eyelids from the contents of the orbital cavity. In the upper eyelid, it fuses with the aponeurosis of the levator palpebrae superioris. At the medial and lateral corners of the eye, it attaches to the medial and lateral palpebral ligaments, respectively. Inferiorly, there is a similar relationship between the septum and the suspensory ligament of Lockwood (Figs 1.4 A and B).
“Tenon's capsule” is a smooth-surfaced elastic and fibrous tissue that envelops the globe and separates it from the orbital fat. It remains uncertain whether this capsule should be considered principally a socket, in which the eye rotates, or simply a fat barrier that moves with the globe. Tenon's capsule is perforated by the ciliary vessels and nerves, and fuses posteriorly with the optic nerve sheath. Anteriorly, it fuses with the bulbar conjunctiva to attach to the globe at the corneoscleral junction. The tendons of the extraocular muscles all must perforate Tenon's capsule to insert on the globe. At the site of penetration, the capsule fuses with the “muscle sheath”. Prior to and after penetrating Tenon's capsule, the sheaths of the four rectus muscles spread out to form an “intermuscular membrane”. Posterior to the globe the intermuscular membrane encases the muscle cone only for a short distance.
Additional fusions of the muscle sheaths are noteworthy. In the superior orbit, fusion of the sheaths of the superior rectus and levator muscles enhances their synergistic action. In the inferior orbit, the sheaths of the inferior rectus and inferior oblique fuse with each other and Tenon's capsule, forming a substantial band of fibrous tissue beneath the globe, which tapers upwardly to the medial and lateral rectus muscles. Because the latter have attachments to the orbital wall, it is thought that this suspension of fascia supports the globe like a hammock. This hammock-like band of tissue is called “Lockwood's ligament”, although precisely which tissues constitute Lockwood's ligament are difficult to define. Typically included in the definition are extensions anterior to the fused inferior rectus and oblique sheaths to the tarsal plate of the lower lid and the inferior orbital septum.
Figs 1.4A and B: Fascia of the eye. (A) Lateral view; (B) Superior view.Source: (A) Figure modified from Gray H, Lewis WH: Anatomy of the Human Body. Philadelphia: Lea & Febiger, 1918. (B) Figure modified from Deaver JB: Surgical Anatomy of the Head and Neck. Philadelphia: P. Blakiston's son & Co;1904.
Failure to separate these attachments during surgery of the inferior rectus can result in a change in the resting position of the lower lid.
Triangular extensions from the sheaths of the medial and lateral rectus muscles attach to the lacrimal and zygomatic bones, respectively. These expansions are strong and have been called “check ligaments”, although it remains uncertain whether they actually limit eye movements.
The function of the fascial system is to support the globe and to allow smooth excursions of the eye. Essential to the integrity of the system is the elastic tissue septum attached to Tenon's capsule and the immovable periorbita. Inflammation that can result from laceration of the periorbita or Tenon's capsule converts elastic tissue to inelastic, resulting in restriction of ocular movement. Laceration of Tenon's capsule, with prolapse of extraconal fat into the sub-Tenon's capsule space, and the attendant inflammatory response are serious complications of strabismus surgery. These complications can result from blunt or careless sharp dissection of the muscle capsule or from searching for a rectus muscle beyond 10 mm from the limbus.
TOPOGRAPHIC ANATOMY OF THE GLOBE
Anterior to the equator of the globe, the four rectus muscles gently curve toward the eye to insert on the sclera at varying distances from the limbus (Fig. 1.5). Because the nasal aspect of the globe is closest to the orbital apex, the medial rectus muscle does not wrap around the globe as much as the other rectus muscles. Furthermore, the insertions of the “rectus muscles” are not equidistant from the limbus. The medial rectus inserts closest to the limbus followed sequentially by the inferior, lateral and superior rectus muscles. If one were to draw a line connecting the insertions of the rectus muscles, starting from the medial rectus, a spiral, termed the “spiral of Tillaux”, would be formed. The insertions of the superior and inferior rectus muscles are curved slightly forward and obliquely. The nasal ends of their insertions are closer to the cornea than their temporal ends. The medial and lateral rectus muscles are more concentrically inserted.
Fig. 1.5: Anterior view of the eye.Source: Figure modified from Hogan MJ, Alvarado JA, Weddell JE. Histology of the Human Eye. Philadelphia: WB Saunders Co;1965.
Anterior to the rectus muscles, the “anterior ciliary arteries” emerge from the muscular branches of the ophthalmic artery. Two such arteries arise from each rectus muscle except for the lateral rectus muscle, from which there is only one.
The oblique muscles insert temporal to the vertical meridian of the eye, principally posterior to the equator (Figs 1.6 and 1.7). The obliquity of the insertion of the “superior oblique” causes the anterior edge to be closer to the limbus than the posterior edge. The anterior edge lies close to the temporal edge of the superior rectus. The “inferior oblique” muscle has either no tendon or a very short tendon.
Fig. 1.6: Superior view of the eye.Source: Figure modified from Hogan MJ, Alvarado JA, Weddell JE. Histology of the Human Eye. Philadelphia: WB Saunders Co;1965.
Fig. 1.7: Posterior view of the eye.Source: Figure modified from Hogan MJ, Alvarado JA, Weddell JE. Histology of the Human Eye. Philadelphia: WB Saunders Co;1965.
The medial border of its insertion lies close to the optic nerve and is about 2 mm below and temporal to the macula.
Posteriorly, about twenty “short posterior ciliary arteries” and eight “short posterior ciliary nerves” pierce the sclera around the optic nerve. Two “long posterior ciliary arteries” and “nerves” enter more distally along the horizontal meridian. Seven to eight “vortex veins” in each eye drain the venous system of the uveal tract. Their most common location is 3.0 mm posterior to the equator. Vortex veins exit on the temporal and medial aspects of the superior and inferior rectus muscles; these veins can be injured during surgery on the vertical recti or the oblique muscles.
BIBLIOGRAPHY
- Bossy J. Atlas of Neuroanatomy and special sense organs. WB Saunders Co; Philadelphia: 1970.
- Hogan MJ, Alvarado JA, weddell JE. Histology of the Human Eye. WB Saunders Co; Philadelphia: 1971.
- Warwick R. Eugene Wolff's Anatomy of the Eye and orbit. WB Saunders Co; Philadelphia: 1977.