- Anatomy and Physiology of the Ear
- Symptoms of the Ear Diseases
- Examination of the Ear
- Diseases of the Pinna
- Diseases of the External Auditory Canal
- Diseases of the Tympanic Membrane
- Diseases of the Eustachian Tube
- Nonpurulent Diseases of the Middle Ear
- Acute Suppurative Otitis Media
- Chronic Suppurative Otitis Media
- Complications of Otitis Media
- Otalgia
- Tumors of the Middle Ear Cleft
- Otosclerosis
- Conductive Hearing Loss
- Sensorineural Hearing Loss
- Vertigo
- Tinnitus
- Meniere's Disease
- Acoustic Neuroma
- Deaf Mutism
- Rehabilitation of Hearing Impaired
- Facial Nerve and Facial Palsy
Embryology of the Ear
- Pinna develops from six tubercles around the first branchial cleft. Time of development is given in Table 1.1.
- External auditory canal develops from the first branchial cleft.
- Tympanic membrane develops from all the three germinal layers. Outer epithelial layer is formed by the ectoderm, inner mucosal layer by the endoderm and the middle fibrous layer by the mesoderm.
- Middle ear cleft develops from the tubotympanic recess.
- The malleus and incus develop from the first branchial arch.
- Inner ear: The ectoderm in the region of hind brain thickens to form an auditory placode, which is invaginated to form auditory vesicle or the otocyst. It differentiates into the endolymphatic duct and sac, utricle, semicircular canals, saccule and cochlea.
External Ear
It consists of the pinna and external auditory canal.
Pinna (Auricle)
The pinna is formed by yellow elastic cartilage covered by the skin. There is no cartilage between the tragus and crus of the helix and this area is called the incisura terminalis. The lobule is also devoid of cartilage.
Clinical Importance
- Endural incision: It is made in incisura terminalis for the surgery of external auditory canal and middle ear. It does not cut through the auricular cartilage.
- Grafts in tympanoplasty: Tragal and conchal cartilage and perichondrium and fat from lobule are often used during tympanoplasty surgery.
- Frost bite: The outer surface of pinna is more prone to frost bite because the skin is adherent to the underlying perichondrium. There is no subcutaneous tissue.
- Sebaceous cysts: They are more common on medial surface of pinna.
External Auditory Canal
It is about 24 mm in length. The canal is S-haped. It extends from the bottom of the concha to the eardrum. The outer one-third (8 mm) is cartilaginous. The inner two-third portion (16 mm) of the canal is bony. In outer one-third, the skin is immediately adherent to the cartilage, hence the furuncle in this area are painful. The skin covering the cartilaginous canal is thick and contains ceruminous and pilosebaceous glands which secret wax. Hair is only present in outer one-third of the canal and therefore furuncles are seen only in the outer canal. The cartilaginous part of the canal has two deficiencies—the fissures of Santorini and through them the parotid or superficial mastoid infections can appear in the canal or vice versa.
The skin covering the bony part is thin and continuous over the tympanic membrane. About 6 mm lateral to tympanic membrane, the bony meatus has narrowing called isthmus. Foreign bodies lodged medial to the isthmus, get impacted and are difficult to remove. Anteroinferior part of the bony canal may present a deficiency called foramen of Huschke, in children up to the age of four or sometimes in adults which allow infection to and from the parotid.6
Tympanic Membrane (Eardrum/Drum Head)
It is situated between the external auditory canal and middle ear. It presents in oblique manner where its posterosuperior part is more lateral than its anteroinferior part. It is 9–10 mm tall, 8–9 mm wide and 0.1 mm thick. The tympanic membrane is divided into two parts—the pars tensa and pars flaccida (Shrapnel's membrane). The tympanic membrane is divided into four quadrant (Fig. 1.1).
The pars tensa forms major part of the tympanic membrane. Its periphery is thickened to form a fibrocartilaginous ring called the annulus tympanicus, which fits in the tympanic sulcus. The central part of the pars tensa is tented inwards at the level of the tip of malleus, called the Umbo. A bright cone of light can be seen radiating from the tip of malleus to the periphery in the anteroinferior quadrant (Figs 1.2 and 1.3). The pars flaccida is not so taut and appears slightly pinkish. Pars flaccida is situated above the lateral processus malleus between the notch of Rivinus and anterior and posterior malleal folds (Table 1.2).
The tympanic membrane consists of 3 layers: outer epithelial layer, inner mucosal layer and middle fibrous layer. The fibrous layer encloses the handle of malleus and has 3 types of fibers—the radial, circular and parabolic.
Middle Ear Cleft
The middle ear cleft consists of middle ear, Eustachian tube, aditus, antrum and mastoid air cells (Fig. 1.4).
The entire 7middle ear cleft is lined by the respiratory mucous membrane, which is an extension of the mucosa of the nasopharynx.
|
Middle Ear (Tympanic Cavity)
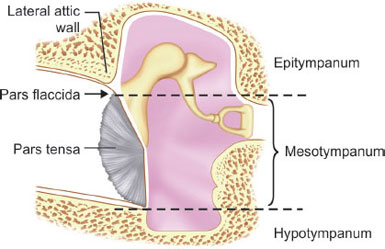
The middle ear space is divided into hypotympanum (lying below the level of pars tensa), mesotympanum (lying opposite the pars tensa) and epitympanum (lying above the pars tensa 10and medial to pars flaccida) (Table 1.3). The area of the middle ear around the tympanic orifice of the Eustachian tube is also called as protympanum.
Relations of the Middle Ear
- The roof is formed by a thin plate of bone called tegmen tympani.
- The floor is formed by a thin plate of bone, which separates tympanic cavity from the jugular bulb.
- The anterior wall is formed by opening for canal of tensor tympani muscle above, below opening of Eustachian tube and a thin bony plate separating the tympanic cavity from internal carotid artery.
- The posterior wall is related to pyramid, aditus, facial nerve and facial recess. Facial recess is a depression in the posterior wall lateral to pyramid and is bounded medially by the vertical part of facial nerve, laterally by chorda tympani nerve and above by the fossa incudis.
- The medial wall is related to promontory (most prominent and bulging part of the medial wall formed by the basal turn of the cochlea), bony lateral semicircular canal, oval window (fenestra vestibule), round window (fenestra cochlea) and the facial nerve running in bony fallopian canal above the oval window.
Communication
The middle ear communicated anteriorly to the nasopharynx by Eustachian tube. Posteriorly middle ear is connected to mastoid antrum by aditus.
Contents of the Middle Ear
- Ossicles (Fig. 1.5)
- Malleus: Hammer shaped, largest and most lateral ossicle measuring 8 mm in length. It has head, neck, handle and also anterior and lateral processes.
- Incus: Anvil shaped, has a body, short process and long process. The body articulates with the head of the malleus in the attic.
Table 1.4 The muscles of tympanic cavity MuscleOriginInsertionInnervationFunctionTensor tympaniCartilaginous pharyngotympanic tube, greater wing of sphenoid, its own bony canalUpper part of handle of malleusMandibular nerve (V3)Contraction pulls handle of malleus medially, tensing tympanic membrane to reduce the force of vibrations in response to loud noiseStapediusAttached to inside of pyramidal eminenceNeck of stapesBranch of facial nerveContraction, usually in response to loud noises, pulls the stapes posteriorly and prevents excessive osscillation - Stapes: Stirrup shaped, smallest ossicle, measuring about 3.5 mm and consists of a head, neck, footplate and also anterior and posterior crura. The footplate is held to the oval window by the annular ligament.
- Muscles: Tensor tympani and stapedius muscles (Table 1.4).
- Ligaments keep the ossicles in their place.
- Nerves: Chorda tympani nerve. It enters the middle ear from posterior wall, runs forwards and lateral to the incus and medial to the malleus, exit through the anterior wall.
Eustachian Tube
It connects the middle ear with the nasopharynx. It is bony at the posterior one-third and cartilaginous at the anterior two-thirds of its length. It is approximately 3.75 cm long in adults. In infants, the tube is shorter, wider, more horizontal and opens at a lower level (Table 1.5). It remains closed at rest and opens intermittently during swallowing, yawning and sneezing. The Eustachian tube helps in ventilation and regulation of the middle ear pressure. It protects against nasopharyngeal sound and reflux of nasopharyngeal secretions. It also helps in middle ear clearance of secretions.
|
Mastoid
It is of three types:
- Cellular or well pneumatized—Mastoid cells are well- developed and intervening septa are thin. There are large and numerous air cells (Fig. 1.6).
- Diploic—Mastoid consists of marrow spaces and a few air cells. Air cells are small and less in number.
- Sclerotic or acellular—Air cells are practically absent.
The cellular mastoid accounts for 80% of the subjects and is considered to be normal. The diploic and sclerotic types may be due to the Eustachian tube dysfunction.
The mastoid air cells are named according to anatomical sites, e.g. tip cells, perisinus cells, subdural cells, zygomatic cells, retrofacial cells, perilabyrinthine cells, etc. (Box 1.1). The antral cell is the constant and largest air cell present from birth.
MacEwen's (Suprameatal) Triangle (Fig. 1.7)
It is bounded by temporal line (a), posterosuperior segment of bony external auditory canal (b) and the line drawn as a tangent to the external auditory canal (c). It is an important landmark to locate the mastoid antrum in mastoid surgery.16
Korner's Septum
Mastoid develops from the squamous and petrous bones. The petrosquamous suture may persist as a bony plate—the Korner's septum, separating superficial squamous cells from the deep petrosal cells. Presence of Korner's septum cause difficult in locating the antrum and the deeper cells.
Internal Ear/Inner Ear
- It consists of bony and membranous labyrinth (Table 1.6).
- The membranous labyrinth is filled with endolymph while the space between the membranous and bony labyrinth is filled with perilymph (Table 1.7).17
- Bony labyrinth consists of three parts: the vestibule, the semicircular canals and the cochlea.
Table 1.6 Parts of the inner ear Parts of bony labyrinthParts of membranous labyrinthSensory end organsExciting stimulusNerve- Semicircular canals
Semicircular canalsCrista in the ampulaAngular accelerationCaloric stimulationVestibular- Vestibule
UtricleSacculeMaculaGravitational pullLinear accelerationSoundVestibular- Cochlea
Cochlear ductOrgan of CortiSoundCochlear - The vestibule is the central part of the bony labyrinth.
- The oval window is present in the lateral wall of the vestibule.
- The inside of the medial wall of the vestibule presents two recesses, a spherical recess, which lodges the saccule and an elliptical recess which possesses utricle. Below the elliptical recess, there is opening for aqueduct of vestibule through which passes the endolymphatic duct.
- There are three semicircular canals, the lateral, posterior and superior, and lie in planes at right angles to one another.
- The three semicircular canals open into the vestibule by 5 openings.
- The bony cochlea is a coiled tube making 2.5–2.75 turns round a central pyramid of bone called the modiolus.
- The bony cochlea contains three compartments—scala vestibuli, scala tympani and scala media (Fig. 1.10).
- The scala vestibuli and scala tympani are filled with perilymph and communicate with each other at apex called helicotrema.
- The scala tympani is closed by secondary tympanic membrane; it is also connected with the subarachnoid space through the aqueduct of cochlea.
- The membranous labyrinth consists of the cochlear duct, the utricle and saccule and the endolymphatic duct and sac.
- The cochlear duct present in the bony cochlea around the modiolus. It is connected to the saccule by the ductus reunions. The cochlear duct is triangular in cross-section with Reissner's (vestibular) membrane, stria vascularis and the basilar membrane forming its three sides. The end organ in the cochlea is the neuroepithelium called the organ of Corti and it is spread like a ribbon along the entire basilar membrane. It is stimulated by sound. It consists of tunnel of Corti which is composed of two rows of rods of Corti. It forms triangle with basilar membrane and contains cortilymph. The tectorial membrane overhangs the organ of Corti. There are hair cells in the organ of Corti which are important receptor cells of hearing and transduce sound energy into electrical energy. Inner hair cells form a single row while outer hair cells are arranged in three or four rows. Inner hair cells are richly supplied by afferent cochlear fibers whereas the outer hair cells mainly receive efferent innervation from the olivary complex and are concerned with modulating the function of inner hair cells (Table 1.8). There are supporting cells like Deiters’ cells which present between the outer hair cells and provide support to latter. Cells of Hensen lie outside the Deiters’ cells.
Physiology of Hearing
|
Conducting Apparatus
It consists of the conduction of sound through air and bone which include external ear, tympanic membrane and the ossicular chain. The external auditory canal conducts the sound to the eardrum. When sound wave falls over tympanic membrane, it sets into vibration and these vibration are transmitted to the cochlea via three ossicles which transmits the sound waves to the oval window by footplate of stapes.
The tympanic membrane is 14 times the size of the footplate (Hydraulic ratio). The ratio of the malleus handle length to that of the long process of incus is 1.3:1. These two factors (14 × 1.3 = 18) reduce the amplitude of the vibrations but increase the force of sound 18 times (Transformer action).
|
|
Perceiving Apparatus
The sound waves reaching the oval window set into vibration, the perilymph in the cochlea, which in stimulates the organ of Corti. The eardrum transmits the sound to the oval window via ossicles and protects the round window. This preserves a phase difference between the oval and round window which is necessary for the fluid displacement in the inner ear.
Theories of Hearing
Place Theory (Helmholtz)
According to this theory each pitch has its own separate place on the basilar membrane. There are separate vibration points on the basilar membrane for each frequency.
Telephone Theory (Rutherford)
According to this theory, the discrimination of pitch depends upon the rate of firing of individual nerve fibers, and the frequency is analyzed in the central nervous system.
Volley Theory (Wever)
This theory represents a combination of both place and telephone theories. According to this, high frequencies are perceived by the place mechanism and low frequencies are perceived by telephone mechanism.
Traveling Wave Theory (Von Bekesy)
According to this theory, the higher frequencies are represented at the base of cochlea and the lower frequencies at the apex.24
Physiology of Vestibular System
The balance or equilibrium of the body is maintained by coordination of the three systems. They are vestibular system, proprioceptors and vision. Loss of any two, create severe imbalance. The vestibular system consists of semicircular canals, utricle and saccule. The semicircular canals detect changes in the position of the body in response to angular acceleration in a direction corresponding to a particular canal. The anterior and posterior semicircular canals function in the vertical plane while the lateral canals function in the horizontal plane. They function as pairs, the superior of one side with the posterior of the other and both lateral canals respectively.
The utricle and saccule detect changes in the position of the body during linear acceleration. Utricle in the horizontal axis and saccule in the vertical axis. The receptor organs in the semicircular canals and the utricle and saccule are specialized sensory hair cells bathed in the endolymph. The cilia (stereocilia) on the hair cells are arranged in an ascending order with the tallest called the kinocilia. During change of posture of body, the endolymph also moves correspondingly and in turn, moves the hair cells in the labyrinth. When the stereocilia moves towards the kinocilia the hair cells are stimulated, while move in opposite direction, cause inhibition. Conditions which stimulate only one labyrinth results in unequal impulses reaching the brain and hence a state of disequilibrium. This may manifest clinically as giddiness, dizziness or imbalance.