INTRODUCTION
Hysteroscopy is a procedure that involves direct visualization of cervical canal and uterine cavity. Office hysteroscopy allows minor pathologies to be treated in an outpatient setting. Surgical hysteroscopic procedures, or in other words, major hysteroscopic surgery, is performed in the operating room.
Instruments used are (Fig. 1):
- Distending media
- Light source
- Camera
- Telescope
- Diagnostic and operative sheaths
- Accessory instruments.
Fig. 1: Fully equipped mobile cart for both diagnostic and surgical hysteroscopy as well as laparoscopy.
MEDIA FOR DISTENDING THE UTERINE CAVITY
All hysteroscopic procedures require adequate distension of the uterine cavity.
Due to office hysteroscopy and the bipolar resectoscope, it is possible to use physiological saline solution as the unique method of distension. Current is strictly limited to the resectoscope's two poles without flowing through the patient's body for high-frequency bipolar intrauterine electrosurgery, hence it is possible to use physiological saline as distension media.1
Types
- Gaseous—carbon dioxide (CO2)
- Liquid
- High viscosity—Hyskon
- Low viscosity
- Ionic: NS, RL, 5% D, 10% D, 4% and 6% dextran solution
- Nonionic: 1.5% glycine, 35 sorbitol, 5% mannitol
- Combination of 2.8% sorbitol and 0.5% mannitol.
CO2 as Distending Media
- Used in office hysteroscopy
- Rate of flow: 30–40 mL/min (should be less than 100 mL/min)
- Intrauterine pressure 60–70 mm Hg.
Advantages
- Provides clean media
- Allows entry evaluation of endocervical canal.
Disadvantages
- Does not flush cavity of debris
- Flattens endometrium
- Emboli can form causing gas embolism and death.2
Low Viscosity Distending Media
- Delivered fluid must be circulated out and clear fluid added in order to maintain view and distension of cavity
- Delivery Systems used are:
- Gravity fall system
- Pressure cuff
- Electronic suction irrigation pump.
- Proper monitoring of infused volume is important and infusion is stopped when positive.
- Infusion difference is
- 500 cc for hypo-osmolar solution
Normal Saline
- 0.9% NS is commonly used.
Advantages: Easily available, low operative cost and physiological disposal by peritoneal absorption.
Disadvantages: Efficient conductor of electrons so electrosurgery with monopolar devices is not possible. Not suitable for office hysteroscopy. Fluid overload and pulmonary edema risk.2
Glycine (1.5%) and Sorbitol (3%)
Advantages
Inexpensive, easily available, media of choice for monopolar cautery.
Disadvantages
- Hypoosmolar solution causing dilutional hyponatremia and hypervolemia.
- Interferes with oxygenation and coagulation.3
Mannitol (5%) and Glycine (2.2%)
- Isosmolar
- Can be used with electrosurgical instruments
- Decreased risk of fluid overload and hyponatremia.
High Viscosity Media––Hyskon
- It is a 32% high molecular weight dextran solution
- Colorless viscid medium
- Volume required: Diagnostic—100 mL, operative—200–500 mL, upper safe limit—500 mL
- One mL of Hyskon withdraws 20 mL of water in circulation.
Advantages
- Being highly viscous small quantities required for examination
- Provides excellent visualization due to high refractive index.
Disadvantages
- Expensive mechanical pump necessary to deliver these fluids
- Pulmonary edema, coagulopathies, electrolyte imbalance, anaphylactic reaction.3
LIGHT SOURCE
Quality depends upon:
- Wattage
- Remote light generator
Wattage
- 175 W for routine procedures
- 300 W for special interventions.
Light Generator
- Tungsten orange yellow light
- Metal halide bluish coloration
- Xenon white light
- LED source.4
IMAGING SYSTEMS
The use of an endocamera is essential in modern hysteroscopy. Different types of video cameras are available; their quality depends on the following technical parameters: resolution (given by number of lines or pixels), and sensitivity (Lux), as well as the quality of the reproduction or video images. A high signal-to-noise ratio indicates that variations in image quality under extreme situations, e.g. hemorrhages or other reasons for loss of light intensity are reduced to a minimum. Modern high definition (HD) cameras offer a very high resolution and almost natural color reproduction.
TELESCOPE
It has three parts:
- Eyepiece
- Barrel
- Objective lens.
Available in various diameters:
- 4 mm (standard)––gives high quality, sharpest image
- 3 mm—inferior to 4 mm, but gives satisfactory image quality.
Types
- Straight on, i.e. 0°––distant panoramic view
DIAGNOSTIC SHEATHS
- Usually 4–5 mm
- Required to deliver the distending media into the uterine cavity. Telescope fits into the sheath and there is 1 mm gap left between the sheath and scope through which distending media is transmitted and is controlled by external stopcock. The endoscopes used in this field of application are available in different outer diameters. Miniature endoscopes should be used in diagnostic hysteroscopy in order to render the procedure minimally invasive. Microhysteroscopy is usually performed with a 2 mm telescope, which involves considerable limitations due to fragility of scope. It should be reserved for special cases of cervical stenosis. The hysteroscope with a diameter of 2.9 mm is most widely used in office setting, including purely diagnostic hysteroscopy, using physiological saline as distension media.1,5
OPERATIVE HYSTEROSCOPES
It has channels for:
- 3–4 mm telescope
- Instillation of medium
Types
- Standard operating sheath:
- Single cavity for medium, telescope and operating tools.
- Disadvantage of not being able to flush the cavity with distending medium and operating tool manipulation within the cavity is difficult.
- Isolated multiple channel operating sheath:
- Double flushing sheath that allows media instillation by inner sheath and return by perforated outer sheath, constant flow of medium leads to very clear operative field.
Operative hysteroscopes have been definitively superseded by office hysteroscopy systems that allow for diagnostic hysteroscopy while providing the option to perform minor surgical procedures in an office setting (small endometrial polyps or pedunculated uterine leiomyomas).
For this purpose, the inner diameter of the sheath used in conjunction with an office hysteroscope must be large enough to permit the passage of operating instruments. Indeed, even if the same telescope is used as in diagnostic hysteroscopy (2.9 mm diameter), the sheath must have an outer diameter ranging between 3.2 mm and 5.3 mm to permit the passage of surgical instruments and to provide adequate uterine distension by use of liquid media. In this field of application, most operating instruments have a semi-rigid design and a diameter of 1.67 mm (5 Fr): scissors, biopsy forceps, and various types of probes, electrodes for unipolar and bipolar coagulation, and Essure microinsert for hysteroscopic sterilization by tubal occlusion in a clinical setting.1,68
RESECTOSCOPES
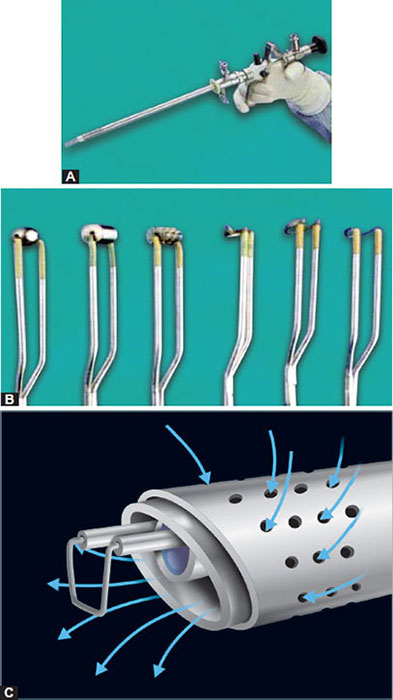
Electrosurgical Endoscope (Fig. 5)
- Consists of:
- Inner sheath has a common channel for telescope, distending media and electrode.
- Outer sheath––for the return of distending media.
- Lens is angled towards the electrode for clear view.
- Electrode can be ball, barrel, knife, or cutting loop type.
Figs. 5A to C: (A) Resectoscope, (B) Accessories with resectoscope, (C) Distension medium flow through resectoscope.
9Resectoscope is specially designed for the resection and removal of abnormal intrauterine tissue as well as endometrial ablation and septal dissection. There are essentially two types of resectoscopes, which differ in outer diameter: (1) 7.3 mm (22 Fr); (2) 8.7 mm (26 Fr). The 8.7 mm-resectoscope is commonly used only in patients with a large uterus (endometrial ablation) or in the presence of pathologies (myoma) with a diameter larger than 3 cm, or if a myoma is found to have a difficult intramural location. In cases which require dilation of the cervical canal (Hegar no. 8), the 22-Fr resectoscope is usually preferred. The resectoscope consists of a classic endoscope, with diameters ranging between 2.9 mm and 4 mm, preferably with a 12° viewing angle to keep the electrode within the field of view, combined with a cutting loop operated by a passive spring mechanism, and two sheaths for continuous irrigation and suction of the distension medium. Apart from the cutting loop, other instruments such as micro knives and a variety of vaporizing or coagulating electrodes can be used with the working element of the resectoscope. All these instruments are available for both the 22-Fr and the 26-Fr resectoscope. The same resectoscope can be used both as unipolar and bipolar instrument, simply by changing the working element and the electrodes. For distension and irrigation of the uterine cavity, a 1.5% glycine solution or sorbitol mannitol is used, as previously stated, for unipolar surgery. For bipolar resectoscopy, physiological saline solution must be used as distension medium.1,5
Surgical instruments are available in both rigid and flexible forms to be inserted through the operating channels of the scopes. Examples of surgical instruments and their uses are listed below (Figs. 6 and 7):
- Scissors: To incise a septum, excise a polyp, or lyse synechiae
- Biopsy forceps: To perform directed biopsy for pathologic review
- Grasping instruments: To remove foreign bodies
- Roller ball, barrel, or ellipsoid: To perform endometrial ablation and/or desiccation (This instrument is used with a resectoscope)
- Loop electrode: To resect a fibroid or polyp or endometrium (This instrument is used with a resectoscope)
- Scalpel: To cut or coagulate tissue, with high power density at its tip (This instrument is used with a resectoscope)
- Vaporizing electrodes: To destroy endometrial polyps, fibroids, intrauterine adhesions, and septa; also used for endometrial ablation (This instrument is used with a resectoscope)
- Morcellator: To cut and remove endometrial polyps or fibroids.4
Improvements in hysteroscope design have improved the effectiveness of the inflow-outflow channels and of specific operating instruments. For example, the Chip E-Vac System (Richard Wolf Medical Instruments Corporation, Vernon Hill, IL) incorporates a suction channel and a pump to aid in removing chips of tissue during resection. This feature improves visibility and may decrease time otherwise spent emptying the pieces from the endometrial cavity.10
Fig. 6: Instruments that can be inserted through the office hysteroscope: forceps, scissors, unipolar and bipolar electrodes.
Another instrument in the forefront is a hysteroscopic morcellator (Smith & Nephew, Inc., Andover, Mass), which may reduce myomectomy and polypectomy time by morcellating and removing tissue in one movement under direct visualization. It requires cervical dilation to 9 mm. A new hysteroscopic morcellating system called MyoSure (Interlace Medical, Inc., Framingham, Mass) is reported to work just as well, removing submucosal fibroids up to 3 cm in diameter, with a unit that only requires cervical dilation to 6 mm. This smaller diameter suggests it may be used in an office setting.4
ELECTROSURGICAL UNIT FOR HIGH-FREQUENCY SURGERY
The resectoscope is connected to a high-frequency electrosurgical unit with automatic power supply control and alarm function. Modern high-frequency systems can be operated both in unipolar and bipolar mode, for hysteroscopy as 11well as for laparoscopy and open surgery. Resectoscopy can be performed with unipolar or bipolar current depending on the available system. In the unipolar system, the electrons flow from the high-frequency electrosurgical unit to the active electrode (e.g. cutting loop or knife electrode) before passing through the tissue to the neutral electrode and then returning to the electrosurgical unit. In the bipolar system, the high-frequency generator produces an initial peak of around 400 RMSV (root mean square voltage) which creates an electrical arc between the two bipolar electrodes. Once the electrode is sufficiently close to the tissue, the electrical arc converts the conductive solution of sodium chloride to a plasma containing sodium particles that are active because they are highly charged with energy. Once this plasma effect has been created, it can be maintained with a lower voltage (100–350 RMSV). Contact with the activated sodium ions (and thus not with the electrode) provokes disintegration of the tissue due to breaking of the carbon-carbon and carbon-hydrogen bonds and dissociation of the water molecules to H+ and hydroxide ion (OH-) ions. The result is collapse of the cellular membranes with ensuing cutting of the tissue.
The temperature of the surrounding tissues remains between 40° and 70° using the bipolar system but reaches 400° when the unipolar system is used resulting in deep surrounding tissue changes.1,7 Electrosurgery can be used for coagulation, dissection and also for combination of both modes using nonmodulated (soft coagulation) and modulated flow (spray coagulation). The coagulation current is characterized by intermittent phases of electrical activity which cause dehydration of the cells and coagulation of the proteins with successive hemostasis. The nonmodulated cutting current is a continuous flow of electrons which produces a rapid increase of temperature inside the cells causing them to explode. Use of nonmodulated current is recommended for coagulation as lower voltages current is used. It is a less risky option and as efficacious as the modulated coagulation current6 (Fig. 8).
HYSTEROSCOPIC LASER SURGERY
Argon, neodymium, YAG and KTP lasers are the most frequently used lasers in hysteroscopy and have good characteristics in terms of coagulation, although they do have some weak points in terms of vaporization. Laser generators are significantly more expensive than electrosurgical equipment and do not offer particular advantages in clinical practice.1
MAINTENANCE AND STERILIZATION OF INSTRUMENTS
Autoclave sterilization is the cheapest system, and owing to the diffusion of steam, it cleans even the smallest gaps and openings. Only the optical systems and instruments which are specifically certified for the autoclave may be sterilized with a 20-minute cycle at 121°C or 7 minutes at 134°C.
Gas sterilization with ethylene oxide is an ideal system since it is performed at low temperatures obviating the risk of damaging the endoscopic instruments.8
REFERENCES
- Mencaglia L, De Albuquerque Neto LC, Alfonso Arias Alvarez R. Manual of Hysteroscopy: Diagnostic, Operative and Office Hysteroscopy. Tuttlingen: End Press; 2014.
- Litta P, Bonora M, Pozzan C, et al. Carbon dioxide versus normal saline in outpatient hysteroscopy. Hum Reprod. 2003;18(11):2446–9.
- Valle RF, Sciarra JJ. Current status of hysteroscopy in gynaecological practice. Fertil Steril. 1979;32:619–32.
- Petrozza JC, Attaman JA. Hysteroscopy. Drug Dis Obs Gyn. 2015.
- Bettocchi S1, Nappi L, Ceci O, et al. What does diagnostic hysteroscopy mean today? The role of the new techniques. Curr Opin Obstet Gynecol. 2003;15(4):303–8.
- Di Spiezio Sardo A, Taylor A, Tsirkas P, et al. Hysteroscopy: a technique for all? Analysis of 5,000 outpatient hysteroscopies. 2008;89:438–43.
- Ozturk E1, Ugur MG, Balat O, et al. An analysis of hysteroscopy experience over a seven year period. Clin Exp Obstet Gynecol. 2010;37(2):150–1.
- Block SS. Disinfection, Sterilization, and Preservation in Hospitals, 5th edition. Philadelphia: Lippincott Williams & Wilkins; 2001.