LONG ESSAYS
Question 1
Define gingiva. Enumerate the zones of oral mucosa. What are the different parts of gingiva? Explain in detail about the microscopic features of gingiva.
Answer
According to Glickman, gingiva is defined as “that part of oral mucosa that covers the alveolar processes of the jaws and surrounds the necks of the teeth in a collar-like fashion.”
There are Three Zones of Oral Mucosa
- Masticatory mucosa, e.g. Gingiva and covering of the hard palate.
- Specialised mucosa, e.g. dorsum of the tongue.
- Lining mucosa, e.g. oral mucous membrane lining the remainder of the oral cavity.
Gingiva is divided into three parts viz. marginal, attached and interdental (Fig. 1.1).
- Marginal gingiva
- It is also called as unattached gingiva, which is loosely bound and surrounds the teeth in a collar like manner.
- It is differentiated from the attached gingiva by a mild/small (shallow) depression, which is called as free gingival groove.
- Gingival sulcus: It is a V-shaped crevice around the tooth which is bounded by marginal gingiva on one side and tooth on the other side.
- Normal depth of gingival sulcus is 1.3 mm. In pristine condition the depth of sulcus is 0 mm.
- Gingival crevicular, fluid (GCF) is found in the gingival sulcus.
- Attached gingiva
- It begins after marginal gingiva and is tightly bound to the underlying periosteum of the alveolar bone (Fig. 1.2).
- Attached gingiva is separated from the loosely bound alveolar mucosa by mucogingival junction.
- It is maximum in the incisal region approx. 3.5–4.5 mm (maxilla) and 3.3–3.9 mm (mandible) and minimum is the posterior region i.e. 1.9 mm (maxilla) and 1.8 mm (mandible).
- Interdental gingiva
- It is found between the adjacent teeth, occupying the gingival embrasure.
- Underneath the facial and the lingual papillae, there is a valley like depression known as Col.
Microscopic Features of Gingiva
Gingiva is microscopically divided into two parts, viz., gingival epithelium and gingival connective tissue.
Gingival Epithelium
- The epithelium not only provides a physical barrier to various infections but also plays an important role in host defence mechanisms
- Gingival epithelium protects the deep structures which are achieved by proliferation and differentiation of keratinocytes
- Proliferation occurs by mitosis in basal cell layer
- Few cells remain in the basal cell layer to act as proliferative compartment while majority of the cells move towards the surface
- Differentiation occurs during this movement of the cells to the surface, they undergo biochemical and morphologic changes, thus differentiating into keratinocytes. This process is called as keratinisation
- Keratinocytes form the bulk of the gingival epithelium.
- Other cells like Langerhans cells, Merkel cells and melanocytes are seen in small numbers. These cells are together called as non-keratinocytes
- Melanocytes: These are specialised cells which synthesize melanin and cause melanin pigmentation which is occasionally seen on the gingiva
- ➤ They are derived from neural crest cells and are located in stratum basale
- ➤ Melanin is produced as melanosomes which is present in the cytoplasm of melanocytes and keratinocytes.
- Langerhans cells: They are dendritic cells seen in suprabasal region. They play a role in immune reaction as they act as antigen presenting cells for lymphocytes. They also have G-specific granules known as Birbeck's granules
- Merkel cells: These are present in deeper layers containing nerve endings and therefore have a sensory function.
- The epithelium is connected to the underlying connective tissue by a basal lamina which is approximately 300–400 Å thick
- It consists of lamina densa and lamina lucida. Hemidesmosomes are attached to the lamina lucida composed mainly of glycoprotein laminin. Type IV collagen forms the bulk of lamina densa.
Gingival epithelium is of three types:
- Oral epithelium.
- Sulcular epithelium.
- Junctional epithelium.
Oral Epithelium
- It is also known as the outer epithelium that covers the outer surface of the keratinised gingiva, i.e. the marginal gingiva and attached gingiva
- It is composed of four layers viz., stratum basale, stratum spinosum, stratum granulosum and stratum corneum
- Keratinisation varies in different areas of the oral cavity, i.e. it is maximum in the palate, gingiva, ventral aspect of tongue, cheeks in the descending order
- The outer epithelium loses its keratinisation if it contacts a tooth.
Sulcular Epithelium
- It is a non-keratinised stratified squamous epithelium that lines the gingival sulcus
- It extends from the crest of the gingival margin till the coronal portion of the junctional epithelium. It lacks stratum granulosum and corneum
- It has the capacity to keratinise in certain conditions like:
- Upon exposure to oral cavity
- Upon complete elimination of inherent bacterial flora.
Junctional Epithelium
- It is also referred to as attachment epithelium which is stratified, squamous and non-keratinising in nature. 5It is found at cemento-enamel junction in healthy conditions. The width of JE is 10– 29 cells coronally and 1– 2 cells apically. The length of the junctional epithelium is approximately 0.25–1.35 mm
- It is formed by confluence of outer epithelium and reduced enamel epithelium during tooth eruption
- Junctional epithelium exhibits ribosomes, Golgi bodies and cytoplasmic vacuoles. The junctional epithelium is attached to the tooth by internal basal lamina and to the connective tissue by external basal lamina
- The epithelial attachment of junctional epithelium consists of internal basal lamina which consists of lamina densa that is adjacent to the enamel and lamina lucida to which hemidesmosomes are attached
- Hemidesmosomes help in cell-to-cell attachment and also take part in gene expression regulation, cell proliferation and cell differentiation
- The junctional epithelium and the gingival fibres together are referred as dentogingival unit because the attachment of the junctional epithelium to the tooth is reinforced by the gingival fibres.
Thus it could be concluded that junctional epithelium has various functions such as:
- JE forms an epithelial barrier against plaque bacteria as it is firmly attached to the tooth surface
- It also acts as a semipermeable membrane as it allows access of gingival fluid, inflammatory cells and immunologic components of host defence mechanism to the gingival sulcus
- It helps in rapid repair of the damaged tissue as cells of junctional epithelium exhibit rapid turnover.
Gingival Connective Tissue
It is also referred as lamina propria and it consist of two layers:
- Papillary layer adjacent to epithelium.
- Reticular layer adjacent to the periosteum of the alveolar bone.
- Connective tissue is mainly composed of collagen fibres which are about 60% by volume, fibroblasts (5%), and remaining 35% is formed by vessels, nerves and matrix
- It also consists of a ground substance which occupies the space between fibres and cells along with high water content. Ground substance is mainly composed of proteoglycans like hyaluronic acid, chondroitin sulphate and glycoproteins, mainly fibronectin
- Connective tissue consists of three types of fibres, i.e. collagen, reticular and elastic. Type I collagen is the main fibre seen in lamina propria and provides tensile strength. Elastic fibre is composed of elaunin, elastin and oxytalan fibres distributed among collagen fibres.
SHORT ESSAYS
Question 1
What is attachment epithelium? What is epithelial attachment?
Answer
Junctional epithelium is also referred to as attachement epithelium which is stratified, squamous and non keratinizing in nature. It is found at cemento–enamel junction in healthy conditions.
- Its width is 10–29 cells coronally and 1–2 cells apically.
- The length of the junctional epithelium is approxiametely 0.25 – 1.35 mm
- It is formed by confluence of outer epithelium and reduced enamel epithelium during tooth eruption
- It can be completely formed after surgery or instrumentation
- Junctional epithelium exhibits ribosomes, golgi bodies and cytoplasmic vacuoles. Lysosome- like bodies are seen in this epithelium. There is absence of keratinosomes which is also referred as Odland bodies and also acid phosphatase is related to lower degree of differentiation, which reflects weak defence mechanism against bacteria in d dental plaque
- Poly morphonuclear leucocytes (PMN) are commonly found, but its number increases considerably at the time of bacterial attack to fight against infection (Fig. 1.4).
Epithelial Attachment
- The junctional epithelium is attached to the tooth by internal basal lamina and to the connective tissue by external basal lamina
- The epithelial attachment of junctional epithelium consists of internal basal lamina which consists of lamina densa which is adjacent to the enamel and lamina lucida to which hemidesmosomes are attached
- Hemidesmosomes help in cell-to-cell attachment and also take part in gene expression regulation, cell proliferation and cell differentiation
- The junctional epithelium and the gingival fibres together are referred as dentogingival unit because the attachment of the junctional epithelium to the tooth is reinforced by the gingival fibres
- Thus it could be concluded that junctional epithelium has various functions like:
- It forms an epithelial barrier against plaque bacteria as junctional epithelium is firmly attached to the tooth surface
- It acts as a semipermeable membrane as it allows access of gingival fluid, inflammatory cells and immunologic components of host defence mechanism to the gingival sulcus
- It helps in rapid repair of the damaged tissue as cells of junctional epithelium exhibit rapid turnover.
Question 2
Describe in detail about gingival connective tissue.
Answer
Gingival Connective Tissue
It is also referred as lamina propria and it consists of two layers:
- Papillary layer adjacent to epithelium.
- Reticular layer adjacent to the periosteum of the alveolar bone.
- Connective tissue is mainly composed of collagen fibres which are about 60% by volume, fibroblasts (5%), and remaining 35% is formed by vessels, nerves and matrix
- It also consists of a ground substance which occupies the space between fibres and cells and has a high-water content
- Ground substance is mainly composed of proteoglycans like hyaluronic acid and chondroitin sulphate and glycoproteins, mainly fibronectin
- Connective tissue consists of three types of fibres, i.e. collagen, reticular and elastic
- Type I collagen is the main fibre seen in lamina propria and provides tensile strength
- Elastic fibre is composed of elaunin, elastin and oxytalan fibres distributed among collagen fibres
- Connective tissue is highly collagenous, containing bundles of fibres known as gingival fibres consisting of collagen type I. They serve the following functions:
- It holds the marginal gingiva tightly against the tooth
- Provides strength to withstand the masticatory forces
- Unites the marginal gingiva with the cementum and attached gingiva of the adjacent tooth.
- Group of principal gingival fibres are:
- Dentogingival group
- Alveologingival group
- Dentoperiosteal group
- Circular group
- Transseptal group.
- Group of secondary fibres are:
- Periosteogingival group
- Inter-papillary group
- Trans-gingival group
- Inter-circular group
- Inter-gingival group
- Semi-circular group.
Cellular Composition of Gingival Connective Tissue
- Fibroblast is the main cell type of gingival connective tissue. Fibroblasts are responsible for synthesising collagen, elastic fibres, glycoproteins and glycosaminoglycans. They also play an important role in development, maintenance and repair
- Mast cells, fixed macrophage and histiocytes are present in gingival connective tissue
- Also seen are adipose cells and eosinophils, which are less in number. Leucocytes and lymphocytes are also seen.
Question 3
Explain in detail about gingival sulcus.
Answer
Gingival sulcus is also referred to as gingival crevice.
- It is a V-shaped shallow crevice around the tooth which is surrounded by gingiva on one side and tooth on another side
- Normal depth of gingival sulcus is 1–3 mm. In pristine condition the depth of sulcus is 0 mm
Development of Gingival Sulcus
- When the tooth erupts into the oral mucosa, the reduced enamel epithelium combines with the oral epithelium forming, the junctional epithelium (Fig. 1.4)
- Further this united epithelium becomes condensed along the crown and ameloblasts gradually transform into squamous epithelial cells
- This transformation moves in an apical direction. This epithelium continuously renews itself by mitotic activity and moves in a coronal direction to the gingival sulcus, where they are shedded
- Gingival sulcus formation takes place when the tooth erupts into the oral cavity (Fig. 1.5).
Gingival Crevicular Fluid
- Gingival crevicular fluid can be a transudate or an exudate which contains a wide range of biochemical factors which can be used as a potential diagnostic biomarker of the biologic state of the periodontium in health and disease
- Gingival crevicular fluid is mainly composed of epithelium, connective tissue, serum, inflammatory cells and microbial flora
- In the state of health GCF is present in small quantities whereas in inflammation, GCF increases and resembles an inflammatory exudate.
- Functions of GCF are as follows:
- It has a cleansing action.
- It provides adhesion of the gingival epithelium to the tooth as it contains plasma proteins.
- It has anti-microbial action.
- It acts as gingival defence mechanism as it possesses antibody activity.
- Various methods of collecting GCF:
- Filter paper strips.
- Micro-capillary tubes.
- Crevicular washing methods.
- Twisted threads.
- GCF samples can be measured on a blotter or a perio paper on an electronic transducer called as periotron.
- Ninhydrin staining method.
- Isotope dilution method.
Dento-gingival Junction
- Attachment of junctional epithelium to the tooth is reinforced by gingival fibre, therefore junctional epithelium and gingival fibres together is referred to as dento-gingival unit.
- The gingival fibres are highly collagenous consisting of collagen fibres mainly Type I collagen. Principal fibres of gingival connective tissue are:
- Dento-gingival group
- Alveolo-gingival group
- Dento-periosteal group
- Circular group
- Transseptal group.
- Group of secondary fibres are:
- Periosteoa-gingival group
- Inter-papillary group
- Trans-gingival group
- Inter-circular group
- Inter-gingival group
- Semi-circular group.
- These fibres originate from cementum and are inserted into connective tissue of gingiva and periosteum of the alveolar bone.
- They provide stabilization and maintain the position of teeth in the arch by securing them.
Question 4
Correlate various clinical and microscopic features of gingiva.
Answer
Various clinical features of gingiva are:
- Colour
- Size
- Contour
- Shape
- Consistency
- Surface texture
- Colour: Normal colour of gingiva is pink. There are three factors on which the colour of gingiva is dependent, i.e. vascularity, degree of keratinisation, and pigment containing cells.
- Vascularity: If the vascularity increases, the colour of gingiva becomes red. It is seen in cases of inflammation, but in absence of inflammation the vascularity is normal, and the colour of gingiva appears as coral pink.
- Degree of keratinisation: More the keratinisation lesser would be the redness in gingiva. Therefore a highly keratinized gingiva would appear as pale pink, whereas if the keratinisation is low, gingiva would appear as reddish. Since the attached gingiva and marginal gingiva are keratinised, it appears as pink, whereas alveolar mucosa which is non-keratinised, appears red, smooth and shiny.
- Pigmentation containing cells: Melanin is a brown coloured pigment which is responsible for normal pigmentation. But if these pigment containing cells increase in number, then the gingiva appears brownish-black in colour (Fig. 1.6).
- Size: Size of gingiva depends upon the total amount of cellular and intercellular content of gingiva. In cases of gingival inflammation, size is enlarged, otherwise in normal conditions it is not enlarged.
- Contour: Contour of gingiva is dependent on various factors like alignment of teeth in the arch, shape of the teeth, location, size of the proximal contact and size of the gingival embrasure. In normal conditions the gingiva follows a scalloped contour, but in cases of inflammation, mostly it becomes a scalloped. In relatively flat teeth, the gingival contour is flat. If there is pronounced mesio-distal convexity or if there is gingival recession, the scalloping along the teeth becomes more accentuated.
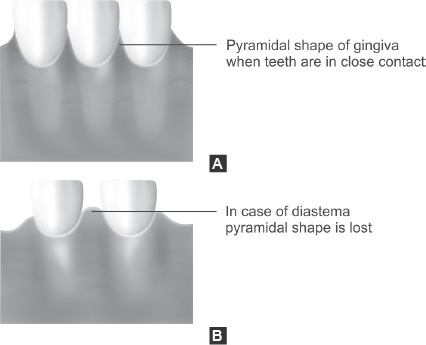
- Shape: Shape of the gingiva depends upon the proximal teeth contacts and shape of teeth. If the teeth are in tight contact and teeth are narrow mesio-distally, gingiva exhibits a pyramidal shape, e.g. in case of anterior teeth, but if the teeth are not in close contact the shape of the interdental gingiva becomes flattened. If the teeth are wide mesio-distally, that means if the teeth are broad, e.g. in posterior region, then the interdental gingiva exhibits a broader shape.
- Consistency: In normal conditions, gingiva is firm and resilient, but in cases of inflammation it becomes soft and oedematous.
- Surface texture: In health, gingiva exhibits an orange peel-like appearance referred to as stippling. Stippling is an adaptive specialisation or reinforcement of function produced by alternate rounded depressions and protuberances in gingiva. In this state of disease stippling becomes absent.
- Position: The normal position of gingiva is at cementoenamel junction (CEJ). In disease, this position is either above CEJ or below the level of CEJ which is also referred to as gingival recession.
SHORT NOTES
Question 1
What is continuous tooth eruption?
Answer
There are two types of eruption viz., active and passive eruption.
- Active eruption is referred as the eruption of the teeth in an occlusal direction.
- Passive eruption is exposure of the crown by the apical migration of the gingiva. It can be divided into four stages:
- Stage 1: In this the teeth are in the line of occlusion. The junctional epithelium and the base of the gingival sulcus are at the enamel.
- Stage 2: In this stage there is an apical proliferation of the junctional epithelium such that one part is on cementum while other part is on enamel. Whereas, the base of the gingival sulcus is still on the enamel.
- Stage 3: In this the junctional epithelium completely rests on the cementum and the base of the sulcus is at cemento-enamel junction.
- Stage 4: Both junctional epithelium and the base of the gingival sulcus are present on the cementum such that some part of the cementum is exposed (Fig. 1.7).
Question 2
Define is gingival col and what is its significance?
Answer
It is a valley like depression connecting the facial and lingual papillae and conforms to the shape of the interproximal contact. The interproximal space consists of interdental gingiva that occupies the gingival embrasure.
Significance of col: Since col is formed of non-keratinised epithelium, it is very prone to infections and inflammation and is the most prone site for disease initiation.
Question 3
What is attached gingiva? How is it measured? What is its significance?
Answer
It is that part of the gingiva that starts immediately after marginal gingiva and extends till mucogingival junction. It is separated from the marginal gingiva by a very shallow groove known as marginal groove and it is separated from adjacent loose alveolar mucosa by mucogingival junction.
It can be measured using a periodontal probe by subtracting the sulcular depth from the total distance between the marginal gingiva and the mucogingival junction.
It can also be measured using Schiller's potassium iodide solution which stains the keratinised gingiva.
Significance of attached gingiva are as follows:
- It helps in protection against microbes and other foreign bodies as it is tightly bound to the periosteum
- Since it is keratinised, it aids in bearing the masticatory forces
- It helps in proper placement of the toothbrush head
- It also enhances the aesthetics.
Question 4
Discuss the blood supply, lympatics and nerve supply of gingiva?
Answer
Blood Supply
- Supraperiosteal arterioles present along the surface of the alveolar bone that also pass through surrounding tissue.
- Periodontal ligament vessels, which extend into the gingiva and anastomose with the capillaries in the sulcular area.
- Arteries that emerge from the interdental septa and are extended parallel to the crest of the bone to anastomose with the vessels of the periodontal ligament.
Lymphatic Drainage
Gingiva brings in the lymphatic vessels of connective tissue papillae. It progresses to the periosteum of the alveolar process and then to the regional lymph nodes, mainly submaxillary group.
Nerve Supply
Neural system of gingiva is very extensive and is distributed throughout the gingiva. Neural innervation is derived from the nerves in the periodontal ligament and from the labial, buccal and palatal nerves. Nerve structures which are present in the connective tissue are:
- Meshwork of terminal argyrophilic fibres
- Meissner-type tactile corpuscles
- Temperature receptors, i.e. Krause type end bulbs
- Encapsulated spindles.
Question 5
What are clear cells?
Answer
Non-keratinocytes (melanocytes, Langerhans cells and Merkel cells) are referred to as clear cell because in the histologic section, the zone around their nuclei appears lighter than in the zone around the keratin producing cells.
Question 6
What is the difference between keratinised gingiva and attached gingiva?
Answer
Keratinised gingiva consists of both loose marginal gingiva and firmly adherent attached gingiva but, attached gingiva does not contain any movable mucosa.
Question 7
What are Stillman's cleft?
Answer
According to Carranza, they are defined as apostrophe-shape indentations extending from and into gingival margin of varying distances on facial surface. They are narrow V-shaped gingival recessions.
Quesiton 8
What are McCall's festoons?
Answer
These are rolled thickened margins of gingiva seen near the canines when recession reaches upto the mucogingival junction. These are also called as life preserver-shaped enlargement. They represent the inflammatory changes seen in the gingiva.
Question 9
What is mucogingival junction?
Answer
It is a junction which demarcates the firm attached gingiva from the loosely bound alveolar mucosa. Its position remains consistent throughout life.