INTRODUCTION
Capnography is the measurement of the partial pressure of exhaled carbon dioxide (CO2) and display of CO2 waveform. The graphic representation is expressed as expired CO2 concentration over time, or volume and is known as time, or volume capnogram. Capnography became a standard of monitoring during anesthesia practice in Europe in the late 1970s and the United States in mid-1980s. Since then, it has evolved as an essential component of standard anesthesia monitoring armamentarium.1 Capnography has also expanded beyond the operating room into the emergency department, radiology, gastroenterology procedures, adult, and pediatric sedation sites. Furthermore, capnography has also made its impact in intensive care units (ICUs) across the world for monitoring ventilation and assuring correct location of endotracheal tube (ETT) continuously. Capnometry is a numeric measurement and display of the level of CO2 concentration without waveform. The waveform of capnography is more valuable and reliable than capnometry for clinical interpretation.2,3
PHYSICS
There are two types of capnography devices (Figs. 1, 2 and Table 1): (1)“sidestream” and (2) “mainstream”4 depending upon where the CO2 analyzer is located in relation to the ventilator circuit. In a “mainstream” analyzer, sampling window is in the ventilator circuit (near the hub of ETT) and measures CO2, while in a “sidestream”, the gas is located out of the ventilator circuit and gas sample is aspirated via 6 feet sampling tube. In both types, the gas analyzers work mostly using the principle of infra-red (IR) absorption spectroscopy (Fig. 3). An IR diode emits the light that traverses the chamber containing airway sample. The CO2 molecules absorb IR light and unabsorbed IR light is detected by an IR detector. Molecules of CO2 absorb IR radiation at a very specific wavelength (4.26 μm), with the amount of radiation absorbed having a nearly exponential relation to the CO2 concentration (Beer-Lambert Law) present in the breath sample. The difference between the source light and absorbed light is transformed into CO2 concentration and displayed as a capnography waveform.2
Fig. 2: Sidestream capnography: Infra-red (IR) light sensor is positioned outside the airway circuit. A T-piece adapter with a 6 feet disposable tubing is inserted between the breathing tube and airway circuit. (ET: endotracheal tube)
Water vapor, nitrous oxide, and anesthetic agents absorb IR light, but at a different wavelength. There are other techniques of measuring CO2 using photoacoustic spectroscopy, Raman scattering, and mass spectrometry, which are not commonly used.
In the majority of capnographs, the exhaled concentration is plotted against the time (time capnography) and is the common method in practice. In volume capnography, the exhaled CO2 is serially plotted against expired lung volume. Volume capnography is not routinely used. However, this may be a preferred technique in near future, as it enables indirect estimation of physiological dead space.53
COLORIMETRIC DEVICE
The colorimetric CO2 detector (Figs. 4A and B) can be used for verification of correct placement of an ETT in the trachea. It has especially treated litmus paper, which changes color from purple to yellow. The device is not very accurate, particularly when CO2 output is low during CPR. 4Waveform capnography is the preferred approach currently. Nonetheless, the colorimetric device is a reasonable option to check placement of an ETT for emergency intubations.
Figs. 4A and B: Calorimetric capnometer. The pH sensitive paper changes from purple to yellow when CO2 is detected.
PHYSIOLOGICAL OVERVIEW
A good understanding of time capnogram (Fig. 5) and volume capnogram (Fig. 6) will help clinicians to avail of full benefit of capnography in clinical practice.
Time Capnography
Time capnogram (Fig. 5) is usually interpreted as two segments—(1) an inspiratory segment and (2) an expiratory segment, and two angles— alpha and beta.6 Capnograms may be evaluated breath by breath, or trends may be assessed as valuable clues to a patient's physiologic status. Expiratory segment is divided into three phases, I to III. Inspiratory segment is designated as phase 0 (Table 2).
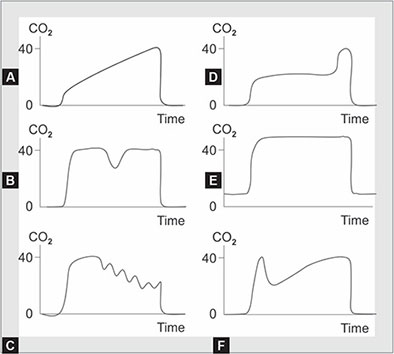
The angle between phase II and III is called alpha angle, which increases as slope of phase III increases. Normally, it is about 100–110°. Airway obstruction increases the angle due to increase in the slope phase II and phase III. The response time of the capnograph, sweep speed, and the respiratory cycle time also affect the angle. On the other hand, the angle between phase III and phase 0 is called beta angle, which is normally about 90°. During rebreathing, this angle increases. Occasionally, an upward blip or spike, known as phase IV, can occur towards the end of phase III. This terminal elevation represents emptying of alveoli with long time constants containing higher CO2 concentration. The maximal CO2 level, the best reflection of alveolar CO2, is known as end-tidal CO2 (EtCO2). This is generally depicted in concentration as EtCO2 or if in partial pressure of CO2, PEtCO2. This is the number that is displayed on the monitor. PEtCO2 is the best reflection of alveolar CO2 (PACO2) and, normally the arterial CO2 (PaCO2)−PEtCO2 difference is about 5 mm Hg due to the alveolar dead space. 5There are several clinical possibilities where abnormal capnograms can occur; the most common to anesthesia practice are depicted in Figures 7A to F.
Fig. 5: Normal time capnogram: Phase I: End of inhalation and beginning of exhalation (dead space ventilation). Phase II: Rapid rise of CO2 due to mixing of the dead space gas with alveolar CO2. Phase III: Alveolar plateau. The exhalation of the CO2 from the alveoli. It reaches a peak where the partial pressure of CO2 is the highest. Phase 0: Partial pressure of CO2 decreases rapidly at the beginning of the inspiration.
Applications of Time Capnography
In the operating rooms, capnography plays a vital role in detecting breathing circuit disconnection instantly when the capnograph no longer detects the EtCO2.6
|
Figs. 7A to F: Examples of several abnormal capnograms. (A) Capnogram of a patient with severe chronic obstructive pulmonary disease (COPD), or other causes leading to the increased airway resistance, such as asthma, endobronchial intubation, endotracheal tube kinking. No plateau is reached before the next inspiration. The gradient between PEtCO2 and arterial CO2 is increased; (B) Downward wave during plateau phase indicates spontaneous respiratory effort; (C) Cardiogenic oscillations appear as small, regular, tooth like humps at the latter part of the expiratory phase. The rate of the “humps” is identical to the patient's heart rate; (D) A leak in the sampling line during positive pressure ventilation; (E) Failure of inspired CO2 to return to zero due to an incompetent expiratory valve or exhausted CO2 absorbent; (F) Bifid waveform of expired CO2 in patient with emphysema undergoing elective surgery after unilateral lung transplantation. The initial upstroke represents gas from the normal (transplanted) lung, which is followed by gas exhaled from the remaining (emphysematous) lung.
This is followed by drop-in oxygen saturation. EtCO2 is probably the best method to detect disconnections; a decrease or absence of EtCO2 is highly sensitive but not specific for anesthesia circuit disconnections. Beyond this important and vital application, capnography serves to provide the clinician with enormous data information about the patient's overall physiology that can help clinicians to identify cardiac, ventilatory, and metabolic abnormalities and they are outlined below:
- Confirmation of tracheal intubation: 2015 American Heart Association Guidelines on Advanced Adult Cardiac Life Support endorsed continuous waveform capnography in addition to clinical assessment for confirming the ETT placement.7 To note, a normal waveform can occur when the tube has been placed in the right mainstem bronchus too. A flatline waveform immediately after ETT placement usually indicates esophageal placement. Other common scenarios with a flatline waveform include:
- Anesthesia circuit disconnections.
- Technical malfunction of the monitor or sampling tube.
- Endotracheal tube complete obstruction (e.g., clotted blood).
- Prolonged cardiac arrest with cellular death (no CO2 production at a cellular level).
Unrecognized misplaced endotracheal intubation by healthcare providers was widespread in the past8,9 and has been significantly reduced by the use of EtCO2 monitoring. Confirmation of correct tube placement using clinical signs has shown to be unreliable. The “Fourth National Audit Project” by Royal College of Anesthetists (RCoA) and Difficult Airway Society stressed the importance of capnography in confirming tracheal intubation in all clinical settings through “No Trace = Wrong Place” campaign. Capnography also provides reliable information on the correct placement of supraglottic airway devices. - Assessing tracheal tube and tracheostomy patency and position: Capnography for the duration the patient remains on artificial airway was cited as the most effective way of reducing morbidity and mortality.10 Capnography monitoring gives real-time information on the patient's airway patency. A change in waveform is usually seen before a decrease in oxygen saturation and should be immediately assessed.11
- Guide adequacy of ventilation: Capnography is commonly used to detect hypercapnia due to hypoventilation and hypocapnia due to hyperventilation.11 In general, the PaCO2 levels are higher by about 5 mm Hg. In patients with essentially normal lungs and cardiac output, EtCO2 can be used to noninvasively monitor PaCO2. An initial arterial blood gas can be performed to determine the gradient (Arterial-EtCO2), further ventilatory adjustments can be made just using EtCO2 as a guide. If the patient has chronic obstructive pulmonary disease (COPD) or unstable cardiac output, EtCO2 may not be a perfect guide. It can also be used for weaning patients from mechanical ventilation. Arterial to EtCO2 difference gives a fair idea about physiological dead space. If the gradient stabilizes or it decreases over time from initially a large gradient, this demonstrates indirectly that the patient's V/Q status is improving.128
- Procedural sedation: Capnography has been widely used as a respiratory monitor in addition to pulse oximeter during surgical procedures requiring sedation. Capnography will identify hypoventilation long before the pulse oximeter detects hypoxemia, this is especially true in patients receiving supplemental oxygen during sedation (Figs. 8A and B). A comprehensive meta-analysis of 13 randomized clinical trials provides clear evidence that capnography monitoring is more sensitive to identify respiration related adverse events used during procedural sedation. In addition, there is a statistically significant and clinically meaningful reduction in episodes of desaturation as well as requirement of assisted ventilation.13 During sedation, expired gases are diluted by oxygen administration, and the CO2 waveforms may not appear in normal shape. Under these circumstances, a change from baseline is an important criterion of excessive sedation resulting in hypoventilation or airway obstruction. A systematic approach to changes in CO2 waveforms can troubleshoot respiratory events during sedation (Flowchart 1).
- During percutaneous tracheostomy placement: Percutaneous tracheostomy is an invasive procedure and may rarely result in significant patient harm due to incorrect placement. Capnography improves safety by confirming that the tracheostomy tube is correctly placed in the trachea at the end of the procedure. Capnography can be also used as an alternative to fiberoptic bronchoscopy, if unavailable or contraindicated, to detect correct tracheal needle placement before performing percutaneous tracheostomy.14
- Monitoring patients with raised intracranial pressure: Capnography is an essential tool for management of patients with raised intracranial pressure (ICP), both in the operating room and critical care setting. PaCO2 has a profound and reversible effect on cerebral blood flow. Cerebral blood flow is linearly responsive to PaCO2 level.15 Capnography can be used as a continuous monitor of EtCO2 which is the best reflective of PaCO2 level during ICP management.
- Monitoring response to treatment of bronchospasm: A patient with bronchospasm usually has a capnogram with an exaggerated up-sloping plateau phase, with a prolonged phase II representing slow expiration of respiratory gases. In addition to conventional methods, capnography can be used to assess response to bronchodilators.11 Capnography is advantageous when compared to peak flow meter because it is independent of efforts and provides continuous monitoring.
- Estimation of cardiac output: An increase in cardiac output and pulmonary blood flow results in better perfusion of the alveoli and a rise in EtCO2. Provided the ventilation remains constant, the EtCO2 provides a continuous trend of pulmonary blood flow and therefore, an estimation of cardiac output. During constant minute ventilation and tissue CO2 production, an abrupt reduction in blood flow reduces EtCO2 via two mechanisms. First, a reduction in venous return causes a decrease in delivered CO2 to the alveoli, resulting in a decrease in alveolar PCO2 (PaCO2) and, consequently, EtCO2. Second, reduced pulmonary vascular flow will result in an increase in alveolar dead space, which will dilute the CO2 from normally perfused alveolar spaces, thus decreasing EtCO2 below PaCO2.16 A number of studies have shown that EtCO2 can be useful in estimating a change in cardiac output in a variety of clinical scenarios like cardiac arrest, circulatory shock, and major surgeries.17,18
- Assessment of efficacy of cardiopulmonary resuscitation (CPR) and prediction of survivability: Utilization of capnography in the following ways during CPR improves the survival outcomes in cardiac arrest.19,20
- Confirms the correct placement and patency of the airway device.
- Monitor ventilation, avoiding hyper and hypoventilation.
- Assess the adequacy of chest compression during CPR.
- Early assessment of return of spontaneous circulation (ROSC) during CPR.
- Used in decision making for prognostication during CPR. In intubated patients, failure to achieve an EtCO2 of >10 mm Hg by waveform capnography after 20 minutes of CPR may be considered as one component of a multimodal approach to decide when to terminate resuscitative efforts but should not be as a sole criterion7(Fig. 9).10
- Detection of inadvertently placed nasogastric tube: In a meta-analysis of nine clinical trials of mechanically ventilated patients, the use of capnography for inadvertent tracheal placement of the nasogastric tube had a sensitivity ranging from 0.88 to 1.00, specificity 0.95–1.00, positive likelihood ratio 15.22–283.35, negative likelihood ratio 0.01–0.25.21
- Monitoring during patient transport: Monitoring capnography waveforms with pulse oximetry during transport assures the integrity of airway and prevents mishaps during interhospital or intrahospital transfers. If ventilation is kept constant, an abrupt decrease in EtCO2 values must be immediately investigated; it may be due to decreased cardiac output.22
- Sepsis: Capnography has potential prognostic value in sepsis to gauge lactate levels. EtCO2 demonstrates an inverse relationship with lactate levels.23,24 EtCO2 levels <25 mm Hg demonstrate a 0.93 sensitivity for mortality in these studies. In another study, a significant correlation was noted between EtCO2 and sequential organ failure assessment (SOFA) score (r = −0.35, p < 0.01), and EtCO2 and lactate level (r = −0.35, p < 0.01). A receiver operator curve for EtCO2 and SOFA > 2 had an area under curve (AUC) of 0.69. EtCO2 of <35 has a sensitivity of 0.73 (95% CI 0.56–0.85) and specificity 0.50 (0.38–0.62) in predicting SOFA scores >2. EtCO2 < 35 mm Hg had a sensitivity of 0.60 (0.22–0.88) and specificity 0.42 (0.32–0.52) in predicting lactate >4 with an AUC of 0.62. There was a statistically significant correlation between EtCO2 and SOFA scores, but association was not strong enough for clinical decision making.25
- Trauma resuscitation: In blunt trauma prehospital patients who underwent intubation, EtCO2 were greater in survivors (30.8 mm Hg in survivors and 26.3 mm Hg in nonsurvivors). EtCO2 also demonstrates a strong inverse relationship with lactate in patients with penetrating trauma.26 A recent 11study released in injury finds capnography levels <35 mm Hg had an association with indicators of shock and need for blood transfusion in the first 6 hours of admission.27
- Fluid responsiveness: In a recent study, capnography outperformed other indices such as, pulse pressure variation, systolic blood pressure, heart rate, and mean blood pressure during fluid challenge in patients undergoing mechanical ventilation.28 Further studies are required to assess the efficacy of EtCO2 for fluid management.
- Seizures: EtCO2 can provide an assessment of the ventilatory status of a patient who is actively seizing or in a postictal state.26
Volume Capnography
Volume capnography is the graphical representation of partial pressure of CO2 versus exhaled volume. This measurement is made noninvasively at every breath by a combination of flow and CO2 sensors, which are positioned together at the Y piece of ventilator circuit. Under normal circumstances there is a difference of 2–5 mm Hg between arterial and alveolar CO2, (PaCO2-PEtCO2 gradient) but this can differ considerably with ventilation perfusion (V/Q) mismatch in the lungs. Volume capnography can provide much more information than time capnography in situations where there is an alteration in V/Q ratio. A volume capnogram can be divided into various components as defined here (Fig. 6). A horizontal line representing PaCO2 (arterial blood sampled during the PEtCO2 recordings) is drawn on the CO2 trace. The area under the curve (green area), is the volume of CO2 in the breath and represents effective alveolar ventilation. The remaining area represents wasted ventilation (physiological dead space). A vertical line is drawn through phase II so that the two areas p and q are equal. Area under light blue represents anatomical dead space and area under dark blue represents alveolar dead space.22
Applications of Volume Capnography
- Assessing adequacy of ventilation.
- Volume capnography can assess the adequacy of ventilation. However, in mechanically ventilated ICU patients, there is often a large difference between simultaneous measurements of PaCO2 and PEtCO2. Once the difference between PEtCO2 and PaCO2 is established volume capnography can be used as a guide of PaCO2.
- Estimation of optimal positive end-expiratory pressure (PEEP).
- Exclusion of pulmonary embolism.
- Pulmonary embolism can be excluded by volume capnography when D-dimers are positive and track the efficacy of thrombolysis in patients with major thromboembolism.
- Noninvasive estimation of cardiac output and volume responsiveness.
- The accuracy of estimation with volume capnography is similar to esophageal Doppler ultrasound, pulse contour analysis, and thoracic bioimpedance.
- Estimation of dead space.
- Volume capnography can be used to determine breath by breath physiological dead space (Bohr Dead space).5
LIMITATIONS
Even more than 40 years after the introduction of capnography, patients are still dying because of unrecognized esophageal intubation or tracheal tube displacement. These deaths are occurring either through failure to use this reliable technology, or failure to interpret an abnormal capnograph waveform.31 In some countries, capnography units are not used even when available due to lack of knowledge to interpret capnography.31 Despite valuable information provided by capnography, there are few limitations like any other monitoring modality and hence requires caution in the interpretation of the data. Capnography is more reliable in patients where there is isolated ventilation, perfusion, or metabolism issue. However, patients with mixed pathophysiology pose challenges for interpretation.
False-positive CO2 detection could occur in esophageal intubations if the patient ingested carbonated beverages. Acidic solution exposure, such as stomach content fluid or vinegar, can result in qualitative color change in colorimetric method. Waveform capnography is much more reliable under these circumstances.
Mainstream devices are near ETT and face, and hence caution must be exercised to avoid facial burns due to IR assembly. Sidestream devices may result in time delay, but this is of less clinical significance in clinical practice. The sampling lines and IR window are prone to obstructions by secretions. The sampling tube must be positioned antigravity (vertically upward) and a small filter between the sampling line and the ETT minimizes the blockade with secretions.
It is common to use EtCO2 monitoring during transfer of patients by aircraft and in high altitude locations. In order to provide safe patient transport care, a knowledge about ambient pressure effect on gas analysis is essential. Gas analyzers are calibrated to measure partial pressure of the gas at sea level. Reduction of atmospheric pressure at high altitude will affect capnography in the following ways:32
- Pumping of gas through the sample chamber—more powerful pump may be required to maintain flow rates.
- Fall in barometric pressure may be electronically sensed as a gas leak within the monitor. However, the clinical significance of these variations can be minimized, or must be considered while interpreting EtCO2 values.
FUTURE TRENDS AND CONCLUSION
With growing understanding of capnography, and increasing litigations outside of the operating rooms, it is inevitable that many procedural sedation facilities, ICU, and emergency departments will use capnography in future. In the emergency medicine environment, capnography has expanded from CPR and ventilated patients, to use in spontaneously breathing patients in every clinical application, across the continuum of care. The use of capnography could soon become a standard of care in all critically ill on mechanical ventilation during interhospital or intrahospital transfer. The addition of algorithms and technology like integrated pulmonary index (IPI) has also helped clinicians to recognize and intervene in any respiratory compromise. Capnography can facilitate airway management in a neonate as an indicator of gas exchange, lung aeration, early identification of obstruction, early recognition of ROSC, and probably the quality of the administered chest compressions.33 Volumetric capnography can make a profound impact on the respiratory weaning protocol and shorten the duration of respiratory life support on patients requiring mechanical ventilation. There is growing trend of utilization of this technology in the ICU to measure physiological dead space, oxygen consumption, and CO2 production.
REFERENCES
- Gelb AW, Morriss WW, Johnson W, Merry AF, International Standards for a Safe Practice of Anesthesia Workgroup. World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) International Standards for a Safe Practice of Anesthesia. Can J Anaesth. 2018;65(6):698–708.
- Bhavani-Shankar K, Moseley H, Kumar AY, Delph Y. Capnometry and anaesthesia. Can J Anaesth. 1992;39(6):617–32.
- Bhavani-Shankar K, Kumar AY, Moseley HS, Ahyee-Hallsworth R. Terminology and the current limitations of time capnography: a brief review. J Clin Monit. 1995;11(3):175–82.
- Block FE Jr, McDonald JS. Sidestream versus mainstream carbon dioxide analyzers. J Clin Monit. 1992;8(2):139–41.
- Bhavani-Shankar K, Philip JH. Defining segments and phases of a time capnogram. Anesth Analg. 2000;91(4):973–7.
- Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S444–64.
- Jones JH, Murphy MP, Dickson RL, Somerville GG, Brizendine EJ. Emergency physician-verified out-of-hospital intubation: miss rates by paramedics. Acad Emerg Med. 2004;11(6):707–9.
- Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37(1):32–7.
- Cook TM, Woodall N, Harper J, Benger J, Fourth National Audit P. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth. 2011;106(5):632–42.
- Kerslake I, Kelly F. Uses of capnography in the critical care unit. BJA Education. 2016;17(5):178–83.
- Lucangelo U, Bernabe F, Vatua S, Degrassi G, Villagra A, Fernandez R, et al. Prognostic value of different dead space indices in mechanically ventilated patients with acute lung injury and ARDS. Chest. 2008;133(1):62–71.
- Saunders R, Struys M, Pollock RF, Mestek M, Lightdale JR. Patient safety during procedural sedation using capnography monitoring: a systematic review and meta-analysis. BMJ Open. 2017;7(6):e013402.
- Mallick A, Venkatanath D, Elliot SC, Hollins T, Nanda Kumar CG. A prospective randomised controlled trial of capnography vs. bronchoscopy for Blue Rhino percutaneous tracheostomy. Anesthesia. 2003;58(9):864–8.
- Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth edition. Neurosurgery. 2017;80(1):6–15.
- Isserles SA, Breen PH. Can changes in end-tidal PCO2 measure changes in cardiac output? Anesth Analg. 1991;73(6):808–14.
- Matsumoto A, Itoh H, Eto Y, Kobayashi T, Kato M, Omata M, et al. End-tidal CO2 pressure decreases during exercise in cardiac patients: association with severity of heart failure and cardiac output reserve. J Am Coll Cardiol. 2000;36(1):242–9.
- Jin X, Weil MH, Tang W, Povoas H, Pernat A, Xie J, et al. End-tidal carbon dioxide as a noninvasive indicator of cardiac index during circulatory shock. Crit Care Med. 2000;28(7):2415–9.
- Soar J, Nolan JP, Bottiger BW, Perkins GD, Lott C, Carli P, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100-47.
- Kodali BS, Urman RD. Capnography during cardiopulmonary resuscitation: current evidence and future directions. J Emerg Trauma Shock. 2014;7(4):332–40.
- Chau JP, Lo SH, Thompson DR, Fernandez R, Griffiths R. Use of end-tidal carbon dioxide detection to determine correct placement of nasogastric tube: a meta-analysis. Int J Nurs Stud. 2011;48(4):513–21.
- Kodali BS. Capnography outside the operating rooms. Anesthesiology. 2013;118(1):192–201.
- Guirgis FW, Williams DJ, Kalynych CJ, Hardy ME, Jones AE, Dodani S, et al. End-tidal carbon dioxide as a goal of early sepsis therapy. Am J Emerg Med. 2014;32(11):1351–6.
- McGillicuddy DC, Tang A, Cataldo L, Gusev J, Shapiro NI. Evaluation of end-tidal carbon dioxide role in predicting elevated SOFA scores and lactic acidosis. Intern Emerg Med. 2009;4(1):41–4.
- Long B, Koyfman A, Vivirito MA. Capnography in the Emergency Department: a review of uses, waveforms, and limitations. J Emerg Med. 2017;53(6):829–42.
- Stone ME, Jr., Kalata S, Liveris A, Adorno Z, Yellin S, Chao E, et al. End-tidal CO2 on admission is associated with hemorrhagic shock and predicts the need for massive transfusion as defined by the critical administration threshold: a pilot study. Injury. 2017;48(1):51–7.
- Lakhal K, Nay MA, Kamel T, Lortat-Jacob B, Ehrmann S, Rozec B, et al. Change in end-tidal carbon dioxide outperforms other surrogates for change in cardiac output during fluid challenge. Br J Anaesth. 2017;118(3):355–62.
- Lam T, Nagappa M, Wong J, Singh M, Wong D, Chung F. Continuous pulse oximetry and capnography monitoring for postoperative respiratory depression and adverse events: A systematic review and meta-analysis. Anesth Analg. 2017;125(6):2019–29.
- Whitaker DK. Time for capnography - everywhere. Anaesthesia. 2011;66(7):544–9.
- Cook TM, Harrop-Griffiths W. Capnography prevents avoidable deaths. BMJ. 2019;364:l439.
- Pattinson K, Myers S, Gardner-Thorpe C. Problems with capnography at high altitude. Anaesthesia. 2004;59(1):69–72.
- Cereceda-Sanchez FJ, Molina-Mula J. Systematic review of capnography with mask ventilation during cardiopulmonary resuscitation maneuvers. J Clin Med. 2019;8(3):358.