1. Which one of the following infections is mainly responsible for recurrent exacerbation of COAD in elderly?
- Rota virus
- Mycobacterium tuberculosis
- Staphylococcus aureus
- Hemophilus influenza
Ans. d. Hemophilus influenza
Explanation
Chronic obstructive airways disease or chronic obstructive pulmonary disease (COAD/COPD).
- Disease state characterized by airflow limitation that is not fully reversible.
- Third most common cause of death and fifth most common cause of disability.
- It consist of either chronic bronchitis, chronic asthma or emphysema.
- Cigarette smoking is most common etiological factor (> 90%), infection with H. influenza, pseudomonas, Streptococcus pneumoniae, Moraxella catarrhalis increase acute exacerbation of disease. a1- antitrypsin(protease inhibitor which is produced in liver secreted into blood vessels and diffuse into lung) deficiency accounts for about 2% emphysema (mostly pan-acinar).
- Most consistent pathological finding is increased numbers of mucus secreting goblet cells in the bronchial mucosa, which blocks small airway, other mechanism of airway obstruction is due to inflammation and scarring and loss of elasticity of alveoli.
Ref: Kumar and Clerk, 7/e p835-8; Harrison, 18/e p2132
2. The following diseases have autosomal dominant inheritance, except:
- Polycystic kidney disease
- Peutz Jegher syndrome
- Von Willebrand disease
- Phenylketonuria
Ans. d. Phenylketonuria
Explanation
Autosomal dominant traits Prevalence 2–10 per 1,000 | ABO blood group system, Achondroplasia, Acute intermittent porphyria, Brachydactyly, Ehlers–Danlos syndrome, Familial breast cancer, Familial hypercholesterolemia, Familial hypertrophic cardiomyopathy, Familial malignant melanoma, Familial poliposis coli, Hereditary hemorrhagic telangiectasia, Hereditary nonpolyposis colon cancer, Hereditary spherocytosis, Hereditary eliptocytosis, Huntington's chorea, Hyperkalemic period paralysis, Hyperlipoproteinemia I, II, III, IV, Hypokalemic periodic paralysis, Malignant hyperthermia, Marfan's syndrome, Maturity onset diabetes of the young (MODY), Multiple endocrine neoplasia type 1, Multiple endocrine neoplasia type 2, Neurofibromatosis, Osteogenesis imperfecta, Peutz–Jeghers syndrome, Polycystic kidney (adult), Retinoblastoma, Rotor syndrome, Crigler–Najar type II, Tuberous sclerosis types 1 and 2, Von Hippel-Lindau syndrome, Von Willebrand disease |
Autosomal recessive traits Prevalence 2 per 1,000 | Agammaglobulinemia, Swiss type, Albinism, Alkaptonuria, Congenital adrenal hyperplasia, Crigler-Najjar type I, Cystic fibrosis, Dubin–Johnson syndrome, Familial Mediterranean fever, Fibrocystic disease of pancreas, Friedreich's ataxia, Galactosemia, Gaucher's disease, Glycogen storage disease type I-VIII, Hemochromatosis, Hemoglobinopathies, Hirschsprung's disease, Homocystinuria, Maple syrup urine disease, Mucopolysaccharidosis types I–VII, Niemann–Pick disease, Obesity, Phenylketonuria, Sickle-cell anemia, Tay–Sachs disease, Thalassemia, Wilson's disease, α1-Antitrypsin deficiency, Fragile X syndrome |
X-linked recessive traits Prevalence 1–2 per 1,000 | Hemophilia type A and type B, Duchenne type of muscular dystrophy, Color blindness, G6-phosphate-dehydrogenase deficiency, Hydrocephalus, Retinitis pigmentosa, Agammaglobulinemia, (Bruton type), Fragile X syndrome, Adrenoleukodystrophy, Becker's muscular dystrophy, Fabry disease, Hunter syndrome, Nephrogenic DI, Wiskott–Aldrich syndrome |
X-linked dominant traits | Vitamin D–resistant rickets, Familial hypophosphatemia, Blood group Xg |
Ref: Park, 21/e p763; Nelson, 19/e p383–9; Devidson, 21/e p52–5; Harrison, 16/e p373
3. A young female presents with right heart failure. On examination she has an elevated JVP with giant wave, systolic murmur at left sternal border, soft delayed P2 with an ejection sound. The ECG shows right ventricular hypertrophy. She is likely to have:
Ans. a. Pulmonary stenosis
Explanation
Pulmonary stenosis | Tricuspid regurgitation | Atrial septal defect | Ventricular septal defect |
|---|---|---|---|
Pulmonary ejection systolic murmur and a thrill in left second interspace, concentric right ventricular hypertrophy, S1 normal, wide and variable split of second heart sound, in valvular pulmonary stenosis wide ejection click audible soon after S1. C/F-Mild to moderate PS are asymptomatic, In severe stenosis dyspnea on effort. palpitation easy fatiguability and rarely chest pain. Cardiac size normal, left parasternal heave. Infundibular stenosis distinguish from valvular PS by absence of click, absence of post stenotic dilatation, relatively lower point of maximum intensity of systolic murmur in 2–3th left interspace. | Feature of TR is seen in 20–50% RHD in India. It may be organic (associated with RHD) or functional (due to pulmonary hypertension). All patient of TR having feature of pulmonary hypertension. TR associated with MS may be functional or organic but TR associated with MR is mostly organic. Both systolic and diastolic murmur. C/F- right hypochondial pain due to congested liver, fatiguability. Pancystolic murmur over left sternal border. ECG- right ventricular hypertrophy. T/T- decongestive therapy, TR may resolve following mitral vulvotomy. | Enlarged right ventricle results in parasternal impulse. Ejection systolic murmur. S1 Loud, S2 wide and fixed split P2 ECG of ostium secundum – right axis deviation with right ventricular hypertrophy. Left axis deviation beyond -300 suggest ostium primum. CXR- shows mild to moderate cardiomegaly, right atrial and right ventricular enlargement, prominent main pulmonary segment, plethoric lung field. Echo- enlarge right ventricle with paradoxical ventricular motion. Larger the shunt, more cardiomegaly, larger pulmonary and tricuspid murmur C/F- Heart failure rare in infancy. Pulmonary hypertension, may develop arrhythmia and heart failure in late adulthood. | Most common congenital cardiac lesion. 90% in communication of membranous part of ventricle. Shunting of blood from left to right ventricle. Murmur start early masking S1, pansystolic murmur at left sternal border. Ejection systolic murmur at pulmonary valve, delayed diastolic at mitral valve. S2 widely split and variable in large shunt. S3 may audible at apex. C/F- symptomatic around 6–10 weeks with CCF. Palpitation, dyspnea on exertion and frequent chest infection are main symptoms in older children. If VSD is small, left to right shunt murmur continue to be pansystolic, absence of delayed diastolic. If VSD is very small |
ECG- right axis deviation, right ventricular hypertrophy, P pulmonale – severe stenosis, Pulmonary oligemia occurs if right to left shunt at atrial level. Balloon pulmonary valvuloplasty is TOC In isolated valvular PS... surgical treatment for failure balloon valvoplasty or infundibular PS | T/T- closure of fossa ovalis percutaneously, closure recommended before school entry to prevent late complication | murmur is ejection systolic, if VSD is large left to right shunt murmur is shorter and softer and appear as ejection systolic murmur. Spontaneous closure (highest for muscular type) within 3 month in small VSD. It can complicate to infective endocarditis CXR- pulmonary plethora. T/T- control CCF, chest infection Surgery indication – CCF in infancy, LR shunt is large (pulmonary flow more than twice as systemic flow), If PS present than pulmonary atrial hypertension or aortic regurgitation. Surgery – closure of VSD with patch through right atrium. Complication of surgery:- complete heart block, bifascicular block, residual VSD | |
Ref: Ghai, 8/e p413-443
4. Nocturnal hypoxemia in COPD is due to all the following except:
- An increase in upper airway resistance because of muscle tone
- Stimulation of peripheral chemoreceptors
- Shallow breathing in REM sleep, reduced ventilation
- Inhibition of intercostals and accessory muscles in REM sleep
Ans. b. Stimulation of peripheral chemoreceptors
Explanation
In nocturnal hypoxemia the mechanism of alveolar hypoventilation:
- Inhibition of intercostal and accessary muscle in REM sleep.
- Shallow breathing in REM sleep, which reduces ventilation, particularly in severe COPD.
- An increase in upper airway resistance because of a reduction in muscle tone.
This nocturnal hypoxemia associated with further rise in pulmonary arterial pressure because of vasoconstriction, and majority of death in patient of COPD occurs during night probably due to cardiac arrhythmia. The patient may develop secondary polycythemia.
Treatment
Avoid sleeping pill. Noninvasive bilevel positive pressure ventilation.
Ref: Kumar and Clerk, 7/e p840
5. A 50-year-old male presented with acute onset dyspnea, orthopnea and pinkish frothy sputum. The clinical diagnosis is:
- Acute bronchial asthma
- Acute pulmonary edema
- Acute pulmonary embolism
- Pneumonia
Ans. b. Acute pulmonary edema
Explanation
Ref: CMDT 51/e p397, Devidson 21/e p716-18, 680
6. Pseudo membranous colitis is caused by which of the following organisms?
- Shigella
- E. coli
- Clostridium perfringens
- Clostridium difficile
Ans. d. Clostridium difficile
Explanation
Pseudomembranous Colitis
- Acute, potentially severe disease of the colon characterized by exudative plaques that cover the intestinal mucosa.
- The disease is caused by an enterotoxin produced by C. difficile, an anaerobic bacteria.
- Symptoms begin 3 days to 4 weeks after initiating antibiotic therapy. Virtually all antibiotics have been associated with this disease, but clindamycin, fluoroquinolones, and the cephalosporins are the most common offenders.
- Signs and symptoms include watery diarrhea, crampy abdominal pain, lower, abdominal tenderness, and fever, leukocytosis.
- Dehydration and electrolyte disturbances may develop in severely ill patients. Toxic megacolon and colonic perforation are rare, but serious, complications.
- Approximately 20% of patients relapse after primary treatment.
- Demonstration of C. difficile toxin in the stool or sigmoidoscopic visualization of the characteristic yellow-white plaques in an erythematous and edematous mucosa suggests the diagnosis. Biopsy of the plaques shows a mucinous, fibrinous, polymorphonuclear exudate. Most patients have disease throughout the colon; however, the disease may be confined to the right colon, and in such cases sigmoidoscopic findings are negative.
Treatment
- The first step in treatment is to discontinue unnecessary antibiotics. metronidazole is first-line therapy, vancomycin should be used in severe cases. Relapse is treated with a second course of therapy. Multiple relapses can be treated with tapering or pulsed doses of vancomycin; or probiotics including Lactobacillus or Saccharomyces boulardii, or cholestyramine.
Ref: NMS medicine, 6/e p212
7. The ventricular tachycardia can respond to all of the following except:
- D C Cardioversion
- IV Amiodarone
- IV Lidocaine
- IV Digitalis
Ans. d. IV Digitalis
Explanation
Ventricular Tachycardia (VT)
- Feature in favor of ventricular tachycardia in the differential diagnosis of board-complex tachycardia
- A history of myocardial infarction
- AV dissociation (pathognomonic)
- Capture/fusion beats (pathognomonic)
- Extreme left axis deviation
- Very broad QRS complexes (> 140 ms)
- No response to carotid sinus massage or IV adenosine
- The common causes of ventricular tachycardia include acute myocardial infarction, cardiomyopathy and chronic ischemic heart disease.
- Patients may complain of palpitation or the symptoms of low cardiac output, such as dizziness, dyspnea or syncope.
- The ECG shows tachycardia with broad, abnormal QRS complexes with a rate above 120/min.
- Prompt action to restore sinus rhythm is required which should followed by prophylactic therapy. DC cardioversion is the treatment of choice if systolic BP is less than 90 mm Hg If the arrhythmia is well tolerated, IV amiodarone maybe given as a bolus followed by an IV infusion.
- Intravenous lidocaine can be used but it can depress left ventricular function, causing hypotension or acute heart failure. Beta-blockers may be effective at suppressing VT.
- Aggravating factor like Hypokalemia, hypomagnesemia, acidosis and hypoxemia should be corrected.
Ref: Devidson, 20/e p566-67
8. Which one of the following cardiac enzymes does not remain elevated for more than 48 hours after myocardial infarction?
- Creatinine kinase MB
- Troponin T
- Lactic dehydrogenase
- Aspartate amino transferase
Ans. a. Creatinine kinase MB
Explanation
- Troponin T and Troponin I, become positive as early as 4–6 hours of onset of MI and should be abnormal by 8–12 hours. Level of troponin elevated upto 5–7 days (7–10 days in Harrison) so not useful for evaluating suspected reinfarction.
- LDH level begins to rise by 12 hours, reaches maximum at 48 hours and return to normal by 11th days.
- Aspartate amino transferase rises from normal level 5–17 to 200IU/L is useful diagnostically in the first few days then the level drops to normal after 3 days.
Ref: Walter & Israel general pathology, 7/e p715; CMDT 51/e p357
9. All the following are helpful in the management of acute pulmonary edema except :
- Administration of high flow high concentration oxygen
- Use of Morphine
- Administration of loop diuretics
- Make the patient lie in supine position
Ans. d. Make the patient lie in supine position
Treatment of Pulmonary Edema
- Patient should be sitting position with leg dangling over side of bed.
- Oxygen is delivered by mask or to obtain arterial Po2 > 60 m Hg. If needed endotracheal intubation and mechanical ventilation may be needed.
- Morphine is highly effective. It increase venous capitance, lowering LA pressure, and relieves anxiety, which can reduce the efficiency of ventilation. It should be avoid in patient with opioid induced pulmonary edema.
- IV diuretics (furosemide and bumetanide) indicated even patient is not exhibited prior fluid retention.
- Nitrate therapy accelerates clinical improvement by reducing both BP and LV filling pressure. It ameliorate dyspnea rapidly. IV nesiritide when given as a bolus followed by infusion, improves dyspnea more rapidly than IV nitroglycerine. Norepinephrine, dopamine or dobutamin can be given to increase BP which maybe due to nitroglycerin induced hypotension.
- β-adrenergic agonist or IV amynophyllin may useful to reduce bronchospasm.
Ref: CMDT, 51/e p398
10. All of the following aggravate heart failure except:
- Intercurrent Infection
- Arrhythmia
- Fluid restriction
- Anemia
Ans. c. Fluid restriction
Explanation
Factors That May Precipitate Acute Decompensation in Patients with Chronic Heart Failure:
- Dietary indiscretion
- Myocardial ischemia/infarction
- Arrhythmias (tachycardia or bradycardia)
- Discontinuation of Heart Failure therapy
- Infection
- Anemia
- Drug (Calcium antagonists (verapamil, diltiazem) Beta blockers, NSAID, Antiarrhythmic agents [all class I agents, sotalol (class III)], Anti-TNF antibodies
- Alcohol consumption
- Pregnancy
- Worsening hypertension
- Acute valvular insufficiency.
Ref: Harrison, 18/e p1907
11. The following are true for hypertrophied cardio myopathy except:
- Systolic murmurs
- Triple apical impulse
- Diastolic murmur
- Jerky carotid pulse
Ans. c. Diastolic murmur
Explanation
Some important point regarding Hypertrophic cardiomyopathy:
- Hypertrophic cardiomyopathy is characterized by marked left ventricular hypertrophy in the absence of other causes, such as hypertension or valve disease.
- This was previously termed hypertrophic obstructive cardiomyopathy (HOCM), as distinguished from nonobstructive hypertrophic cardiomyopathy. Other terms that have been used include asymmetric septal hypertrophy (ASH) and idiopathic hypertrophic subaortic stenosis (IHSS).
- The prevalence is 1:500 adults. Autosomal dominant pattern, and spontaneous mutations also arise.
- Characterized hemodynamically by diastolic dysfunction, originally attributed to the hypertrophy, fibrosis, and intraventricular gradient when present.
- Usually presents between the ages of 20 and 40 years.
- Dyspnea on exertion MC, orthopnea, and paroxysmal nocturnal dyspnea
- Chest pain with either an atypical or typical exertional pattern occurs.
- Sudden death from ventricular tachycardia or fibrillation. It is the most common lesion found at autopsy of young athletes dying suddenly.
- Loud fourth heart sound and prominent ‘a’ wave in JVP - due to decreased ventricular compliance.
- The electrocardiogram usually shows left ventricular hypertrophy, often with prominent septal Q waves. Systolic anterior motion (SAM) of the mitral valve is a classic finding on the echocardiogram.
- Jerky pulse.
- Triple apical impulse at the apex (due to prominent atrial filling wave and early and late systolic impulses).
- Mid-systolic murmur at the base. Murmur may be enhanced by Valsalva maneuver, or standing may be decreased by squatting or handgrip.
- Pansystolic murmur (due to mitral regurgitation) at the apex.
Ref: Harrison, 18/e p1968; CMDT, 51/e p404
12. ‘Shrinking lungs ‘in systematic lupus erythematosis is attributed to:
- Fibrosing alveolitis
- Vasculitic infarcts
- Pulmonary emboli
- Diaphragmatic myopathy
Ans. d. Diaphragmatic myopathy
Explanation
Clinical Feature of SLE or Presentation of SLE
System involved | Presentation |
|---|---|
Systemic | Fatigue, malaise, fever, anorexia, weight loss |
Musculoskeletal | Arthralgia and symmetrical arthritis often are features of acute SLE, but the rare joint deformities (Jaccoud's arthropathy) that occur, are a function of tendon or ligament laxity rather than erosive joint disease. Myalgia, Nonerosive polyarthritis, Hand deformities, Myopathy/myositis, Ischemic necrosis of bone are other features |
Cutaneous | Photosensitivity, Malar rash(butterfly rash), Oral ulcers, alopecia, Discoid rash(coin-shaped lesions with hyperemic margins, Central atrophy, and depigmentation), Vasculitis rash, other {e.g., urticaria, subacute cutaneous lupus(associated with the Ro antibody)} |
Hematologic | Anemia (chronic disease), Leukopenia (<4000/L), Lymphopenia (<1500/L), Thrombocytopenia (100,000/L), Lymphadenopathy, Splenomegaly, Hemolytic anemia |
Neurologic | Reactive depressions, Psychoses (antibody to ribosomal P protein), Cognitive disorder, Mood disorder, Headache, Seizures, Mono-, polyneuropathy, Stroke, TIA, Acute confusional state or movement disorder, Aseptic meningitis, Myelopathy |
Cardiopulmonary | Pleurisy, pericarditis, effusions, myocarditis (conduction abnormalities, arrhythmias, and CHF), endocarditis, Lupus pneumonitis, Coronary artery disease, Interstitial fibrosis, Pulmonary hypertension, ARDS, hemorrhage, Diaphragmatic fibrosis or diaphragm dysfunction may manifest as ‘shrinking lung syndrome’. It has restrictive picture on pulmonary function testing |
Renal | Proteinuria 500 mg/24 h, cellular casts, Nephrotic syndrome, End-stage renal disease |
Gastrointestinal | Nonspecific (nausea, mild pain, diarrhea), Abnormal liver enzymes, Vasculitis |
Thrombosis | Venous, Arterial |
Ocular | Sicca syndrome, Conjunctivitis, Episcleritis, Vasculitis |
Ref: NMS Medicine, 6/e p483-6; Kumar and Clerk, 7/e p543
13. Which of the following is a longer acting insulin?
- Aspart
- Glulisine
- Lispro
- Glargine
Ans. d. Glargine
Explanation
Type of Insulin
Type | Onset (hour) | Peak (hour) | Duration (hour) |
|---|---|---|---|
Rapid acting | |||
Insulin lispro | 0.2–0.3 | 1–1.5 | 3–5 |
Insulin aspart | 0.2–0.3 | 1–1.5 | 3–5 |
Insulin glulisine | 0.2–0.4 | 1–2 | 3–5 |
Short acting | |||
Regular (soluble)insulin | 0.5–1 | 2–3 | 6–8 |
Intermediate acting | |||
Insulin –zinc suspension or Lente | 1–2 | 8–10 | 20–24 |
Natural protamine hagedom or isophane insulin | 1–2 | 8–10 | 20–24 |
Long insulin | |||
Insulin glargine | 2–4 | 24 | |
Insulin detemir | 1–4 | 20–24 | |
Ref: KDT, 7/e p263
14. Which one of the following is not a risk factor for alcoholic liver disease?
- Gender
- Hepatitis C
- Quality of alcohol
- Malnutrition
Ans. c. Quality of alcohol
Explanation
Risk Factors for Alcoholic Liver Disease
Risk Factor | Comment |
|---|---|
Quantity | In men, 40–80 g/d of ethanol produces fatty liver; 160 g/d for 10–20 years causes hepatitis or cirrhosis. Only 15% of alcoholic develop alcoholic liver disease |
Gender | Women exhibit increased susceptibility to alcoholic liver disease at amounts >20 g/d |
Hepatitis C | HCV infection concurrent with alcoholic liver disease is associated with younger age for severity, decreased survival |
Genetics | Genepolymorphisms may include alcohol dehydrogenase, cytochrome P4502E1, and those associated with alcoholism |
Malnutrition | Alcohol injury does not require malnutrition, but obesity and fatty liver from the effect of carbohydrate on the transcriptional control of lipid synthesis and transport may be factors. |
Ref: Harrison, 18/e p2589
15. All of the following are true about renal cell carcinoma except:
- Secondaries more common than Primary
- More common in males
- Mainly arise from renal medulla
- Mostly occur in sixth and seventh decade
Ans. a. Secondaries more common than Primary
Explanation
Renal Cell Carcinoma
- Account for 90–95% of malignant neoplasms arising from the kidney.
- The male to female ratio is 2:1.
- Peak incidence between the ages of 50 and 70 years, may be at any age.
- Associated with cigarette smoking. Risk increased in patients who have acquired cystic disease of the kidney associated with end-stage renal disease, and for those with tuberous sclerosis.
- Clear cell carcinoma (60% of cases), papillary tumors (5–15%), chromophobic tumors (5–10%), oncocytomas (5–10%), and collecting or Bellini duct tumors (<1%).
- Papillary tumors tend to be bilateral and multifocal.
- Signs and symptoms :-classic triad include hematuria, abdominal pain, and a flank or abdominal mass(10–20% of cases). Other symptoms are fever, weight loss, anemia, and a varicocele. Most commonly detected as an incidental finding on a radiograph.
- A spectrum of paraneoplastic syndromes has been associated with these malignancies, including erythrocytosis, hypercalcemia, nonmetastatic hepatic dysfunction (Stauffer syndrome), and acquired dysfibrinogenemia. Erythrocytosis is noted at presentation in only about 3% of patients. Anemia, a sign of advanced disease, is more common.
- Of solid tumor lung cancer (20%), breast (10%), stomach (10%), contralateral kidney 10%, lymphoma metastasize to kidney.
Ref: Harrison, 18/e p793; CMDT, 51/e p1594
16. Which one of the following is a renal complication of sickle cell anaemia?
- Pyuria
- Acute papillary necrosis
- Reduced GFR
- Inability to acidify urine
Ans. b. Acute papillary necrosis
Explanation
Sickle Cell Syndromes
- Caused by a mutation in the β-globin gene that changes the sixth amino acid from glutamic acid to valine.
- Most patients with sickling syndromes suffer from hemolytic anemia, with hematocrits from 15 to 30%, and significant reticulocytosis.
- Granulocytosis is common.
- Usually asymptomatic, anemia and painful crisis are rare.
- Painful crises, (Intermittent episodes of vasoocclusion in connective and musculoskeletal structures produce ischemia manifested by acute pain and tenderness, fever, tachycardia, and anxiety) are the most common clinical manifestation. Repeated crises(>3 per year) requiring hospitalization.
- Spleen is frequently lost within the first 18–36 months of life, causing susceptibility to infection, particularly by pneumococci.
- Splenic sequestration crisis (Acute venous obstruction of the spleen), a rare occurrence in early childhood, may require emergency transfusion and/or splenectomy.
- Renal papillary necrosis invariably produces isosthenuria. More widespread renal necrosis leads to renal failure in adults, a common late cause of death.
- Bone and joint ischemia can lead to aseptic necrosis, especially of the femoral or humeral heads; chronic arthropathy; and unusual susceptibility to osteomyelitis( Salmonella).
- The hand-foot syndrome is caused by painful infarcts of the digits and dactylitis.
- Stroke is especially common in children.
- Priapism, due to infarction of the penile venous outflow tracts; permanent impotence is a frequent consequence.
- Acute chest syndrome is a distinctive manifestation characterized by chest pain, tachypnea, fever, cough, and arterial oxygen desaturation.
Ref: Harrison, 18/e p855-6
17. A 65-year-old male presents with flexed posture, slowness of gait, expression less face and tremor 4–6 Hz in hand. He is most likely suffering from:
- Alzheimer's disease
- Huntington's disease
- Parkinson's disease
- Lathyrism
Ans. c. Parkinson's disease
Explanation
Some important point regarding Parkinsonism:
- Cause is unknown, Sex incidence is about equal. It is less common in cigarette smokers.
- Depletion of the pigmented dopaminergic neurons in the substantia nigra, hyaline inclusions in nigral cells (Lewy bodies).
- The classical syndrome of tremor, rigidity and bradykinesia may be absent initially, when non-specific symptoms of tiredness, aching limbs, mental slowness, depression and small handwriting (micrographia) may be noticed.
- Presentation is almost always unilateral, gradual bilateral involvement is the rule. Resting tremor in an upper limb being a common presenting feature and may also affect the legs, mouth and tongue.
- Rigidity, or increased muscular tone, causes stiffness and a flexed posture
- Speech becomes softer and indistinct in advanced disease.
- Postural righting reflexes are impaired early, falls tend not to occur until later.
- Paucity of facial expression (hypomimia) and the blink reflex may be exaggerated and fail to habituate (glabellar tap sign).
- Sensation is normal and intellectual faculties are not affected initially.
- Physical abnormality
- General
- Expressionless face
- Greasy skin
- Soft, rapid, indistinct speech
- Flexed posture
- Impaired postural reflexes
- Gait
- Slow to start walking
- Shortened stride
- Rapid, small steps, tendency to run (festination)
- Reduced arm swing
- Impaired balance on turning
- Tremor: Resting 4–6 Hz
- Usually first in fingers/thumb
- Coarse, complex movements, flexion/extension of fingers
- Abduction/adduction of thumb
- Supination/pronation of forearm
- May affect arms, legs, feet, jaw, tongue
- Intermittent, present at rest and when distracted
- Diminished on action
- Tremor: Postural 8–10 Hz
- Less obvious, faster, finer amplitude
- Present on action or posture, persists with movement
- Rigidity
- Cogwheel type, mostly upper limbs
- Plastic (leadpipe) type, mostly legs
- Bradykinesia
- Slowness in initiating or repeating movements
- Impaired fine movements, especially of fingers
Some Important Point Regarding Huntington's Disease
- Autosomal dominant disorder affecting both males and females, and usually starting in middle adult life due to expansion of a trinucleotide repeat on chromosome 4. Slightly different features of the disease occur, depending on whether the abnormal gene is inherited from father or mother.
- In juvenile-onset disease, there maybe parkinsonian features with rigidity. Seizures may occur late in the disease.
Some Important Point Regarding Alzheimer's Disease
- Most common cause of dementia, occurring mostly in patients over 45 years
- About 15% of cases are familial. Early- onset; autosomal dominant pattern; and a later-onset group whose inheritance is not so clear.
- Impairment of delayed recall, i.e. the inability to retrieve (remember) information acquired in the past. Both short-term and long-term memory are affected but defects in the former are usually more obvious.
- Later: Typical features are apraxia, visuo-spatial impairment and aphasia. Depression is common.
Ref: Devidson, 20st/1218-22
18. A 19-year-old female presents with a history of repeated falls in the past one year. A Diagnosis of epilepsy is supported by all of the following except:
- Occurs only in the presence of the mother
- Occurs when watching the TV
- Acute and chronic hypocalcemia
- Aura before the attack
Ans. c. Acute and chronic hypocalcemia
Explanation
Among above given choice all choices are correct and support diagnosis of epilepsy. If we see the table of harisson at page no 3256, hypocalcemia is causes of epilepsy in only neonates. While other books write as cause but age not mentioned. In this question, age of female is 19 years so from my point of view answer is option ‘c.’ option ‘a’ maybe correct because it cause emotional factor. Option ‘b’ is correct as per CMDT and Devidson. Option ‘d’ is correct because aura may proceed generalized seizure.by few second and minute.
Some important point regarding recurrent seizure (epilepsy)
- Trigger factor for seizures:
- Sleep deprivation
- Missed meal, menstruation
- Emotional stress
- Alcohol (particularly withdrawal)
- Recreational drug misuse
- Flickering lights, including TV and computer screens (primary generalised epilepsies only)
- Intercurrent infections and metabolic disturbances, fever
- Uncommonly: loud noises, music, reading, hot baths.
Causes of secondary generalized epilepsy | Causes of partial seizure |
|---|---|
|
|
Ref: Harrison, 18/e p3256; CMDT, 51/e p971; Devidson, 21/e p1172-74
19. Bell's Palsy is:
- Usually bilateral
- Usually associated with normal nerve conduction studies in early stages
- Presenting feature of acoustic neuroma
- Associated with herpetic vesicles in ipsilateral ear
Ans. c. Presenting feature of acoustic neuroma
Explanation
Some important point regarding Bell's Palsy:
- The most common form of facial paralysis
- Idiopathic, affect all ages and both sexes.
- Abrupt onset, maximal weakness being attained by 48 hour as a general rule.
- Inflammation of the facial nerve with mononuclear cells, consistent with an infectious or immune cause. Herpes simplex virus (HSV) type 1 DNA was frequently detected in endoneurial fluid and posterior auricular muscle. Reactivation of varicella zoster virus is associated in one-third of cases. also reported among recipients of inactivated intranasal influenza vaccine.
- Pain behind the ear may precede the unilateral paralysis for 1–2 days (lower motor neuron type). Unilateral loss of taste sensation, hyperacusis may be present.
- CSF lymphocytosis.
- Approximately 80% of patients recover within a few weeks or months.
- Electromyography may be of some prognostic value.
- Diagnosis clinically in patients with
- a typical presentation,
- no risk factors or preexisting symptoms for other causes of facial paralysis,
- absence of cutaneous lesions of herpes zoster in the external ear canal (Ramsay Hunt syndrome, caused by reactivation of herpes zoster in the geniculate ganglion, consists of a severe facial palsy associated with a vesicular eruption in the external auditory canal and sometimes in the pharynx and other parts of the cranial integument; often the eighth cranial nerve is also affected)
- a normal neurologic examination with the exception of the facial nerve.
- Treatment: Symptomatic
- the use of paper tape to depress the upper eyelid during sleep and prevent corneal drying, and
- massage of the weakened muscles
- glucocorticoids, given as prednisone.
Although all option is not absolute correct but option ‘c’ is partially correct. Now it's upon you to choose your answer.
Ref: Harrison, 18/e p3362; Devidson, 21/e p1228; CMDT, 52/e p1028
20. Which of the following regarding hemophilias is not correct?
- Hemophilia A is commoner than Hemophilia B
- Hemophilia is a X-linked recessive disorder
- Hemophilia B is commoner than Hemophilia A
- Bleeding normally affects joints
Ans. c. Hemophilia B is commoner than Hemophilia A
Explanation
Some important point regarding Hemophilia:
- X-linked recessive due to mutations in the F8 gene (Hemophilia A or classic Hemophilia) or F9 gene (Hemophilia B).
- Hemophilia A represents 80% of all cases.
- Male subjects are clinically affected; women are generally asymptomatic.
- Family history of the disease is absent in 30% of cases.
- In the severe and moderate forms, the disease is characterized by bleeding into the joints (hemarthrosis), soft tissues, and muscles after minor trauma or even spontaneously. Patients with mild disease experience infrequent bleeding that is usually secondary to trauma.
- The diagnosis is made after specific determination of factor VIII or factor IX clotting activity.
- Early in life, bleeding may present after circumcision or rarely as intracranial hemorrhages.
- The most common bleeding manifestations are the acute painful or recurrent hemarthroses, which can affect every joint but mainly affect knees, elbows, ankles, shoulders, and hips. To avoid pain, the patient may adopt a fixed position, which leads eventually to muscle contractures.
- Hematomas into the muscle leads to compartment syndrome.
- Bleeding into the oropharyngeal spaces, central nervous system (CNS), or the retroperitoneum is life threatening.
- Pseudo tumor syndrome due to retroperitoneal hemorrhage and calcification.
- Hematuria is self-limiting.
- Prolongation of the aPTT assay. Patients with Hemophilia have normal bleeding times and platelet counts.
Ref: Harrison, 17/e p726
21. Which one of the following diseases is deficient in Glycoprotein IIbIIIa (GpIIbIIIa) platelet receptor?
- Von Willebrand's disease
- Glanzmann's disease
- Bernard-Souler syndrome
- Storage pool disease
Ans. b. Glanzmann's disease
Explanation
Primary Hemostatic (Platelet Plug) Disorders
Defects of Platelet Adhesion
- Von Willebrand disease
- Bernard-Soulier syndrome (absence of dysfunction of GpIb-IX-V).
Defects of Platelet Aggregation
- Glanzmann's thrombasthenia (absence or dysfunction of GpIIbIIIa)
- Afibrinogenemia.
Defects of Platelet Secretion
- Decreased cyclooxygenase activity
- Drug-induced (aspirin, nonsteroidal antiinflammatory agents, thienopyridines).
- Inherited.
- Granule storage pool defects
- Inherited.
- Acquired.
- Nonspecific inherited secretory defects.
- Nonspecific drug effects.
- Uremia.
- Platelet coating (e.g., paraprotein, penicillin).
Defect of Platelet Coagulant Activity
Scott's syndrome.
Ref: Harrison, 18/e p460
22. Which of the following is not found in severe Beta thalassemia?
- Hepatospleenomegaly
- Growth retardation
- Bone deformities
- Hemoglobin level of 7 to 8 gm percent
Ans. d. Hemoglobin level of 7 to 8 gm percent
Explanation
Some important points regarding β-thalassemia:
- Thalassemia is an inherited disorder (autosomal recessive traits) in which there is partial or complete failure to synthesize a specific type of globin chain.
β-thalassemia major:
- Most common type of thalassemia
Features of Thalassemia Major
- Children develop characteristic ‘chipmunk’ faces due to maxillary marrow hyperplasia and frontal bossing, prominent parietal eminence, flattened vault, prominent malar eminence, depressed nasal bridge, puffy eyes. Thinning of cortex and widening of madula and pathologic fracture of long bones and vertebrae may occur. Earliest changes occur in the small bones of the hand which shows rectangular appearance. Growth retardation, hemolytic anemia, hepatosplenomegaly, leg ulcers, gallstones, irregular fever, high-output congestive heart failure may occur. Erythroid hyperplasia can become exuberant and produce masses of extramedullary erythropoietic tissue in the liver and spleen. Usually prove fatal by age 30 years
Laboratory Investigations
- Hemoglobin: Usually 2–6 g%, absence or gross reduction of the amount of hemoglobin A, raised levels of hemoglobin F, HbA2 normal.
- Cells: Hematocrit is reduced. MCV, MCH, or MCHC are low. Reticulocytes count elevated. Mild leukocytosis and thrombocytosis. Evidence of severe red cell dysplasia.
- Peripheral smear: RBC shows hypochromia, anisocytosis, poikilocytosis; microcytes, target cells, tear drop cells; basophilic stippling; fragmented RBC, Howell–Jolly bodies and Heinz bodies; early, intermediate, late normoblast are characteristic findings.
- Bone marrow: Hypercellular with erythroid hyperplasia, increased stippled erythroblast and sideroblasts; hemosiderin deposition increased.
- Osmotic fragility: Decreased (increase in hereditary spherocytosis).
- Serum bilirubin: Moderately elevated (1–3 mg/dL);
- Urinary urobilinogen moderately increased.
- Fecal stercobilinogen markedly increased.
- Serum iron: High; iron-binding capacity reduced; ferritin level increases; free erythrocyte porphyrin level is normal.
- Radiological picture.
- Skull bone shows ‘hair-on-end’ appearance due to vertical striations from widening of the diploic space and atrophy of the outer table of the skull.
- Evidence that both parents have thalassemia minor.
Treatment of Beta-Thalassemia Major
Clinical problem | Management |
|---|---|
Erythropoietic failure | Allogenic bone marrow transplantation from human leucocyte antigen (HLA)-compatible sibling, transfusion to maintain Hb >100 g/L, folic acid 5 mg daily |
Iron overload | Iron therapy forbidden, deferoxamine therapy (parental preparation) Deferiprone in oral formulation |
Splenomegaly causing mechanical problems, excessive transfusion needs | Splenectomy |
Newer approach | Gene manipulation, gene therapy (under trial) |
Ref: Harrison, 18/e p858; CMDT, 2012/e p478–479; Ghai, 6/e p09; 7/e p307
23. Polycythemia may be seen with all of the following except:
- Heavy smokers
- High altitude
- Renal cell carcinoma
- Congenital heart disease with left to right shunt
Ans. d. Congenital heart disease with left to right shunt
Explanation
Causes of Polycythemia
Primary | |
|---|---|
Polycythemia vera Mutation in erythropoietin receptor High oxygen-affinity- hemoglobin | |
Secondary | |
Due to an appropriate increase in erythropoietin | Due to an in appropriate increase in erythropoietin |
High altitude Pulmonary disease Hypoxia, Carbon monoxide poisoning Right to left cardiac or vascular shunts Heavy smoking Increase affinity of hemoglobin, e.g. familial polycythemia | Renal disease – renal cell carcinoma, Wilm's tumors, Hepatocellular carcinoma Adrenal tumor Cerebellar hemangioblastoma Massive uterine myoma Meningioma Bronchogenic carcinoma |
Relative (due to decrease plasma volume, normal red cell mass) | |
Stress or spurious polycythemia Dehydration Burn Diuretics Ethanol abuse, androgens or tobacco abuse | |
Ref: Devidson, 21/e p999; Harrison, 18/e p899; Kumar Clerk, 7/e p419
24. Hypertension and hypokalemia are observed in which one of the following conditions?
- Renal artery stenosis
- Cushing's syndrome
- Pheochromocytoma
- Barter's syndrome
Ans. a. Renal artery stenosis
Explanation
Renal artery stenosis | Barter syndrome (Similar to loop diuretic) | Pheochromocytoma | Cushing syndrome |
|---|---|---|---|
Atherosclerosis is most common cause in older patient (M: F = 2:1) while fibromuscular dysplasia is common in younger (<50years) patient. F>M,; PAN and Takayasu disease may associated with it. Hypertension is sever or recent onset or difficult to control.; Kidneys are asymmetrical in size; Flash pulmonary edema occurs repeatedly ; There is peripheral vascular disease of lower limbs ; Renal function has deteriorated on ACE inhibitors; Acute loin pain with dipstick hematuria; Hypokalemia due to hyperaldosteronism; Mild metabolic alkalosis; Elevated plasma renin level | Metabolic alkalosis, hypokalemia, hypercalciuria; magnesium wasting may occur; normal blood pressure; elevated plasma renin and aldosterone; primary defect is impairment of sodium and chloride reabsorption in the thick ascending limb of the loop of Henle.; high urinary potassium and chloride | Derived from chromaffin cells; Located primarily in the adrenal medulla; They also are located in sympathetic ganglia and elsewhere in the adrenal medulla produce epinephrine and norepinephrine; the extra-adrenal chromaffin cells make only norepinephrine; sporadic or familial MEN II (Sipple's syndrome) - Pheochromocytoma and medullary carcinoma of the thyroid; hyperparathyroidism Maybe associated with Neurofibromatosis and Von Hippel-Lindau disease. Mostly single tumors. A useful ‘rule of tens’ in this condition: ~10% are malignant, ~10% are extra-adrenal (i.e. elsewhere in the sympathetic chain) and ~10% are familial, and 1%–3% are in the chest or neck. Approximately 20% are multiple | MC cause is corticotrope pituitary microadenoma, due to excessive activation of glucocorticoid receptor. C/F-Weight gain, central obesity, rounded face, fat pad on back of neck ('buffalo hump'), moon face, Facial plethora, thin and brittle skin, easy bruising, broad and purple, stretch marks, acne, Hirsutism, Osteopenia, osteoporosis (vertebral fractures), decreased linear growth in children, Weakness, proximal myopathy (prominent atrophy of gluteal and upper leg muscles), Hypertension, hypokalemia, edema, atherosclerosis, Glucose intolerance/diabetes, dyslipidemia, Decreased libido, in women |
C/F- Hypertension is paroxysmal in approximately 50% of cases. Palpitation, headache, nervousness, tremor, sweating, weight loss The diagnosis is often suggested by the paroxysmal nature of the symptoms, caused by variations in the function of the tumor. Attacks typically last less than 1 hour and maybe precipitated by exercise, induction of anesthesia, urination or palpation of the abdomen; Other feature are Anxiety and panic attacks, Pallor, Nausea, Abdominal pain, Weakness, Paradoxical response to antihypertensive drugs, Polyuria and polydipsia, Constipation, Orthostatic hypotension, Dilated cardiomyopathy, Erythrocytosis, Elevated blood sugar, Hypercalcemia | amenorrhea (due to cortisol-mediated inhibition of gonadotropin release), Irritability, emotional lability, depression, sometimes cognitive defects, in severe cases, paranoid psychosis, Increased susceptibility to infections, increased white blood cell count, eosinopenia, hypercoagulation with increased risk of deep vein thrombosis and pulmonary embolism | ||
In this question hypokalemia and hypertension found in both option ‘a’ and option ‘b’. I will like to go with option ‘a’ because in Cushing syndrome hypertension is less common.
Ref: Kumar and Clerk, 7/e p665; Devidson, 21/e p497; NMS medicine, 6/e 273, 423-4, 431, 432; Harrison, 18/e p2897, 2963
25. In Endemic Cretinism:
- Deafness is common
- Treatment with thyroxine in early neonatal period results in normal neurological development
- Thyroid antibodies are present in high titres
- Treatment of pregnant women with antithyroid drugs is an important cause
Ans. a. Deafness is common
Explanation
Endemic Cretinism
- Is a disorder associated with endemic goiter and severe iodine deficiency with characteristic clinical feature like deaf mutism, squint, mental retardation, and characteristic spastic or rigid neuromuscular disorder. Two types :
- Neurological cretinism:
- Characterized by deaf mutism, squint, proximal spasticity, and rigidity more in lower extremity.
- Disorder of stances and gait with preservation of vegetative functions, occasional sign of cerebellar or occulomoter disturbance or sever mental deficiency
- Myxedematous cretinism :-
- Retard psychomotor development, very short stature, coarse facial feature, and myxedema without deaf -mutism.
- Pathogenesis of it is poorly understand.
Ref: Ghai, 8/e p519
26. In a stable insulin dependent (Type-I) Diabetes Mellitus patient, an increased daily dose of insulin is likely to be required in:
- Chronic renal failure
- Third trimester of pregnancy
- Treatment with propranolol
- Weight loss
Ans. b. Third trimester of pregnancy
Explanation
- Common factors that need to increase insulin doses are infections, injuries, emotional stress, excessive alcohol intake, and intercurrent illness.
- Insulin requirements of women with type 1 diabetes rise considerably.
- As in all patients with diabetes treated with insulin, careful glucose monitoring is esssential.
- Ketoacidosis during pregnancy is dangerous for the mother and is associated with a high fetal mortality rate.
- Pregnancy is associated with a worsening of diabetic complications, most notably retinopathy so careful eye screening is required throughout pregnancy.
Ref: Devidson, 20/e p826-7; NMS medicine, 6/e p409
27. Pheochromocytoma is characterised by the following features except:
- It arises from the chromaffin cells of adrenal medulla
- It may be a part of multiple endocrinal neoplasia type II
- It may lead to hypertensive encephalopathy and cause convulsions
- It is a 5-HT secreting tumor
Ans. d. It is a 5-HT secreting tumor
Explanation
Some Important Point Regarding Pheochromocytoma
| |
Clinical manifestations of pheochromocytoma and paraganglioma | |
Blood pressure | Hypertension: paroxysmal or sustained; orthostasis; hypotension/shock |
Vasospasm | Cyanosis, Raynaud syndrome, gangrene; severe radial artery vasospasm with thready pulse |
Multisystem crisis | Severe hypertension/hypotension, fever, encephalopathy, ARDS, renal failure, hepatic failure, death |
Cardiovascular | Palpitations, dysrhythmias, chest pain, acute coronary syndrome, cardiomyopathy, heart failure |
Gastrointestinal | Abdominal pain, nausea, vomiting, weight loss, intestinal ischemia; pancreatitis, cholecystitis, jaundice,constipation, toxic megacolon |
Metabolic | Hyperglycemia, lactic acidosis, fever |
Neurologic | Headache, paresthesias, numbness, dizziness, CVA, TIA, hemiplegia, hemianopsia, seizures, hemorrhagic stroke; compression syndrome due to compression in different part because metastasis |
Pulmonary | Dyspnea; hypoxia |
Psychiatric | Anxiety attacks; depression; chronic fatigue; psychosis |
Renal | Renal insufficiency, nephrotic syndrome, malignant nephrosclerosis |
Skin | Apocrine sweating during paroxysms, drenching sweats as attack subsides; eczema; mottled cyanosis |
Thyroid | Paroxysmal thyroid swelling |
Ectopic hormones | ACTH (Cushing syndrome); VIP (Verner-Morrison syndrome); PTHrP (hypercalcemia); erythropoietin (erythrocytosis) |
Children | More commonly have sustained hypertension, diaphoresis, visual changes, seizures, edematous or cyanotic hands; more commonly harbor germline mutations, |
Women | More symptomatic than men: more frequent headache, weight loss, numbness, dizziness, tremor, anxiety, and fatigue |
Pregnancy | Hypertension mimicking eclampsia; hypertensive multisystem crisis during vaginal delivery; postpartum shock or fever; having high mortality |
laboratory finding | Leukocytosis, erythrocytosis, eosinophilia, ↑ ESR, ↑ blood Sugar |
Ref: CMDT, 52/e p1066-67
28. Following are the hallmarks of Cushing's disease except:
- There is a bilateral adrenal hyperplasia secondary to excessive pituitary ACTH
- It generally occurs from an acidophilic pituitary adenoma
- Manifestations are attributed to gluconeogenesis
- Urinary free cortisol and 17-hydrosteroids are elevated
Ans. b. It generally occurs from an acidophilic pituitary adenoma
Explanation
Some important point regarding Cushing's syndrome:
- F/M: 3:1.
- Most common cause of spontaneous Cushing's syndrome is bilateral adrenal hyperplasia (also known as Cushing's disease), which is caused by increased secretion of ACTH by a corticotroph adenoma (baophillic adenoma) of the pituitary gland. Excess production of ACTH by the pituitary gland is Cushing's disease. Acidophilic adenoma of pitutatry gland secrets excess growth hormone and cause acromegaly and gigantism.
- Clinical feature
- Central obesity is caused due to effect of excess glucocorticoid levels on fat distribution. Most of them accumulates in the face, neck, and trunk, while the limbs remain thin. The ‘plethoric moon face’, ‘buffalo hump’ (cervical fat pad), and supraclavicular fat pads contribute to the ‘cushingoid’ appearance.
- Hypertension, decreased glucose tolerance is common; 20% develops overt diabetes due to increased hepatic gluconeogenesis and decreased peripheral glucose utilization caused by elevated levels of glucocorticoid.
- Excess of androgen in women may cause oligomenorrhea, hirsutism, purple striae, erectile dysfunction in male.
- Muscle wasting and weakness due to catabolic effects of cortisol on muscle protein.
- Osteoporosis is a frequent result of cortisol excess. It is caused by increased bone catabolism and perhaps by the inhibitory effects of cortisol on collagen synthesis and calcium absorption.
- Susceptibility to bruising is probably caused by enhanced capillary fragility.
- Psychiatric disturbances, Growth retardation in children may be severe.
- Investigation
- The overnight low-dose dexamethasone suppression test is an initial screening procedure. Patients with an abnormal dexamethasone suppression test require further investigation, which includes a 24–hours urine collection for free cortisol and creatinine.
- An abnormally high 24-hours urine free cortisol or free cortisol to creatinine ratio confirm hypercortisolism. In pregnancy 17-hydroxycor-ticosteroids remain normal and diurnal variability of serum cortisol is normal.
- Leukocytosis, with a relatively low percentage of lymphocytes and eosinophils, and ↑serum glucose level.
- Loss of the normal diurnal variation of cortisol and an increase in the evening level are more consistent findings. The serum cortisol level in normal individuals is highest in early morning low at midnight.
- The 24-hours urinary free cortisol excretion rate is increased in most patients with Cushing's syndrome. This test is the most useful indicator of daily cortisol secretion.
- ACTH measurement may help differentiate the causes of Cushing's syndrome. It is slightly elevated in patients with Cushing's disease and may be markedly elevated in patients with ectopic ACTH production.
Ref: CMDT, 52/e p1158; NMS medicine, 6/e p420-22
29. Galactorrhea maybe caused by treatment with:
- Isoniazid
- Spironolactone
- Haloperidol
- Ketoconazole
Ans. c. Haloperidol
Explanation
Condition Causing Galatorrhea are same as Causing Hyperprolectinoma
Physiologic hypersecretion |
|
Hypothalamic–pituitary stalk damage | Tumors
Empty sella Lymphocytic hypophysitis Adenoma with stalk compression Granulomas Rathke's cyst Irradiation Trauma
|
Pituitary hypersecretion | Prolactinoma Acromegaly |
Systemic disorders | Chronic renal failure Hypothyroidism Cirrhosis Pseudocyesis Epileptic seizures |
Drug-induced hypersecretion | Dopamine receptor blockers
Dopamine synthesis inhibitors
Catecholamine depletors
Opiates H2 antagonists
Imipramines
Serotonin reuptake inhibitors
Calcium channel blockers
|
Ref: Harrison, 17/e p2205,18/e
30. Antibodies diagnostic of systemic lupus erythematosus are:
- dsDNA antibodies
- Anti-centromere antibodies
- Anti-histone antibodies
- SCL-70 antibodies
Ans. a. dsDNA antibodies
Explanation
Antibody in SLE
Antibody | Prevalence | Clinical Utility |
|---|---|---|
Antinuclear antibodies | 98 | Best screening test; repeated negative tests make SLE unlikely |
Anti-dsDNA | 70 | High titers are SLE-specific and in some patients correlate with disease activity, nephritis, vasculitis |
Anti-Sm | 25 | Specific for SLE, most patients also have anti-RNP |
Anti-RNP | 40 | Not specific for SLE |
Anti-Ro (SS-A) | 30 | Nonspecific, associated with sicca syndrome, predisposes to subacutecutaneous lupus, and to neonatal lupus with congenital heart block; associated with decreased risk for nephritis |
Anti-La (SS-B) | 10 | Usually associated with anti-Ro, associated with decreased risk for nephritis |
Antihistone | 70 | More frequent in drug-induced lupus than in SLE |
Antiphospholipid | 50 | Predisposes to clotting, fetal loss, thrombocytopenia |
Antierythrocyte | 60 | Measured as direct Coombs' test; a small proportion develops overt hemolysis |
Antiplatelet | 30 | Associated with thrombocytopenia; not a useful clinical test |
Antineuronal (includes anti-glutamate receptor) | 60 | In some cases positive test in CSF correlates with active CNS lupus |
Antiribosomal P | 20 | In some cases a positive test in serum correlates with depression or psychosis due to CNS lupus |
As CMDT writes ‘Antibodies to double-stranded DNA and to Sm are specific for SLE but not sensitive, since they are present in only 60 and 30% of patients, respectively’. Both option ‘a’ and option ‘b’ are specific of SLE but sensitivity of option ‘a’ is more, so I will like to go with option ‘a’. Now it's upon you to choose answer
Ref: Harrison, 18/e; CMDT, 52/e p833
31. Hypogonadotrophic hypogonadism is typically associated with:
- Atrophy of the testicular interstitial (Leydig) cells
- Klinefelter's syndrome (XXY)
- Isolated GnRH deficiency (Kallmann's syndrome)
- Cryptorchidism
Ans. c. Isolated GnRH deficiency (Kallmann's syndrome)
Explanation
Swyer's syndrome (testicular regression syndrome) | Kallmann syndrome | |
|---|---|---|
Physical appearance | Normal growth Absence of secondary sexual character | Deficient secretion of GnRH Feature of hypogonadotropic hypogonadism Mental retardation Cleft lip cleft palate Obesity Bone and Renal anomalies Nerve deafness Optic atrophy |
External genitalia | Female | Under developed Cryptorchidism |
Internal genitalia | Female | Underdeveloped |
Investigation | Karyotype | GnRH FSH LH Sex steroid |
Finding | 46XY Primary amenorrhea Gonads—fibrous X-linked recessive trait | Primary amenorrhea Failure of secondary sexual character development Micropenis Delayed puberty X-linked, autosomal dominant, or autosomal recessive |
Others | — | Anosmia or hyposmia Color blindness |
Ref: NMS OBS and Gyn, 6/e p219, 325; Dutta Textbook of Gynecology, 5/e p434; Harrison, 18/e p3053–4; BRS Gyn and Obs, 2/e p293
32. Systemic hypertension may be seen in all of the following conditions except:
- Conn's syndrome
- Polyarteritis nodosa
- Chronic glomerulonephritis
- Addison's disease
Ans. d. Addison's disease
Explanation
Causes of Hypertension
In more than 95% of cases, a specific underlying cause of hypertension cannot be found. Such patients are said to have essential hypertension.34
Renal disease |
|
Renovascular |
|
Endocrine disease |
|
Drugs |
|
Neurogenic |
|
Alcohol | |
Obesity | |
Pregnancy (pre-eclampsia) | |
Obstructive sleep apnea | |
Coarctation of the aorta |
Ref: Devidson, 20/e p608-9; Harrison, 17/e p1554 and 18/e
33. Regarding hyperosmolar nonketotic diabetic coma, all the following are true except:
- It is seen in non-insulin dependent diabetes
- It is precipitated by infections
- Blood urea nitrogen may be elevated
- There is large anion gap
Ans. d. There is large anion gap
Explanation
Hyperosmolar Non ketotic diabetic coma
- Type 1 diabetes (insulin dependent) due to beta cell destruction, usually leading to absolute insulin deficiency.
- Type 2 diabetes (non-insulin dependent) may range from predominantly insulin resistance with relative insulin (abnormal insulin secretion) deficiency to a predominantly insulin secretory defect with insulin resistance.
- Characterized by severe hyperglycemia in the absence of significant ketosis, with hyperosmolality and dehydration.
- Occurs in patients with mild or occult diabetes, and mostly middle-aged to elderly individual with type 2 DM.
- As serum osmolality exceeds 310 mosm/kg, Lethargy and confusion may develop and if osmolality exceeds 320–330 mosm/kg coma may occur
- Infection, myocardial infarction, stroke, pneumonia, or recent operation are precipitating factors.
- If a patient is unable to maintain adequate fluid intake because of an associated acute or chronic illness or has suffered excessive fluid loss, marked dehydration results. As plasma volume contracts, chronic kidney disease develops severe hyperosmolality develops that causes mental confusion and finally coma.
- Laboratory finding
- Blood glucose values ranging from 800 mg/dL to 2400 mg/dL
- In mild cases -dilutional hyponatremia - reduce serum sodium to 120–125 mEq/L,
- Prerenal azotemia is the rule, with blood urea nitrogen elevations > 100 mg/dL is typical.
- Serum osmolality > 310 mosm/kg.
- blood pH above 7.3 i.e. no acidosis;
- Serum bicarbonate > 15 mEq/L.
- Normal anion gap (< 14 mEq/L).
Ref: Harrison, 18/e p1769; CMDT 52/e p1236-7
34. All of the following can be used as microbial bioterrorism agents except:
- Salmonella
- Plague
- Anthrax
- Botulism
Ans. a. Salmonella
Explanation
Although all of the above given bacteria can be used for bioterrorism. Among all option given above most correct answer is option ‘a’.
Category A | Category B | Category C |
|---|---|---|
|
|
|
|
|
|
|
|
Ref: Harrison, 17/e p1343
35. Which one of the following is not a characteristic of respiratory acidosis?
- Elevated arterial pCO2
- Decreased plasma pH
- Bounding pulse and mental stupor
- Rapid shallow breathing
Ans. d. Rapid shallow breathing
Explanation
Some important point regarding Respiratory acidosis:
- Can be due to severe pulmonary disease, respiratory muscle fatigue, or abnormalities in ventilatory control (variety of drugs, general anesthetics, sedatives, and head trauma).
- Recognized by an increase in Pa CO2 and decrease in pH.
- In acute case there is an immediate compensatory elevation in HCO3–, which increases 1 mmol/L for every 10-mmHg increase in Pa CO2. In chronic. (>24 hours), renal adaptation increases the HCO3–by 4 mmol/L for every 10-mm Hg increase in Pa CO2.
- C/F: Vary according to the severity and duration. A rapid increase in PaCO2 may cause anxiety, dyspnea, confusion, psychosis, and hallucinations and may progress to coma.
- Dysfunction in chronic hypercapnia include sleep disturbances; loss of memory; daytime somnolence; personality changes; impairment of coordination; and motor disturbances such as tremor, myoclonic jerks, and asterixis. Headaches and other signs that mimic raised intracranial pressure, such as papilledema, abnormal reflexes, and focal muscle weakness.
- T/t: Treatment of cause. A blood PaCO2 of more than 60 mm Hg may be an indication for assisted ventilation.
Ref: Harrison, 17/e p293,18/e
36. Which one of the following statements concerning porphyric neuropathy is correct?
- It is symmetrical and weakness is more proximal than distal
- It predominantly involves the sensory system
- It is associated with inflammation of nerve
- It causes elevated protein concentration in CSF
Ans. a. It is symmetrical and weakness is more proximal than distal
Explanation
Some important point regarding acute intermittent porphyria:
- This autosomal dominant disorder is caused by partial deficiency of porphobilinogen deaminase activity, leading to increased excretion of aminolevulinic acid and porphobilinogen in the urine.
- Common precipitating factors are endogenous and exogenous steroids, porphyrinogenic drugs, alcohol ingestion, and low-calorie diets, usually instituted for weight loss.
- Abdominal pain, the most common symptom, Ileus, abdominal distention, and decreased bowel sounds are common. diarrhea may occur. Abdominal tenderness, fever, and leukocytosis are usually absent because the symptoms are neurologic rather than inflammatory.
- Nausea; vomiting; constipation; tachycardia; hypertension; mental symptoms; pain in the limbs, head, neck, or chest; muscle weakness; sensory loss; dysuria; and urinary retention are characteristic.
- Tachycardia, hypertension, restlessness, tremors, and excess sweating are due to sympathetic over activity.
- The peripheral neuropathy is due to axonal degeneration (rather than demyelinization) and primarily affects motor neurons.
- Motor neuropathy affects the proximal muscles initially, more often in the shoulders and arms.
- Deep tendon reflexes initially may be normal but decreased or absent later on as the neuropathy advances. Sensory changes such as paresthesia and loss of sensation are less prominent.
- Sudden death may result from sympathetic over activity and cardiac arrhythmia.
- Mental symptoms such as anxiety, insomnia, depression, disorientation, hallucinations, and paranoia can occur in acute attacks. Seizures can be due to neurologic effects or due to hyponatremia.
The major manifestations of the acute hepatic porphyria are neurologic, including neuropathic abdominal pain, peripheral motor neuropathy, and mental disturbances, with attacks often precipitated by steroid hormones, certain drugs, and nutritional changes such as dieting.
Ref: NMS medicine, 6/e p552; Harrison, 17/e p1438-1440,18/e
37. Which one of the following tests is the most sensitive for detecting diabetic nephropathy?
- Serum creatinine level
- Creatinine clearance
- Microalbuminurea
- Ultrasonography
Ans. c. Microalbuminurea
Explanation
- The incidence of nephropathy in Patients with type 1 diabetes have a 30–40% and in type 2 diabetes patients, about 15–20% after 20 years.
- End-stage chronic kidney disease is much more prevalent in type 2 than in type 1 diabetes.
- Sensitive radioimmunoassay: methods of detecting small amounts of urinary albumin have permitted detection of microgram concentrations—in contrast to the less sensitive dipstick strips, whose minimal detection limit is 0.3–0.5%.
- Conventional 24-hours urine collections, not useful because several factors such as sustained erect posture, dietary protein, exercise, urinary tract infections, heart failure, and acute febrile tend to increase albumin excretion rates.
- Subsequent end-stage chronic kidney disease can be predicted by persistent urinary albumin excretion rates exceeding 30 mcg/min.
- The renal lesion that is specific for diabetes is intercapillary glomerulo-sclerosis (Kimmelstiel-Wilson disease). Other renal diseases associated with diabetes are papillary necrosis, chronic interstitial nephritis, and arteriosclerotic disease.
Ref: CMDT, 52/e p1223-4
38. Monitoring of antiretroviral treatment in a case of HIV is based on:
- Lymphocyte count
- CDS count
- CD4 Count
- Viral load
Ans. d. Viral load
Explanation
- In general, decisions about prophylaxis of opportunistic infections are based on the CD4 count, other evidence of severe immunosuppression (e.g., oral candidiasis), and a history of having had the infection in the past.
- Treatment should be initiated for all symptomatic patients, and for asymptomatic persons who
- Have CD4 cell counts below 500 cells/mcL.
- Have rapidly dropping CD4 counts (> 100 cells/mcL/year).
- Have very high viral loads (> 100,000/mcL).
- Have active infection with hepatitis B or C (rapid HIV replication is thought to hasten progression of hepatitis B and C).
- Have risk factors for cardiac disease (ongoing HIV replication may increase the risk of cardiac disease).
- Have HIV related renal impairment and pregnancy.
- Have risk factors for non–AIDS-related cancers (rapid HIV replication may increase such cancers).
- Current guidelines suggests that patients who does not have above conditions but are at high risk for transmitting HIV to another person should be considered for ART.
- Once ART has been initiated in a patient, it is not advisable to stop the therapy unless there is a important reason (e.g. toxicity, poor adherence, etc). So-called ‘drug holidays’ or ‘structured treatment interruptions’.
Ref: CMDT, 52/e p1436-43
39. All of the following are clinical presentations of hypercalcemia except:
- Polyuria
- Diarrhea
- Abdominal pain
- Psychosis
Ans. b. Diarrhea
Explanation
Hypercalcemia | |
|---|---|
Etiology |
Sarcoidosis Benign familial hypercalcemia Hypervitaminosis D Milk alkali syndrome Hyperthyroidism Thiazide therapy Immobilization |
Clinical feature | Mild hypercalcemia (up to 11–11.5 mg/dL) is usually asymptomatic. Some patients may complain of vague neuropsychiatric symptoms, including trouble concentrating, personality changes, or depression. Other presenting symptoms may include peptic ulcer disease or nephrolithiasis, and fracture risk may be increased. More severe hypercalcemia (>12–13 mg/dL), particularly if it develops acutely, may result in lethargy, muscle weakness, stupor, or coma, as well as gastrointestinal symptoms (anorexia, constipation, weight loss, constipation, nausea and vomiting, and abdominal pain, peptic ulcer disease or pancreatitis). It decreases renal concentrating ability, which may cause polyuria and polydipsia,bone pain or pathologic fractures. |
ECG change | Including bradycardia, AV block, and short QT interval; changes in serum calcium can be monitored by following the QT interval |
Ref: NMS, 6/e p402-3, Harrison, 18/e p3099
40. Which one of the following is not a feature of measles (Rubeola)?
- Usually occurs in childhood
- Incubation period is about 10 days
- Koplik's spots are characteristic
- Resolution occurs with scarring
Ans. d. Resolution occurs with scarring
Explanation
Measles virus is the only member of the genus Morbillivirus that infects humans.
- It is RNA virus belonging to paramyxovirus family (mumps and parainfluenza also belong to the same group). So far as is known, there is only one serotype. The virus cannot survive outside the human body for any length of time, but retains infectivity when stored at subzero temperature. The virus has been grown in cell cultures. The only source of infection is a case of measles. Carriers are not known to occur. The virus is transmitted by droplet infection, usually 4 days before and 5 days after onset of rash. The inclusion body of measles is Warthin–Finkeldey body.
- Incubation period is 10 days from exposure to onset of fever 14 days to appearance of rash.
- Secondary attack rate is 90%.
- The virus multiplies in respiratory epithelium.
- The disease is most common in preschool child, and infants are usually protected by maternal immunity.
- Koplik's spot is pathognomonic of measles, appears on 2nd and 3rd day of onset of measles, it is gray/white sand-like lesions with surrounding erythematus halo (which differentiates it from Fordyce's spot) opposite the lower second molars on the buccal mucosa. Koplik spots increase in number for 2–3 days and disappear by the end of 2nd day of the rash.
- Characteristic erythematous, nonpruritic, maculopapular rash begins at hairline and behind ears usually appearing on the 4th day with rise in fever and spreads over face, palm, and sole, etc. (most severe point of illness). Fever usually subsides 4–5 days after onset of rash. Prolong fever suggests complication of measles. Lymphadenopathy, diarrhea, vomiting are common features. Milder form of measles with less intense feature and mild illness is termed as modified measles and it is due to pre-existing immunity. Hemorrhagic measles is characterized by pruritic rash and bleeding from the nose, mouth, or bowel. Diarrhea is the most common complication. One attack of measles generally confers lifelong immunity. Second attacks are rare.
- Treatment is usually supportive.
- Vitamin A, 2 lac unit given orally to children older than 1 year of age for two consecutive days decreases the severity, complication rate and mortality due to measles (Park—all cases of severe measles and all cases of measles in areas with high case fatality rates should be treated with vitamin A, as 42many children develop acute deficiency of vitamin A, which may lead to keratomalacia and blindness from corneal scarring).
Ref: Harrison, 18/e p1603; Park, 21/e p137; Ghai, 7/e p185
41. Mycoplasma pneumoniae characteristically may produce complications except:
- Stevens-Johnson syndrome
- Raynaud's phenomenon
- Rapid and severe hemolysis due to cold agglutinin
- Pericardial tamponade
Ans. b. Raynaud's phenomenon
Explanation
Some Important Point Regarding Mycoplasma
- Prokaryotes, closer to that of viruses than to that of bacteria,; grow in cell-free culture media; smallest organisms capable of independent replication.
- Cell wall absent so no action by β lactam antibiotic.
- M. pneumoniae primarily infects the respiratory tract, while M. hominis, U. urealyticum, and U. parvum infects genitourinary tract.
- M. pneumoniae is generally thought to act as an extracellular pathogen
- Incubation period for M. pneumoniae is 2–4 weeks.
- C/F -Pharyngitis, tracheobronchitis, reactive airway disease/wheezing, or a nonspecific upper respiratory syndrome, otitis media, with or without bullous myringitis, pneumonia, headache, malaise, chills, and fever are noted in the majority of patients.
- The most common radiographic pattern is that of peribronchial pneumonia with thickened bronchial markings, streaks of interstitial infiltration, and areas of subsegmental atelectasis; pleural effusions are uncommon.
- Extrapulmonary Manifestations
- Can be a result of active infection (e.g., septic arthritis) or postinfectious autoimmune phenomena (e.g., Guillain-Barré syndrome).
- Many patients with extrapulmonary M. pneumoniae disease do not have respiratory disease.
- Erythema multiforme major (Stevens-Johnson syndrome) is the most clinically significant skin eruption associated with M. pneumoniae infection,.; other features are erythematous (macular or maculopapular), vesicular, bullous, petechial, and urticarial rashes, exanthem.
- The most common neurological manifestation are meningoencephalitis, others encephalitis, Guillain-Barré syndrome, and aseptic meningitis, cranial neuropathy, acute psychosis, cerebellar ataxia, acute demyelinating encephalomyelitis, cerebrovascular thromboembolic events, and transverse myelitis.
- Hepatitis, glomerulonephritis, pancreatitis, myocarditis, pericarditis, rhabdomyolysis, and arthritis (septic and reactive).
Ref: Harrison, 17/e p1068-9,18/e
42. Chlamydial infection can lead to all of the following diseases except:
- Trachoma
- Urethritis
- Atypical pneumonia
- Appendicitis
Ans. d. Appendicitis
Explanation
Some important point regarding chlamydial infection
Organism | Disease caused |
|---|---|
Chlamydia trachomatis | Trachoma Lymphogranuloma venereum Cervicitis, urethritis, proctitis |
Chlamydia psittaci | Psittacosis |
Chlamydia pneumonia | Atypical pneumonia
Acute/chronic sinusitis |
| |
Ref: Devidson, 20/e p341; CMDT, 52/e p1461-62
43. Forced alkaline diuresis is indicated in:
Ans. c. Salicylate poisoning
Explanation
Treatment of acute salicylate poisoning—symptomatic and supportive. Most important is external cooling and IV fluid with Na+, K+, HCO–3, and glucose according to need and determined by repeated monitoring. Gastric lavage done to remove unabsorbed drug,; forced alkaline diuresis, or hemodialysis done to remove absorbed drug and indicated in severe cases. Blood transfusion and vitamin K should be given if bleeding occurs.
As Harrison writes ‘acidic poisons are ionized and trapped in alkaline urine, whereas basic ones become ionized and trapped in acid urine’. Urinary alkalinsation increases chlorophenoxyacetic acid herbicides, chlorpropamide, diflunisal, fluoride, methotrexate, phenobarbital, sulfonamides, and salicylates excretion. ‘Urinary alkalinisation may enhance the elimination of salicylates and a small number of other poisons’. So both forced alkaline diuresis done in both option ‘b’ and option ‘c’. But from my opinion option c is more correct from the last sentence taken from Harrison.
Ref: Harrison, 18/e p367; Tripathi, 6/e p190
44. Which one of the following chemotherapeutic drugs is M-phase specific?
- Hydroxyurea
- Methotrexate
- Vincristine
- Cyclophosphamide
Ans. c. Vincristine
Explanation
Cytotoxic drug are either cell cycle non-specific or cell cycle specific:
Cell cycle specific (kills only actively dividing cells. Toxicity generally expressed in S phase) | Cell cycle non- specific (kill resting as well as dividing cell) | ||
|---|---|---|---|
G1 phase | : | Vinblastine | Mustine |
S phase | : | Methotrasate, cytarabin, fludarabine, 6-TG, 6-MP, 5-FU, hydroxyurea, mitomycin C, doxorubicin, dounorubicin | Cyclophosphamide Chlorambucil Carmustine Decarbazine Busulfan |
G2 phase | : | Daunorubicin, bleomycin, etoposide, Topotecan | L-asparaginage Cisplatin |
M phase | : | Vincristine, vinblastine, vinorelbine, paclitexal, docetaxel | Procarbazine Actinomycin D |
Ref: KDT, 7/e p875
45. Gum hypertrophy can be seen in:
- ALL
- CLL
- AML
- CML
Ans. c. AML
Explanation
Some important point regarding diagnosis of chronic myeloid leukemia
History/ symptoms |
|
| |
Sign |
|
Ref: Harrison, 18/e p909; NMS medicine, 6/e p106
46. Polymorphonuclear leucocytosis is seen in which one of the following?
- Whooping cough
- Typhoid
- Pneumococcal infection
- Tuberculosis
Ans. c. Pneumococcal infection
Explanation
Disease | Investigation |
|---|---|
Whooping cough occur due to pertussis infection |
|
Typhoid |
|
Tuberculosis |
|
| |
Pneumococcal infection |
|
Ref: CMDT, 52/e 1423, 1440, 1445; NMS medicine, 6/e p349
47. The most common infective cause of retinal disease with HIV infection is:
- Toxoplasmosis
- Cytomegalo virus infection
- Cryptococcal infection
- Parvo virus infection
Ans. b. Cytomegalo virus infection
Explanation
Some important complication of HIV infection
Organ involved | Manifestation |
|---|---|
Skin lesions |
|
| |
Lymphatic system |
|
Nervous system |
|
Eye |
|
Upper alimentary tract |
|
Gastrointestinal tract distal to the esophagus |
|
Liver |
|
Lungs |
|
Musculoskeletal system |
|
Hematopoietic abnormalities |
|
Endocrine system |
|
Reproductive system |
|
Ref: NMS medicine, 6/e p372-5
48. Alzheimer's dementia is a syndrome characterized by all of the following features except:
- It is usually progressive in nature
- It is associated with seizures
- The consciousness of the patient is not clouded
- It is marked by disturbance of higher mental functions
Ans. c. The consciousness of the patient is not clouded
Explanation
Some important features of Alzheimer's disease:
- Alzheimer's disease is a clinicopathologic entity characterized by progressive memory loss and other cognitive deficit.
- Most common cause of chronic dementia, occurring mostly in patients over 45 years.
- About 15% of cases are familial and these cases fall into two main groups: an early-onset, autosomal dominant pattern and a later-onset group whose inheritance is not so clear.
- Genetic abnormalities—inheritance of one of the alleles of apolipoprotein ≥, apo ≥ 4, is associated with an increased risk of developing the disease.
- Macroscopically, the brain is atrophic, particularly the cerebral cortex and hippocampus.
- Many different neurotransmitter abnormalities have been described in particular impairment of cholinergic transmission, although noradrenaline, 5-HT, glutamate and substance P are also involved.
- Patients present with gradual impairment of memory, usually in association with disorders of other cortical functions. Short-term memory lost earlier later on long-term memory loss. The key feature is impairment of delayed recall, i.e. the inability to retrieve (remember) information acquired in the past.
- Language becomes impaired—first naming, then comprehension and finally fluency.
- Aphasia is an early and prominent feature in some patient.
- Visuospatial deficits begin to interfere with dressing, eating, or even walking, etc.
- Delusions are common and usually simple, clouding of conciseness.
- Approximately 10% develop Capgras' syndrome, believing that a caregiver has been replaced by an impostor.
- Sleep-wake patterns are disrupted and night time wandering becomes disturbing to the household.
- Some patients develop a shuffling gait with generalized muscle rigidity associated with slowness and awkwardness of movement.
- In end-stage patients become rigid, mute, incontinent, and bedridden.
- Hyperactive tendon reflexes and myoclonic jerks (sudden brief contractions of various muscles or the whole body) may occur spontaneously or in response to physical or auditory stimulation.
- In the early stages, patients themselves may complain of difficulties, but as the disease progresses, it is common for patients to deny that there is anything wrong (anosognosia).
- Depression is common. Occasionally, patients become aggressive and the clinical features are made acutely worse by coexistent intercurrent illness.
- Generalized seizures may also occur.
- Death results from malnutrition, secondary infections, pulmonary emboli, heart disease or most commonly, aspiration.
Ref: Harrison, 18/e p3305; Devidson, 20/e p1217
49. The following are known causes of dementia that can be treated effectively with timely medical or surgical intervention except :
- Subdural hematoma
- Vitamin B12 deficiency
- Alzheimer's disease
- Thyroid hormone deficiency
Ans. c. Alzheimer's disease
Explanation
Causes of Dementia
Reversible cause | Irreversible cause/degenerative disease |
|---|---|
Hypothyroidism | Alzheimer's |
Thiamine deficiency | Frontotemporal dementia |
Vitamin B12 deficiency | Huntington's |
Normal-pressure hydrocephalus | Dementia with Lewy bodies |
Subdural hematoma | Vascular |
Chronic infection | Leukoencephalopathies |
Brain tumor | Parkinson' |
Ref: Harrison, 18/e p3302
50. Likely causes of laryngotracheobronchitis in a two year old child are all the following except:
- Coxsackie virus
- Parainfluenza virus type-1
- Respiratory syncytial virus
- Influenza A virus
Ans. a. Coxsackie virus
Explanation
- Nearly always caused by viral infection
- Usually Parainfluenza virus type 1, other causing viruses are respiratory syncytial virus and para influenza virus 2 and 3, influenza virus, adenovirus and rhinovirus.
Ref: Ghai, 8/e p376
51. The dose of zinc for treatment of diarrhea in children (above the age of 6 months) is:
- 5 mg per day for 10 days
- 10 mg per day for 10 days
- 15 mg per day for 14 days
- 20 mg per day for 14 days
Ans. d. 20 mg per day for 14 days
Explanation
WHO and UNICEF recommended that all children with acute diarrhea in at risk area should receive oral Zinc for 10–14 days during and after diarrhea. Dose for children less than 6 months is 10 mg/day and more than 6 month is 20 mg/day.
Ref: Nelson, 19/e p1336
52. A newborn baby is defined as very Low Birth Weight baby if the birth weight is:
- Below 1500 gm
- Below 1750 gm
- Below 2000 gm
- Below 2250 gm
Ans. d. Below 2250 gm
Explanation
Some important terminology
Low birth weight neonate | Weighing < 2500 gm irrespective of gestational age |
Very low birth weight neonate | Weighing < 1500 gm irrespective of gestational age |
Extremely low birth weight neonate | Weighing < 1000 gm Irrespective of gestational age |
Postterm neonate | Neonate born at gestation age 42 weeks or more |
Preterm neonate | Neonate born at gestation age 37 weeks or less |
Term neonate | Neonate born at gestation age 37 to 42 weeks |
Still birth | Fetal death at gestational age of 22 weeks or more or weighing more than 500 gm at birth |
Ref: Ghai, 8/e p124
53. Which of the following is not advised for breast abscess in a lactating mother?
- Administer analgesics
- Stop breast milk to infant
- Administer antibiotics
- Abscess maybe incised and drained
Ans. b. Stop breast milk to infant
Explanation
Treatment of breast abscess
- Stop breast feeding on abscess side but continue on other side
- Expressed breast milk every 2 hourly on abscess side
- Recurrent aspiration of breast abscess for cosmesis if not responded than radial incision and drainage
- Administer antibiotic after culture and sensitivity
- Administer analgesic.
Ref: Dutta Textbook of Obstetrics, 7/e p439
54. The anticonvulsant drug of choice for infantile spasms (West syndrome) is:
- Phenytoin sodium
- Phenobarbitone
- Vigabatrin
- Carbamazepine
Ans. c. Vigabatrin
Explanation
West Syndrome (Infantile Spasm)
- Onset between three to eight months of life.
- Common causes are: hypoxic ischemic encephalopathy, neurocutaneous syndrome specially tuberous sclerosis, perinatal infection, hemorrhage, injury, metabolic disorder, localized structural malformation and ideopathic.
- Characterized by salaam spells (sudden dropping of head and flexion of arm), developmental retardation and hypsarrhythmia on EEG.
- Prognosis for mental development poor.
- ACTH and corticosteroid may help duration of t/t is 2–12 weeks.
- DOC is vigabatrin specially in tuberous sclerosis.
Ref: Ghai, 8/e p559
55. Obesity in children is defined as:
- Body Mass Index (BMI) more than 85th percentile for age
- Body Mass Index (BMI) more than 90th percentile for age
- Body Mass Index (BMI) more than 95th percentile for age
- Body Mass Index (BMI) more than 97th percentile for age
Ans. c. Body Mass Index (BMI) more than 95th percentile for age
Explanation
Children with BMI > 85 percentile for age considered as over weight while those >95% for age considered as Obese.
BMI = weight (kg) ÷ height (m)2
Ref: Ghai, 8/e p528
56. A four week, term male baby presents with jaundice. His total bilirubin is 18 mg% and indirect is 4 mg%. What is the least helpful investigation?
Ans. d. Blood group type of mother
Explanation
Causes of Neonatal Jaundice
First day | 2nd and 3rd days | 4th to 7th days | After 1 weeks | Persistent During one month | |
|---|---|---|---|---|---|
Causes | Rh and ABO incompatibility Intrauterine infection like toxoplasma and CMV infection G-6-PD deficiency | Physiologic Hyperbilirubinemia of newborn Birth asphyxia Cephalohematoma Acidosis Hypothermia Hypoglycemia Drugs Familial non-hemolytic icterus (Crigler-Najjar syndrome, Gilbert- syndrome, | Septicemia Syphilis Toxoplasmosis CMV Extrahepatic biliary atresia Breast-milk jaundice | Extrahepatic biliary atresia Septicemia Hereditary spherocytosis Neonatal hepatitis | Inspissated bile syndrome Cretinism Congenital hypertrophic pyloric stenosis Hyperalimentation associated with cholestasis Hepatitis |
Hereditary spherocytosis Drug administration to mother (vitamin, salicylate, etc) Homozygous α- thalassemia | Dubin-Johnson syndrome) | Drug induced hemolytic anemia Galactosemia | CMV Syphilis Toxoplasmosis Congenital atresia of bile duct Familial non-hemolytic icterus Galactosemia |
In this question direct bilirubin is more than indirect bilirubin. Indirect hyper bilirubinemia occur in Hypothyroidism as well as ABO incompatibility. But by the end of month jaundice due to ABO incompatibility does not persist.
Ref: Suraj Gupte, 8/e p511; Nelson, 19/e p605
57. Which of the following heart disease is common in Down syndrome?
Ans. a. Common AV canal
Explanation
Some important syndrome and associated cardiac abnormality
Di George syndrome | Aortic arch abnormalities, truncus arteriosus, tetralogy of Fallot, pulmonary atresia with VSD |
Marfan syndrome | Dilation of ascending aorta/aortic sinus, aortic and mitral regurgitation |
Noonan syndrome | Dysplastic pulmonary valve, ASD |
Edward syndrome | VSD, polyvalvular disease, coronary abnormalities |
Patau syndrome | PDA, ASD, VSD, PS, AS, aortic and pulmonary atresia |
Down syndrome | Atrioventricular septal defect, VSD, PDA, anomalous subclavian artery |
William's syndrome | Supravalvular aortic stenosis, pulmonary artery stenosis |
Turner syndrome | Coarctation of aorta, bicuspid aortic valve |
Ref: Ghai, 6/e p552, 7/e p570; Nelson, 19/e p2119–2130
58. A ten year old child presented with decreased urine output and cola colored urine for four days. She had hypertension and periorbital puffiness. Most useful test will be:
- Ultrasound abdomen(KUB)
- Throat swab for Group A Beta hemolytic streptococci
- Urine culture
- Urine routine and microscopy
Ans. b. Throat swab for Group A Beta hemolytic streptococci
Explanation
This patient suffering from post streptococcal glomerulonephritis. Some important point:
- PSGN caused by group A β-hemolytic streptococci.
- Commonly follows streptococcal pharyngitis during cold weather months and skin infection or pyoderma during warm weather month.
- Epidemic of nephritis associated with throat (serotype 12) and skin (serotype 49) infections, this disease is mostly sporadic.
- Kidney appear symmetrically enlarged.
- Immunofluorescence microscopy reveals a pattern of ‘lumpy bumpy’ deposit of immunoglobulin and compliment of the glomerular basement membrane. On electron microscopy, electron dense deposits or humps.
- Most common in children of 3–12 years age; uncommon before three years.
- Typical patient develop nephritis syndrome 12 week after pharyngitis and three to six weeks after pyoderma.
- Mild proteinuria and microscopic hematuria.
- Onset is rapid with puffiness around the eyes and pedal edema. Urine is coca-cola colored.
- Hematuria usually do not persist beyond two weeks but Persistent microscopic hematuria may present one to two years after the initial presentation.
- Hypertension persist in 60% of patient among them 10% got encepha-lopathy (blurred vision, severe headache, altered mental status or new seizure). Other complication are left ventricular failure and pulmonary edema (respiratory, orthopnoea, cough), acute kidney injury and nephrotic syndrome.
- Urine shows 1-2 + protein with red cells and granular cast polymorphonuclear leukocytosis. ESR-↑, urea and createnine-↑, hyponetremia and hyperkalemia, C3 is low in 90% patient and normalize after 8–12 weeks, persistent low means other form of GN.
- Confirmation of diagnosis require clear evidence of a prior streptococcal infection. ASO titre increase after pharyngeal infection rarely after skin infection.
- The best single antibody titre to document cutaneous streptococcal infection is the anti-deosyribonuclease (DNase)B level.
- Renal biopsy should only consider if presence of acute renal failure, nephrotic syndrome absence of evidence of streptococcal infection or normal compliment level.
- Complete recovery in > 95% case.
Ref: Nelson, 19/e p1783; Ghai, 8/e p474
59. All of the following features can be present in achondroplasia except:
- Autosomal dominant inheritance
- Parents with normal height
- Small head
- Short limbs
Ans. c. Small head
Explanation
Some Important Point Regarding Achondroplasia
- Caused by failure of normal ossification of bones mainly long bones resulting in disproportionate dwarfism.
- Shortening marked in proximal segment of limb.
- Autosomal dominant inheritance but many case arise from fresh gene mutation.
- Normal intelligence.
- Normal life except who have spinal canal stenosis.
Ref: J Maheshwari, 4/e p306
60. Which one of the following is not a part of the Revised Trauma Score?
- Glasgow coma scale
- Systolic blood pressure
- Pulse rate
- Respiratory rate
Ans. c. Pulse rate
Explanation
Revised trauma score (RTS)—most widely applied
Glasgow coma scale | Systolic blood pressure (mmHg) | Respiratory rate (per minute) | Points |
|---|---|---|---|
13–15 | > 89 | 10–19 | 4 |
9–12 | 76–89 | >29 | 3 |
6–8 | 50–75 | 6–9 | 2 |
4–5 | 1–49 | 1–5 | 1 |
3 | 0 | 0 | 0 |
Ref: Bailey & Love, 23/e p276, 279; Harrison, 16/e p1582
61. Which of the following is not associated with cleft palate?
- Otitis media
- Speech problems
- Detention abnormalities
- Missing teeth in lower jaw
Ans. d. Missing teeth in lower jaw
Explanation
Cleft palate
Cleft palate maybe associated with eustachian tube dysfunction, otitis media with effusion, increased risk of sensorineural and conductive loss. In speech, patient may have velopharyngeal incompetence (hypernasal quality speech), articulation problem, speech problem. Dental problems include delayed tooth development, delayed eruption, reduced no of teeth (hypodontia) or increased no of teeth (hyperdontia) and defective facial growth.
Ref: Bailey & Love, 25/e p659
62. Which one of the following is not correct regarding Meckel's diverticulum?
- It is present at birth
- It has ectopic gastric mucosa
- Technetium scan is a diagnostic investigation
Ans. c. Present on the mesenteric border
Explanation
Some Important Points Regarding Meckel's Diverticulum
- Most prevalent congenital abnormality of the GI tract found in approximately 2% of population, situated in antimesenteric border; male/female ratio is 2:1; located 2 feet proximal to ileocecal junction; approximately 2 cm long; one-half of those who are asymptomatic are below 2 years of age.
- It is a true diverticulum; 60% carries ectopic gastric mucosa; pancreatic acini are second most common; others include Brunner's gland, pancreatic islets, colonic mucosa, endometriosis and hepatobiliary tissue.
- It is due to persistence of omphalomesenteric (vitelline) duct.
- Symptoms maybe due to complications.
Complications
- Severe hemorrhage (most common presentation in children; bleeding is rare in adults above 30 years of age).
- Intussusception.
- Meckel's diverticulitis mimics with acute appendicitis, whereas perforated diverticulitis mimics with perforated duodenal ulcer.
- Chronic peptic ulceration.
- Intestinal obstruction, most common presentation in adults.
- Technetium-99m scanning maybe useful in identifying Meckel's diverticulum as a source of gastrointestinal bleeding.
Treatment
Bailey writes, it can be left during abdominal operation, provided it is wide mouth and wall of diverticulum in not thickened, whereas Schwartz writes, management of asymptomatic diverticulum is controversial. Some authors advocate surgery due to lifetime risk of complications.
Ref: Bailey & Love, 25/e p1158; Schwartz, 9/e p1002
63. In a malignant melanoma of the skin, the invasion to epidermis, papillary and reticular dermis refers to Clark's level:
- II
- III
- IV
- V
Ans. c. IV
Explanation
AJCC Staging Melanoma
Primary | Breslow thickness | Clark's level |
|---|---|---|
PT1 | In situ | I (Confined to epidermis) |
PT1 | Melanoma < 0.75 mm | II (Invade papillary dermis) |
PT2 | Melanoma 0.76–1.5 mm | III (Invade papillary-reticular dermal junction) |
PT3 | Melanoma 1.51–4.0 mm | and/or IV (invade reticular dermis) |
PT4 | Melanoma 4.0 and/or satellites within 2 cm of primary | and/or V (involve subcutaneous fat) |
Malignant Melanoma
- Most common type is superficial spreading (70%), Distribution is superficial (radial). Most likely to arise from preexisting nevus. Most common site in male is back and in female is leg.
- Least common type is acral lentiginous. Distribution is superficial (radial) occurs in palm and sole and in subungual region (Hutchinson's sign is diagnostic of subungual melanoma).
- Lentigo melanoma—least common, most benign form and has best prognosis, previously known as Hutchinson's melanotic freckle. Distribution is superficial (radial). Face, head, neck of elderly people involved.
- Nodular type is aggressive tumor. It is often present at middle age, distribution is vertical (penetrating), usually on trunk, head and neck. Typical appearance of blue-black papule.
- Amelanotic has worse prognosis. It often arises from gastrointestinal tract presenting with obstruction or metastasis of unknown etiology.
- Desmoplastic melanoma mostly found in head and neck and has propensity for perineural infiltration and often recur locally if not widely excised.
Prognostic Factors
- Tumor thickness (stage) has been recognized as the most important prognostic factor in melanoma patient with grades I and II. Two methods commonly used to measure thickness are Clark level and Breslow thickness.
- Evidence of tumor in regional lymph node is poor prognostic sign. The number of positive lymph node is also correlated with survival rates.
- The presence of distant metastasis is a poor prognostic sign.
- For same criteria, in people, lesion of extremities has better prognosis than lesion in head and neck.
- Presence of ulceration in a lesion has worse prognosis.
- Females have better prognosis than males.
- Nodular type and superficial spreading have same prognosis.
- Large inflammatory infiltrate on histology—good prognostic sign.
Ref: CSDT, 13/e p951, 1112; Bailey & Love, 25/e p615; Schwartz 9/e p413–415
64. Which one of the following tests is done to detect subclinical infection in tuberculosis of intestine?
- X-ray abdomen
- Interferon-gamma release assay
- Ultrasound of abdomen
- Barium meal and follow through
Ans. b. Interferon-gamma release assay
Explanation
IFN-gamma Release Assays used for sub clinical tuberculosis infection
- Two in vitro assays that measure T-cell release of IFN-gamma in response to stimulation with the highly TB-specific antigens ESAT-6 and CFP-10 are available.
- The T-SPOT. TB is an enzyme-linked immunospot (ELISpot) assay and the QuantiFERON-TB Gold is a whole-blood enzyme-linked immunosorbent assay (ELISA) for measurement of IFN-gamma.
- IFN-gamma Release Assays are more specific than the TST as a result of less cross-reactivity due to BCG vaccination and sensitization by nontuberculous mycobacteria.
Ref: Harrison, 18/e p1350
65. The quality of bone formation in transplanted bone is best improved by:
- Autogenous cortical bone graft
- Allogenic cancellous bone graft
- Allogenic composite bone graft
- Autogenous cancellous bone graft
Ans. d. Autogenous cancellous bone graft
Explanation
- Autograft (from same person) is gold standard bone grafting. Iliac crests are commonest site for taking bone grafts. When a graft is required for osteogenic purpose (in non-nion) cancellous bone graft is preferred. It is available in plenty from iliac crests and upper end of tibia. Although a cancellous graft does not provide much, if any, immediate structural support, it incorporates quickly and is completely replaced by host bone and marrow after 1 year. When graft is used for stability (as filling long bone 61gaps) cortical graft is used. Fibula are common source of cortical bone graft other are ribs, or shell of the ilium. These graft are free grafts. These do not survive. A bone stimulating protein called bone morphogenic protein is liberated from bone grafts and helps osteogenesis which later on replaced by new living bone. New techniques are muscle pedicle bone graft (used in treating nonunion of fracture neck of femur) and free vascularized bone graft (fibula commonly taken along with its blood supply i.e. peroneal vessel).
- Allograft (from another person of same species) is needed when not enough bone is available. Bone preserved at deep freezing (-700C), freeze dried, preservation by decalcifying bone (decal bone) or by formalin preservation.
- Xenograft (bone graft from other species like bovine).
- Artificial bone material derived from corals. it is hydroxyapatite with porous structure.
Ref: J Maheshwari, 4/e p82; Rockwoods and Greens Fracture in adult, 6/e p314-6
66. Following are the complications of ectopia vesicae except:
- Vesicoureteric reflux
- Hydronephrosis
- Carcinoma of urinary bladder
- Renal failure
Ans. a. Vesicoureteric reflux
Explanation
Some important point regarding ectopia vesicae
- Male-Female ratio 4:1. In the male, the penis is broad and short
- Epispedias almost always present
- Umbilicus absent
- Prostate and seminal vesicle is rudemantary or absent
- Clitoris is cleft
- Labia minora separated
- Bilateral inguinal herniae maybe present. There is separation of the pubic bones
- Treatment: The bladder is closed in the first year of life, usually following osteotomy
- Complications:
- Exposed vesical mucus membrane ulcerate with hemorrhage
- Recurrent ascending infection is common
- Hydronephrosis by ureterovesical obstruction
- Bad odor of urine with patient
- Hyperchloremic acidosis
- Half patient dies with renal failure
Ref: Bailey & Love, 25/e p1314; S Das 4/e p1225
67. In a catheter sized 16 F; 16 F stands for:
- 16 mm diameter at the tip of catheter
- 16 inch diameter
- 1.6 inch circumference
- 16 mm circumference
Ans. d. 16 mm circumference
Explanation
Size of catheter in French or Charriere scale is indicator of the external circumference in millimeters.
Ref: Pie Surgical Handicraft, 22/e p312
68. A young man with steering wheel injury on chest reveals palpable multiple fracture of ribs and paradoxical movement. X-ray shows pulmonary contusion on right side without pneumothorax or hemothorax. The treatment of choice is:
- Stabilization of chest wall with sand bags
- Stabilization with towel clips
- Tracheostomy/endotracheal tube and mechanical ventilation
- Immediate operative stabilization
Ans. c. Tracheostomy/endotracheal tube and mechanical ventilation
Explanation
As per sabiston stabilization of chest has been attempted using weight and rib binders, as well as fixation devices such as pin and plate. Main goal of treatment is to maintain adequate ventilation. In this question stability of patient is not clear but as per question it can be presumed that patient is unstable and may get deteriorate further. So best option is option c, i.e. endotracheal tube and mechanical ventilation. In stable case only analgesic and supportive treatment is sufficient.
According to Bailey, surgery to stabilize the flail chest is currently in use again; it maybe useful in selected groups with isolated or severe chest injury and pulmonary contusion which have been shown to benefit from internal operative fixation of the flail segment.
Ref: Sabiston, 18/e p1664; Bailey & Love, 25/e p343
69. Thinning of cornea occurs in:
Ans. d. Keratoconus
Explanation
Keratoconus
- Bilateral usually symmetrical conical protrusion of the central part of the cornea with thinning of its central and inferior paracentral area
- Starts at around puberty and slowly progressive, no family history
- Initial symptom is impaired vision
- Irregular retinoscopic reflex, vertical folds at the level of deep stroma and Descement membrane (Vogt's lines)
- Prominent corneal nerve
- Munson's sign-buldging and tenting of lower lids when patient looks down
- Fleischer's ring: epithelial iron deposition at the base of the cone
- It does not rupture spontaneously even if there is extreme thinning of cornea
Megalocornea
- Bilateral condition in which corneal diameter is more than 14 mm
- Myopic patient
- Deep anterior chamber, tremulousness of iris and sublaxation of the lens with or without cataract formation.
Bullous Keratopathy
- Develop due to persistent epithelial edema in Fuch's endothelial dystrophy, usually autosomal dominant inheritance
- When bullae rupture it causes severe pain, photophobia and lacrimation
- Other cause of Bullous keratopathy is post surgical aphatic bullous keratopathy, absolute glaucoma, chronic aridocyclitis, disciform keratitis, hydrops keratoconus
Ref: Basak's Essential Ophthalmology, 3/e p149
70. A two year old child is found to have ptosis of one eye with defective elevation of the eye. Opening the mouth causes elevation of the ptosed lid. The most likely clinical condition is:
- Partial third nerve palsy
- Congenital ptosis
- Ocular myasthenia
- Congenital ptosis with Mercus-Gunn phenomenon
Ans. d. Congenital ptosis with Mercus-Gunn phenomenon
Explanation
Congenial Ptosis
- Due to imperfect differentiation of the levator muscle
- Often hereditary
- Maybe associated with synkinesis (synkinetic ptosis)
- Maybe associated with epicanthus or blepherophimosis
- Marcus –Gunn Jaw winking phenomenon—the retraction of ptotic eye lid with stimulation of ipsilateral pterygoid muscle (Jaw movement)
Ref: Basak's Essential Ophthalmology, 3/e p98
71. ‘Pulsatile Tinnitus’ occurs in patients with:
- Otosclerosis
- Secreting otitis media
- Palatal myoderma
- Glomus jugular tumor
Ans. d. Glomus jugular tumor
Explanation
Glomus Jugular Tumor or Chemodectoma
- Very slow growing tumor arises from carotid body like structure on the dome of jugular bulb and floor of the middle ear
- Also called nonchromaffin paraganglioma
- Middle age, M:F-5:1,
- Histoclogically benign but locally invade
- Insidious onset, deafness is earliest symptom, unilateral and conductive
- Tinnitus is pulsatile and roaring in nature, profuse hemorrhage often occur
- Rising sun appearance when tumor arises from floor of middle ear
- Pulsation sign (Brown sign) is positive, i.e. when ear canal pressure is raised with Siegel's speculum, tumor pulsate vigorously and then blench
- Otorrhea may occur due to secondary infection
- VII cranial nerve frequently involved and other nerve involved are IX, X, XI
- Systolic bruit may heard over the temporal bone.
- Diagnosis confirmed by biopsy but never done preoperatively
- T/t—in early stage sparing tympanic membrane–hypotympanotomy. Moderate advanced case/VII nerve involvement—Redical mastoidectomy with removal of tumor mass.
Ref: PL Dhingra, 4/e
72. Following are the specific causes of hypoxaemia following thoracic spinal injury at T6 and above except:
- Intercostal nerve paralysis
- Partial phrenic paralysis
- Abdominal wall paralysis
Ans. d. Abdominal wall paralysis
Explanation
Lung is supplied by parasympathetic fiber derived from vegous nerve and sympathetic fiber derived from T2-T5. Both provide motor supply to bronchial muscle and secretomotor supply to mucus gland of bronchial tree.
Intercostal muscle is supplied by intercostal nerves. Intercostal nerve are anterior primary rami of spinal nerve T1-T11. Upper three intercostal nerve also supply upper limb and thorax and lower five T7-T11 also supplies abdominal muscle.
Root value of phrenic nerve is C2–5 which supplies diaphragm.
Ref: BDC, 3/e p185
73. In ‘Gastroschisis’:
- The cord is inserted on the top of the sac
- The gut lies outside the abdomen without a covering sac
- The sac covers the gut or liver lying outside the abdominal cavity
- None of these statements is true
Ans. b. The gut lies outside the abdomen without a covering sac
Explanation
The two types of abdominal wall defects are Gastroschisis and omphalocele. In both condition abdominal contents are located outside of the peritoneal
Gastroschisis | Omphalocele |
|---|---|
|
|
|
|
Ref: NMS Surgery, 5/e p555-556; Baily & Love, 25/e p86
74. A 2-year-old previously healthy child develops sore throat, stridor and increasing dyspnea and becomes severely ill within a matter of hours with prostration and collapse. The most likely clinical diagnosis is:
- Acute tonsillitis
- Acute pharyngitis
- Epiglottitis
- Acute laryngotracheobronchitis
Ans. c. Epiglottitis
Explanation
Disease | Laryngotracheobronchitis (Croup) | Acute tonsillitis | Acute pharyngitis | Acute epiglottitis (supraglottitis) |
|---|---|---|---|---|
Etiology | Viral infection | Hemolytic streptococcus (MC), staphylococci, pneumococci, H. influenza | Viral (rhino, influenza, parainfluenza, measles) bacterial (b hemolytic) fungal (candida) | Bacterial Mostly H. influenzae type B |
Stridor | Biphasic | Inspiratory | ||
Age | 1–5 years | School going rare in infant and > 50 | Any age | Any age |
Onset | Over several days | Vary with severity of infection. | Vary with severity | Acute (over several hours of sore throat, marked dysphagia and fever) |
Examination | Narrowing of subglottic region (Steeple sign) on chest X-rays Cough present | Sore throat, difficulty in swallowing, fever, earache, hyperemia or pillars, uvula soft palate, tonsil swollen with yellowish spots, white membrane | Milder with discomfort in throat, low grade fever, severe with pain in throat, dysphagia, headache, high fever Pharyngeal erythema, congestion, enlarged tonsil | Tripod position, toxic appearance, cough absent Thumb-like thickening of epiglottis and other supraglottic regions on chest X-rays |
Outcome | Mostly mild and resolve within 1–2 days | Chronic tonsillitis, peritonsilalar abscess, paraphyringeal abscess, cervical abscess, acute otitis media, rheumatic fever, SABE, acute glomerulonephritis | May proceed to tonsillitis | Depending upon the management (instrumentation of throat and tongue can precipitate fatal laryngospasm) |
Treatment | Reassurance, rest and hospitalization, steroid (moderate and sever case), antibiotic | Analgesic, penicillin is DOC. If sensitive to penicillin than erythromycin is doc. For 7 D. | Penicillin G is TOC or sephylococcal pharyngitis | Airway management Antibiotic |
Ref: Ghai, 7/e p339, 341; Dhingra, 6/e p259
75. An infant with recurrent abdominal colic, a palpable mass on the right side of the abdomen and passage of bloody stools is most likely to be suffering from:
- Congenital pyloric stenosis
- Intussusception
- Wilms' tumor
- Amoebiasis
Ans. b. Intussusception
Explanation
Some Important Points Regarding Intussusceptions
- Most common cause of intestinal obstruction in infant of age 6–18 months (peak age is 5–10 month Bailey and love). (Schwartz—In young child it is most common cause of intestinal obstruction). This occurs when one portion of the gut becomes invaginated within an immediately adjacent segment; almost invariably, it is the proximal into the distal.
- Ileocolic (77%) is the most common type, ileocolic (12%), ileoileal (5%), colocolic (2%).
- First born male child is commonly affected.
- Etiology—in infants—the lead point is presumed to be enlarged Peyer's patch, the lymphoid tissue presumably responding to a viral stimulant. In older children—lead point maybe Meckel's diverticulum, polyp, enteric cyst, HS purpura.
- Weaning, loss of passively acquired maternal immunity and common viral pathogens have all been implicated in the pathogenesis of intussusception in infancy.
- Painful cry, drawing up the knees and going pale, presumably in relation to colic (88%), intermittent, with increasing frequency. Vomiting (86%), red currant jelly stool (56%), palpable mass (50–60%) with associated feeling of emptiness in right iliac fossa (sign of dance).
- Radiographic findings include presence of mass, distal small bowel obstruction and sparse gas within the colon.
- Barium enema—claw sign (meniscus sign).
- Ultrasonographically, target sign on transverse view and pseudokidney sign on longitudinal view and mass (doughnut sign).
- Treatment is nonoperative reduction with air or barium enema successful at 70%. If contraindicated, (perforation or peritonitis) then operation is indicated.
Ref:. Bailey & Love, 25/e p1191
76. Which one of the following bronchial carcinomas has the best prognosis?
- Adenocarcinoma
- Adenosquamous carcinoma
- Squamous carcinoma
- Small cell carcinoma
Ans. c. Squamous carcinoma
Explanation
Lung Cancer
Etiology/ risk factor |
|
Pathology | There are four major varieties of lung cancer which grouped into non small-cell lung cancer (non-SCLC) and small cell lung cancer (SCLC).
|
Clinical feature |
|
Clinical feature |
|
Common radiological findings |
|
Prognosis | Very poor prognosis around 80% of patients dying within a year of diagnosis. The best prognosis is with well-differentiated squamous cell tumors which have not metastasised and are amenable to surgical treatment. |
Ref: Harrison, 18/e p742; Devidson, 21/e p698-9; NMS medicine, 6/e p138-9
77. The bone most prone to avascular necrosis following a fracture is:
- Scaphoid
- Humerus
- Femur
- Talus
Ans. c. Femur
Explanation
Among all given option except humerus all of the above mentioned may underwent fracture but femur is most common bone to underwent avascular necrosis
Bone | Site of fracture and mechanism of avascular necrosis |
|---|---|
Femur | After fracture through neck, all the medullary blood supply and most of the capsular blood supply to the head are cut off. |
Talus | Because of poor blood supply after fracture through neck, the body of the talus becomes avascular. |
Scaphoid | In fracture through waist, there is high probability of the proximal fragment becoming avascular. |
Lunate dislocation | Avascular necrosis is a common complication in anterior or posterior dislocation. |
Ref: Maheshwari, 4/e p116, 140
78. All of the following statements are true of the keloids except:
- It is rarely seen in white skinned persons
- It is more common over the sternum
- True keloid does not spread into normal tissue
- The maturation and stabilization of the collagen fibrils is inhibited
Ans. c. True keloid does not spread into normal tissue
Explanation
Some important differences between keloid and hypertrophic scar:
Keloid | Hypertrophic scar |
|---|---|
|
|
Ref: Bailey and Love, 25/e p30, 599; Das, 4/e p123
79. Which one of the following is a palliative shunt procedure created between the left subclavian artery and the pulmonary artery to treat cyanotic heart disease?
- Gatt's shunt
- Lieno renal shunt
- Blalock Taussig shunt
- Waterston's shunt
Ans. c. Blalock Taussig shunt
Explanation
Shunt name | Structure anastomosed | Used for treatment of |
|---|---|---|
Blalock Taussig shunt | Subclavian artery with pulmonary artery | Tetralogy of fallot |
Waterston's shunt | Ascending aorta with right pulmonary artery | Tetralogy of fallot |
Pott's shunt | Descending aorta to pulmonary artery | Tetralogy of fallot |
Lieno renal shunt | Splenic vein and left renal vein | Portal hypertension |
Gott's shunt | Ascending aorta and the descending aorta | Descending thoracic aortic aneurysm |
Ref: Ghai, 7/e p410
80. Which is the most important local factor responsible for wound healing?
- Tissue oxygenation
- Absence of foreign body
- Absence of infection
- Absence of tension in wound
Ans. a. Tissue oxygenation
Explanation
Factor influencing wound healing:
General factor | Local factor |
|---|---|
Age- healing is fast in young and slow in older Protein deficiency—decrease wound healing Vitamin C deficiency- decrease wound healing Vitamin A—it require for epithelialization Zn, Ca, Cu, Mn deficiency reduce wound healing Hormone—corticosteroid—delay fibrosis Deoxycorticosterone acetate anabolic steroid—increase wound healing Other cause which retard wound healing
| Blood supply—poor blood supply heal slowly. Oxygen supply is most important. Position of wound-parallel to langer line heal fast Tension—tension heal slowly Infection—hamper wound healing Movement—delay wound healing Exposure to ionizing radiation—delay wound healing Foreign body- retard wound healing Adhesion to bony surface—delay wound healing Necrosis- retard wound healing Lymphatic drainage—obstruction in lymphatic retard wound healing Ultraviolet light—increase wound healing Faulty technique of wound closure—delay wound healing Hyperbaric oxygen—increase wound healing |
Ref: S Das, 4/e 7
81. Which one of the following is not a metabolic complication of pyloric stenosis?
- Alkalosis
- Hyponatremia
- Hypochloremia
- Hyperkalemia
Ans. d. Hyperkalemia
Explanation
Congenital Hypertrophic Pyloric Stenosis:
- 3/1000 live births, 5 times more common in boys (most common surgical disorder of infancy).
- Hypertrophy of circular muscle (Resembles an olive in about 80%) nonbilious vomiting, usually at 3–6 weeks (may develop as early as 1st week), vomiting usually progressive, may or may not be projectile initially.
- After feeding, visible peristalsis wave moves from left hypochondrium to umbilicus.
- Constipation is usual, malnutrition, dehydrated, hypochloremic alkalosis, hypokalemic, metabolic alkalosis with paradoxical aciduria. Alkalosis leads to a lowering in the circulating ionized calcium and tetany can occur.
- Diagnosis by palpating abdominal mass. Barium meal shows string sign or double track sign. Ultrasound confirms the diagnosis (> 4 mm pyloric muscle thickness, > 14 mm pyloric length).
Procedure of choice—Pyloromyotomy splits the hypertrophied muscle leaving the mucosa intact Ramstedt pyloromyotomy
Ref: Bailey & Love, 25/e p84–85, 1066
82. Which one of the following is the commonest complication of blood transfusion?
- Hemolytic transfusion reaction
- Transmission of Hepatitis B infection
- Transmission of human-immunodeficiency virus (HIV) infection
- Coagulopathy
Ans. a. Hemolytic transfusion reaction
Explanation
Complication maybe from Single and Massive Transfusion
Single transfusion | Massive transfusion |
|---|---|
|
|
Organism Transmitted through Blood Transfusion
- Hepatitis C virus, human immunodeficiency virus type 1, hepatitis B virus, hepatitis A virus are rarely transmitted by transfusion; TTV, SEN-V and GBV-C, West Nile virus, Cytomegalovirus, human T-lymphotropic virus (HTLV) types I and II, Parvovirus B19.
- Yersinia, Pseudomonas, Serratia, Acinetobacter and Escherichia species have all been implicated in infections related to PRBC transfusion. Gram-positive organisms including coagulase-negative staphylococci.
- Various parasites, including those causing malaria, babesiosis and Chagas disease can be transmitted by blood transfusion.
- Dengue, chikungunya virus, variant Creutzfeldt–Jakob disease, Anaplasma phagocytophilum and yellow fever vaccine virus.
Ref: High yield facts-Microbiology, 18/e p954-56; Bailey & Love, 25/e p22
83. The ‘Advanced Trauma Life Support’ system defines an order of priorities given by ABCD in which A stands for Airway, B for Breathing, C for Circulation and D for which of the following?
- Diagnosis
- Disability
- Death
- None of these
Ans. b. Disability
Explanation
Advanced Trauma Life Support (ATLS) System
- A—Airway maintenance and cervical spine protection
- B—Breathing and ventilation
- C—Circulation with hemorrhage control
- D—Disability: neurological status
- E—Exposure: completely undress the patient and assess for other injuries
Ref: Bailey & Love, 25/e p290
84. A 60-year-old female presents with gradually increasing dysphagia to solids and loss of weight. The most likely diagnosis is:
- Stricture esophagus
- Carcinoma esophagus
- Achalasia cardia
- Plummer-Vinson syndrome
Ans. b. Carcinoma esophagus
75
Explanation
Carcinoma of The Esophagus
- Cancer of the esophagus is the sixth most common cancer in the world.
- Common in mid to late adulthood with a poor survival rate.
- Squamous cell carcinoma common in upper two-thirds of the esophagus and adenocarcinoma in the lower one-third. Worldwide, squamous cell cancer is most common, but adenocarcinoma predominates in the west and is increasing in incidence.
- The cause of the disease in the endemic areas is not known, but maybe due to a combination of fungal contamination of food and nutritional deficiencies. Tobacco and alcohol are major factors in the occurrence of squamous cancer. Supplementation of the diet with beta-carotene, vitamin E and selenium may reduce the incidence.
- Dysphagia is the most common presenting symptom. Dysphagia initially for solids but eventually it progress to liquids. Weight loss > 50% cases, pain on swallowing, bone pain due to metastasis, hoarsness due to involvement of recurrent laryngeal nerve, regurgitaion may cause pneumonia and TEF due to metastasis to bronchus.
- Endoscopy is the first-line investigation for most patients Cytology and/or histology specimens taken via the endoscope are crucial for accurate diagnosis, bronchoscopy to rule out TEF. Barium swallows shows (rat tail appearance) location and extent of tumor.
Achalasia
- Achalasia is due to loss of the ganglion cells in the mysenteric (Auerbach's) plexus, cause not known. Trypanosoma cruzi causes Chagas' disease which has marked clinical similarities to achalasia.
- Most common in middle life, but can occur at any age.
- Dysphagia most common symptom (for both solid and liquid; liquid first); regurgitation is second most symptom, heart burn, chest pain usually after meal.
- Abnormal contractions in the esophageal body and a tapering structure in the distal esophagus, often described as a ‘bird's beak’ appearance on barium swallow. Gastric bubble usually absent. A firm diagnosis is established by esophageal manometry.
- T/T-heller's myotomy
Ref: Bailey & Love, 25/e p1026-1040; CSDT, 13/e p442
85. Swan-Ganz catheter is used to measure:
- Portal venous pressure
- Peripheral arterial blood pressure
- Pulmonary wedge pressure
Ans. d. Pulmonary wedge pressure
Explanation
The pulmonary artery (or Swan-Ganz) catheter is traditionally regarded as the gold standard method of cardiac output measurement at bedside. Direct measurements include cardiac output, pulmonary artery pressure, central venous pressure, right ventricular end-diastolic pressure, left ventricular filling pressure pulmonary artery wedge pressure and mixed venous oxygen saturation.
Ref: Bailey and Love, 25/e p219; Sabiston, 18/e p608; NMS medicine, 6/e p18
86. In case of HIV and TB combined infection which of the following is the line of management?
- Antiretroviral therapy should be initiated first for two weeks followed by antitubercular therapy.
- Both antitubercular and antiretroviral therapies should be initiated simultaneously
- Antitubercular therapy should be initiated first for two weeks followed by antiretroviral therapy
- Antitubercular therapy should be completed first and then anti-retroviral therapy should be initiated
Ans. b. Both antitubercular and antiretroviral therapies should be initiated simultaneously
Explanation
Some Important Point Regarding Treatment of HIV and TB Patient
- In general, the standard treatment regimens are equally efficacious in HIV-negative and HIV-positive patients.
- Three important considerations are relevant to TB treatment in HIV-infected patients:
- Increased frequency of paradoxical reactions
- Drug interactions between ART and rifamycins
- Development of rifampin monoresistance with widely spaced intermittent treatment.
- All HIV-infected TB patients should take ART and the optimal timing for its initiation is as soon as possible and within the first 8 weeks of anti-TB therapy.
Ref: Harrison, 18/e p1355
87. Syndromic management of urethral discharge comprises of, in addition to health education and partner management:
- Treatment of gonorrhea and Chlamydia
- Treatment of Klebsiella granulomatis and Chlamydia
- Treatment of Treponoma pallidum and Hemophylus ducreyi
- Treatment of gonorrhea and Treponoma pallidum
Ans. a. Treatment of gonorrhea and Chlamydia
Explanation
- Syndromic management of sexually transmitted disease (WHO, 1988).
- Women are liable to several infections in lower genital tract, most common of which are gonorrhea, chlamydia, candida infection, mycoplasma infection trichomonal infection, monilial infection and bacterial vaginosis. Therefore, syndromic management approach is implemented by giving multiple drugs in one sitting which include 1 g azithromycin, 2 g metronidazole, 150 mg fluconazole. Only those who fail to respond with this drug are subjected to further investigation.
Ref: Dutta Textbook of Gynecology, 5/e p172; Shaw, 15/e p151; Park, 22/e p306-7
88. Which of the following are the sources of infection of plague?
- Infected fleas, cases of bubonic plague and poor environmental status
- Infected rodents, cases of septicemic plague and poor environmental status
- Infected rodents, cases of bubonic plague, septicemic plague and poor environmental status
- Infected rodents, fleas and cases of pneumonic plague
Ans. d. Infected rodents, fleas and cases of pneumonic plague
Explanation
Some Important Point Regarding Plague
- Source of infection is infected rodents and fleas and case of pneumonic plague
- Incubation period of bubonic plague 2–7 days
- Incubation period of septicemic plague 2–7 days
- Incubation period of pneumonic plague 1–3 days
- Bubonic plague is most common type of disease
- Specific flea index: Average number of fleas of each species found per rodent
- Percentage incidence of flea species: Percentage of fleas of each species found per rodent
- Rodent infestation rate: Percentage of rodents infested with the various flea species
- Cheopis index: Average number of X. Cheopis per rat (if > 1, regarded as indicative of potential explosiveness of the situation should a plague outbreak occur)
Ref: Park, 22/e p267
89. In normal pregnancy, following changes occur in maternal blood except:
- Erythrocyte sedimentation rate (ESR) is increased
- Maternal blood volume increases by 15%
- Erythrocyte volume increases by 15–20%
- Absorption of iron is increased
Ans. b. Maternal blood volume increases by 15%
Explanation
Physiological Changes during Pregnancy
Value increased | Value decreased | |
|---|---|---|
Hematological changes |
|
|
Blood coagulation factors (H&B writes that factors II, V, XII remain unchanged) | Fibrinogen (+50%) factors X, IX, VIII, VII and II, I | Factors XI, XII, XIII Platelet survival time Fibrinolytic activity |
Plasma proteins |
|
|
Hemodynamic changes | Cardiac output(reaches peak + 40–50% by 30–34 wks, + 50% during labor and + 70% immediately following delivery Stroke volume (+ 27%) Heart rate (+ 17%) Heart size | Systemic vascular resistance (21%) Pulmonary vascular resistance Diastolic BP Mean atrial pressure Colloid oncotic pressure |
Endocrine and metabolic changes | BMR (+30%; total metabolism) Steroid-binding globulin Total free cortisol Insulin secretion | Blood urea Sensitivity of insulin receptor |
Lipid metabolism | Total lipid (+50%), LDL and cholesterol (+40%), HDL (+15%), triglyceride (+50%), lipoprotein | — |
Respiratory system | Tidal volume (+40%), Inspiratory capacity (IC) Respiratory minute volume CO2 sensitivity to respiratory center | All lung volume except TV (IRV, ERV, RV), functional residual capacity, total lung capacity |
Acid-base changes | pH, arterial pO2 Maternal O2 consumption | Arterial pCO2 |
Liver function test | Alkaline phosphatase | — |
Renal function test | GFR, renal blood flow, creatinine clearance | BUN, serum creatinine, Serum uric acid Peristalsis of ureter |
Gastrointestinal tract | Appetite Salivation Absorption of food | Muscle tone and motility of GIT Peristalsis |
Liver function test | Alkaline phosphate | — |
Thyroid test | Thyroid-binding globulin (TBG), total T3, total T4, thyroid gland size | T3 resin uptake |
Calcium metabolism | Calcium absorption, 1, 25-dihydroxyvitamin D3, Calcitonin level | Total calcium level |
Ref: Dutta Textbook of Obstetrics, 7/e p 51–6; BRS Obs and Gyn, 2/e p17
90. Implantation occurs on:
- 4th day post fertilization
- 6th day post fertilization
- 8th day post fertilization
- 10th day post fertilization
Ans. b. 6th day post fertilization
Explanation
Implantation occurs in the endometrium of anterior or posterior wall of the body near the fundus on the 6th day which corresponds to the 20th day of menstrual cycle.
Ref: Dutta Textbook of Obstetrics, 7/e p22
91. According to White's classification, a pregnant diabetic woman with proliferative retinopathy belongs to:
- Class D
- Class F
- Class R
- Class H
Ans. c. Class R
Explanation
White Classification of Pregnant Diabetic Women
Class | Onset | Fasting plasma glucose | 2-hours postprandial | Treatment |
|---|---|---|---|---|
A gestational diabetes | Any age | A1: glucose < 105 mg/dl A2: > 105 mg/dl | < 120 mg/dl > 120 mg/dl | Diet insulin |
Class | Age of onset | Duration (year) | Vascular disease | Treatment |
B | > 20 years | < 10 years | None | Insulin |
C | 10–19 years | 10–19 years | None | Insulin |
D | < 10 years | > 20 years | Benign retinopathy | Insulin |
F | Any | Any | Nephropathy | Insulin |
H | Any | Any | Coronary artery disease | Insulin |
R | Any | Any | Proliferative retinopathy | Insulin |
T | Any | Any | Renal transplant | Insulin |
Ref: Dutta Textbook of Obstetrics, 7/e p283
92. Which of the following high-risk factors are associated with preterm labor?
- Previous history of preterm labor
- Multiple pregnancy
- Bacterial vaginosis
- All of these
Ans. d. All of these
Explanation
Etiology of Preterm Labor
History |
| |
Complication in present pregnancy | Maternal |
|
Fetal |
| |
Placental |
| |
Iatrogenic |
| |
Idiopathic |
| |
Ref: Dutta Textbook of Obstetrics, 7/e p314
93. An elderly patient gives history of 12 weeks amenorrhoea with vaginal bleeding and the size of uterus is 16 weeks, with doughy feel and absence of internal ballotment. The clinical diagnosis is:
- Fibroid with pregnancy
- Ovarian tumor with pregnancy
- Hydatidiform mole
- Multiple pregnancy
Ans. c. Hydatidiform mole
Explanation
Hydatidiform Mole (Vesicular Mole)
- Age of onset: Young women below 20 years or in multiparous women 40 years and above
- Cytologic abnormality: Complete moles have a 46 XX karyotype (85%), the molar chromosomes are derived from father
- Association/constitutional symptom: Patient becomes sick without any reason, hyperemesis, PIH before 24 weeks in 33%, thyrotoxicosis results in supraventicular tachycardia, raised T3 and T4, breathlessness due to pulmonary embolism
- Clinical features: Vaginal bleeding is the most common presentation, ‘White currant in red currant juice’ appearance discharge, abdominal pain, excessive vomiting, breathlessness, expulsion of grape-like vesicles per vaginam is diagnostic, the size of uterus is more than that expected for period of amenorrhea, the uterus feels doughy in consistency due to absence of amniotic fluid, external and internal ballottement cannot be elicited and fetal heart cannot be heard on doppler
- Diagnosis: Characteristic echogram: Snowstorm appearance, rapidly increasing value of serum hCG (hCG > 100,000 mIU/mL) is usual with molar pregnancy (in normal pregnancy < 60,000 mIU/mL), routine use of CT or MRI for diagnosis or to detect metastasis is not recommended
- Complications: Hemorrhage, anemia, thyroid storm, embolism with acute pulmonary insufficiency and DIC, uterine perforation, delayed recurrent mole, choriocarcinoma
Ref: Dutta Textbook of Obstetrics, 7/e p191–7; Shaw, 15/e p255-840
94. Monitoring of MgSO4 therapy for eclampsia is done using all except:
- Urine output
- Knee jerks
- Fundus examination
- Serum magnesium levels
Ans. c. Fundus examination
Explanation
- The appropriate use of MgSO4. 7H2O will nearly always arrest eclamptic seizures and prevent recurrences.
- Dose: Loading dose of 10 g, IM or 4 g IV, maintenance is best achieved with continuous IV infusion 2 g/hours or 5 g IM every 4 hours. Repeat injections given only if
- Knee jerk is present,
- Urine output exceeds 30 mL/hour,
- Respiration rate > 12/minute.
- Antidote of magnesium sulfate is IV calcium gluconate.
Ref: Dutta Textbook of Obstetrics, 7/e p235; NMS Obs and Gyn, 6/e p168; BRS, Obs and Gyn, 2/e p119
95. Fetal distress is diagnosed by:
- Early acceleration
- Late acceleration
- Early deceleration
- Late deceleration
Ans. d. Late deceleration
Explanation
Deceleration pattern | Condition |
|---|---|
Early deceleration | Head compression |
Late deceleration | Uteroplacental insufficiency and fetal hypoxia |
Variable deceleration | Cord compression (most common type) |
Acceleration | Intact neurohormonal and cardiovascular activity, i.e. healthy fetus |
Ref: Dutta Textbook of Obstetrics, 6/e p612
96. Oxytocin Challenge test is used to assess the
- Fetal well-being
- Period of gestation
- Cervical ripening
- Uterine response to induction
Ans. a. Fetal well-being
Explanation
Oxytocin challenge test is invasive method to assess fetal well-being.
Interpretation are
Positive: Persistent late deceleration of FHR with >50% uterine contraction
Negative: No late deceleration or significant variable decelaration
Suspicious: Inconsistent but definite deceleration do not persist with most uterine contractions
Unsatisfactory: Poor quality recording or adequate uterine contraction not achieved.
Ref: Dutta Textbook of Obstetrics, 7/e p501
97. The most commonly used method to deliver the after coming head of breech is:
- Lovset's maneuver
- Burn Marshall technique
- Pinard's maneuver
- Mauriceau-Smellie viet technique
Ans. b. Burn Marshall technique
Explanation
- Modified Brand—Andrews method: Assisted expulsion of placenta by controlled cord traction
- Burns—Marshall method: Delivery of after-coming head in breech
- Lovset maneuver: Delivery of extended arms of complicated breech delivery
- Pinard maneuver: Frank breech extraction is done by intrauterine manipulation (for breech decomposition) to convert frank breech to footling breech
- Malar flexion and shoulder traction (modified Mauriceau–Smellie–Veit technique): Delivery of after-coming head in breech
Ref: Dutta Textbook of Obstetrics, 7/e p383–6
98. A patient with previous LSCS done for placenta praevia has come now in second stage of labor with head at +2 station. FHS is 100/ min. You will
- Do LSCS
- Apply forceps and deliver
- Start pitocin drip and augment labor
- Wait and watch
Ans. b. Apply forceps and deliver
Explanation
- Apply forceps and deliver. In this question fetus is in distress; pulse is 100/min so we cannot take risk by waiting.
- One previous LSCS which has gone to full dilatation and passed the pelvis means scar integrity is good and pelvis is adequate. So LSCS not needed.
- Contraction is also adequate because the women has progressed pretty well so no need augmentation.
- Had there been no fetal distress can just wait for normal delivery.
Ref: Dutta Textbook of Obstetrics, 8/e
99. During spermatogenesis meiotic division occurs at which cellular level?
- Spermatocyte
- Spermatid
- Spermatogonia
- Spermatozoa
Ans. a. Spermatocyte
Explanation
Ref: Dutta Textbook of Obstetrics, 7/e p19
100. Decontamination of reusable instrument is done by:
- Soaking in 1% hypochlorite solution
- Cleaning with soap and water
- Boiling
- Steaming
Ans. a. Soaking in 1% hypochlorite solution
Explanation
Decontamination is a process of cleaning an object or substance to remove contaminants such as microorganism or hazardous materials, including chemical and infectious disease, etc.
86Decontamination can be done by all the above mentioned process. Lets discuss all option one by one
- Hypochlorite: Hypochlorite are most widely used chlorine disinfectant. Most prevalent chlorine products are acquous solution of 5.25 to 6.15 percent of sodium chloride, usually called household breach. These have broad spectrum of antimicrobial without toxic residues. It is fast acting, removes dried or fixed organisms and biofilms from surface.
- Boiling: Is effective method of disinfection. It kills bacteria but not virus or spores. For killing spores, temperature above 1000 required. Boiling is suitable for disinfection of small instruments, tools which are not used for subcutaneous insertion, linen and rubber good such as gloves.
- Autoclaving (saturated steam): It acts on high temperature and pressure. They are most effective sterilizing agent. It is widely used hospital and laboratory practice. It destroy all form of life including spores and viruses. It is most effective method for sterilization of linen, dressing, gloves, syringe, certain instrument and culture media it is not suitable for plastics and sharp instruments.
Although it is not clear in questions that it want to say but among all option given above most correct is option ‘d’.
Ref: Park, 22/e p120
101. The drug of choice for the treatment of galactorrhea is:
- Danazol
- Clomiphene citrate
- Bromocriptine
- Estrogen or progestogen
Ans. c. Bromocriptine
Explanation
Treatment of choice of galactorrhoea is dopamine agonist cabergoline and bromocriptin is second choice. Among above given choice Bromocriptin is best option.
Ref: CMDT, 51/e p1076
102. The fertilization life span of the released ovum is:
- 12 hours
- 24 hours
- 48 hours
- 72 hours
Ans. b. 24 hours
Explanation
Fertilizable life span of oocyte ranges from 12–24 hours whereas that of sperm is 48–72 hours. Sperm reaches to fallopian tube only in few minute. Almost always fertilization occurs in the ampullary part of uterine tube.
Ref: Dutta Textbook of Obstetrics, 7/e p21
103. Bacterial vaginosis is caused by
- Staphylococcus aureus
- Gardenella
- Trichomonas
- Streptecoccus
Ans. b. Gardenella
Explanation
Bacterial vaginosis is caused by Gardnerella vaginalis.
Amsel Criteria for Clinical Diagnosis of Bacterial Vaginosis
Any Three of the following Four Clinical Abnormalities
- Objective signs of increased white homogenous noninflammatory vaginal discharge.
- Vaginal discharge, pH > 4.5.
- Fishy (amine) odor vaginal secretions (attributable to volatile amines such as trimethylamine) after mixed with 10% KOH-Whiff test.
- Clue cells (vaginal epithelial cells coated with coccobacillary organisms, giving them granular appearance and indistinct borders)—diagnostic of bacterial vaginosis. Clue cells are the most reliable indicator of bacterial vaginosis.
Nugent Criteria
When gram stain is applied to the discharge, assessment of the relative concentration of bacterial morphotypes characteristics of the altered flora is an acceptable laboratory method for diagnosing bacterial vaginosis.
Ref: Dutta Textbook of Gynecology, 5/e p147; William Gyn, p50
104. Maximum cardiac output during pregnancy is at:
- 12 weeks
- 28 weeks
- 32 weeks
- 40 weeks
Ans. c. 32 weeks
Explanation
See explanation of Question No. 89.
105. Which one of the following is not correct regarding normal values of semen analysis as per WHO?
- pH in the range of 7.2 to 7.8
- Sperm concentration 20 × 106/ml
- Motility 60% or more progressively motile
- Viability 75% or more live
Ans. c. Motility 60% or more progressively motile
Explanation
Semen Analysis (WHO 2010)
Semen analysis | Normal reference value |
|---|---|
Volume | 2 ml or more lower reference point is 1.5 ml |
pH | 7.2–7.8 |
Viscosity | < 3 (scale 0–4) |
Sperm concentration | 20 million/ml (lower reference value 15 million/ml) |
Total sperm count | > 40 million/ejaculate |
Motility | > 50% progressive forward motility |
Morphology | > 14% normal form (4%) |
Viability | 75% or more living |
Leukocytosis | Less than 1 million/ml |
Round cells | < 5 million/ml |
Sperm agglutination | < 10% spermatozoa with adherent particle |
Ref: Dutta Textbook of Gynecology, 6/e p222
106. What is the most common genital malignancy seen in women in India?
- Carcinoma cervix
- Endometrial carcinoma
- Ovarian malignancy
- Vulval malignancy
Ans. a. Carcinoma cervix
Explanation
Most common carcinoma in India is breast followed by cervix
Ref: Dutta Textbook of Gynecology, 6/e p325
107. A young woman of 28 years of age has to participate in a religious function on 22nd April. She has a regular menstrual cycle and is expecting her menstrual period around same time, which she wants to avoid. What will be the best advice to her?
- Prepone the period by producing withdrawal bleeding a week earlier
- Postpone the period by taking medroxy progesterone acetate everyday from 12th April, till the function is over
- Do nothing and observe
- Take high doses of oral estrogens on the previous day
Explanation
- Artificial change of date of menstruation should prefer to be defer rather than advance the date. Artificial withdrawal bleeding maybe continued for a variable period.
- Combined OCP, two tablets daily or progesterone such as norethisterone 5 mg twice daily.
- Drug should be take three to six days before the expected date and continue until the function over. Bleeding may start two to three days after withdrawal of drug.
Ref: Dutta Textbook of Gynecology, 6/e p93
108. The most common causative organism responsible for septic shock is:
- E. coli
- Bacteroids
- Clostridium
- Klebsiella
Ans. a. E. coli
Explanation
Some Important Point Regarding Septic Shock
- It is sepsis with hypotension (arterial blood pressure < 90 mm Hg systolic, or 40 mmHg less than patient's normal blood pressure) for at least 1 h despite adequate fluid resuscitation.
- Due to toxins released by microbes result in profound hyperinflammatory physiologic derangements, including hypovolemia, cardiac dysfunction and vasodilatation.
- The complex nature of shock results in progressive maldistributive hypoperfusion associated with hypovolemia due to decreased blood volume and increased vascular space.
- Cardiac output maybe decreased, normal or increased, depending on the degree of hypovolemia and the severity of the inflammatory insult.
- Sepsis is typically secondary to bacteremia caused by Gram-negative organisms such as Escherichia coli, Klebsiella, Proteus and Pseudomonas 90and less frequently due to Gram-negative anaerobes (e.g. Bacteroides), it is incidence from gram-positive bacteria (e.g. S aureus) and fungal organisms is increasing.
- Risk factors include extremes of age, diabetes, immunosuppression and history of a recent invasive procedure.
Ref: NMS Surgery, 5/e p31; CMDT, 52/e p485
109. A 30-year-old lady has severe dysmenorrhoea and dyspareunia. On examination the uterus is 8 weeks size, uniformly enlarged and there is tenderness in posterior fornix. What is the most probable diagnosis?
- Fibroid uterus
- Dysfunctional uterine bleeding
- Adenomyosis
- Endometrial carcinoma
Ans. c. Adenomyosis
Explanation
Some Important Points Regarding Adenomyosis
- It is uterine pathology characterized by the presence of ectopic foci of endometrial glands and stroma in the myometrium without direct connection with endometrial cavity.
- Maybe due to repeated child births vigorous curettage, or excess of estrogenic effect.
- Second most benign cause of enlarged nonpregnant uterus.
- Half patient has coexistence of leiomyomas.
- Prevalence is 20% in hysterectomy specimen.
- Forty percent associated with endometriosis.
- Risk factors are late reproductive period, multipara.
- Symptoms are menorrhagia, progressive increasing severe dysmenorrhea, pelvic discomfort, backache, dyspareunia and frequency of urination (due to enlarged uterus) and infertility (due to block of isthmus of oviduct as a result of extension of adenomyosis known as salpingitis isthmica nodosa).
- Signs maybe hypogastric mass arising out of pelvis and occupying midline. Usually not exceed 14 weeks gestation size, pelvic examination reveal uniform enlargement of uterus.
- Treatment is mostly hysterectomy because most women are elderly and past childbearing age.
Ref: Shaw, 15/e p475; NMS Gyn and Obs, 4/e p258; BRS Gyn and Obs, 2/e p346; Dutta Textbook of Gynecology, 5/e p304
110. Maximum duration for which lactational amenorrhoea can prevent conception is:
- 01 month
- 02 months
- 04 months
- 06 months
Ans. d. 06 months
Explanation
Menstruation | Ovulation | Contraception | |
|---|---|---|---|
Nonlactating women | First menstrual flow usually returns within 6 to 8 weeks after delivery at 6th week in 40% and at 12th week in 80% | As early as 4 weeks of delivery | Should be after 3 weeks |
Lactating women | Maybe suspended in about 70% until baby stops feeding | As early as 10 weeks of delivery | A women who is on exclusively breastfeeding, the contraceptive protection is about 98% up to 6 months |
Ref: Dutta Textbook of Obstetrics, 7/e p148, 537; NMS Obs and Gyn, 4/e p15
111. Which of the following is not a barrier method of contraceptives?
- Diaphragm
- Female condom
- Cervical cap
- Progestogen containing intravaginal ring
Ans. d. Progestogen containing intravaginal ring
Explanation
Barrier Method of Contraception
Physical method
- Condom
- Female condom
- Diaphragm (cervical cap, vault cap, vimule cap)
- Vaginal sponge
Chemical methods
- Foam (foam tablet, foam aerosol)
- Cream jellies and pastes (squeezed from tubes)
- Suppositories inserted manually
- Soluble films C films inserted manually
Ref: Park, 22/e p456
112. Cu-T 380 A intrauterine device provides effective contraception for:
- 03 years
- 05 years
- 08 years
- 10 years
Ans. d. 10 years
Explanation
Hormone-containing IUD | Release per day | Duration |
|---|---|---|
CuT 200 | — | 3 years |
CuT 200B | 50 μg/24 hours | 4 years |
CuT 380A | — | 10 years |
Nova T | 5 years | |
Multiload 250 | 60–100 μg/day | 3 years |
Multiload 375 | — | 5 years |
Progestasert | 65 μg/day | 1 year |
LNG-IUS (T-shaped device with polydimethylsiloxane) | 20 μg/day | 5 years |
Ref: Dutta Textbook of Obstetrics, 7/e p538; Park, 22/e p458
113. A lady who is using oral contraceptive pills comes with a complaint of vaginal discharge and pruritus vulvae. On local examination, there is curdy white discharge from the vagina. What is the most likely clinical diagnosis?
- Trichomonal vaginitis
- Monilial vaginitis
- Gardnella vaginitis
- Atrophic vaginitis
Ans. b. Monilial vaginitis
Explanation
Diagnostic Features and Management of Vaginal Infection
Features | Normal vaginal examination | Vulvovaginal candidiasis | Trichomonal vaginitis | Bacterial vaginosis |
|---|---|---|---|---|
Etiology | Uninfected, lactobacilli | Candida albicans, moniliasis | Trichomonas vaginalis | Gardnerella vaginalis, various anaerobic |
Incidence | — | 2nd most common in the United States | 3rd most common | Most common in the united states |
Typical symptoms | None | Intense itching and burning | Foul odor, valvular irritation, pruritus | 50%—asymp-tomatic, malodorous slightly |
Discharge
| Variable, usually scanty Clear Nonhomogenous, flocular | Scanty White (curdy) Thick | Profuse Green/yellow Frothy | Moderate Gray Homogenous |
Vaginal pH | 3.8–4.2 | ≤ 4.5 | ≥ 5 | > 5 |
Pruritus | -- | __++ | +++ | Nonirritating |
Diagnosis:
| None | Valvular erythema and edema with patchy adherent ‘cottage cheese like’ | Punctuations (strawberry cervix) | |
| None | May present | Present | |
Microscopy |
| Pseudohyphae | Motile organism—100% specific |
|
Treatment | None |
| Metronidazole— 2 g single dose, 200 mg × TID for 7 days | Metronidazole (200 mg × TID for 7 days) |
Ref: Harrison, 18/e p1102; Dutta Textbook of Gynecology, 6/e p158-60; William Gyn p50
114. The combined oral contraceptive pills decrease the risk of the following except:
- Endomentrial cancer
- Ovarian cancer
- Breast cancer
- Ectopic Pregnancy
Ans. c. Breast cancer
Explanation
Benefits of oral contraceptive pills | |
|---|---|
1. Contraceptive benefits | 2. Noncontraceptive benefits |
|
|
Ref: Dutta Textbook of Gynecology, 6/e p466-7; Park, 21/e p465; BRS, 2/e p272
115. In comparison to conventional vasectomy, which of the following statements is not true about no-scalpel technique of vasectomy?
- No-scalpel vasectomy is equally effective
- Less tissue injury leads to less bleeding
- The people appear to be less apprehensive about it
- Vas can be easily identified
Ans. d. Vas can be easily identified
Explanation
Some Important Point Regarding No Scalpel Vasectomy (NSV)
- No scalpel vasectomy is a surgical attempt to reduce complications and thereby always the fear in the minds of the couples.
- No scalpel vasectomy is gold standard for vasectomy today. Training is mandatory for experienced surgeons. Expertise needed for to identify vas.
- No scalpel vasectomy is truly minimally invasive with minimal scrotal handling, minimal instrumentation, minimal pain, minimal dissection, minimal time taken for surgery, minimal complications, minimal postoperative rest, minimal dressing, minimal drugs, minimal follow-up—10 Ms of NSV, which result in maximal client satisfaction.
Postvasectomy Precautions
- Additional contraceptive protection needed for about 2–3 months following operations.
- It requires about 20 ejaculations to empty the stored semen.
- Semen should be examined once a month and then again at 2 months and if the two consecutive semen analyses show an absence of spermatozoa, the man is declared as sterile.
Ref: Dutta Textbook of Obstetrics, 7/e p553; Park, 21/e p471; Chaudhuri Practice of Fertility Control, 5/e p178
116. Following are the methods of emergency contraception except:
- Intrauterine devices inserted within 7 days of unprotected sex
- Yuzpe regimen
- Single tablet of Mala D
- Levonorgestrel only regimen
Ans. c. Single tablet of Mala D
Explanation
Emergency Contraceptives Are Taken After Intercourse
- These are ethinyl estradiol 2.5 mg, premarin (conjugated estrogen)—the drug taken twice daily for 5 days and should be started within 72 hours of intercourse.
- Combined hormonal regimen (Yuzpe method) is equally effective. Two tablets should be taken as early as possible or within 72 hours of intercourse and two more tablets are taken 12 hours of first dose
- Levonorgestrel—two doses given at 12 hours interval and should be started as early as possible within 72 hours. Its failure rate is 1.1%.
- Antiprogesterone (RU-486, mifepristone) acts as a contraceptive. A single dose of 10 mg is effective in preventing pregnancy in 99.1% cases (failure rate: 0.9%).
- Centchroman—two tablets (60 mg) taken twice in a day within 24 hours prevent implant upto 99% of cases.
- Ulipristal acetate as an emergency contraceptive is as effective as levonorgestrel. A single dose of 30 mg to be taken orally as soon as possible within 120 hours of coitus.
Ref: Dutta Textbook of Gynecology, 6/e p472-3; Shaw, 15/e p237
117. Which one of the following is the most sensitive indicator for assessing Maternal and Child Health Services?
- Infant mortality rate
- Perinatal mortality rate
- Still birth rate
- Postneonatal mortality rate
Ans. a. Infant mortality rate
Explanation
Indicator of MCH Services
- Maternal mortality ratio; it measure women dying from puerperal causes.
- Mortality in infancy and childhood
- Perinatal mortality rate.
- Neonatal mortality rate.
- Postneonatal mortality rate.
- Infant mortality rate:
- The ratio of infant deaths registered in a given year to the total number of live births registered in the same year.
- Most important indicator of the health status of a community but also of the level of living of people in general and effectiveness of MCH service in particular. It get separate treatment by demographer because
- Infant mortality is largest single age category mortality
- Death at this age are due to a peculiar set of disease and condition to which adult population is less exposed or less vulnerable
- Infant mortality is affected rather quickly and directly by specific health programs and hence change more rapidly than the general death rate
- 1–4 years mortality rate
- Under -5 mortality rate
- Child survival rate.
Objective of Maternal and Child Health are
- Reduction of maternal, perinatal, infant and childhood mortality and morbidity
- Promotion of reproductive health
- Promotion of physical and psychological development of the child and adolescent within the family. The ultimate objective is lifelong health.
Ref: Park, 22/e p516, 482, 525
118. Essential obstetric care includes:
- Early registration in first 12-16 weeks
- Antenatal checkups
- Providing tetanus immunization and iron folic acid tablets
- All of these
Ans. d. All of these
Explanation
Essential obstetric suppose to provide the basic maternity services to all pregnant women through
- Early registration of pregnancy (between 12–16 weeks)
- Provision of minimum three antenatal checkup by ANM or medical officer to monitor progress or the pregnancy and to detect any risk/complication so that appropriate care done
- Provision of safe delivery at home or in the institution
- Provision of three post natal checkups to monitor the post natal recovery and to detect complication
Ref: Park, 22/e p416
119. Blood storage facility is available at:
- Village level
- Subcentre level
- CHC level
- PHC level
Ans. c. CHC level
Explanation
One community health center should covering population of 80,000 to 1.20 lakh with 30 beds and one specialists in surgery, one medicine, one obstetrics and gynecology and one pediatrics with X–ray and laboratory facility. Every CHC has to provide following services
- In surgery incision and drainage, surgery for hernia, Hemorrhoid, appendicitis, fistula, hydrocele and handling emergency like intestinal obstruction and Hemorrhage, etc.
- In medicine all emergency as per national health programs like dengue/DHF, cerebral malaria, etc.
- Essential and emergency obstetric care including CS
- Full range of family planning services including laparoscopic services
- Safe abortion services
- Newborn care
- Routine and emergency care of sick children
- Other management including nasal packing, tracheostomy, foreign body removal
- All national health programs delivered through CHC
- Blood storage facility
- Essential laboratory services
- Referral services.
Ref: Park, 22/e p847
120. Unmet needs of contraception covers all the following groups except:
- All women who are sexually active, are not using contraception and want more children
- All women who are sexually active and are not using contraception, either do not want more children or want to postpone the next birth
- Pregnant married women whose pregnancies are unwanted
- Women who have recently delivered and are in lactational amenorrhoea
Ans. a. All women who are sexually active are not using contraception and want more children
Explanation
- The concept of unmet need of family planning was first explored in 1960
- Many women who are sexually active would prefer to avoid becoming pregnant, but not using any contraceptive including their partner. These women are considered to have an ‘unmet need’ of family planning
- Unmet need can be powerful concept of family planning
- Most common reason of unmet need are inconvenient or unsatisfactory services, lack of information, fears about contraceptive side effect and opposition from partner or relatives
- It is highest among women below 20 years of age and is almost always for spacing birth. Above 30 years it is used mainly for limiting the birth
- It is higher in rural area than urban area and low in muslim than hindu and Christians.
Ref: Park, 22/e p471
121. Emergency obstetric care facility of first referral unit includes the following:
- Twenty four hour delivery services normal and assisted
- Safe abortion services
- All of these
Ans. d. All of these
Explanation
In RCH II phase the minimal emergency obstetric care service to be provided by fully functional first referral unit are:
- Twenty four hours delivary services including normal and assisted delivary
- Emergency obstetric care including surgical interventions like cesarian sections
- Newborn care
- Emergency care of sick children
- Full range of family planning service including laparoscopic service
- Safe abortion service
- Treatment of STI/RTI
- Blood storage facility
- Essential laboratory services
- Referral services.
Ref: Park, 22/e p418
122. Who is the implementing worker at the grass root level under Janani Suraksha Yojana?
- Health Care Worker female
- Anganwadi Worker
- Accredited Social Health Activist
- Trained Birth Attendant
Ans. c. Accredited Social Health Activist
Explanation
The national maternity benefit scheme has been modified into a new scheme called Janani Suraksha Yojana. it was launched in 12 April 2005. Objective of this scheme are reducing maternal mortality and infant mortality through encouraging delivery at health institutions and focusing at institutional care among those women who are below poverty line families.
The accredited social health activist would work as a link health worker between the poor pregnant women and public sector health institution in the low performing states like Bihar, Jharkhand, UP, Chattisgarh, etc. Accredited social health activist (ASHA) should responsible for making available institutional antenatal as well as postnatal care. She would also responsible for escorting the pregnant women to the health centre.
Ref: Park, 22/e p419
123. In induction of ovulation clomiphene citrate acts as:
- Gonadotropin
- Progesterone
- Antiprogesterone
- Antiestrogen
Ans. d. Antiestrogen
Explanation
Clomiphene citrate is nonsteroidal commercially available in the form of two isomers clomiphene is potent Antiestrogen and zuclomiphene is weakly estrogenic. It Blocks estrogen receptor in the hypothalamus → increase GnRH pulse amplitude → increase gonadotropin secretion from pituitary.
Ref: Dutta Textbook of Gynecology, 6/e p510
124. WHO recommended strategy for control of trachoma is identified by which one of the following abbreviations?
- SAFE
- STOP
- VISION 2020
- BEAT
Ans. a. SAFE
Explanation
Trachoma is controlled by a WHO endorsed integrated strategy of surgery for trichiasis, antibiotic therapy, facial cleanliness and environmental improvement which is known by acronym SAFE. This strategy is based on evidence from field trials and is continually being refined. Progress can be measured using the WHO endorsed simplified grading system to measure trachoma prevalence; this allows comparison between and within countries. The ‘S’ component of lid surgery for trachomatous trichiasis is believed to reduce the risk of progressive corneal opacification and blindness. The A component of antibiotic has two advantages, first to reduce each patient's risk of developing pathologically significant conjunctival scarring and second to limit transmission of infection to others. Mass treatment with single dose of oral azithromycin is effective and feasible, well tolerated, relatively free from side effects. The ‘F’ and ‘E’ components of the SAFE strategy (facial cleanliness and environmental improvement) are frequently described together since their primary function is to prevent transmission rather than to treat trichiasis or infection. A series of risk factor analysis found an association between not having of a clean face and an increased individual likelihood of having signs of active trachoma, suggesting the face washing could reduce the prevalence of trachoma. Eye-seeking flies have been associated with trachoma for hundreds of years but fly control was not incorporated into national trachoma plans 101because there was no evidence that investment in fly control would have an impact on trachoma transmission.
The STOP strategy is for tuberculosis.
VISION 2020: The Right to Sight—India is a national forum for eliminating avoidable blindness by year 2020. It is a key driver of the World Health Organization (WHO) and International Agency for the Prevention of Blindness (IAPB) joint global initiative for eliminating avoidable blindness.
Ref: Park, 22/e p407; Journal of Community Eye Health (Vol. 7, Issue 14)
125. One of the following is not a risk factor for common cancers:
- Tobacco chewing
- Alcohol consumption
- Obesity
- Mental stress
Ans. d. Mental stress
Explanation
Risk Factors for Cancer
- Tobacco: Major cause of cancer of lung, larynx, mouth, pharynx, esophagus, bladder, pancreas and kidney
- Alcohol: May cause esophagus and lung cancer, rectal cancer
- Dietary factor: smocked fish (stomach cancer), dietary fibre (intestinal cancer), beef (bowel cancer)
- Occupational exposure: Benzene, arsenic, cadmium, chromium, vinyl chloride, asbestos, polycyclic hydrocarbons, etc.
- Viruses: Hepatitis B and C (hepatocellular carcinoma), HIV (Kaposi sarcoma, nonhodzkins lymphoma), EBV (Burkitt's lymphoma, naso-pharyngeal carcinoma), CMV (Kaposi sarcoma), HPV (cervical cancer), shcistosomiasis bladder (cancer)
- Customs, habits and lifestyles: Tobacco betel chewing (oral cancer), smocking (lung cancer)
- Others: Sunlight, radiation, air and water pollution, medications
- Genetic: Retinoblastoma occur in children of the same parents, monglian more like to develop cancer.
Ref: Park, 22/e p356
126. All of the following are true about epidural analgesia in labor except:
- It is the most effective form of labor analgesia
- It aims at achieving T10 sensory level
- It can be extended to provide surgical anaesthesia for cesarian section
- It should not be given in early labor
Ans. d. It should not be given in early labor
Explanation
Some Important Point Regarding Epidural Analgesia
- It is safest and simplest method of proceeding labor
- A lumber puncture is made between L2 and L3 level
- For complete analgesia block from T10 to S5 dermatome needed
- For cesarean delivery a block from T4 to S1 needed
- Epidural analgesia as general rule should be given when labor is well stabilized
- Patient BP, pulse and heart rate monitored every 15 minutes
- Benefit:
- Pregnancy induced hypertension, breech presentation, twin pregnancy, preterm labor, previous CS is not contraindication. It does not change 1st stage of labor but prolong 2nd stage of labor
- Contraindication:
- Maternal coagulopathy or anticoagulant therapy
- Supine hypotension
- Hypovolemia
- Neurological disease
- Spinal deformity or chronic low back pain
- Skin infection at injection.
Ref: Dutta Textbook of Obstetrics, 7/e p517
127. The Physical Quality of Life Index consolidates the indicators:
- Infant mortality, life expectancy at age one and literacy
- Infant mortality, per capita caloric consumption and literacy
- Perinatal mortality, life expectancy at birth and per capita caloric consumption
- Neonatal mortality, life expectancy at birth and per capita caloric consumption
Ans. a. Infant mortality, life expectancy at age one and literacy
Explanation
Physical Quality of Life Index (PQLI)
- Indicators—infant mortality, life expectancy at one year of age and literacy
- Scaled 0–100
- It measures result of social, economic and political policies.
Human Development Index (HDI)
- Indicators—longevity (life expectancy at birth), knowledge (adult, literacy rate and mean years of schooling) and income (real GDP per capita in purchasing power)
- HDI for India is 0.612.
Ref: Park, 22/e p16
128. In which one of the following diseases, carrier status is not an important source of transmission?
- Typhoid
- Poliomyolitis
- Diphtheria
- Measles
Ans. d. Measles
Explanation
Typhoid |
|
Poliomyelitis |
|
Diphtheria |
|
Measles |
|
Although in polio, rubella and measles main source of infection is a case. But among all answer given above most correct answer is option ‘d’.
Ref: Park, 22/e p215, 185, 138
129. In which one of the following, typhoid bacilli can live longest?
- Ice cream
- Soil irrigated with sewage
- Water
- Sweets
Ans. b. Soil irrigated with sewage
Explanation
Outside of human body typhoid bacilli are found in water, ice, food, milk and soil for varying period of time.
- It do not multiply in water, many of them perish within 48 hours, but some may survive for about 7 days
- It may survive for more than one month in ice and ice cream
- It grow rapidly in milk without altering its taste.
Ref: Park, 22/e p215
130. Following is not a measure of health promotion:
- Immunization
- Health education
- Environmental modifications
- Nutritional intervention
Ans. a. Immunization
Explanation
Mode of Intervention
- Health promotion: By health education, environmental modifications, nutritional interventions, lifestyle and behavioral changes
- Specific protection:
- Immunizations
- Specific nutrients
- Chemoprophylaxis
- Protection against occupational hazards
- Protection against accidents
- Protection from carcinogens
- Avoidance of allergens
- Control of air pollution, noise control, consumer product quality and safety of foods, drugs and cosmetics.
- Early diagnosis and treatment
- Disability limitation
- Rehabilitation.
Ref: Park, 22/e p40-41
131. Which of the following diseases are subject to International Health regulations?
- Cholera
- Hepatitis B
- HIV/AIDS
- None of these
Ans. a. Cholera
Explanation
Under international health regulations certain disease are notified by the national health authority to WHO. These may divide into two group
- Those disease subject to international health regulation, third annotated edition 1983: cholera plague, yellow fever.
Ref: Park, 22/e p112
132. Which one of the following is not a control measure for epidemic of human plague?
- Vaccination
- Chemoprophylaxis
- Disinfection
- Rodent control
Ans. a. Vaccination
Explanation
Prevention and Control of Plague
- Control of cases
- Early diagnosis: During epidemic diagnosis done on clinical ground i.e. acute fever and painful lymphadenopathy.
- Notification: If a human or rodent cases is diagnosed it must be notified promptly.
- Isolation: Must bubonic case are noninfectious but it must be isolated as well as pneumonic plague cases.
- Treatment must started without confirming diagnosis—TOC is streptomycin.
- Disinfection: Disinfection of sputum discharge and article soiled by the patient should be carried out.
- Control of fleas
- The most effective method to break chain of transmission (rodent-rat-man) by killing fleas. DDT and BHC should be used. All wall up to 3 feet above floor should be sprayed. Insecticidal spraying up to a radius of 5 miles of infected locality is adequate. Within 48 hours flea index should be drop to zero.
- Control of rodents
- Continuous mass destruction of rodent is an important plague preventive measures
- Vaccination
- It is valuable preventive measure. WHO recommends that under all circumstances, vaccine should be only for the prevention not for control of human plague. Two doses of vaccination should be carried out at least one week before an anticipated outbreak, at difference of 7–14 days.
- Chemoprophylaxis
- Is a valuable preventive measure and highly recommended. DOC is tetracycline
-
- In area where natural foci exists or where there is history of past infection surveillance is essential.
- Health education
- It is an essential part of any plague control program.
Ref: Park, 22/e p270-1
133. Which one of the following is correctly matched in relation to available human resources?
- Community Health Centre ____ Medical Specialist in Paediatrics
- Health Sub-centre ____ Medical Specialist in General Medicine
- Primary Health Centre ____ Gynaecologist
- ICDS Centre ____ Medical Officer
Ans. a. Community Health Centre ____ Medical Specialist in Paediatrics
Explanation
See explanation of question 119. Medical officer at PHC level
Ref: Park, 22/e p848
134. The first step in conducting an epidemic investigation is:
- Determining the number of cases
- Determining the population at rise
- Verifying the diagnosis
- Calculating the incubation period
Ans. c. Verifying the diagnosis
Explanation
Investigation of Epidemic
- Verification of diagnosis (first step in epidemic investigation)
- Confirmation of the existence of an epidemic (next step)
- Definition of population at risk
- Rapid search for all cases and their characteristics
- Data analysis
- Formulation of hypothesis
- Testing of hypothesis
- Evaluation of ecological factors
- Further investigation of population at risk
- Writing the report.
Ref: Park, 22/e p122-3
135. A cholera case differs from the case of food poisoning on following points except:
- Incubation period in cholera is longer, i.e. tow to five days
- Frequent effortless purging
- Rice watery stools
- Fever, fast pulse and headache
Ans. b. Frequent effortless purging
Explanation
Differential Diagnosis of Cholera and Food Poisoning
Cholera | Food poisoning | |
|---|---|---|
Epidemiology | Often in epidemic form Secondary cases occurs | Often a single group of person shared a common meal No secondary cases |
Incubation | Few hours to five days | 1–24 hours |
Onset | With purging | With vomiting |
Nausea | None | Present |
Retching | None | Present |
Vomiting | Projectile, effortless, watery and continuous | Often single, severe vomit, mucus and blood stained |
Stools | Copious rice watery in offensive | Frequent, offensive, may contain mucus and blood |
Tenesmus and abdominal tenderness | None | Yes |
Dehydration | Very marked | Distinct |
Muscular cramps | Constant and severe | Less constant |
Surface temperature | Subnormal | Often up to 100–102°F |
Headache | None | Often |
Urine | Suppressed | Seldom suppressed |
Blood | Leukocytosis | Normal |
Ref: Park, 22/e p218
136. Sampling technique which selects every fifth person from a community is called:
Ans. b. Systematic sampling
Explanation
Simple random sample | Stratified random sample | Systemic random sample | Cluster samples |
|---|---|---|---|
Is the simplest probability sample. It is a sample drawn so that every element in the population has equal probability of being included. The random sample is defined by the method of drawing the sample not by outcome. Random samples are haphazard collection of certain numbers, arranged in cunning manner to eliminate personal selection of unconscious bias in taking out the sample. A sample or a result demonstrates relative bias if it consistently moves in a particular direction. Biased samples are therefore unrepresentative | In this sample, the population is first divided relatively into internal homogenous strata or groups, from which random sample is then drawn. This stratification represents greater representativeness, e.g., instead of drawing one sample of 50 people from total population consisting of 1,000 white and 1,000 black people (or Hindu, Muslim, Christian, age group), two random samples of 25 could be taken from each racial group separately, thus guarantee the racial representativeness of the resulting overall sample of 50 | This involves choosing elements in a systemic way, such as, selecting every fifth patient admitted to a hospital, or every third infant born in a given area. This type of sampling provides the equivalent of a simple random sample without actually using randomization, | This maybe used when it is too laborious to draw a sample random or stratified random sample, e.g. in a survey of medical students in India. An investigator might start by selecting a random set of group or ‘clusters’—such as a random set of 10 medical colleges in India. In cluster sampling, the clusters are sampled randomly and all members of cluster are sampled. This method is much more economical and practical. |
Ref: Park, 21/e p792; High Yield Biostatics, p1, 2
137. Humoral immunity is effective against which of the following?
- Mycobacterium leprae
- Candida albicans
- Mycobacterium tuberculosis
- Clostridium tetani
Ans. d. Clostridium tetani
Explanation
Humoral immunity comes from B-Cells (bone marrow derived lymphocytes) which proliferate and manufacture specific antibodies after antigen presentation by macrophage. Although antibodies are quite effective in combating most infectious disease, humoral immunity does not cover all 109the situation that one finds in infectious disease for example, M. Laprae, M tuberculosis, S typhi, candida albicans and many virus infection escape from bactericidal action of leucocyte.
Ref: Park, 22/e p98
138. If the specificity of the test was 80% and the sensitivity remains the same in a population with 50% prevalence, the positive predictive value of the test will be:
- 90%
- 80%
- 70%
- 60%
Ans. b. 80%
Explanation
In this question sensitivity is 80%, i.e. 0.8, specificity is same, i.e. 0.8 and prevalence is 50%, i.e. 0.5
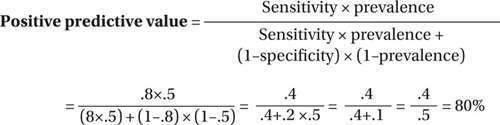
139. Prevalence of a disease affects:
- Sensitivity of a test
- Specificity of a test
- Positive predictive value of a test
- Dependability of a test
Ans. c. Positive predictive value of a test
Explanation
In addition to sensitivity and specificity, the performance of a screening test is measured by its ‘predictive value’. It reflects the diagnostic power of disease. Predictive accuracy depends upon the sensitivity, specificity, and disease prevalence. More prevalent a disease in a given population, the more accurate will be the predictive value of positive screening test.
Ref: Park, 22/e p132
140. ‘The number of daughters a newborn girl will bear during her life time assuming fixed age specific fertility and mortality rates’ is referred to as:
Ans. b. Net reproduction rate
Explanation
Gross reproductive rate (GRR): Average number of girls that would be born, if a women experiences the current fertility pattern throughout her reproductive span (15–44 or 49 years), assuming no mortality.
Net reproduction rate: Defined as number of daughter a women will bear during her lifetime assuming fixed age specific fertility and mortality rates. The NRR is demographic indicator. NRR of 1 is equivalent to attaining approximately the 2-child norm. If NRR < 1 means reproductive performance of population is below replacement level.
General fertility rate (GFR): Number of live births per 1000 women in the reproductive age group (15–44 or 49 years) in a given year.
Age specific fertility rate: Number of live birth in a year to 1000 women in any specific age group.
Ref: Park, 22/e p451-2
141. All of the following statements are true of case control studies except:
- Requires relatively few subjects
- Suitable to investigate rare diseases
- Attrition problem of study population is present
- Matching removes confounding bias
Ans. c. Attrition problem of study population is present
Explanation
Some Important Point Regarding Case Control Study
- Both exposure and outcome has occurred before the start of study
- It proceed backward from effect to cause
- Relatively easy to carry-out. It is rapid and in expensive
- Require comparatively few subjects
- Suitable to investigate rare disease or disease about which little known
- No risk to subject
- Allow the study of several different etiological factors
- Risk factor can be identified
- No attrition problem because it do not require follow-up
- Minimal ethical problem
- Confounding bias removed by matching in this study, selection bias can be best controlled by prevention, interviewer bias can be eliminated by double-blinding.
Ref: Park, 22/e p71
142. ASHA posted at village level under National Health Mission should meet the following qualifications except:
- She should be residing in the same village
- She should be unmarried
- She should be able to communicate with villagers in the local language
- She should be literate
Ans. b. She should be unmarried
Explanation
Some Important Points Regarding ASHA
- She should be resident of village.
- A women (married, divorcee, or widow) preferably age of 25–45 years with formal education up to 8th class having communication skills and leadership quality.
- General norm is selection of one ASHA for 1,000 population.
There is a general norm followed by the government to select ASHA that at least each village should have the population of 1000.
Roles and Responsibilities of ASHA
- Bring awareness and provide information to the community on determinants of health such as nutrition, basic sanitation and hygienic practices, healthy living and working conditions, information on existing health services, and the need for timely utilization of health and family welfare services.
- Counsel women on birth preparedness, importance of safe delivery, breastfeeding and complementary feeding, immunization, contraception and prevention of common infections including reproductive tract infection/sexually transmitted infection (RTIs/STIs), and care of the young child.
- Mobilize the community and help them in accessing health and health-related services such as immunization, Ante Natal Check-up (ANC), Post Natal Check-up (PNC), ICDS, sanitation, and other services being provided by the government available at the village/subcenter/primary health centers.
- Arrange escort/accompany pregnant women and children requiring treatment/admission to Primary Health Centre/Community Health Centre/First Referral Unit (PHC/CHC/FRU).
- Provide primary medical care for minor ailments such as diarrhea, fevers, and first aid for minor injuries. She is a provider of Directly Observed Treatment Short-course (DOTS) under Revised National Tuberculosis Control Programme (RNTCP).
- Promote construction of household toilets under total sanitation campaign.
Ref: http://www.mohfw.nic.in/eag/ROLES.htm; Park, 22/e p413
143. CSF examination in a case of tubercular meningitis shows all of the following except:
- Elevated protein levels
- Raised sugar level
- Low chloride level
- Lymphocytosis
Ans. b. Raised sugar level
Explanation
CSF Parameters in Health and Some Common Disorders
Normal | Subarachnoid hemorrhage | Acute bacterial meningitis | Viral menin gitis | Tuberculous meningitis | Multiple sclerosis | |
|---|---|---|---|---|---|---|
Pressure | 50–180 mm of water | Increased | Normal/increased | Normal | Normal/increased | Normal |
Color | Clear | Blood-stained
xanthochromic | Cloudy | Clear | Clear/cloudy | Clear |
Red cell count ×106/L | 0–4 | Raised | Normal | Normal | Normal | Normal |
White cell count ×106/L | 0–4 | Normal/slightly raised | 1,000–5,000 polymorphs | 10–2,000 lymphocytes | 50–5,000 lymphocytes | 0–50 lymphocytes |
Glucose | > 60% of blood level | Normal | Decreased | Normal | Decreased | Normal |
Protein | < 0.45 g/L | Increased | Increased | Normal/increased | Increased | Normal/ Increased |
Microbiology | Sterile | Sterile | Organisms on Gram stain and/or culture | Sterile/virus detected | Ziehl-Neelsen/auramine stain or tuberculosis culture positive | Sterile |
Oligoclonal bands | –ve | –ve | Can be +ve | Can be +ve | Can be +ve | Often +ve |
Ref: Devidson, 21/e p1147
144. All of the following are Jone's major criteria for rheumatic fever except:
- Arthralgia
- Carditis
- Subcutaneous nodule
- Chorea
Ans. a. Arthralgia
Explanation
Some Important Points Regarding Acute Rheumatic Fever
Jones criteria for diagnosis of rheumatic fever: two major criteria/one major or two minor criteria with essential criteria needed for diagnosis of acute rheumatic fever.
Major criteria | Feature |
|---|---|
1. Carditis | The rheumatic carditis is a pancarditis (early manifestation). Those who develop carditis, among them 80% develop within 2 weeks of onset of fever. Pericarditis associated with small effusion; never develop tamponade or constrictive pericarditis. Pericarditis always has additional mitral or mitral and mitral and aortic regurgitation murmur. Features of myocarditis are (soft first sound, cardiac enlargement, protodiastolic S3 gallop, CCF, Carry Coombs' murmur– a soft mid (delayed) diastolic murmur may sometimes be heard in patients with acute rheumatic fever. Endocarditis represented by pansystolic murmur with or without aortic regurgitation. Pathologically mitral valve involves all cases of RF, pulmonary valve is never involved. Mitral regurgitation is characterized by high pitched apical holosystolic murmur radiating to axilla. |
2. Arthritis | It is early manifestation. Migrating polyarthritis with affected joint showing redness, warmth, swelling, pain, and limitation of movement, involving large joined like knees, ankles and elbows. Small joint uncommon. Pain and swelling last for 3 to 7 days and subside spontaneously and appear in other joint. No residual damage to joint. Incidence is directly proportional to age. |
3. Subcutaneous nodules | It is late manifestation; appear around 6 weeks after rheumatic fever in bony prominence like elbow, shin, occiput, and spine. It is non tender. Patient having subcutaneous nodules almost always have carditis. It lasts from few days to weeks. |
4. Chorea | Sydenham chorea: it is late manifestation. it usually presents as an isolated, neurologic behavior disorder. Emotional lability, incoordination, poor school performance, uncontrollable movement, and facial grimacing exacerbated by stress and disappearing with sleep are characteristic. It is occasionally unilateral. Phenobarbitone is drug of choice. Antiinflammatory not indicated. Untreated it has self-limiting course of 2 to 6 weeks. It resolves without sequelae. |
5. Erythema marginatum | Early manifestation. Nonitching, faintly reddish rash with pale center predominantly seen over trunk. |
Minor criteria | Feature |
Clinical | |
1. Fever | Temperature rarely goes above 39.5°C, it present almost in 90% patients. |
2. Arthralgia | It is a subjective pain whereas arthritis is subjective symptom and sign. It Present in 90% patients. |
3. Previous rheumatic fever or rheumatic heart disease | It is only applicable for second attack or rheumatic fever. |
Laboratory | |
Acute phase reactant; leukocytosis elevated sedimentation rate and C- reactive protein | Polymorphonuclear. Leukocytosis, increased sedimentation rate (4 to 10 weeks) and increased C-reactive protein. TLC is usually 10,000 to 15,000/cmm. Absence of C-reactive protein is strongly against the diagnosis of acute rheumatic fever. Absence of it maybe seen in patient treated with steroid. |
Prolong PR interval in ECG | Prolong PR interval is not diagnostic criteria. Prolong QTc is suggestive of myocarditis. |
Essential criteria | Feature |
Evidence of recent streptococcal infection, as indicated by | |
Increase ASO titer | Most useful is presence of antibodies against streptococci. Increased titer of ASO is more useful in diagnosis of recent streptococcal infection. |
Positive throat culture | Positive throat culture is uncommon. This only shows presence of Streptococci and not infection. |
Recent scarlet fever | It is presence of residual of scarlet fever. The desquamation of skin of palms and soles indicates that patient have scarlet fever in previous 2 weeks. |
Treatment
After obtaining throat swab culture, patient should be treated with penicillin. For primary and secondary prevention. Intramuscular benzathine penicillin is mandatory for prevention of rheumatic fever. Aspirin and steroids are given as suppressive therapy.
Ref: Nelson, 19/e p1144; Ghai, 7/e p380–82
145. A three year old child can do all of the following except:
- She can use hands and feet simultaneously
- She can copy a square
- She can throw a ball without losing balance
- She can ride bicycle
Ans. b. She can copy a square
Explanation
Milestones | Age | Milestones | Age |
|---|---|---|---|
Sitting with support | 5 months | Crawling | 8 months |
Sitting without support | 8 months | Indicate desire by pointing | 15 months |
Reach out to an object and hold it by bidextrous grasp | 5 months | Makes towers of 2 cubes | 15 months |
Can transfer object from one hand to other by | 5–7 months | 4 cubes | 16–24 months |
Hold the cube in palm in crude manner (palmar grasp) | 7 months | 6 cubes | 22 months |
Holding the object with index finger and thumb (pincer grasp) | 9–10 months | Scribbles spontaneously | 1½ years (12 – 24 months) |
Monosyllabic babble (Nelson) | 6 months | Horizontal or vertical line | 2 years |
Throw and catch ball | 3 years | ||
Stand with support | 9 months | Copies circle | 3 years |
Stand without support | 12 months | Copies a cross or plus sign | 4 years |
Wave “bye-bye” | 9 months | Copy squire | 4.5 years |
Creeping | 10 months | Tilted cross (multiplication sign) | 5 years |
Ref: Ghai, 6/e p327; 7/e p321; Ghai, 8/e p51; Nelson, 19/e p26
146. Which of the following is an absolute contraindication for pertussis vaccine?
Ans. d. Progressive neurological disease
Explanation
Contraindications to Some Important Vaccines are given below:
Vaccine | Contraindication |
|---|---|
All | All anaphylactic reaction to previous dose of a particular vaccine |
Live vaccine (MMR, BCG, yellow fever, etc.) | Pregnancy Radiation therapy (i.e., total body radiation) |
Yellow fever | Egg allergy Immunodeficiency |
BCG | Symptomatic HIV infection |
Influenza, yellow fever | History of anaphylactic reaction following egg ingestion |
Pertussis containing | Anaphylactic reaction to pervious dose Evolving neurological disease(uncontrolled epilepsy or progressive encephalopathy) |
Ref: Park, 21/e p109; Park, 22/e p111
147. What is the dose of paracetamol in children?
- 5 mg/kg of body weight
- 15 mg/kg of body weight
- 25 mg/kg of body weight
- 30 mg/kg of body weight
Ans. b. 15 mg/kg of body weight
Explanation
Dose of paracetamol is 40–60 mg/kg/day PO, 4–6 hourly or 15 mg/kg/dose 4–6 hourly; 5 mg/kg IM
Ref: Ghai, 8/e p739
148. The mode of inheritance of hereditary elliptocytosis is:
- Autosomal dominant
- Autosomal recessive
- X-linked recessive
- X-linked dominant
Ans. a. Autosomal dominant
Explanation
See explanation of Question No. 2.
149. What is the correct amount of fluid for the treatment of severe dehydration in a two year old baby?
- 30 ml/kg in first half hour and 70 ml/kg in next two and half hours
- 50 ml/kg in first half hour and 50 ml/kg in next two and half hours
- 30 ml/kg in first hour and 70 ml/kg in next 5 hours
- 50 ml/kg in first hour and 50 ml/kg in next 5 hours
Ans. a. 30 ml/kg in first half hour and 70 ml/kg in next two and half hours
Explanation
Treatment Plan of Rehydration Therapy in:
Intravenous fluid immediate therapy | Maintenance therapy (when the sign of dehydration gone) | |
|---|---|---|
| Mild diarrhea: Not more than one stool for every 2 hours or longer, or less than 5 stools /kg/hour | Severe diarrhea: More than one stool every 2 hours, or more than 5 ml of stool /kg/hour |
100 ml/kg body weight per day until diarrhea stops | Replace stool losses volume, for volume if not measurable give 10–15 ml/kg body weight/hour | |
Reduced osmolarity ORS | gm/lit | Reduced osmolarity ORS | mmol/lit |
|---|---|---|---|
Sodium chloride | 2.6 | Sodium | 75 |
Anhydrous Glucose | 13.5 | Anhydrous Glucose | 75 |
Potassium chloride | 1.5 | Chloride | 65 |
Trisodium citrate dehydrate | 2.9 | Citrate | 10 |
Total weight | 20.5 | Potassium | 20 |
Total osmolarity | 245 |
Ref: Park, 22/e p203-5
150. All of the following are causes of neonatal thrombocytopenia except:
- Alloimmune thrombocytopenia
- Autoimmune thrombocytopenia
- Maternal hypothyroidism
Ans. d. Maternal hypothyroidism
Explanation
Neonatal thrombocytopenia rarely a indactive of a primary disorder of megakaryopoisis
It may occurs in association with congenital viral infection, specially rubella, cytomegalovirus, protozoal infection, such as toxoplasma, syphilis, and perinatal bacterial infection specially caused by gram negative bacilli. DIC, Neonatal alloimmune thrombocytopenia, children born to mother with ITP, congenital like amegakaryocutic thrombocytopenia and TAR (thrombocytopenia, radial anomalies, limb shortening) syndrome
Ref: Nelson, 19/e p1720



