Snapshot
- 3• Introduction and Historical Perspective
- • Left Main Coronary Artery
- • Left Anterior Descending Coronary Artery (Anterior Interventricular Artery)
- • Left Circumflex Coronary Artery
- • Right Coronary Artery
- • Posterior Descending Coronary Artery
- • Intramural Coronary Vasculature
- • Coronary Venous System
- • Coronary Sinus
- • Anterior Interventricular Vein
- • Middle Cardiac Vein
- • Small Cardiac Vein
- • Anterior Cardiac Veins
- • Veins Draining the Right and Left Atria
INTRODUCTION AND HISTORICAL PERSPECTIVE
The circulatory system and coronary anatomy were described and illustrated many centuries ago (Figs. 1.1 and 1.2). For centuries though, the course, position and variations of the coronary arterial system were of interest only to anatomists and pathologists and of no interest to clinicians. However, with the development of coronary angiography, coronary bypass surgery, and more recently percutaneous coronary intervention, knowledge of the details of coronary arterial anatomy has become essential.
The anatomy of the coronary sinus and venous system is important in retrograde myocardial perfusion in patients undergo cardiopulmonary bypass, during the placement of a left ventricular pacing wire in patients treated with cardiac resynchronization therapy (CRT), and in some patients undergoing radiofrequency catheter ablation for the treatment of cardiac arrhythmias.
Fig. 1.1: Purported first drawing of the circulatory system by Leonardo da Vinci. [Image from Mehrotra BM and Kasliwal RR. The history of acute coronary syndrome. In: Chopra HK and Nanda NC (Eds). Textbook of cardiology (a clinical & historical perspective). Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, India 2013].
Although coronary arteriography has been the “gold standard” for visualizing the coronary arteries, the development of non-invasive imaging with computed tomography (CT) coronary angiography (Figs. 1.3 and 1.4) and magnetic resonance imaging (MRI) (Fig. 1.5) has markedly improved our ability to define the exact origin and course of the coronary arteries as they spread out across the surface of the heart. Another advance in coronary artery imaging is intravascular ultrasound (IVUS), which allows for visualizing the details of the coronary artery lumen and walls (Figs. 1.6A and B).
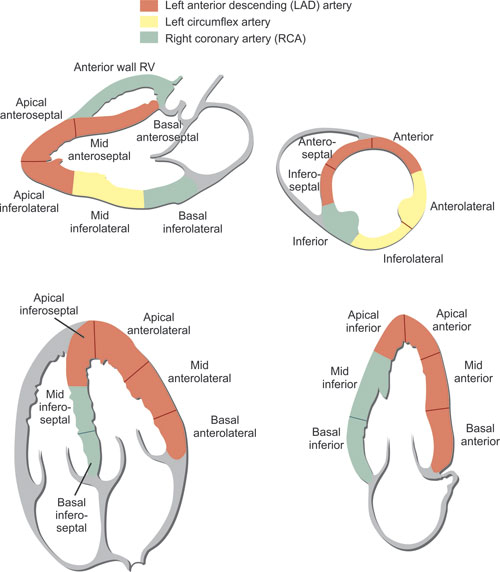
The coronary arteries arise as the first branches off the aorta and provide the blood supply to the heart (Figs. 1.7 to 1.10). The descriptions of the course of the coronary arteries and veins over the epicardial surface of the heart (extramural vessels) in this chapter apply to the majority of normal hearts. The coronary arteries that penetrate the myocardium are called intramural vessels and unlike the extramural coronary arteries do not become atherosclerotic. In adults, the extramural coronaries are frequently encased in epicardial fat. At times varying lengths of myocardium called “myocardial bridges” cover portions of the extramural arteries (Figs. 1.11 and 1.12). There are reports that these muscle-encased segments of extramural coronary artery can have clinical significance in that the vessel can be severely compressed during systole, causing myocardial ischemia or even infarction. The regions of the myocardium perfused by the major coronary arteries are illustrated in Figure 1.13.
LEFT MAIN CORONARY ARTERY
The left main coronary artery arises from the left sinus of Valsalva (Figs. 1.14 and 1.15) and passes leftward, posterior to the right ventricular outflow tract and anterior to the left atrial appendage, before bifurcating into the left anterior descending (LAD) and left circumflex coronary arteries. The subjacent position of these arteries to the left atrial appendage is important to electrophysiologists when performing ablations for arrhythmias. The length of the the left main coronary artery varies between 0.5–2.5 cm. The location of the ostium of the left coronary artery with respect to the sinotubular junction is: 48% of the time at the same level; 34% above the sinotubular junction; and 18% below the sinotubular junction. The left main coronary artery is absent in 0.5–1.0% of hearts. The left main coronary artery bifurcates into the LAD and left circumflex artery in approximately two-thirds of patients. In approximately one-third of patients the left main trifurcates and there is a third branch, called the ramus intermedius artery (Fig. 1.16), which supplies the anterolateral left ventricular wall.
LEFT ANTERIOR DESCENDING CORONARY ARTERY (ANTERIOR INTERVENTRICULAR ARTERY)
The left anterior descending (LAD) artery arises from the left main coronary artery as a direct continuation and passes in the anterior descending interventricular groove distally toward the apex (Figs. 1.17 and 1.18). It terminates before or at the apex in 35% of hearts, and continues around the apex to the inferior interventricular groove of the heart (“wrap around LAD”) in 64% of hearts. It has a variable number of secondary branches to the right and left ventricles adjacent to the artery. The right ventricular branches are usually small and not constant in arrangement. Those to the left ventricle are termed diagonal branches. These branches supply the anterolateral wall and the anterior papillary muscle of the left ventricle. Occasionally, shortly after its origin, the LAD divides into two equal parallel vessels that pass in the anterior interventricular groove distally (referred to as a “dual LAD”).
5
Figs. 1.3A and B: D volume rendered CT coronary angiography images of the coronary anatomy. (A) Anterior view of the heart. (B) Posterior view of the heart. (Ao: Aorta; GCV: Great cardiac vein; IVC: Inferior vena cava; LA: Left atrium; LAD: Left anterior descending artery; MCV: Middle cardiac vein; OM: Obtuse marginal coronary artery; PDA: Posterior descending artery; PLV: Posterolateral vein). [Image reproduced with permission from Okere C and Sigundsson G. Cardiac Computed Tomography. In: Chatterjee K, et al (Eds). Cardiology—an illustrated textbook. Jaypee Brothers Medical Publishers (P) Ldt., New Delhi, India 2013].
6
Figs. 1.4A to D: CT coronary angiography demonstrating normal coronary anatomy. (A) 3D volume rendered reconstruction of heart and coronary arteries. (B) Right coronary artery. (C) Left anterior descending (LAD) coronary artery. (D) Left circumflex artery. [Image from Pelgrim GJ, et al. Computed tomography imaging of the coronary arteries. In: Baskot BG (Eds). What should we know about prevented, diagnostic, and interventional therapy in coronary artery disease. Intechweb.org].
7
Fig. 1.5: Magnetic resonance imaging cross-sectional view of the origin of the coronary arteries. (Ao: Aorta; LA: Left atrium; LAD: Left anterior descending coronary artery; LCx: Left circumflex artery; LMCA: Left main coronary artery; LV: Left ventricle; RA: Right atrium; RCA: Right coronary artery; RVOT: Right ventricular outflow tract). [Image reproduced with permission from Dr. Alan H. Stolpen and Dr. RM Weiss, Department of Radiology, University of Iowa Carver College of Medicine. Image from Weiss RM. Cardiovascular magnetic resonance. In: Chatterjee K, et al (Eds). Cardiology—an illustrated textbook. Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, India 2013].
Shortly after the origin of the LAD there are a number of perforating intramural septal branches (Figs. 1.19A and B), the largest being the most proximal. These perforating septal branches (Fig. 1.20) supply the anterior two-thirds of the interventricular septum, as well as the atrioventricular (His) bundle and the bundle branches of the conduction system. A septal branch may pass along the moderator band and supply the anterior papillary muscle of the right ventricle.
8
Figs. 1.6A and B: Cross-sectional format of a representative coronary intravascular ultrasound (IVUS) image. IVUS is the imaging catheter in the coronary lumen. Histological section with elastic stain shows correlation with intima, media, and adventitia. The media has a lower ultrasound reflectance owing to less collagen and elastin than neighboring layers. Since the intima reflects ultrasound more strongly than the media, there is spillover in the image resulting in slight overestimation of intimal thickness and underestimation of medial thickness. [Image and legend text adapted from Kume T, et al. Intravascular coronary ultrasound and beyond. In: Chatterjee K, et al. Cardiology—an illustrated textbook. Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, India 2013].
Fig. 1.7: 3D image of the coronary arteries. The coronary arteries arise as the first branches off the aorta and provide the blood supply to the heart. (LCx: Left circumflex artery; LAD: Left anterior descending coronary artery; RCA: Right coronary artery). (Image purchased for use from canstockphoto.com).
9
Figs. 1.8A and B: Plaster cast of extramural coronary arteries. (A) Anterior view. (B) Posterior surface of the heart. (Image modified with permission from Baroldi G and Scomazzoni G. Coronary Circulation in the Normal and the Pathologic Heart. Part 1. Page 5, Armed Forces Institute of Pathology, Office of the Surgeon General, Dept of the Army, Washington D.C. 1965).
Fig. 1.9: Ventral surface of the heart showing coronary veins and arteries. [Image with permission from Cheitlin MD and Ursell P. Cardiac anatomy. In: Chatterjee K, et al. Cardiology—an illustrated textbook. Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, India 2013. Imaged reproduced with permission from Charles C Thomas Publisher LTD, Springfield IL].
Figs. 1.11A to C: Myocardial bridge involving the mid left anterior descending (LAD) artery demonstrated by CT coronary angiography. (A) Maximum intensity projection (MIP) CT coronary angiogram demonstrating myocardial bridging over the mid LAD (orange arrows). The area where the artery emerges from the myocardium and becomes epicardial is shown with the red arrow. (B) Volume rendered image of the heart. The point where the LAD becomes epicardial is denoted by the white arrow. (C) 3D reconstruction of the coronary arteries. A clear “step up” of the LAD is visible (red arrow), corresponding to where the LAD becomes epicardial. [Images from Bamoshmoosh M and Marraccini P. Myocardial bridges in the era of non-invasive angiography. In: Baskot BG (Ed). What should we know about prevented, diagnostic, and interventional therapy in coronary artery disease. Intechweb.org].
11
Figs. 1.12A to C: Still images from a coronary angiogram demonstrating an area of bridging in the distal LAD. In diastole (A), the coronary artery at the area where a myocardial bridge exists does not appear to be narrowed. In early systole (B), there is clear compression and narrowing of the artery. In later diastole (C), the artery appears to be completely compressed.
LEFT CIRCUMFLEX CORONARY ARTERY
The left circumflex coronary artery arises at right angles from the left main coronary and proceeds in the anterior atrioventricular groove, giving off small obtuse marginal branches to the left ventricular lateral wall and the left atrium (Fig. 1.21). The left circumflex artery terminates between the obtuse margin and the crux of the heart in 85% of cases, and at or beyond the crux in 15% of hearts. It may also continue down the inferior interventricular groove a variable distance as the posterior descending artery (PDA). Occlusion of the left circumflex artery will result in infarction of the lateral wall of the left ventricle.
There is a constant ventricular branch arising at right angles from the circumflex at the obtuse margin of the heart called the obtuse marginal coronary artery that passes distally along the left obtuse margin toward the apex. The internal diameter of the vessel is 2 mm. In 10% of the hearts, the circumflex does not follow the atrioventricular groove but passes obliquely over the lateral left ventricular wall toward the apex.
RIGHT CORONARY ARTERY
The ostium of the right coronary artery (RCA) is in the right coronary sinus of the aortic valve. The RCA originates at the same level with respect to the sinotubular junction in 70% of hearts, above the level of the sinotubular junction in 20% of hearts, and below the level of the sinotubular junction in 10% of the hearts. The RCA then passes posterior to the right ventricular infundibulum and into the right anterior atrioventricular groove (Figs. 1.22A to C). In about 10% of the hearts the RCA terminates at or just beyond the acute margin of the heart, but usually it passes around to the inferior atrioventricular groove and then at the crux of the heart, down the inferior interventricular groove as the posterior descending coronary artery (PDA). In this more common situation, the heart is said to have a right dominant coronary system. In cases in which the RCA does not give off the PDA but is only a small artery that supplies the right ventricle, the RCA is referred to as a “non-dominant” RCA.
The first branch of the right coronary artery, called the conal artery, passes anteromedially to the anterior surface of the right ventricular outflow tract. In 50% of hearts, the conal artery arises from the right coronary sinus from a separate ostium from the right coronary artery.
In most patients, the RCA gives off the sinoatrial (SA) nodal artery, which supplies the SA node. The SA nodal artery originates shortly after the origin of the RCA. In a minority of hearts, the SA nodal artery arises from a continuation of an anterior atrial branch of the circumflex coronary artery.
13
Fig. 1.14: Pathologic specimen demonstrating the origin of the left main coronary artery (LMCA) from the left coronary sinus (LCS). The left circumflex artery (LCx) arises from the left main artery. The right coronary artery (RCA) is seen originating from the right coronary sinus (RCS). NCS: Non-coronary sinus. [Image modified with permission from Cheitlin MD and Ursell PC. Cardiac anatomy. In: Chatterjee K, et al. Cardiology—an illustrated textbook. Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, India 2013].
Fig. 1.15: Anterior aspect of the heart showing the origin of the left main coronary artery from the aorta and the course of the coronary arteries. With the parietal pericardium removed, epicardial fat has been partially dissected away to show the proximal courses of the coronary arteries. The pulmonary trunk (PT) is truncated to uncover the origin of the left main coronary artery (LM) from the left side of the aortic root and its relatively short course. With the left atrial appendage (LAA) reflected superiorly, the divergence of the left anterior descending (LAD) and circumflex (Circ) branches is revealed. The left anterior descending branch continues in the anterior interventricular groove (dashed line) that is filled with non-dissected fat that covers the distal portion of artery. The circumflex branch courses under the left atrial appendage in the left atrioventricular groove posteriorly toward the inferior surface of the heart. From the right side of the aortic root, the right coronary artery (RCA) courses in the fat-filled atrioventricular groove toward the heart's inferior surface. A small conal branch (*) of the RCA courses toward the infundibulum.
Fig. 1.16: 3D volume rendered CT coronary angiogram showing trifurcation of the left main coronary artery (LMCA) in to the left anterior descending artery (LAD), ramus intermedius artery, and left circumflex artery (LCx). [Image adopted from Ravelo DR, et al. Multislice coronary angiotomography in the assessment of coronary artery anomalous origin. Arq Bras Cardiol. 2012;98(3):266-272].
As the RCA travels around the right ventricle (RV), it gives off at right angles one or two acute marginal arteries (also called RV branches) which supply the anterior wall of the right ventricle. Proximal occlusion of the RCA will compromise blood flow to the RV, and thus approximately 1/3 of inferior STEMI patients will have some clinical degree of RV infarction.
As the RCA turns at the crux to become the PDA, the atrioventricular nodal artery arises and passes superiorly to supply the atrioventricular (AV) node.
In 65% of hearts the RCA continues past the crux and after giving off the PDA continues on as the posterolateral segment, giving off one or more posterolateral branches, supplying the inferior (or “posterior”) wall of the left ventricle. In patients with this anatomy, acute occlusion of the RCA will result in not only inferior wall MI but also what is referred to as posterior wall MI.
14
Fig. 1.17: Coronary angiogram of the left anterior descending (LAD) artery. The LAD is seen arising from the left main (LM) coronary artery. The LAD usually gives off several diagonal branches, though in this case it gives off one very large branching diagonal branch. Numerous septal perforators (arrows) arise at right angles from the LAD and penetrate into the interventricular septum. The LAD can be seen wrapping around the apex of the heart.
Fig. 1.18: Gross pathology specimen of the heart demonstrating the course of the LAD (arrows), running from base to apex, along the interventricular septum between the left ventricle (LV) and right ventricle (RV). [Image reproduced with permission from Cheitlin MD and Ursell PC. Cardiac anatomy. In: Chatterjee K et al. Cardiology—an illustrated textbook. Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, India 2013].
Figs. 1.19A and B: Perforating branches from extramural coronary arteries as intramyocardial resistance arteries. (A) As the left anterior descending (LAD) coronary emerges from under the left atrial appendage (LAA, ), the proximal portion of the vessel has been opened to show the origins of several septal perforators (arrows). (B) A histological section from an infant shows the perpendicular course of similar resistance arteries (arrows) in the left ventricular free wall. These perforating branches arise at right angles from the extramural coronary arteries.
15
Fig. 1.20: Interventricular septal arterial circulation. Septal perforating arteries arise from the left anterior descending artery (LAD) and the posterior descending artery (PDA) branch, which most commonly arises from the right coronary artery. (With permission from Baroldi G and Scommazoni G. Coronary Circulation in the Normal and Pathologic Heart, Part 1, page 20, Fig 11, Armed Forces Institute of Pathology, Washington D.C., 1967).
POSTERIOR DESCENDING CORONARY ARTERY
In the majority of patients the posterior descending artery (PDA) (more anatomically correct termed the inferior descending artery) is given off by the RCA, and the patient is said to have a “right dominant system”. In a minority of patients, the PDA is given off by the left circumflex artery and the patient is said to have a “left dominant system”. In 30% of the hearts there are either two parallel inferior descending arteries from the right coronary or one from the right and one from the circumflex coronary artery (Figs. 1.23A and B).
In 50% of the hearts the PDA descending coronary artery terminates at the left ventricular apex, and in the other half it terminates before it reaches the apex. Whether arising from the distal RCA or the left circumflex coronary artery the PDA supplies the left and right ventricular inferior walls. It also has vertical perforating intramural branches which supply the inferior third of the interventricular septum.
INTRAMURAL CORONARY VASCULATURE
Arising at right angles from the extramural coronary arteries, the perforating branches in the ventricular walls form a complex network of resistance arteries that form a capillary meshwork around myocardial fibers. The perforating arteries vary in their course through the myocardium, branching off at right angles at all levels of the ventricular wall like the tines of a fork (Fig. 1.24). Some proceed to the subendocardium and then spread out parallel to the endocardium of the cardiac chambers. At the subendocardial level there are anastomosing vessels as well as end-arteries. There are also arterioluminal and venoluminal channels connecting terminal intramural arteries with the ventricular and atrial chambers that have different names depending on the connections and histology of the small vessels. The ostia of these vessels can be seen on examination of the endocardial surface of the ventricles and more prominently of the atria. A general name for these vessels that empty into the cardiac chambers is that of The besian veins or vessels.
16
Figs. 1.22A to C: The right coronary artery (RCA) as imaged by invasive coronary angiography, CT coronary angiography, and magnetic resonance angiography. [Image from Schonenberger E, et al. Patient acceptance of noninvasive and invasive coronary angiography. PLoS ONE 2(2):e246. doi:10.1371/journal.pone.0000246].
Figs. 1.23A and B: Coronary angiograms of the right coronary artery (RCA) and the posterior descending artery (PDA). The RCA is seen giving off an right ventricular (RV) branch (also called an acute marginal branch), then giving off the PDA. The RCA continues as the posterolateral segment, which gives off a posterolateral (PL) branch.
Collateral or anastomosing subarteriolar arteries of 25–250 µm between coronary arterial systems (Fig. 1.25) have been demonstrated by post-mortem coronary contrast injections. Those that connect different branches of the same coronary artery are called homocoronary anastomoses, and those that connect branches of the other two or three coronary arteries, intercoronary anastomoses. These vessels form the basis for collateral circulation that becomes visible on angiography when a major coronary artery becomes obstructed or occluded by atherosclerosis. The homocoronary and intercoronary collaterals are rare in the subepicardium but are found at all other levels of the ventricular wall. This explains why collateral vessels are rarely seen on the epicardial surface of the heart on coronary angiograms.
There are also extracardiac collaterals that connect the coronary arterial system with vessels other than the heart. These collaterals are very small vessels that connect the left circumflex coronary with the vasa vasorum of the aortic root, the pulmonary artery with the bronchial and mediastinal arteries, the atrial branches to the vasa vasorum of the venae cavae, and the atrial branches to the pericardial vessels along the pericardial reflections.
CORONARY VENOUS SYSTEM
The coronary venous system (Fig. 1.26) can be divided into two sections: the extramural veins that drain into the coronary sinus as well as the anterior cardiac veins that drain directly into the right atrial chamber, and the intramural or The besian veins that are at every level within the cardiac walls and are arranged parallel to the myocardial fibers. As with other veins, the cardiac veins have both unifoliate (one leaflet) and bifoliate (two leaflets) valves.
CORONARY SINUS
Not a proper vein histologically, the coronary sinus (Figs. 1.27 to 1.29) is a muscular conduit that is formed at the confluence of the oblique vein of the left atrium and the great cardiac vein near the obtuse margin of the heart. The coronary sinus then courses in the inferior left atrioventricular groove toward the right atrium and drains most of the left ventricular wall, as well as parts of the left and right atrium. Joining the coronary sinus is the oblique vein of the left atrium that passes between the left atrial appendage and the left pulmonary veins. The proximal end of the oblique vein is a tendon of Marshall, a vestige of the embryonic left anterior cardinal vein. However, if the embryonic vein remains open, it functions as a persistent left superior vena cava draining into the coronary sinus.
As the coronary sinus courses rightward in the inferior left atrioventricular groove, it receives tributary veins from the left and right atria and from the inferior wall of the left ventricle, finally emptying into the right atrial cavity posteroinferiorly. The diameter of the coronary sinus is 6-16 mm and its length from 2-5 cm, depending on the size of the heart. The ostium of the coronary sinus is inferior and medial to the entrance of the superior vena cava and is guarded in two-thirds of hearts by the usually inconspicuous Thebesian valve. However, at times the valve covers the ostium almost completely, may be fenestrated, and may make it impossible to enter by catheter.
ANTERIOR INTERVENTRICULAR VEIN
A major vein, the anterior interventricular vein is the most consistent of the coronary venous system. It originates at or near the left ventricular apex and ascends in the anterior interventricular groove, draining the apex and anterior wall of the left ventricle, the anterior two-thirds of the interventricular septum, and the adjacent right ventricular wall. As it reaches the anterior atrioventricular groove the vein passes leftward between the origin of the pulmonary trunk and the tip of the left atrial appendage. It continues as the great cardiac vein, receiving branches that drain the anterior left atrial wall and superior left ventricle, and then becomes the coronary sinus where the oblique vein of the left atrium enters the coronary sinus.
Fig. 1.28: Cardiac CT venography demonstrating the coronary sinus (CS), great cardiac vein (GCV), posterior interventricular vein (PIV), posterior vein of the left ventricle (PVLV), and anterior interventricular vein (AIV). (Image from Ohta Y, et al. Evaluation of the optimal image reconstruction interval for noninvasive coronary 64-slice computed tomography venography. Open Journal of Radiology, 2013, 3, 66-72. doi:10.4236/ojrad.2013.32010. Published Online June 2013).
MIDDLE CARDIAC VEIN
The middle cardiac vein (Fig. 1.30), also known as the inferior interventricular vein, drains the diaphragmatic wall of the left ventricle and the posterior third of the interventricular septum. At the inferior aspect of the left ventricular apex, the middle cardiac vein arises from one or two small superficial veins. Enlarging as it courses in the inferior interventricular groove toward the base of the heart, it usually drains into the coronary sinus near that conduit's entrance to the right atrium, and less often directly into the right atrium. From 2 to 6 veins drain the diaphragmatic and lateral left ventricular wall into the coronary sinus, the most consistent of these being the inferior left ventricular vein draining the diaphragmatic lateral wall of the left ventricle and the obtuse marginal vein draining the lateral wall of the left ventricle.
SMALL CARDIAC VEIN
The small cardiac vein (also known as the right coronary vein) is present in about 70% of hearts. The small cardiac vein, when present, runs in the right inferior atrioventricular groove and terminates at the ostial opening of the coronary sinus or directly into the right atrium. It drains most of the walls of the right atrium, and in the absence of the right cardiac veins, the anterior surface of the right ventricle. In some hearts, the small cardiac vein receives the right marginal vein in which case it drains the anterior wall of the right ventricle.
ANTERIOR CARDIAC VEINS
The anterior cardiac veins, between 3 and 6 in number, drain most of the anterior and lateral wall of the right ventricle directly into the right atrium. Within this group is the right marginal vein, originating at or near the cardiac apex, and ascending along the acute margin of the heart, draining both the adjacent anterior and diaphragmatic surfaces of the right ventricle.
Fig. 1.30: Cardiac veins on the diaphragmatic (inferior) surface of the heart. Cardiac veins run superficial to their corresponding arteries. On the inferior surface of this adult heart the middle cardiac vein (MCV) courses in the interventricular groove toward the base of the heart, where it connects with the coronary sinus. The obtuse marginal vein (OMV) courses along the obtuse margin toward the base of the heart and coronary sinus. (IVC: Inferior vena caval vein connection with right atrium; LV: Left ventricle; RV: Right ventricle).
VEINS DRAINING THE RIGHT AND LEFT ATRIA
The walls of the right atrium are drained through small, largely intramural, vessels and intramural conduits. They predominantly drain through very small orifices directly into the right atrial cavity and are called The besian veins. The large intramyocardial tunnels, numbering from 1 to 3, are located variably but usually in the posterior and lateral atrial walls, and drain venous blood from the anterior cardiac veins and from the sinoatrial and atrioventricular nodes.
21The left atrial veins are small and are divided into three groups. The posterolateral group drains the posterolateral areas of the left atrium through two or three veins, as well as draining the left atrial appendage. Included in the posterolateral group is the oblique vein of the left atrium. Most of the posterolateral groups of veins drain into the coronary sinus. The posterosuperior groups of veins, usually 3 in number, drain the small area of left atrial wall surrounded by the pulmonary venous ostia. The venous drainage of the atria and ventricles is illustrated in Figure 1.26.
CONCLUSION
Our understanding of cardiovascular anatomy and physiology continues to advance, even in the current age. A detailed knowledge of normal coronary vascular anatomy is important to understanding the heart's circulation. It is critical to deciphering images of the pathologic anatomy in living patients.
BIBLIOGRAPHY
- Almuwaqqat Z, Tranquilli M, Elefteriades J. anatomy of main coronary artery location: radial position around the aortic root circumference. Int J Angiol. 2012;21:125–8.
- Anderson RH, Becker AE. The Heart—Structure in Health and Disease Gower Medical Publishing, London. 1992, 132–35.
- Baroldi G, Scomazzoni G. Coronary circulation in the normal and pathologic heart. Office of the Surgeon General, Dept of the Army. Washington D.C. 1965.
- Fiss DM. Normal coronary anatomy and anatomic variations. Applied Radiology. 2007;36: 14–26.
- Loukas M, Bilinsky S, Bilinsky E, et al. Cardiac Veins: A Review of the Literature. Clinical Anatomy. 2009; 22:129–45.
- Loukas M, Groat C, Khangura R, et al. The normal and abnormal anatomy of the coronary arteries. Clin Anat. 2009; 22:114–28.
- Miynarski R, Miynarski A, Sosnowski M. Anatomical variants of left circumflex artery, coronary sinus and mitral valve can determine safety of percutaneous mitral annuloplasty. Cardiol J. 2013;20:2350240.
- Spenser J, Fitch E, Iaizzo PA. Anatomical reconstructions of the human cardiac venous system using contrast-computed tomography of perfusion-fixed specimens. J Vis Exp. 2013; (74). Doi: 10.3791/50258
- Triveliato M, Angelini P, Leachman RD. Variations in coronary artery anatomy: Normal versus abnormal. Cardiovasc Dis. 1980;7:357–70.
- Von Lüdinghausen M. The venous drainage of the human myocardium. Adv Anat Embryol Cell Biol. 2003;168;1–104.