Applied Physiology of Ventilation
Mechanical ventilation in children and neonates is different from adults. While basic principles of physics and gas flow apply to all age groups, anatomical and physiological differences play a significant role in selecting the type of ventilator as well as ventilatory modes and settings.
The upper airway in infants is cephalad, funnel shaped with its narrowest area being at the subglottic region (at the level of cricoid ring as compared to the relatively tubular adult airway. Airway resistance increases inversely by 4th power of the radius; i.e. in an already small airway even 1 mm of edema or secretions will increase the airway resistance and turbulent flow markedly necessitating treatment of airway edema, suctioning of secretion, measures to control secretions. Low functional residual capacity (FRC: Volume of air in the lungs at end of expiration) reduces the oxygen reserve and hence the time that apnea can be tolerated by a child.
Respirations are shallow and rapid due to predominant diaphragmatic breathing, and inadequate chest expansion due to the more horizontal alignment of the ribs in infancy giving less play in the bucket handle movement of the ribs during inspiration. Therefore, a child tends to get tachypneic rather than increasing the depth of respiration in response to hypoxemia. Oxygen consumption per kg body weight is higher therefore tolerance to hypoxemia is lower.
Susceptibility to bradycardia in response to hypoxemia is also higher due to high vagal tone. Pores of Kohn and channels of Lambert (bronchoalveolar and interalveolar collaterals) are inadequately developed making regional atelectasis more frequent. Closing volumes are lower and airway collapse due to inadequate strength of the cartilage in the airways is common making a child particularly susceptible to laryngomalacia, and tracheobronchomalacia as well as lower airways closure.
Therefore, children tend to require smaller tidal volumes, faster respiratory rates, adequate size uncuffed endotracheal tube, adequately suctioned clear airway for proper management of mechanical ventilation. Other important factors for choosing the ventilatory setting include the primary pathology, i.e. asthma, acute respiratory distress syndrome (ARDS), pneumonia, air leak syndrome raised intracranial tension, neuromuscular weakness, neonatal hyaline membrane disease, or neonatal persistent pulmonary hypertension (PPHN).
Basic Physiology
Gradient between the mouth and pleural space is the driving pressure for the inspired gases, and this gradient is needed to overcome resistance and to maintain the alveoli open, by overcoming elastic recoil forces. Therefore, a balance between elastic recoil of chest wall and the lung determines lung volume at any given time. Normal inspiration is actively initiated by negative intrathoracic pressure driving air into the lungs. Expiration is passive.
Ventilation
Ventilation washes out carbon dioxide from alveoli keeping arterial PaCO2 between 35–45 mm of Hg. Increasing dead space increases the PaCO2.
Alveolar MV = Respiratory Rate × Effective Tidal Volume
Effective TV = TV—dead space
Dead Space = Anatomic (nose, pharynx, trachea, bronchi) + Physiologic (alveoli that are ventilated but not perfused)
Adequate minute ventilation is essential to keep PaCO2 within normal limits.
Oxygenation
Partial pressure of oxygen in alveolus (PaO2) is the driving pressure for gas exchange across the alveolar-capillary barrier determining oxygenation.
PaO2= [(Atmospheric pressure – water vapor) × FiO2] – PaCO2/RQ
RQ = respiratory quotient
Adequate perfusion to alveoli that are well ventilated improves oxygenation.
Hemoglobin is fully saturated 1/3 of the way through the capillary.
Hypoxemia can occur due to:
-
Hypoventilation
-
V/Q mismatch (V– ventilation, Q– perfusion)
-
Shunt (Perfusion of an unventilated alveolus, atelectasis, fluid in the alveolus)
-
Diffusion impairments
Hypercarbia can occur due to:
-
Hypoventilation
-
V/Q mismatch
-
Dead space ventilation
Gas Exchange
Hypoventilation and V/Q mismatch are the most common causes of abnormal gas exchange in the PICU.
One can correct V/Q mismatch by increasing amount of lung that is ventilated or by improving perfusion to those areas that are ventilated.
Compliance = Δ volume/Δ pressure → the change of unit volume over a change of unit pressure applied is the compliance of the lung.
The pressure used for this calculation is the transpulmonary pressure, which is equal to the difference between the alveolar pressure (Palv) at the end of inflation and the pleural pressure (Ppl or Pes).
-
Pplat ➔substituted for Palv
-
The tidal volume ➔substituted for a change in lung volume (Clung):
-
Therefore the Clung = Vt/(Pplat – Pes)
-
Since True esophageal measures are not available ➔ So usually not measured accurately
Importance of compliance when using pressure and volume modes
-
When a gas is delivered at a set pressure ➔ Tidal Volume ∝ complianceIf for the same Pressure change VOLUME increases ➔ Compliance is GOODIf for the same Pressure change VOLUME decreases ➔ Compliance is POOR
-
When a gas is delivered at a set volume ➔ Pressure 1/μ complianceIf For the same VOLUME pressure DECREASES ➔ Cl is GOODIf For the same VOLUME pressure INCREASES ➔ Cl is POOR
Time constant and inspiratory time
The time constant is the time taken for the airway pressure (and volume) changes to equilibrate throughout the lung ➔ It is proportional to the compliance and resistance of the respiratory system.
Time constant = Compliance × Resistance
One time constant that fills an alveolar unit to 63% of its capacity. It takes three time constants to fill an alveolus to 90% capacity and up to 5 Tc to fill it to 95%.
To calculate a full term neonates Tc who has a compliance of 0.004 L/cm and a R of 30 cm H2O/L/sec the Tc will be:
–C = 0.004 L/cm H2O; R = 30 cm H2O/L/sec
–T = 0.004 × 30 = 0.12 sec.
If we want to set the inspiratory time with this knowledge, then we need 3–5 Tc to fill the alveolus so 0.12 × 4 = 0.48 secs. If we are dealing with RDS/ARDS we could use a lower Ti like 0.4 secs and if we are dealing with an obstructive disease requiring more time we could use a higher Ti like 0.55 secs.
An adult has a Tc of about 0.3 so the Ti is set around 0.9–1 sec commonly.
Indications of mechanical ventilation
Indications remain essentially clinical and may not be always substantiated by objective lab parameters such as blood gas analysis. Common indications include:
-
-
Apnea/respiratory arrest
-
Inadequate ventilation
-
Inadequate oxygenation
-
Chronic respiratory insufficiency with failure to thrive
-
-
Cardiac insufficiency/shock
-
Eliminate work of breathing
-
Reduce oxygen consumption
-
-
Neurologic dysfunction
-
Central hypoventilation/frequent apnea
-
Patient comatose, glasgow coma score (GCS) <8
-
Inability to protect airway
-
Commonly used Nomenclature
Airway pressures
-
Peak inspiratory pressure (PIP)
-
Positive end expiratory pressure (PEEP)
-
Pressure above PEEP (PAP or δP)
-
Mean airway pressure (MAP or Paw)
-
Continuous positive airway pressure (CPAP)
Inspiratory time Ti
I:E ratio,
Frequency (F): Ventilatory rate or RR (usually F is what is set on the machine and RR refers to the total rate of machine plus patient).
Tidal volume (Vt):
Amount of gas delivered with each breath. (Vti will be the Inspiratory vol and Vte will be exp vol. the Vte will be the accurate patient volume as leaks occur during inspiration and the machine checks the actual delivered volume during exhalation).
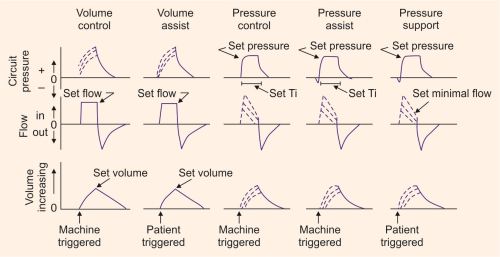
There are five basic breaths that are used. These are shown below.
Various modes are then permutations and combinations of these breaths. It is essential to be familiar with the appearance of the wave forms that are seen in the flow and pressure scalars of these basic breath types. The volume scalar always looks the same.
By convention, the pressure scalar is always the top one followed by the flow scale (Fig. 1.1).
Modes of Ventilation
Control Modes
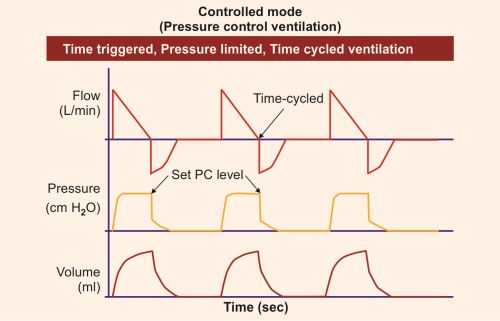
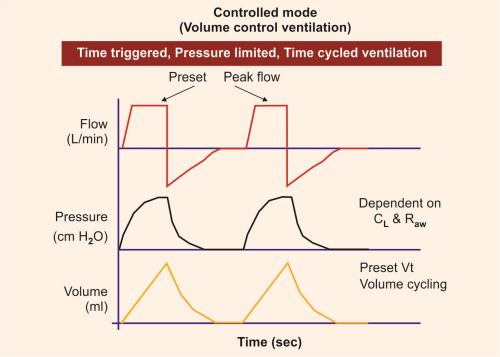
Minute ventilation is determined entirely by the set respiratory rate and tidal volume/pressure.
The patient does not initiate additional breaths above that set on the ventilator (Figs 1.2 and 1.3).
volume control ventilation (VCV): flow-targeted volume-cycled breaths
pressure control ventilation (PCV): pressure-targeted time-cycled breaths
In this mode every breath is fully supported by the ventilator. In classic control modes, patients were unable to breathe except at the controlled set rate. Difficult to wean and asynchrony is a major issue. Patients on control modes will need sedation and/or paralysis. This is usually set with some leeway for patient triggering either SIMV + PSV or in the AC or assist control mode so when the patient awakens and breaths there is adequate flow and to avoid flow hunger and asynchrony.
Assist-control centilation (ACV)
-
Volume assist-control ventilation (VACV): flow-targeted volume-cycled breaths
-
Pressure assist-control ventilation (PACV): pressure-targeted time-cycled breaths
-
Guarantees a set number of positive-pressure breaths.
-
If respiratory rate exceeds this, breaths are patient-triggered breaths (VA or PA). If respiratory rate is below guarantee, ventilator delivers mandatory breaths (VC or PC breaths).
Synchronized intermittent mandatory ventilation (SIMV) (IMV no longer used) (Fig. 1.4)
-
Set ventilator breaths: set minimum minute ventilation with respiratory rate + tidal volume (volume SIMV) or inspiratory P (pressure SIMV)
-
Ventilator breaths are synchronized with patient inspiratory effort
-
Patients increase minute ventilation by additional spontaneous breaths, which can be unassisted or pressure suppart (PS).
Pressure Support
-
Flow-limited mode of ventilation (not volume-limited or pressure-limited)
-
Delivers inspiratory pressure until the inspiratory flow decreases to ∼25% of its peak value.
-
Clinician sets inspiratory pressure, applied PEEP, and FiO2.
-
Patient triggers each breath
-
Comfortable mode, good for weaning, can be combined with SIMV
-
Not good for full ventilatory support, high airway resistance, or central apnea
Pressure support can decrease work of breathing by providing flow during inspiration for patient triggered breaths. It can be given with spontaneous breaths in IMV modes or as stand alone mode without set rate, as well as for weaning to retrain coordination of respiratory muscles in patients on ventilation for longer than few weeks.
Continuous Positive Airway Pressure
-
Continuous level of positive airway pressure.
-
Pt must initiate all breaths
-
Functionally similar to PEEP
-
Good for OSA, cardiogenic pulmonary edema
Bilevel positive airway pressure
-
Mode used during NPPV
-
Delivers set IPAP and EPAP
-
Tidal volume is determined by difference between IPAP-EPAP
Pressure-regulated volume control (PRVC)
-
A form of PACV that uses tidal volume as a feedback control for continuously adjusting the pressure target
-
Combines volume ventilation and pressure control—(for mech., time-cycl. breaths only)
-
Set Vt is “targeted”
-
Ventilator estimates vol./ press. relationship each breath
-
Ventilator adjusts level of pressure control breath by breath
-
Dual mode with flow in the pressure regulated mode, i.e. decelerating.
-
Set PC limit and target Vt, e.g. Vt 100 PIP 28. PEEP 7 Ti 0. 8 seconds
-
First breath = 5–10 cm H2O above PEEP= 11–15 PIP ➔but 100 ml not delivered
-
V/P relationship measured—Next 3 breaths, pressure increased to 75% needed for set TV
-
Then up to +/– 3 cm H2O changes per breath
-
Insp. Time ends inspiration (phase variable)
PRVC – Considerations
-
Like PC, flow varies automatically to varying patient demands
-
Constant press. during each breath—variable press. from breath to breath
-
Time is cycling method; delivered Vt can vary from set.
-
If Vt target not met, dial up PC limit gradually
But check patient—may not need that Vt
Indications:
-
Patient who require the lowest possible pressure and a guaranteed consistent Vt
-
ALI/ARDS
-
Patients requiring high and/or variable insp. flow
-
Patient with the possibility of CL or Raw changes
-
Advantages of PRVC
-
Maintains a minimum PIP
-
Guaranteed Vt and VE
-
Patient has very little WOB requirement
-
Allows patient control of respiratory rate
-
Variable flow and pressure to meet patient demand
-
Decelerating flow waveform for improved gas distribution
-
Breath by breath analysis
Disadvantages and risks:
-
Varying mean airway pressure
-
May cause or worsen auto-PEEP
-
When patient demand is increased, pressure level may diminish when support is needed
-
May be tolerated poorly in awake non-sedated patients
-
A sudden increase in respiratory rate and demand may result in a decrease in ventilator support
Basic Fundamentals of Ventilation
Ventilators deliver gas to the lungs using positive pressure at a certain rate. The amount of gas delivered can be limited by time, pressure or volume. The duration can be cycled by time, pressure or flow.
If volume is set, pressure varies; if pressure is set, volume varies according to the compliance.
Following are three main expectations from the ventilator
-
Ventilator must recognize patient's respiratory efforts (trigger)
-
Ventilator must be able to meet patient's demands (response)
-
Ventilator must not interfere with patient's efforts (synchrony)
-
Whenever a breath is supported by the ventilator, regardless of the mode, the limit of the support is determined by a preset pressure or volume.
-
Volume limited: Preset tidal volume
-
Pressure limited: Preset PIP
Pressure vs Volume Control
Goal is to ventilate and oxygenate adequately. Both pressure and volume control modes can achieve it. Important requirements include adequate movement of the chest and minimal barotrauma or volutrauma.
One must have a set up of high/low pressure alarms in volume cycling and, low expired tidal volume alarm when using pressure cycling.
Pressure Limited Ventilation
Ventilator stops the inspiratory cycle when set PIP is achieved.
Caution: Tidal volume changes suddenly as patient's compliance changes.
Ventilator delivers a decelerating flow pattern (lower PIP for same Vt).
This can lead to hypoventilation or overexpansion of the lung. If endotracheal tube is obstructed acutely, delivered tidal volume will decrease. This mode is useful if there is a leak around the endotracheal tube.
For improving oxygenation, one needs to control FiO2 and MAP, (I-time, PIP, PEEP) and to influence ventilation, one needs to control PIP and respiratory rate.
Volume Limited Ventilation
Ventilator stops the inspiratory cycle when set tidal volume has been delivered.
One can control minute ventilation by changing the tidal volume and rate. For improving oxygenation primarily FiO2, PEEP, I-time can be manipulated. Increasing tidal volume will also increase the PIP, hence affecting the oxygenation by increasing the mean airway pressure. It delivers volume in a square wave flow pattern. Square wave (constant) flow pattern results in higher PIP for same tidal volume as compared to pressure modes.
Caution: There is no limit per se on PIP (so ventilator alarm will have to be set for an upper pressure limit to avoid barotrauma). Volume is lost if there is a circuit leak or significant leak around the endotracheal tube, therefore an expired tidal volume needs to be monitored and set. Some ventilators will alarm automatically if the difference between set inspired tidal volume and expired tidal volume is significant (varies between the ventilators).
Trigger/Sensitivity
Trigger means sensitivity setting of the ventilator.
10Ventilators have a negative pressure sensor which can be set at various levels of sensitivity to initiate a breath usually based on patient effort (negative pressure) or elapsed time before the next breath in the event of respiratory depression or apnea. The patient's effort can be “sensed” as a change in pressure or a change in flow in the circuit (flow triggering). A setting of greater than 0 makes it too sensitive (meaning the triggered breath from the ventilator will be too frequent). A negative setting (negative 1 or negative 2) setting is usually acceptable. Too negative setting will increase the work of the patient (to generate a negative pressure) to trigger a ventilator breath.
Initial Ventilator Settings
One should always have the general idea regarding what initial ventilatory settings to choose when initiating the ventilation. Parameters to chose include:
Rate: start with a rate that is somewhat normal; i.e. 15 for adolescent/child, 20–30 for infant/small child, 30–40 for a neonate.
FiO2: 1 (100%) and wean down to level <0.5.
PEEP: 3–5 cm of H2O (higher if ARDS, low compliance disease, lower if Asthma, high compliance disease.
Inspiratory time (I-time or I:E ratio): 0.3–0.4 sec for neonates, 0.5–0.6 sec for children, 0.7–0.9 in older children. Normal I:E ratio = 1:2–1:3
Higher I-times may be needed to improve oxygenation in difficult situations (Inverse ratio ventilation) increasing the risk of air leak.
Control every breath (Assist control) or some (SIMV)
Choose the mode:
Pressure limited: PIP is set depending upon lung compliance and pathology:
-
Neonates: 18–22 cm H2O
-
Children 18–25 cm H2O
Volume limited:
Tidal volume 6–8 ml/kg.
Adjustments after initiation: usually based on blood gases and oxygen saturations
For oxygenation: FiO2, PEEP, I-time, PIP (tidal volume) can be adjusted (increase MAP) (Fig. 1.5).
For ventilation: Respiratory rate, tidal volume (in volume limited) and PIP (In pressure limited mode) can be adjusted.
PEEP is used to help prevent alveolar collapse at end inspiration; it can also be used to recruit collapsed lung spaces or to stent open floppy airways
Gas exchange related problems:
-
Inadequate oxygenation (hypoxemia)
-
Inadequate ventilation (hypercarbia)
Inadequate oxygenation: low PaO2
Important guidelines:
Fig. 1.5: Mean airway pressure (area under the pressure time curve) and oxygenation(1: increase inspiratory rise time, 2: increase PIP/ VT, 3: increase inspiratory time, 4: increase PEEP, 5: increase rate)
-
Don't just increase FiO2
-
Increase tidal volume if volume limited mode, PEEP, inspiratory time (Ti).
-
Increase peak inspiratory pressure (PIP)/PEEP/Ti if pressure limited mode
-
If O2 worse, get chest X-ray to rule out air leak, if lungs show worsening (increase PEEP further)
-
Do not forget other measures to improve oxygenation:
-
Normalize cardiac output (if low output) by fluids and/inotropes
-
Maintain normal hemoglobin
-
Maintain normothermia
-
Deepen sedation/consider neuromuscular block
-
Determinant of Paw = area under the curve (Mean Airway Pressure) and therefore oxygenation:
-
Inspiratory flow rate
-
Peak inspiratory pressure
-
Inspiratory time
-
PEEP
Inadequate Ventilation: High PaCO2
Common reasons include hypoventilation, dead space ventilation (too high PEEP, decreased cardiac output, pulmonary vasoconstriction),
Increased CO2 production: hyperthermia, high carbohydrate diet, shivering.
Inadequate tidal volume delivery (hypoventilation): will occur with endotracheal tube block, malposition, kink, circuit leak, ventilator malfunction.
Measures for High PaCO2
Guidelines
-
If asthma: Increase expiratory time, may need to decrease rate to achieve an I:E ratio >1:3
-
If pressure limited: Increase peak inspiratory pressure (PIP), decrease PEEP, increase frequency
-
Decrease dead space (increase cardiac output, decrease PEEP, vasodilator)
-
Decrease CO2 production: Cool, increase sedation, decrease carbohydrate load
-
Change endotracheal tube if blocked, kinked, misplaced or out, check proper placement
-
Fix leaks in the circuit, endotracheal tube cuff, humidifier
Measures to Reduce Barotrauma and Volutrauma
Following concepts are being increasingly followed in most pediatric intensive care units:
-
Permissive HypercapniaHigher PaCO2 are acceptable in exchange for limiting peak airway pressures: as long as pH >7.2
-
Permissive HypoxemiaPaO2 of 55–65; SaO2 88–90% is acceptable in exchange for limiting FiO2 (<60) and PEEP, as long as there is no metabolic acidosis.Adequate oxygen content can be maintained by keeping hematocrit >30%.
Patient ventilator dyssynchrony: Incoordination between the patient and the ventilator: Patient fights the ventilator!!
Common causes include hypoventilation, hypoxemia, tube block/kink/malposition, bronchospasm, pneumothorax, silent aspiration, increased oxygen demand/increased CO2 production (in sepsis), inadequate sedation.
If patient fighting the ventilator and desaturating: Immediate measures.
Use Pnemonic: DOPE
D–displacement, O–obstruction, P–pneumothorax, E–equipment failure
-
Check tube placement. When in doubt take the endotracheal tube out, start manual ventilation with 100% oxygen
-
Examine the patient: is the chest rising? Breath sounds present and equal? Changes in exam? Atelectasis, treat bronchospasm/tube block/malposition/pneumothorax? (consider needle thoracentesis). Examine circulation: shock? sepsis?
-
Check arterial blood gas and chest X-ray for worsening lung condition, and for confirming pneumothorax.
-
Examine the ventilator, ventilator circuit/humidifier/gas source
Sedation and muscle relaxation during ventilation
Most patients can be managed by titration of sedation without muscle relaxation.
Midazolam (0.1–0.2 mg/kg/hr) and vecuronium drip (0.1–0.2 mg/kg/hr) is most commonly used. Morphine or fentanyl drip can also be used if painful procedures are anticipated.
Routine ventilator management protocol
The following protocol is commonly followed:
-
Wean FiO2 for SpO2 above 93–94%
-
ABG 1 hour after intubation, then am and pm schedule (12 hourly), and after major ventilator settings change, and 20 minutes after extubation
-
Pulse oximetry on all patients, end-tidal carbon dioxide (EtCO2)/graphics monitoring if available
-
Frequent clinical examination for respiratory rate, breath sounds, retractions, color
-
Chest X-ray every day/alternate day/as needed
Respiratory care protocol
-
Position change 2 hourly right chest tilt/left chest tilt/supine position. Unless highly unstable
-
Suction 4 hourly and as needed (In line suction to avoid de recruitment/loss of PEEP/desaturation if available)
-
Physiotherapy 8 hourly
-
Percussion, vibration and postural drainage. No physiotherapy if labile oxygenation such as ARDS and PPHN
-
Nebulization: In line nebulization is preferred over manual bagging. Metered dose inhalers (MDIs) can also be used.
-
Disposable circuit change if soiled or >96 hours
-
Humidification/in line disposable humidifier.